Abstract
Background
Atrial fibrillation (AF) is a common heart rhythm disorder that can lead to complications such as stroke and heart failure. Radiofrequency ablation (RFA) is a procedure used to treat AF, but it is not always successful in maintaining a normal heart rhythm. This study aimed to construct a clinical prediction model based on extreme gradient boosting (XGBoost) for AF recurrence 12 months after ablation.
Methods
The 27-dimensional data of 359 patients with AF undergoing RFA in the First Affiliated Hospital of Soochow University from October 2018 to November 2021 were retrospectively analysed. We adopted the logistic regression, support vector machine (SVM), random forest (RF) and XGBoost methods to conduct the experiment. To evaluate the performance of the prediction, we used the area under the receiver operating characteristic curve (AUC), the area under the precision-recall curve (AP), and calibration curves of both the training and testing sets. Finally, Shapley additive explanations (SHAP) were utilized to explain the significance of the variables.
Results
Of the 27-dimensional variables, ejection fraction (EF) of the left atrial appendage (LAA), N-terminal probrain natriuretic peptide (NT-proBNP), global peak longitudinal strain of the LAA (LAAGPLS), left atrial diameter (LAD), diabetes mellitus (DM) history, and female sex had a significant role in the predictive model. The experimental results demonstrated that XGBoost exhibited the best performance among these methods, and the accuracy, specificity, sensitivity, precision and F1 score (a measure of test accuracy) of XGBoost were 86.1%, 89.7%, 71.4%, 62.5% and 0.67, respectively. In addition, SHAP analysis also proved that the 6 parameters were decisive for the effect of the XGBoost-based prediction model.
Conclusions
We proposed an effective model based on XGBoost that can be used to predict the recurrence of AF patients after RFA. This prediction result can guide treatment decisions and help to optimize the management of AF.
Similar content being viewed by others
Introduction
Atrial fibrillation (AF) is a common heart rhythm disorder that affects millions of people worldwide. It is characterized by irregular and rapid electrical activity in the upper chambers (atria) of the heart, leading to an irregular heartbeat. The causes of AF are complex and multifactorial. Risk factors for AF include advanced age, hypertension, heart disease, diabetes, obesity, and a family history of the condition [1,2,3]. Certain lifestyle factors, such as excessive alcohol consumption, smoking, and lack of physical activity, can also increase the risk of developing AF. AF can have serious consequences, including an increased risk of stroke and heart failure. The irregular heartbeat can cause blood to pool in the heart, increasing the risk of blood clot formation that can lead to a stroke. The risk of stroke in people with AF is five times higher than that in those without AF [1]. The diagnosis of AF is typically made using electrocardiography (ECG) or other cardiac monitoring techniques [4, 5]. Treatment for AF includes medication to control the heart rate and rhythm, anticoagulation therapy to reduce the risk of stroke, and sometimes procedures such as cardioversion or ablation to restore normal heart rhythm [6].
Radiofrequency ablation (RFA) is a procedure used to treat AF. During RFA, a catheter with an electrode at its tip is guided into the heart through a vein in the groin or neck. The electrode emits high-frequency radio waves that create heat and isolate the abnormal heart tissue that causes irregular heartbeats [7]. While RFA has been found to be effective in treating AF, some patients experience recurrence of AF after the procedure. Studies have shown that the 12-month recurrence rate of AF after RFA is approximately 15–30% [2, 8]. However, the exact rate may vary depending on several factors, including patient characteristics, the extent of AF, and the techniques used during RFA. Several factors have been identified as predictors of the 12-month recurrence rate of AF after RFA. These include a larger left atrial size, a longer duration of AF, and the presence of underlying heart disease [9, 10]. Additionally, inadequate lesion formation during RFA or incomplete pulmonary vein isolation, the pulmonary vein being a common target during the procedure, can also increase the risk of 12-month recurrence of AF [11]. Patients who experience recurrence of AF after RFA may require further treatment, such as repeat RFA or medical therapy [12,13,14]. It is essential to closely monitor patients after RFA to detect those who experience recurrence of AF and provide appropriate treatment promptly.
The anatomical substrate of AF patients is mostly derived from the left atrium. Substantial studies have shown a relationship between the anatomy and function of the left atrium and the recurrence of AF after RFA [15, 16]. In addition, as an accessory structure of the left atrium, the left atrial appendage (LAA) is more sensitive to changes in left atrial function, and its role in predicting recurrence after RFA has been reported [17, 18]. Strain imaging of the LAA can reflect the myocardial deformation of the latter, so it can accurately reflect the function of the LAA [19]. However, due to limitations in sample size and method of measurement, the few studies on the relationship between LAA strain and recurrence of AF did not reach a positive outcome [20, 21].
In this study, we used left atrial parameters, optimized LAA indicators combined with clinical demographics and laboratory indicators to construct clinical prediction models based on the XGBoost method for AF recurrence to accurately identify patients prone to recurrence after RFA and implement individualized treatment among AF patients.
Machine learning algorithms are an important branch of artificial intelligence that can automatically learn from data and be used to better explore data information, so they present high application value in prediction in clinical settings [22, 23]. In this study, we used four high-performance algorithms to build predictive models, including logistic regression, support vector machine (SVM), random forest (RF) and extreme gradient boosting (XGBoost), to identify recurrence after RFA among AF patients.
Methods
Study population
The Ethics Committee of The First Affiliated Hospital of Soochow University approved the study (No.: 184/2022), and the study conformed to the Declaration of Helsinki (2013 Revision). A total of 392 AF patients who underwent RFA at the First Affiliated Hospital of Soochow University from October 2018 to November 2021 were included in the study. The inclusion and exclusion criteria are presented in Table 1. All patients underwent routine echocardiography and 24-hour ECG in our hospital three months after the procedure to determine the negative remodelling of the left atrium and the presence of atrial arrhythmia episodes. If palpitation or other symptoms occurred, patients were recommended to the nearest hospital and completed a 24-hour ECG as soon as possible. AF recurrence was defined as an episode of atrial arrhythmias persisting for at least 30 s in any way after 3 months. All subjects were followed up for 12 months.
Data collection and analysis
All patients’ baseline data were collected from their electronic medical records (EMR), including age, sex, body mass index (BMI), smoking and drinking history, AF classification, hypertension history, diabetes mellitus (DM) history, neutrophil-to-lymphocyte ratio (NLR), haemoglobin concentration, N-terminal probrain natriuretic peptide (NT-proBNP), estimated glomerular filtration rate (eGFR), high sensitivity C-reactive protein (hs-CRP), blood plasma albumin (ALB), and D-dimer levels. In our study, drinking history was defined as moderate or higher drinking, involving more than 8 drinks per week. Twenty-seven-dimensional data (Table 2) were included in the statistical analysis. Variables with a normally distributed or non-normal distribution are expressed as the means ± standard deviations or medians (quartiles), respectively. Categorical variables were expressed as counts (proportion). Numerical differences between two groups were assessed by the Chi-square test or Fisher’s exact test for categorical variables, while the t test and Kruskal–Wallis H test or Mann–Whitney U test were used for continuous variables. The threshold for significance was P = 0.05.
First, parameters with significant differences were initially selected through the T test, Kruskal–Wallis H test or Mann–Whitney U test. Second, considering the collinearity between variables, we further screened the parameters with significant differences from the selected parameters by the backwards stepwise regression method based on the Akaike information criterion (AIC). We also introduced left atrial appendage ejection fraction (LAAEF) as an additional predictor of AF recurrence according to the latest research [24, 25]. Considering that logistic regression is a linear model of the four models, we conducted a collinearity test on the six variables, and the result showed that VIF < 5, so there was no collinearity among the six variables that were finally entered into the models. All data analyses were conducted using Python, Version 3.8.8.
Model development and validation
All data were divided into a training set and a testing set at a ratio of 8:2. Four machine learning algorithms were utilized to construct the prediction model, including logistic regression, SVM, RF and XGBoost. Grid searches were used to adjust the parameters. In this study, we utilized 5-fold cross-validation during the model construction process. The combined area under the receiver operating characteristic curve (AUC) was used to evaluate the accuracy and calibration performance and to select the optimal model for predicting the 12-month recurrence of AF after RFA. Moreover, in this study, we also applied the SHapley Additive exPlanations (SHAP) algorithm to fully demonstrate the marginal contribution of each variable in the optimal model. The data collection, model construction, and evaluation processes are shown in Fig. 1.
Results
Comparison of clinical data between the two groups
After 17 patients were excluded due to poor-quality oesophageal ultrasound images, a total of 392 patients diagnosed with AF were included in this study. Thirty-three patients were excluded from the study due to missing data or loss of follow-up. A total of 359 AF patients were eventually enrolled in the analysis, with 61 patients in the recurrence group and 298 in the nonrecurrence group according to their recurrence status at their 12-month follow-up. Comparison of demographics, laboratory data, echocardiography and oesophageal echocardiography results between the two groups showed significant differences in age, sex, presence of persistent AF, diabetes history, NT-proBNP, hs-CRP, ALB, D-dimer, left atrial diameter (LAD), right atrial diameter (RAD), left ventricular ejection fraction (LVEF), peak mitral valve flow velocity during early ventricular diastole (E), peak mitral ring motion velocity during early ventricular diastole (e’), ratio of E to E’ (E/e’), E deceleration time (EDT), left atrial appendage ejection fraction (LAAEF) and left atrial appendage global peak longitudinal strain (LAAGPLS) as shown in Table 2. Representative LAA strain images from patients in the two groups are shown in Fig. 2.
Variable selection
We conducted a multivariate backwards stepwise logistic regression analysis to identify factors associated with recurrence of AF after univariate regression (Table 3). Five variables, female sex (OR: 2.104, 95% CI: 1.018, 4.349, P = 0.05), DM (OR: 2.362, 95% CI: 0.945, 5.903, P = 0.07), NT-proBNP (OR: 1.000, 95% CI: 1.000, 1.000, P = 0.03), LAD (OR: 1.139, 95% CI: 1.057, 1.228, P < 0.01), and LAAGPLS (OR: 0.763, 95% CI: 0.690, 0.844, P < 0.01), were screened by stepwise regression (P < 0.1) as shown in Table 4. The role of reduced LAAEF in predicting AF recurrence after RFA has been shown in recent studies [24, 25]. Therefore, we also incorporated LAAEF into our prediction model.
Model construction and evaluation
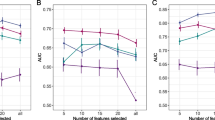
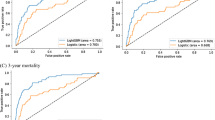
A total of 359 patients were enrolled in this study, but only 61 patients relapsed after RFA. Therefore, it can be said that the sample distribution was unbalanced. To solve the problem of uneven sample distribution, we applied the synthetic minority oversampling technique (SMOTE) to balance the samples in this study. We also applied standardized methods to process the selected 6-dimensional variables before constructing the models. In addition, we simultaneously plotted a precision-recall (PR) curve to fully assess the model power. After adjusting the model parameters (Supplementary Table 1), we found that the logistic regression (LR), SVM, RF and XGBoost models performed well on the training set. As shown in Fig. 3A and Fig. 3B, on the training set, XGBoost had a better performance (AUC = 0.92, AP = 0.77) than RF (AUC = 0.91, P = 0.73), SVM (AUC = 0.82, AP = 0.61) and LR (AUC = 0.85, AP = 0.58). In addition, XGBoost also had a better performance (AUC = 0.87, AP = 0.75) than RF (AUC = 0.86, AP = 0.73), SVM (AUC = 0.78, AP = 0.60), and LR (AUC = 0.82, AP = 0.57) on the testing set (Fig. 3C and Fig. 3D). Figure 4 presents the confusion matrix of the four models in the testing set. Table 5 shows that the superior sensitivity and F1 score of XGBoost were 71.4% and 0.67, respectively. The XGBoost and RF prediction models had the same accuracy (86.1% and 86.1%). XGBoost had a lower specificity (89.7% and 93.1%) and precision (62.5% and 66.7%) than the RF model in predicting 12-month AF recurrence after RFA. Finally, the calibration curve of XGBoost in Fig. 5 was closer to the diagonal (y = x). In view of clinical practice, it is more important to identify as many patients as possible who relapse after RFA. Therefore, the XGBoost model has the best performance and clinical application of the four models.
(A) ROC curve of the training set in the logistic regression, SVM, RF and XGBoost models; a larger AUC indicates a stronger discriminatory ability; (B) PR curve of the training set in the logistic regression, SVM, RF and XGBoost models; a larger AP indicates a better identification ability of 12-month recurrence in the training set data; (C) ROC curve of the testing set in the logistic regression, SVM, RF and XGBoost models; (D) PR curve of the testing set in the logistic regression, SVM, RF and XGBoost models
Explanatory nature of model parameters
To investigate the contribution of the parameters in predicting 12-month AF recurrence, we also applied a SHAP algorithm for the calculation and ranking of the contribution of each parameter; this is illustrated in Fig. 6A, in which LAAEF and LAAGPLS are shown to be negatively correlated with 12-month AF recurrence after RFA, while NT-proBNP, LAD, female sex and DM history are positively correlated with 12-month AF recurrence after RFA. As shown in Fig. 6B, the SHAP values of LAAEF, NT-proBNP, LAAGPLS and LAD were larger, indicating that they were important predictors of 12-month AF recurrence. Female sex and DM history had smaller SHAP values; thus, they made limited contributions to the model.
(A) The SHAP value of each variable in the XGBoost model. Each row represents a variable, and values closer to the top indicate a greater average SHAP value. The SHAP value represents the degree of influence of the variable on the results. One point in each variable represents a sample, and a deeper red colour indicates a greater characteristic value; (B) The average SHAP value of each variable; variables contribute more to the prediction model when their SHAP value is larger
Discussion
This study demonstrated the use of LAA functional parameters in predicting AF recurrence 12 months after RFA, of which LAAEF had the greatest application value, while the optimized LAA functional evaluation index LAAGPLS also had excellent application value. In addition, we combined the results of LAA functional parameters, cardiac global structural and functional parameters, and laboratory tests to construct four clinical prediction models for 12-month AF recurrence after RFA, of which the XGBoost model had the greatest value.
Changes in left atrial structure and function are essential in the development of AF. Several studies have linked left atrial indicators to recurrence of AF after RFA, even in patients undergoing cryoablation [15, 26, 27]. The majority of current studies revealed that left atrial enlargement was an independent predictor of recurrence after RFA [28], while scholars in some studies reported a U-shaped relationship between left atrial size and AF recurrence; that is, patients with small atria were also prone to AF recurrence [8]. In our study, left atrial size was positively correlated with AF recurrence 12 months after RFA. Heart failure is mainly characterized by changes such as decreased LVEF or increased NT-proBNP, and such patients are more likely to suffer from left atrial remodelling due to increased left atrial pressure [3, 29]. Our study found that an increase in NT-proBNP was an independent predictor of AF recurrence 12 months after RFA, which was consistent with previous studies [9, 30, 31]. Compared with research that proved that EDT could reflect cardiac function to some extent [32], the results of this study suggested a certain effect of EDT on predicting 12-month recurrence of AF.
Inconsistent results concerning the use of female sex as a predictor of recurrence after AF ablation have been reported. Some studies have shown a similar recurrence after RFA between females and males [33,34,35]. However, a recent large sample size study revealed that females have a higher recurrence rate after RFA (OR: 1.26, 95% CI: 1.15–1.38) [35]. In our study, female sex seemed to be associated with AF recurrence 12 months after RFA. However, it had a limited application value due to the small SHAP value. Previous studies also revealed that patients with DM had a greater risk of AF recurrence after RFA than those without DM [36, 37]. It appeared that including the variable of DM can increase the predictive power of our models. Since the variable had a minimal SHAP value, we can only state that it is of rather limited use in predicting the 12-month recurrence of AF.
As an accessory structure of the left atrium, the LAA has many trabecular muscles inside, and the myocardial thickness is thin, with a thickness of approximately 1 mm [38]. Some studies on the physiological roles of LAA have shown that 30% of the atrial natriuretic peptide was secreted by the LAA [39]. In addition, the LAA is also the origin of many atrial arrhythmias [40, 41]. In patients with AF, structural and functional changes also occur in the LAA, and LAA structural and functional parameters can predict the recurrence of AF after RFA [42, 43]. Tian et al. followed up on patients undergoing RFA for 19 months, finding a high clinical value of LAAEF in predicting the recurrence of AF with a hazard ratio of 0.790 (95% CI: 0.657–0.950) [20]. In our study, LAAEF was negatively correlated with the 12-month AF recurrence rate with the largest SHAP value, indicating that LAAEF had important clinical value in predicting 12-month recurrence of AF after RFA. New findings in myocardial strain in recent years have shown a high clinical value of left atrial strain in predicting recurrence of AF after RFA, but studies on the value of LAAGPLS remain scarce or have had nonsignificant results [21, 44]. In our study, the follow-up results of 359 patients revealed that LAAGPLS was an independent predictor of AF recurrence after RFA. Considering situations of complex LAA movement patterns, difficult strain measurement, and poor reproducibility, we defined LAAGPLS as the sum of the positive and negative absolute global peak strain values, which was more repeatable. Hence, we believe that the positive results of this study were related to our optimization of measurement methods.
At this stage, artificial intelligence algorithms are widely applied to solve clinical problems due to their ability to overcome the limitations of traditional linear relationships between dependent and independent variables. RF and XGBoost, in particular, as tree model-based integration algorithms, have shown high application value in clinical classification and regression problems [45, 46]. Labarbera et al. noted that a machine learning algorithm combining pulmonary vein morphology and clinical data was useful for predicting AF recurrence after RFA [47], but no known studies have focused on the predictive value of a machine learning model of the functional parameters of the left atrium and LAA. Our machine learning model combined clinical indicators and transoesophageal echocardiographic functional parameters, and the results indicated that the XGBoost algorithm had the best performance and could be used for accurate prediction of AF recurrence 12 months after RFA.
Limitations
In this study, some limitations were identified. Since this study was conducted in a single centre, external validation was not possible. Second, in this study, the sample size was relatively small, with only 61 cases in the recurrence group. Third, the follow-up time of our study was 12 months; thus, there was an absence of long-term follow-up on AF recurrence after RFA. Last, many clinical parameters, such as AF duration, AF burden, and ECG parameters, such as P-wave duration, were not studied in our research. In the future, a larger sample size and more clinical parameters will be needed to improve the efficiency of these models, and an external dataset will also be needed to validate the findings of our model. In addition, we will continue exploring the application of deep learning in predicting AF recurrence.
Conclusion
Due to the high recurrence rate of RFA in AF patients, accurate prediction of the recurrence risk after RFA has important clinical implications. In our study, we selected 6 variables and compared 4 machine learning methods to predict the recurrence of AF 12 months after RFA, and XGBoost had the greatest performance (AUC = 0.87, AP = 0.56, accuracy = 86.1%, specificity = 89.7%, precision = 62.5%, F1 score = 0.67) in the testing set. To obtain the weight of the importance of variables in the XGBoost model, we used the variable importance indicator. The results showed that LAA functional parameters, including LAAEF and LAAGPLS, have important clinical value in predicting AF recurrence after RFA.
Data availability
Data supporting the findings of this study can be obtained from the corresponding authors upon reasonable request.
References
Taborsky M, Dusek L, Kautzner J, Vicha M, Aiglova R, Gloger V, Fedorco M, Duba J, Dusek L, Jarkovsky J, et al. SETAP: epidemiology and prevention of Stroke and transient ischaemic Attack in Czech patients with atrial fibrillation. Europace. 2021;23(4):539–47.
Bai Y, Wang YL, Shantsila A, Lip GYH. The global burden of Atrial Fibrillation and Stroke: a systematic review of the clinical epidemiology of Atrial Fibrillation in Asia. Chest. 2017;152(4):810–20.
Carlisle MA, Fudim M, DeVore AD, Piccini JP. Heart Failure and Atrial Fibrillation, like Fire and fury. JACC Heart Fail. 2019;7(6):447–56.
Passman R. Mobile health technologies in the diagnosis and management of atrial fibrillation. Curr Opin Cardiol. 2022;37(1):1–9.
Santala OE, Lipponen JA, Jantti H, Rissanen TT, Halonen J, Kolk I, Pohjantahti-Maaroos H, Tarvainen MP, Valiaho ES, Hartikainen J, et al. Necklace-embedded electrocardiogram for the detection and diagnosis of atrial fibrillation. Clin Cardiol. 2021;44(5):620–6.
Ceornodolea AD, Bal R, Severens JL. Epidemiology and management of Atrial Fibrillation and Stroke: review of data from four European countries. Stroke Res Treat 2017, 2017:8593207.
Lozano Granero C, Franco E, Matia Frances R, Hernandez-Madrid A, Sanchez-Perez I, Zamorano Gomez JL, Moreno J. Impact of power and contact force on index-guided radiofrequency lesions in an ex vivo porcine heart model. J Interv Card Electrophysiol. 2022;63(3):687–97.
Wang Q, Zhuo C, Shang Y, Zhao J, Chen N, Lv N, Huang Y, Zheng L, Lai J, Han J, et al. U-Shaped relationship between Left Atrium size on Echocardiography and 1-Year recurrence of Atrial Fibrillation after Radiofrequency catheter ablation- prognostic value study. Circ J. 2019;83(7):1463–71.
Xu M, Liu F, Ge ZX, Li JM, Xie X, Yang JH. Functional studies of left atrium and BNP in patients with paroxysmal atrial fibrillation and the prediction of recurrence after CPVA. Eur Rev Med Pharmacol Sci. 2020;24(9):4997–5007.
Shoemaker MB, Husser D, Roselli C, Al Jazairi M, Chrispin J, Kuhne M, Neumann B, Knight S, Sun H, Mohanty S, et al. Genetic susceptibility for Atrial Fibrillation in patients undergoing Atrial Fibrillation ablation. Circ Arrhythm Electrophysiol. 2020;13(3):e007676.
Ouyang F, Antz M, Ernst S, Hachiya H, Mavrakis H, Deger FT, Schaumann A, Chun J, Falk P, Hennig D, et al. Recovered pulmonary vein conduction as a dominant factor for recurrent atrial tachyarrhythmias after complete circular isolation of the pulmonary veins: lessons from double Lasso technique. Circulation. 2005;111(2):127–35.
Liu FZ, Zaman JAB, Ehdaie A, Xue YM, Cingolani E, Bresee C, Chugh SS, Wu SL, Shehata M, Wang X. Atrial fibrillation mechanisms before and after pulmonary vein isolation characterized by noncontact charge density mapping. Heart Rhythm 2022.
Kumagai K, Sato T, Kurose Y, Sumiyoshi T, Hasegawa K, Sekiguchi Y, Yambe M, Komaru T. Predictors of recurrence of atrial tachyarrhythmias after pulmonary vein isolation by functional and structural mapping of nonparoxysmal atrial fibrillation. J Arrhythm. 2022;38(1):86–96.
Donnellan E, Hussain M, Jaber W, Patel DR, Kanj M, Wazni O, Hanna M, Collier P. Atrial uptake of Technetium-99m-Pyrophosphate labeled bone-seeking Tracers is Associated with Post ablation Atrial Fibrillation recurrence. JACC Clin Electrophysiol. 2022;8(2):251–3.
Njoku A, Kannabhiran M, Arora R, Reddy P, Gopinathannair R, Lakkireddy D, Dominic P. Left atrial volume predicts atrial fibrillation recurrence after radiofrequency ablation: a meta-analysis. Europace. 2018;20(1):33–42.
Kranert M, Shchetynska-Marinova T, Liebe V, Doesch C, Papavassiliu T, Akin I, Borggrefe M, Hohneck A. Recurrence of Atrial Fibrillation in Dependence of Left Atrial volume index. In Vivo. 2020;34(2):889–96.
Li Y, Han B, Li J, Ge F, Yang L. Value of echocardiography in evaluating efficacy of radiofrequency catheter ablation in patients with atrial fibrillation. Am J Transl Res. 2022;14(3):1778–87.
Gong S, Zhou J, Li B, Kang S, Ma X, Cai Y, Guo Y, Hu R, Zhang X. The Association of Left Atrial Appendage Morphology to Atrial Fibrillation Recurrence after Radiofrequency ablation. Front Cardiovasc Med. 2021;8:677885.
Kaya EB, Tokgozoglu L, Aytemir K, Kocabas U, Tulumen E, Deveci OS, Kose S, Kabakci G, Nazli N, Ozkutlu H, et al. Atrial myocardial deformation properties are temporarily reduced after cardioversion for atrial fibrillation and correlate well with left atrial appendage function. Eur J Echocardiogr. 2008;9(4):472–7.
Tian X, Zhang XJ, Yuan YF, Li CY, Zhou LX, Gao BL. Morphological and functional parameters of left atrial appendage play a greater role in atrial fibrillation relapse after radiofrequency ablation. Sci Rep. 2020;10(1):8072.
Anagnostopoulos I, Kousta M, Kossyvakis C, Lakka E, Paraskevaidis NT, Schizas N, Deftereos S, Giannopoulos G. The role of left atrial peak systolic strain in atrial fibrillation recurrence after catheter ablation. A systematic review and meta-analysis. Acta Cardiol 2021:1–9.
Feeny AK, Chung MK, Madabhushi A, Attia ZI, Cikes M, Firouznia M, Friedman PA, Kalscheur MM, Kapa S, Narayan SM, et al. Artificial Intelligence and Machine Learning in Arrhythmias and Cardiac Electrophysiology. Circ Arrhythm Electrophysiol. 2020;13(8):e007952.
Han L, Askari M, Altman RB, Schmitt SK, Fan J, Bentley JP, Narayan SM, Turakhia MP. Atrial Fibrillation Burden Signature and Near-Term Prediction of Stroke: a machine learning analysis. Circ Cardiovasc Qual Outcomes. 2019;12(10):e005595.
Kim MN, Lee JJ, Kim SA, Kim YH, Choi JI, Park SM, Park SW, Kim YH, Shim WJ. The difference of predictors for recurrence after catheter ablation of non-paroxysmal atrial fibrillation according to follow-up period. Int Heart J. 2014;55(4):312–8.
He Y, Zhang B, Zhu F, Hu Z, Zhong J, Zhu W. Transesophageal echocardiography measures left atrial appendage volume and function and predicts recurrence of paroxysmal atrial fibrillation after radiofrequency catheter ablation. Echocardiography. 2018;35(7):985–90.
Wen S, Liu N, Bai R, Tang RB, Yu RH, Long DY, Sang CH, Jiang CX, Li SN, Wu JH, et al. Right atrial diameter and outcome of catheter ablation of atrial fibrillation. J Interv Card Electrophysiol. 2017;49(2):157–64.
Takayama K, Hachiya H, Iesaka Y, Hirao K, Isobe M. Early recurrence after Longstanding Persistent Atrial Fibrillation ablation. Int Heart J. 2018;59(2):321–7.
Ishii Y, Sakamoto SI, Miyagi Y, Kawase Y, Otsuka T, Nitta T. Risk factors of recurrence of Atrial Fibrillation (AF) after AF Surgery in patients with AF and Mitral Valve Disease. Semin Thorac Cardiovasc Surg. 2018;30(3):271–8.
Oeing CU, Tschope C, Pieske B. [The new ESC guidelines for acute and chronic Heart Failure 2016]. Herz. 2016;41(8):655–63.
Demarchi A, Neumann L, Rordorf R, Conte G, Sanzo A, Ozkartal T, Savastano S, Regoli F, Vicentini A, Caputo ML, et al. Long-term outcome of catheter ablation for atrial fibrillation in patients with severe left atrial enlargement and reduced left ventricular ejection fraction. Europace. 2021;23(11):1751–6.
Jin X, Pan J, Wu H, Xu D. Are left ventricular ejection fraction and left atrial diameter related to atrial fibrillation recurrence after catheter ablation? A meta-analysis. Med (Baltim). 2018;97(20):e10822.
Bajraktari G, Pugliese NR, D’Agostino A, Rosa GM, Ibrahimi P, Percuku L, Miccoli M, Galeotti GG, Fabiani I, Pedrinelli R, et al. Echo- and B-Type natriuretic peptide-guided Follow-Up versus Symptom-guided Follow-Up: comparison of the Outcome in Ambulatory Heart Failure patients. Cardiol Res Pract. 2018;2018:3139861.
Grecu M, Blomstrom-Lundqvist C, Kautzner J, Laroche C, Van Gelder IC, Jordaens L, Tavazzi L, Cihak R, Rubio Campal JM, Kalarus Z, et al. In-hospital and 12-month follow-up outcome from the ESC-EORP EHRA atrial fibrillation ablation long-term registry: sex differences. Europace. 2020;22(1):66–73.
Cheung JW, Cheng EP, Wu X, Yeo I, Christos PJ, Kamel H, Markowitz SM, Liu CF, Thomas G, Ip JE, et al. Sex-based differences in outcomes, 30-day readmissions, and costs following catheter ablation of atrial fibrillation: the United States Nationwide Readmissions Database 2010-14. Eur Heart J. 2019;40(36):3035–43.
Li J, Sang C, Du X, He L, Lu S, Jiang C, Xia S, Chang S, Zuo S, Guo X, et al. Effectiveness and safety of atrial fibrillation ablation in females. Pacing Clin Electrophysiol. 2020;43(6):583–92.
Chao TF, Suenari K, Chang SL, Lin YJ, Lo LW, Hu YF, Tuan TC, Tai CT, Tsao HM, Li CH, et al. Atrial substrate properties and outcome of catheter ablation in patients with paroxysmal atrial fibrillation associated with Diabetes Mellitus or impaired fasting glucose. Am J Cardiol. 2010;106(11):1615–20.
Creta A, Providencia R, Adragao P, de Asmundis C, Chun J, Chierchia G, Defaye P, Schmidt B, Anselme F, Finlay M, et al. Impact of Type-2 Diabetes Mellitus on the outcomes of catheter ablation of Atrial Fibrillation (European Observational Multicentre Study). Am J Cardiol. 2020;125(6):901–6.
Syed FF, Noheria A, DeSimone CV, Asirvatham SJ. Left atrial appendage Ligation and Exclusion Technology in the incubator. J Atr Fibrillation. 2015;8(2):1160.
Kappagoda CT, Linden RJ, Snow HM. The effect of distending the atrial appendages on urine flow in the dog. J Physiol. 1972;227(1):233–42.
Hocini M, Shah AJ, Nault I, Sanders P, Wright M, Narayan SM, Takahashi Y, Jais P, Matsuo S, Knecht S, et al. Localized reentry within the left atrial appendage: arrhythmogenic role in patients undergoing ablation of persistent atrial fibrillation. Heart Rhythm. 2011;8(12):1853–61.
Di Biase L, Burkhardt JD, Mohanty P, Sanchez J, Mohanty S, Horton R, Gallinghouse GJ, Bailey SM, Zagrodzky JD, Santangeli P, et al. Left atrial appendage: an underrecognized trigger site of atrial fibrillation. Circulation. 2010;122(2):109–18.
Simon J, El Mahdiui M, Smit JM, Szaraz L, van Rosendael AR, Herczeg S, Zsarnoczay E, Nagy AI, Kolossvary M, Szilveszter B, et al. Left atrial appendage size is a marker of atrial fibrillation recurrence after radiofrequency catheter ablation in patients with persistent atrial fibrillation. Clin Cardiol. 2022;45(3):273–81.
Kim YG, Choi JI, Boo KY, Kim DY, Oh SK, Park HS, Lee KN, Shim J, Kim JS, Park SW, et al. Clinical and echocardiographic risk factors predict late recurrence after Radiofrequency catheter ablation of Atrial Fibrillation. Sci Rep. 2019;9(1):6890.
Zeljkovic I, Bulj N, Kordic K, Pavlovic N, Radeljic V, Benko I, Zadro Kordic I, Dula K, Kos N, Delic Brkljacic D, et al. Atrial appendages’ mechanics assessed by 3D transoesophageal echocardiography as predictors of atrial fibrillation recurrence after pulmonary vein isolation. Int J Cardiol Heart Vasc. 2020;31:100642.
Wang H, Wu W, Han C, Zheng J, Cai X, Chang S, Shi J, Xu N, Ai Z. Prediction model of osteonecrosis of the femoral Head after femoral Neck fracture: machine learning-based development and validation study. JMIR Med Inform. 2021;9(11):e30079.
Pan P, Li Y, Xiao Y, Han B, Su L, Su M, Li Y, Zhang S, Jiang D, Chen X, et al. Prognostic Assessment of COVID-19 in the Intensive Care Unit by Machine Learning methods: Model Development and Validation. J Med Internet Res. 2020;22(11):e23128.
Labarbera MA, Atta-Fosu T, Feeny AK, Firouznia M, McHale M, Cantlay C, Roach T, Axtell A, Schoenhagen P, Barnard J, et al. New Radiomic markers of pulmonary vein morphology Associated with Post-ablation recurrence of Atrial Fibrillation. IEEE J Transl Eng Health Med. 2022;10:1800209.
Acknowledgements
We want to thank Fei Gu, School of Computer Science, Soochow University, for his valuable comments and advice throughout the process of this study.
Funding
None.
Author information
Authors and Affiliations
Contributions
ShiKun Sun and Li Wang wrote the main manuscript text and prepared Figs. 3, 4, 5 and 6; Tables 1, 2, 3, 4 and 5 and Supplementary Table 1. Jia Lin,Youfen Sun and Changsheng Ma prepared Figs. 1 and 2 and reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The Ethics Committee of The First Affiliated Hospital of Soochow University reviewed and approved all studies involving human participants (No.: 184/2022). The ethics committee of The First Affiliated Hospital of Soochow University waived the requirement for written informed consent from participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Conflict of interest
There were no conflicts of interest reported by the authors.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Sun, S., Wang, L., Lin, J. et al. An effective prediction model based on XGBoost for the 12-month recurrence of AF patients after RFA. BMC Cardiovasc Disord 23, 561 (2023). https://doi.org/10.1186/s12872-023-03599-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-023-03599-9