Abstract
Background
Our study aimed to investigate the association between type D personality and adverse cardiac events in chinese patients after acute myocardial infarction (AMI).
Methods
Patients with AMI admitted to cardiac care unit (CCU) of China-Japan Friendship Hospital, Beijing, China between January 2016 and December 2017 were enrolled. 257 patients completed psychological questionnaires at enrollment. Type D personality was assessed with 14-item Type D Scale-14 (DS14). Anxiety and depression were quantified using Hospital Anxiety and Depression Scale (HADS). Multivariable logistic regression analysis was used to determine the independent predictors of in-hospital major adverse cardiac events (MACEs), while cox regression analysis was used to evaluate post-discharge endpoints.
Results
54 patients (21%) were classified as Type D personality defined by the combination of a negative affectivity (NA) score ≥ 10 and a social inhibition (SI) score ≥ 10 on the DS14. Patients with Type D personality displayed significantly higher scores of anxiety (7.4 ± 3.1 vs. 4.2 ± 3.1, p < .001) and depression (7.2 ± 3.8 vs. 4.0 ± 3.4, p < .001). AMI patients with Type D personality had higher prevalence rates of anxiety (χ2 = 30.095, P < .001) and depression (χ2 = 27.082, P < .001). Type D group also displayed a significantly higher level of blood lipoprotein(a) (177.2 ± 200.7 vs. 118.1 ± 255.7 mg/L, P = .048). The incidence of in-hospital MACEs was higher in type D than in non-Type D patients (24.1% vs. 11.3%, χ2 = 5.751, P = .026). Multivariable logistic regression showed three significant independent predictors of in-hospital MACEs: age [odds ratio(OR) = 1.055; 95%CI 1.016–1.095, p = .004], type-D personality(OR 3.332; 95% CI 1.149–9.661, p = .014) and killip classification(OR 2.275, 95% CI 1.506–3.437, p < .001). The average follow-up time was 31 (23-37.5) months. Type D patients had higher incidences of post-discharge events(23.1% vs. 11.5%, p = .032). In the analysis of post-discharge events by Cox regression, χ2 of the Cox regression equation was 16.795 (P = .032). Smoking (HR 2.602; 95% CI1.266–5.347, p = .009) and type-D personality (HR 2.265; 95%CI 1.028–4.988, p = .042) were independent predictors of long-term cardiac events. Kaplan–Meier curves showed significant difference in event-free survival between type D and non-type D group (p = .043).
Conclusions
Type D personality is an independent predictor of in-hospital and post-discharge cardiac events after AMI in Chinese patients.
Similar content being viewed by others
Background
Despite great advances in the diagnosis and therapy of coronary heart disease (CHD), patients still suffer from adverse cardiac events. Psychosocial risk factors are equally important in risk prediction for CHD compared with sex, metabolic and behavioural risk factors [1]. Type D (“distressed”) personality is characterized by negative affectivity (NA) and social inhibition (SI). NA refers to the tendency of experiencing negative thoughts, feelings and emotions, while SI people tend to feel inhibited and insecure with difficulty in expressing these emotions in social situations [2]. Type D personality is associated with more severe coronary artery calcification [3], impaired endothelial function [4], hyperlipidemia [5], unhealthy lifestyles [6] and greater risk for cardiac events in CHD [7]. A recent individual patient-data meta-analysis combined the data of 19 previously published prospective cohort studies and proved that Type D personality is related to adverse events in CHD [8]. Acute myocardial infarcrtion (AMI) is the most severe type of CHD and the incidence of it is still increasing. In the US, during the period from 2001 to 2011, in-hospital mortality after AMI did not change for patients who received percutanous coronary intervention (PCI) [9]. The characteristics of type D personality have been found to have a statistically significant association with AMI [10]. However, the predictive value of type D personality remains controversial and inconclusive. Large heterogeneity exists between type D studies and negative findings have been reported [11]. Results varied depending on the selected population, age, ethnicity, choice of endpoints and methods to assess type D personality [12]. Data about the impact of type D personality on AMI in chinese patients is also limited.The aim of our study was to evaluate the predictive value of type D personality for cardiac events in chinese patients with AMI.
Methods
Study design and paticipants
Patients with AMI admitted to cardiac care unit (CCU) of China-Japan Friendship Hospital, Beijing, China between January 2016 and December 2017 were enrolled. A majority of the patients experienced both an AMI and subsequently underwent revascularization. Patients with cancer or other life-threatening medical conditions were excluded. At baseline, 257 patients provided written informed consent and completed psychological questionnaires at enrollment by theirselves or with the nurses’ help. This study was approved by the Ethics Committee of China-Japan Friendship Hospital in Peking of China and performed in accordance with the principles of the Declaration of Helsinki revised in 2013. The original data will be shared on reasonable request by contacting the corresponding author.
Type D personality assessment
Type D Personality was assessed at baseline with the Chinese version of 14-item Type D Scale-14 (DS14), which contains 7-item NA and SI subscales [2, 13]. Items are rated on a 5-point scale ranging from 0 = false to 4 = true. A cut-off ≥ 10 on the NA and SI measures identifies individuals with elevated trait levels, and individuals with a score ≥ 10 on both scales are categorized as type D. The DS-14 is a valid measure of NA and SI in Chinese population [13]. In our study, NA and SI subscales are internally consistent with the Cronbach’s alpha 0.82 and 0.80 respectively.
Hospital anxiety and depression measures
Assessment of psychological status was quantified using Hospital Anxiety and Depression Scale (HADS), which is composed of 14 items and contains two subscales: anxiety (HADS-A) and depression (HADS-D) [13, 14]. Each item is from 0 (no symptoms) to 3 (maximum symptom level). The maximum score for each subscale is 21 and scores 0–7 on each subscale are considered normal. A cutoff score ≥ 8 was used for both subscales to identify patients with likely anxiety and depression. HADS-A and HADS-D are internally consistent with the Cronbach’s alpha 0.78 and 0.79 respectively.
In-hospital cardiac events and post-discharge endpoints
Most literatures recognized that ventricular tachycardia / fibrillation, acute recurrent myocardial ischemia, reinfarction, cardiogenic shock, acute pulmonary edema and cardiac death are the main in-hospital complications of AMI [15]. So in-hospital events were major adverse cardiac events (MACEs; a composite of ventricular tachycardia/fibrillation, acute recurrent myocardial ischemia, reinfarction, cardiogenic shock, acute pulmonary edema and cardiac death). The follow-up interval was fixed at 2-3years. Patients and their families were contacted by telephone to determine the endpoints. Information on mortality, nonfatal myocardial infarction (MI), PCI and CABG were extracted from hospital records and the patient’s attending physician was involved to determine the cause of death. The post-discharge endpoints were defined as a composite of unstable angina, reinfarction, cardiac revascularization (PCI/CABG) and cardiac death [16].
Statistical analysis
All statistical analyses were performed using SPSS version 22.0 software (SPSS Inc., Chicago, IL, USA). Numerical variables were expressed as mean ± standard deviation when normally distributed and Student’s t test was used for comparison between two groups. When not normally distributed, data were expressed as median ± interquartile range (IQR) and Mann-Whitney U test was used. Frequencies and percentages were used to express categorical variables, which were analyzed by Chi square test. Taking the in-hospital MACEs as the outcome variable, and multivariable logistic regression analysis was used to calculate odds ratio (OR) and determine the independent predictors of in-hospital MACEs. We included all baseline variables and made a stepwise selection. The model included variables (age, left ventricular ejection fraction, killip class, type-D persionality, HADS-A, HADS-D, No. of diseased vessels, fasting blood glucose, low-density lipoprotein cholesterol). HADS was modeled to determine the independent predictors of in-hospital MACEs, which was not used to evaluate post-discharge endpoints because anxiety and depression states are dynamically changing and it is believed that the in-hospital score can not have a significant impact on the long-term prognosis. We used separate scores for anxiety and depression. Each subscale was a separate continuous variable. The Hosmer Limeshow Goodness of fit test was selected, and the chi-square test of regression equation model fitting showed that the P-value was less than 0.05, indicating a good fitting of the regression model. Cox regression analysis was used to evaluate post-discharge endpoints. P < .05 was considered significant.
Results
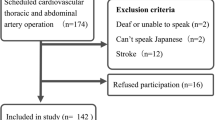
Baseline characteristics
Flow chart of patient screening was shown in Fig. 1. Table 1 presented the characteristics of the 257 patients included in this study. The mean age was 64.3 ± 13.7years, 75% were men, and a majority of patients underwent PCI or CABG. 54 patients (21.0%) were classified as type D personality defined by the combination of a NA score ≥ 10 and a SI score ≥ 10 on the DS14, all other patients were classified as non-type D with 30 (11.7%) NA only, 45 (17.5%) SI only, and 83 (32.3%) having low scores on both traits. Type D personality was not significantly related to age, sex, Body Mass Index (BMI), PCI, hypertension, diabetes and smoking. Patients with type D personality displayed significantly higher scores of anxiety and depressive symptoms than non-type D patients did (Table 1). The prevalence rates of anxiety and depression in type D and non-type D patients are shown in Fig. 2. Chinese AMI patients with a type D personality were at increased risk of anxiety (χ2 = 30.095, P < .001) and depression (χ2 = 27.082, P < .001). Patients with type D personality also displayed significantly higher level of lipoprotein(a) (Lp[a]) (P = .048).
BNP/NT-proBNP level
Normal (BNP < 100 pg/ml or NT-proBNP < 400 ng/ml); Mild(100–299 pg/ml or 400–1500 ng/ml); Moderate (300–500 pg/ml or 1500–3000 ng/ml); Severe(> 500 pg/ml />3000 ng/ml).
In-hospital events
There was no difference in length of stay during hospitalization between type D and non-type D patients (10 ± 7days vs. 10.0 ± 7days, p = .759). The incidence of in-hospital cardiac events was higher in type D than in non-type D patients (24.1% vs. 11.3%, χ2 = 5.751, P = .026). See Table 2 for details of in-hospital MACEs. The results of the logistic regression were presented in Table 3. Multivariable logistic regression showed three significant independent predictors of in-hospital MACEs: age (OR = 1.055; 95%CI1.016-1.095, p = .004), type-D personality (OR 3.332; 95% CI 1.149–9.661, p = .014) and killip class(OR 2.275, 95% CI 1.506–3.437, p < .001).
We also established three other models: including only HADS-A, including only HADS-D, and excluding HADS respectively. Indicators with predictive value for events during hospitalization include age, killip class at admission, and type-D personality. The OR values of type-D personality were 3.018 (95% CI 1.016–8.230, p = .031), 3.506 (95% CI 1.269–9.686, p = .016)and 3.052 (95% CI 1.249–7.458, p = .014), which hinted that adding HADS having no significant impact on type-D personality.
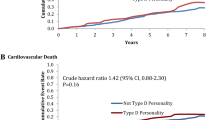
Post-discharge endpoints
The average follow-up time was 31 (23-37.5) months. 4 patients were lost to follow-up with 3 patients in non-type D and 1 in type D group. Three patients died all in non-type D group. One died of severe pneumonia and heart failure. The other two died of Non-ST elevation MI and cardiogenic shock. There were 35 cardiac events in total patients, of which 12 events in type D group and 23 in non-type D group. See details in Table 4, type D patients had higher incidences of cardiac events (23.1% vs. 11.5%, p = .032). The results of the Cox regression were presented in Table 5. χ2 of the Cox regression equation was 16.795 (p = .032). Smoking (HR 2.602; 95% CI1.266–5.347, p = .009) and type-D personality (HR 2.265; 95%CI 1.028–4.988, p = .042) were independent predictors of long-term cardiac events. Kaplan–Meier curves of freedom from the post-discharge events in type D and non-type D group were shown in Fig. 3 (p = .043).
Sensitivity analysis
The logistic regression analysis for in-hospital events was also performed by multiplying NA and SI to represent type-D personality. Predictive indicators that were statistically significant for events during hospitalization included age and killip class at admission. The product of NA and SI representing type-D personality also showed a trend towards predicting prognosis, but it did not reached statistical significance. The OR value of the product of NA and SI was 1.005 (95% CI 1.000-1.010, p = .059) and the Wald value was 3.574 when the regression model including HADS-A and HADS-D. While excluding the HADS, the OR value of the product of NA and SI was 1.004 (95% CI 1.000-1.008, p = .051), and the Wald value was 3.793. The results showed consistence with those using type-D dichotomous variables, but the predictive value using product of NA and SI may be lower (See supplemental Table 1). Attempts were also made to use the sum score of NA and SI representing type D personality, NA or SI as separate continuous variables respectively, but they were not found to be independent risk factors for in-hospital events and post-discharge endpoints .
Discussion
Our study aimed to investigate the association between type D personality and adverse cardiac events in chinese patients after AMI. Over 60% of our selected AMI population were ST-segment elevation myocardial infarction (STEMI) and over 80% of the STEMI patients received primary PCI. Type D personality had a prevalence of 21% in our AMI patients, which is similar to those reported previously [17, 18]. There was a higher prevalence of both anxiety and depression in our type D patients, which supports the viewpoint that type D personality increases the psychological risk factors in AMI patients. The average score of anxiety and depression exceeded seven in our type D group and a cut-off value of seven or higher can combine sensitivity and specificity best when screening for major anxiety and depression [19]. Psychological factors have been implicated in the onset and progression of cardiovascular disease. Anxiety and depression are the most common psychological manifestations after AMI, which are associated with short- and long-term cardiac events after AMI already found by previous studies [14, 15]. Our results showed that the incidence of in-hospital MACEs after AMI in type D is more than twice of that in non-type D group. In addition to age and killip class, type-D personality is the independent predictor for in-hospital MACEs after AMI by multivariable logistic regression analysis. Type D patients also had higher incidences of post-discharge cardiac events by Cox regression analysis. Type-D personality together with smoking are the independent predictors of post-dicharge events in AMI patients, which indirectly confirmed the previous study that type D smokers had a higher incidence of cardiovascular events during the long-term follow-up of AMI [6].
Events definition and endpoints selection are very important in evaluating the prognostic effect of a risk factor in clinical trials. Previous study discussed the heterogeneity in the predictive value of type D personality for cardiac events and mortality [11]. Some type D studies focused on non-cardiac events and reported negative findings, while positive studies selected cardiac endpoints [11]. Type D personality may be more related to cardiac events. So in our study, we selected unstable angina, reinfarction, cardiac revascularization (PCI/CABG) and cardiac death as post-discharge endpoints for cardiac prognosis.
A systematic review compared two popular methods to assess a Type D personality effect using continuous and dichotomous methods, which concluded the dichotomous method may be false positives, with only NA or SI driving the outcome [12]. In our study, the logistic regression analysis for in-hospital events was also performed by multiplying NA and SI to represent type-D personality. Predictive indicators that were statistically significant for events during hospitalization included age and killip class at admission. The product of NA and SI representing type-D personality also showed a trend towards predicting prognosis, but it did not reached statistical significance. The OR value of the product of NA and SI was 1.005 (95% CI 1.000-1.010, p = .059) and the Wald value was 3.574 when the regression model including HADS-A and HADS-D. While excluding the HADS, the OR value of the product of NA and SI was 1.004 (95% CI 1.000-1.008, p = .051), and the Wald value was 3.793. The results showed consistence with those using type-D dichotomous variables, but the predictive value using product of NA and SI may be lower due to the small number of our subjects. And also some critically ill patients who could not cooperate with the DS14 questionnaire and might have a high probability of cardiovascular events were not included in our study. Attempts were also made to use the sum score of NA and SI representing type D personality, NA or SI as separate continuous variables respectively, but they were not found to be independent risk factors for in-hospital events and post-discharge endpoints .
Reza et al. have reported that type D personality is associated with hyperlipidemia in patients with myocardial infarction [5]. In our results, type D personality displayed significantly higher level of blood lipoprotein(a)[Lp(a)], while no difference was shown in low-density lipoprotein cholesterol (LDL-C) level. Lp(a) is an independent risk factor for CHD [20, 21] and more strongly associated with cardiovascular mortality than LDL-C [22].
Conclusions
In summary, type D personality is an independent predictor of in-hospital and post-discharge cardiac events after AMI in Chinese patients. Adding psychotherapy on optimal cardiological care after AMI may bring benefits on the prognosis of AMI.
Data availability
The original data will be shared on reasonable request by contacting the corresponding author.
Abbreviations
- AMI:
-
acute myocardial infarction
- CCU:
-
cardiac care unit
- DS14:
-
14-item Type D Scale-14
- HADS:
-
Hospital Anxiety and Depression Scale
- MACEs:
-
major adverse cardiac events
- NA:
-
negative affectivity
- SI:
-
social inhibition
- OR:
-
odds ratio
- CHD:
-
coronary heart disease
- PCI:
-
percutanous coronary intervention
- HADS-A:
-
Hospital Anxiety and Depression Scale-Anxiety
- HADS-D:
-
Hospital Anxiety and Depression Scale- Depression
- MI:
-
myocardial infarction
- CABG:
-
coronary artery bypass grafting
- IQR:
-
interquartile range
- BMI:
-
Body Mass Index
- ACS:
-
acute coronary syndrome
- STEMI:
-
ST-segment elevation myocardial infarction
- IABP:
-
intra-aortic balloon pump
- Hb:
-
haemoglobin
- Cr:
-
creatine
- BNP:
-
B-Type Natriuretic Peptide
- NT-proBNP:
-
N-terminal proBNP
- TnI:
-
Troponin I
- LDL-C:
-
low-density lipoprotein cholesterol
- Lp(a):
-
lipoprotein(a)
- HbA1c:
-
hemoglobin A1c
- HCY:
-
homocysteine
References
Walli-Attaei M, Rosengren A, Rangarajan S, Breet Y, Abdul-Razak S, Sharief WA, et al. Metabolic, behavioural, and psychosocial risk factors and Cardiovascular Disease in women compared with men in 21 high-income, middle-income, and low-income countries: an analysis of the PURE study. Lancet. 2022;400(10355):811–21. https://doi.org/10.1016/S0140-6736(22)01441-6.
Denollet J. DS14: standard assessment of negative affectivity, social inhibition, and type D personality. Psychosom Med. 2005;67:89–97. https://doi.org/10.1097/01.psy.0000149256.81953.49.
Raykh OI, Sumin AN, Kokov АN, Indukaeva EV, Artamonova GV. Association of type D personality and level of coronary artery calcification. J Psychosom Res. 2020;139:110265. https://doi.org/10.1016/j.jpsychores.2020.110265.
Denollet J, Felius RA, Lodder P, Mommersteeg PM, Goovaerts I, Possemiers N, et al. Predictive value of type D personality for impaired endothelial function in patients with coronary artery Disease. Int J Cardiol. 2018;259:205–10. https://doi.org/10.1016/j.ijcard.2018.02.064.
Bagherian-Sararoudi R, Sanei H, Attari A, Afshar H. Type D personality is associated with hyperlipidemia in patients with Myocardial Infarction. J Res Med Sci. 2012;17:543–7.
Imbalzano E, Vatrano M, Quartuccio S, Ceravolo R, Ciconte VA, Rotella P, et al. Effect of type D personality on Smoking status and their combined impact on outcome after acute Myocardial Infarction. Clin Cardiol. 2018;41:321–5. https://doi.org/10.1002/clc.22865.
Raykh OI, Sumin AN, Korok EV. The influence of personality type D on Cardiovascular prognosis in patients after coronary artery bypass grafting: data from a 5-Year-follow-up study. Int J Behav Med. 2021;1–11. https://doi.org/10.1007/s12529-021-09992-y.
Lodder P, Wicherts JM, Antens M, Albus C, Bessonov IS, Condén E, et al. Type D personality as a risk factor for adverse outcome in patients with Cardiovascular Disease: an individual patient-data Meta-analysis. Psychosom Med. 2023;85(2):188–202. https://doi.org/10.1097/PSY.0000000000001164.
Benjamin EJ, Virani SS, Callaway CW, Chamberlain AM, Chang AR, Cheng S et al. Heart disease and stroke Statistics-2018 update: a report from the American Heart Association. Circulation 2018;137:e67-e492. https://doi.org/10.1161/CIR.0000000000000573.
Manoj MT, Joseph KA, Vijayaraghavan G, Type D, Personality. Myocardial Infarction: a case-control study. Indian J Psychol Med. 2020;42:555–9. https://doi.org/10.1177/0253717620941157.
Kupper N, Denollet J. Explaining heterogeneity in the predictive value of type D personality for cardiac events and mortality. Int J Cardiol. 2016;224:119–24. https://doi.org/10.1016/j.ijcard.2016.09.006.
Lodder P, Kupper N, Antens M, Wicherts JM. A systematic review comparing two popular methods to assess a type D personality effect. Gen Hosp Psychiatry. 2021;71:62–75. https://doi.org/10.1016/j.genhosppsych.2021.04.002.
Yu DS, Thompson DR, Yu CM, Pedersen SS, Denollet J. Validating the type D personality construct in Chinese patients with coronary Heart Disease. J Psychosom Res. 2010;69:111–8. https://doi.org/10.1016/j.jpsychores.2010.01.014.
Murphy B, Grande ML, Alvarenga M, Worcester M, Jackson A. Anxiety and Depression after a Cardiac Event: prevalence and predictors. Front Psychol. 2020;10:3010. https://doi.org/10.3389/fpsyg.2019.03010.
AbuRuz ME. Patients with ST segment elevation Myocardial Infarction: moderating effect of perceived control on the relationship between depression and in-hospital Complications. BMC Cardiovasc Disord. 2019;19:143. https://doi.org/10.1186/s12872-019-1126-z.
Denollet J, Pedersen SS, Vrints CJ, Conraads VM. Usefulness of type D personality in predicting five-year cardiac events above and beyond concurrent symptoms of stress in patients with coronary Heart Disease. Am J Cardiol. 2006;97:970–3. https://doi.org/10.1016/j.amjcard.2005.10.035.
Zhang Y, Wu S, Pan J, Hoschar S, Wang Z, Tu R et al. The impact of the type D personality pattern on prehospital delay in patients suffering from acute Myocardial Infarction. 2020;12:4680–9. https://doi.org/10.21037/jtd-20-1546.
Menon V, Pillai AG, Satheesh S, Kaliamoorthy C, Sarkar S. Factor structure and validity of type D personality scale among Indian (Tamil-speaking) patients with acute Myocardial Infarction. Indian J Psychiatry. 2019;61:572–7. https://doi.org/10.4103/psychiatry.IndianJPsychiatry_27_19.
Wu Y, Levis B, Sun Y, He C, Krishnan A, Neupane D, et al. Accuracy of the hospital anxiety and Depression Scale Depression subscale (HADS-D) to screen for major depression: systematic review and individual participant data meta-analysis. BMJ. 2021;373:n972. https://doi.org/10.1136/bmj.n972.
Emerging Risk Factors Collaboration, Erqou S, Kaptoge S, Perry PL, Angelantonio ED, Thompson A, et al. Lipoprotein(a) concentration and the risk of coronary Heart Disease, stroke, and nonvascular mortality. JAMA. 2009;302:412–23. https://doi.org/10.1001/jama.2009.1063.
Tsimikas SA. Test in Context: lipoprotein(a): diagnosis, prognosis, controversies, and emerging therapies. J Am Coll Cardiol. 2017;69:692–711. https://doi.org/10.1016/j.jacc.2016.11.042.
Langsted A, Kamstrup PR, Nordestgaard BG. High lipoprotein(a) and high risk of mortality. Eur Heart J. 2019;40:2760–70. https://doi.org/10.1093/eurheartj/ehy902.
Acknowledgements
The authors would like to thank the nurses in CCU and the Cardiology Team of China-Japan Friendship Hospital for their support of this study.
Funding
This research was supported by National key clinical specialty construction program of China (2020-QTL-009).
Author information
Authors and Affiliations
Contributions
Y.X. created the idea and designed the study. Y.X. and L.J. collected and analyzed the data, wrote and submitted the manuscript. L.J. prepared figures tables and figures. W.W. and L.N. helped collect the cases. W.J. and Z.L. helped collect informed consent of the patients. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All patients provided written informed consent by theirselves or with the nurses’ help. This study was approved by the Ethics Committee of China-Japan Friendship Hospital in Peking of China and performed in accordance with the principles of the Declaration of Helsinki revised in 2013.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Li, J., Wu, W., Li, N. et al. Predictive value of type D personality for cardiac events in Chinese patients with acute myocardial infarction. BMC Cardiovasc Disord 23, 556 (2023). https://doi.org/10.1186/s12872-023-03598-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-023-03598-w