Abstract
Background
Primary tumors of the heart are a rare phenomenon. Lymphatic malformations are congenital anomalies of the lymphatic system that tend to grow progressively. Lymphatic malformations are typically found in the cervical and axillary regions and found on pediatric patients. We report a 40-year-old woman with giant epimyocardial lymphatic malformation.
Case presentation
A 40-year-old woman was assessed due to suspected traumatic cardiac tamponade. Computed tomography of the heart and cardiac magnetic resonance imaging were compatible with either a large pericardial hemangioma or angiosarcoma. The tumor infiltrated deeply into the myocardium and could only be partially resected. Histopathological diagnosis was a cardiac lymphatic malformation with micro- and macrocystic components. The patient has remained asymptomatic for fourteen years after the surgery. In the latest follow-up, her left ventricular function had remained normal and the maximum thickness of the residual tumor had regressed.
Conclusions
Even when a complete removal of a cardiac lymphatic malformation is not possible, a debulking procedure can yield a good long-term result.
Similar content being viewed by others
Background
Primary tumors of the heart are a rare phenomenon, and most of them are benign. Secondary tumors of the heart are more common, and in some studies the prevalence has been 20 times greater when compared to primary tumors [1]. Lymphatic malformations are congenital anomalies of the lymphatic system that tend to grow progressively. Lymphatic malformations are typically found in the cervical and axillary regions, although rarer, few cases of cardiac lymphatic malformations have been reported as well [2, 3].
We present a 40-year-old woman with giant epimyocardial lymphatic malformation. This case study makes an important contribution by reporting the results of a long-term post-operative follow-up.
Case presentation
A 40-year-old woman was admitted urgently to the emergency department of Helsinki University Hospital, Finland, with a suspected traumatic cardiac tamponade. She had attended an outdoor concert where the crowd pushed her against a fence causing an injury to the head and the left side of the chest. Apart from being operated for a cavernous hemangioma in her temporal lobe eleven years earlier, her past medical history was unremarkable, and she did not have any regular medication. She denied any cardiac symptoms and declared to have a normal exercise tolerance.
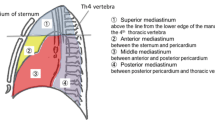
On admission, her chest was sore, and breathing was painful. The chest x-ray revealed a grossly enlarged cardiac silhouette prompting a suspicion of a cardiac tamponade (Fig. 1A). Transthoracic echocardiogram (TTE) revealed a large cystic mass within or adjacent to the pericardial sac that compressed the lateral wall of the normal-sized left ventricle (LV) with a preserved systolic function. A mild mitral valve insufficiency was noted. No pericardial fluid was detected. Contrast-enhanced computed tomography (CT) of the heart and coronaries confirmed an intrapericardial cystic tumor with a 14 cm diameter, which was located mostly in the left and caudal aspects of the heart (Fig. 1B). The arterial blood supply originated from distal branches of both the left circumflex (LCX) and right (RCA) coronary arteries. The venous drainage was to the coronary sinus. No calcifications, fat, or enhancement were found in the tumor.
Imaging findings. A Chest X-ray showed an enlarged cardiac shadow without pneumothorax. B 14 cm diameter cystic pericardial tumor without calcifications, fat or contrast enhancement in CT. Both coronary and CT angiography demonstrated feeding arteries to the tumour from distal branches of LCX and RCA and venous drainage to coronary sinus. C T2-weighted image in CMR. D T1 weighted late enhancement image after contrast in CMR
In cardiac magnetic resonance (CMR) imaging, the pericardial tumor consisted of several septal hemorrhagic lacunae and vessels, which were hyperintense in both T1- and T2-weighted images. Figure 1C demonstrates the T2-weighted images in CMR. According to fat-suppressed images, there was no significant fat consistency in the tumor, and it did not enhance clearly by contrast (Fig. 1D).
To detect any malignant tumors in the chest or abdominal cavities, a whole-body CT was carried out. No malignancies were found thus excluding the possibility of cardiac metastasis. The patient had recent fractures in left costae 10–12 and left transverse processes of L1 and L2 vertebrae corresponding to the history of chest trauma.
Taken together, the imaging studies suggested that the tumor was either a hemangioma or an asymptomatic and slow-growing angiosarcoma. The absence of any calcifications and the lack of intense enhancement after contrast administration typical for hemangiomas, supported the preoperative diagnosis of an angiosarcoma.
A sternotomy with cardiopulmonary bypass and cardiac arrest was performed. The tumor originated with a large base both from the lateral and posterior wall of the LV infiltrating deep into the myocardium and close to the mitral valve annulus without a clear plane of dissection (Fig. 2A). Only partial resection could be performed (172 g of tissue, Fig. 2B).
In histology, the tumor consisted of sponge-like tissue, with cystic spaces of 0.5–10 mm in diameter (Fig. 3A). Connective tissue septa contained paucicellular fibrous tissue, mature adipocytes, and aggregates of small lymphocytes (Fig. 3B). Cystic spaces were lined with non-atypical endothelial cells that were positive both for the pan-endothelial marker CD31 and the lymphatic endothelial marker podoplanin/D2-40 (Fig. 3C-D). No mitotic activity in the endothelium was observable. Cystic spaces contained either proteinaceous lymph, erythrocytes, or hemosiderophages derived from previous episodes of hemorrhage. Histopathological diagnosis was a cardiac lymphatic malformation with micro-and macrocystic components.
The postoperative course was uncomplicated. At discharge, the maximum thickness of the residual tumor was 30 mm in TTE. The patient has been followed-up with decreasing intensity both with CMR and TTE. In the last CMR conducted nine years after the procedure, LV function was normal, and the maximum diameter of the residual tumor had regressed to 13 mm (Fig. 4). Latest follow-up performed by a cardiologist was 13 years after the operation; the patient had remained asymptomatic and used no medication. In TTE, LV size and function were normal, and the residual tumor had remained the same size. By June 2023, the patient had not contacted health care services outside the regular follow-up.
Discussion and conclusions
Primary cardiac and pericardial tumors are very rare and mostly benign [1]. Mesothelial cysts are the most common pericardial primary tumors comprising majority of the cases, followed by teratomas, bronchogenic cysts, benign fibrous tumors, lymphatic malformations, and hyperplastic lymph nodes [1]. Mesotheliomas and sarcomas are the most frequently found types of malignant pericardial diseases [4]. Although rare, angiosarcomas can extend to pericardium or have a pericardial origin, and low-grade angiosarcomas can be difficult to differentiate from hemangiomas. Hemangiomas are rare benign cardiac tumors that may affect both pericardium and myocardium [1]. In our case the imaging studies suggested that the tumor was either a hemangioma or an angiosarcoma. The absence of any calcifications and the lack of intense enhancement after contrast administration typical for hemangiomas, supported the preoperative diagnosis of an angiosarcoma.
In our case histological studies confirmed the diagnosis of lymphatic malformation. Lymphatic malformations are a type of vascular malformation and can be divided to two major subtypes: micro- and macrocystic [5]. Majority of the lymphatic malformations are found in pediatric patients, although lymphatic malformations have been reported in adults as well [3]. Cardiac lymphatic malformations are very rare as lymphatic malformations are typically located in the head, neck, or axillary region [3]. The manifestation of symptoms depends on the location and the size of the tumor. In our case the patient had remained asymptomatic, and the tumor was found incidentally. Similarly, in previous reports some of the patients with cardiac lymphatic malformations had remained asymptomatic [2, 6, 7]. The most common symptoms related to cardiac lymphatic malformation were chest pain, dyspnea, respiratory distress, or palpitations [2, 8,9,10,11]. Surgical removal has been the typical treatment of choice. In some previous reports the tumors have been slightly smaller when compared to our case, and in some cases a complete removal has been possible [9, 11, 12]. In previous studies the results of surgical treatment have been good with no recurrence, but the follow-up time has ranged from only one month to two years [7, 9, 11, 12]. We report a significantly longer follow-up time when compared to most previous studies. Our case demonstrates that if a complete removal is not possible, a debulking procedure can yield a good long-term result. In case of recurrence a repeat debulking procedure could be considered.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- CMR:
-
Cardiac magnetic resonance imaging
- CT:
-
Computed tomography
- LCX:
-
Left circumflex
- LV:
-
Left ventricle
- RCA:
-
Right coronary artery
- TTE:
-
Transthoracic echocardiogram
References
Basso C, Rizzo S, Valente M, Thiene G. Prevalence and pathology of primary cardiac tumors. Cardiovasc Med. 2012;15(1):18–29.
Pichler Sekulic S, Sekulic M. Primary cardiac and pericardial lymphangiomas: clinical, radiologic, and pathologic characterization derived from an institutional series and review of the literature. Virchows Arch. 2022;480(6):1211–21.
Eliasson JJ, Weiss I, Høgevold HE, Oliver N, Andersen R, Try K, et al. An 8-year population description from a national treatment centre on lymphatic malformations. J Plast Surg Hand Surg. 2017;51(4):280–5.
Basso C, Valente M, Poletti A, Casarotto D, Thiene G. Surgical pathology of primary cardiac and pericardial tumors. Eur J Cardiothorac Surg. 1997;12:730–8. Available from: https://academic.oup.com/ejcts/article/12/5/730/347095.
ISSVA Classification of Vascular Anomalies ©2018 International Society for the Study of Vascular Anomalies. Available at https://www.issva.org/classification.
Kadota Y, Utsumi T, Kawamura T, Inoue M, Sawabata N, Minami M, et al. Lymphatic and venous malformation or “lymphangiohemangioma” of the anterior mediastinum: case report and literature review. Gen Thorac Cardiovasc Surg. 2011;59:575–8.
Junqueira N, Ferreira R, Gonçalves J, Nobre Â. Lymphangioma of the heart as a rare tumor: a case report. Int J Surg Case Rep. 2018;53:246–9.
Wen Y, Ren S, Yan Q, Ma G. Surgical Resection of Primary Cardiac Cavernous Hemangioma: A Case Report. Heart Surg Forum. 2022;25(5):E753–5.
Diao WJ, Shi C, Liu G, Liu XG, Li HH, Meng JJ, et al. The diagnosis and treatment of cardiac lymphangioma a case report and literature review. Medicine (United States). 2019;98:e14000. Lippincott Williams and Wilkins.
Robillard J, Pena E, Veinot JP, Fulop J, Dennie C. Pericardial lymphangiohemangioma multimodality imaging features and pathologic correlation. Circulation. 2014;129:e657-9. Lippincott Williams and Wilkins.
Heffron SP, Alviar CL, Towe C, Geisler BP, Axel L, Galloway AC, et al. Dyspnea and chest pain in a young woman caused by a Giant Pericardial Lymphohemangioma: diagnosis and treatment. Can J Cardiol. 2016;32(10):1260.e23-1260.e25.
Chiu P, Edmonson A, Brewer ZE, Woo YJ. Resection of a giant cardiac lymphovenous malformation involving the right atrioventricular groove. Ann Thorac Surg. 2017;104(3):e257–9.
Acknowledgements
Not applicable.
Funding
Open Access funding provided by University of Helsinki including Helsinki University Central Hospital. TH and KH received grants from the Finnish Foundation of Cardiovascular Research and Aarne Koskelo Foundation. TH received special governmental subsidy for health sciences research of the University Hospital of Helsinki.
Author information
Authors and Affiliations
Contributions
All authors collected data and prepared figures. KH and TH wrote the main manuscript text. SK conducted radiological analysis. JL conducted histological analysis. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
According to institutional guidelines, ethical approval was not required as the patient gave written informed consent for publication of this case report.
Consent for publication
The patient gave written informed consent for publication.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Heliö, K., Weckström, S., Kivistö, S. et al. Successful palliative resection of giant epimyocardial lymphatic malformation with 14 years of follow-up: a case report. BMC Cardiovasc Disord 23, 414 (2023). https://doi.org/10.1186/s12872-023-03449-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-023-03449-8