Abstract
Background
Recent studies have reported atrial involvement and coexistence of aortic stenosis in transthyretin (ATTR) cardiac amyloidosis (CA). However, pathological reports of extraventricular ATTR amyloid deposits in atrial structures or heart valves are limited, and the clinical implications of ATTR amyloid deposits outside the ventricles are not fully elucidated.
Case presentation
We report 3 cases of extraventricular ATTR amyloid deposits confirmed in surgically resected aortic valves and left atrial structures, all of which were unlikely to have significant ATTR amyloidosis infiltrating the ventricles as determined by multimodality evaluation including 99mtechnetium-pyrophosphate scintigraphy, cardiac magnetic resonance, endomyocardial biopsy and their mid-term clinical course up to 5 years. These findings suggested that these were extraventricular ATTR amyloid deposits localized in the aortic valve and the left atrium.
Conclusions
While long-term observation is required to fully clarify whether these extraventricular ATTR amyloid deposits are truly localized outside the ventricles or are early stages of ATTR-CA infiltrating the ventricles, our 3 cases with multimodality evaluations and mid-term follow up suggest the existence of extraventricular ATTR amyloid deposits localized in the aortic valve and left atrial structures.
Similar content being viewed by others
Background
Recent studies have reported atrial involvement and coexistence of aortic stenosis (AS) in transthyretin (ATTR) cardiac amyloidosis (CA) [1,2,3,4,5,6,7]. However, pathological reports of extraventricular ATTR amyloid deposits in the valves or in the atrial structures are limited, and the clinical implications of ATTR amyloid deposits outside the ventricles are not fully elucidated.
Herein, we report 3 cases of pathologically diagnosed extraventricular ATTR amyloid deposits in surgically resected aortic valves and left atrial structures, which suggested the existence of extraventricular ATTR amyloid deposits localized in the aortic valve and left atrial (LA) structures.
Case presentations
Case 1
A 79-year-old man was admitted for acute decompensated heart failure. He had atrial fibrillation (AF, 117 beats/min) and elevated B-type natriuretic peptide (BNP, 1381.7 pg/ml; reference range < 18.4 pg/ml). Echocardiogram showed left ventricular (LV) ejection fraction (EF) 26%, LV end-diastolic/end-systolic dimension (LVEDD/ESD) 57/48 mm, interventricular septum/posterior wall thickness (IVS/PWT) 12/10 mm, global longitudinal strain (GLS) -4.4%, severe AS (peak velocity 4.8 m/s, mean pressure gradient 47 mmHg, aortic valve area (AVA) 0.37 cm2) and moderate mitral regurgitation (Fig. 1A). Surgical aortic valve replacement (SAVR), mitral valve repair, Cryo-Maze procedure and LA appendectomy were performed.
Images of Case 1. A Transthoracic echocardiogram showed left ventricular dysfunction (ejection fraction 26%), severe aortic stenosis, and moderate functional mitral regurgitation. B Pathology of the left atrial appendage showed diffuse interstitial amyloid deposits by Hematoxylin-Eosin and direct fast scarlet staining, positive for atrial natriuretic peptide immunohistochemical staining, as well as nodular amyloid deposits positive for transthyretin (asterisks). C Pathology of the aortic valve revealed nodular amyloid deposits by direct fast scarlet staining with apple-green birefringence under polarized light microscopy, positive for transthyretin immunohistochemical staining. D 99mTechnetium-pyrophophate scintigraphy showed no significant myocardial uptake, and cardiac magnetic resonance showed no late gadolinium enhancement and normal extracellular volume fraction (29.9%)
Pathology of the resected LA appendage (Fig. 1B) showed diffuse interstitial amyloid deposits positive for atrial natriuretic peptide (AANP) immunohistochemistry, as well as nodular amyloid deposits positive for ATTR immunohistochemistry. Further, pathology of the aortic valve also revealed nodular ATTR amyloid deposits (Fig. 1C). The patient’s postsurgical course was uneventful. 99mTechnetium-pyrophosphate (99mTc-PYP) scintigraphy showed no atrial or ventricular uptake, and cardiac magnetic resonance (CMR) showed no late gadolinium enhancement (LGE) and normal extracellular volume fraction (29.9%), suggesting that ATTR-CA infiltrating the ventricles was unlikely (Fig. 1D). Troponin T (0.009 ng/ml; reference range < 0.014 ng/ml) and plasma ANP (20.1 pg/ml; reference range < 43.0 pg/ml) were normal. The patient’s EF and GLS improved to 65% and − 17.2%, and BNP decreased to 48.8 pg/ml at 6 months follow up. He has been in NYHA class I and uneventful for 24 months since surgery. No follow up evaluations have suggested ATTR-CA, including latest echocardiogram showing no LV dysfunction or LV hypertrophy (EF 60%, LVEDD/ESD 46/26 mm, IVS/PW 11/11 mm) and low BNP (39.0 pg/ml).
Case 2
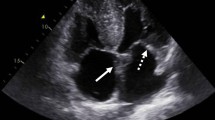
A 73-year-old woman was admitted for transient ischemic attack. She had no AF, normal echocardiogram (EF 60%, LVEDD/ESD 42/28 mm, IVS/PWT 7/7 mm) and normal BNP (16.5 pg/ml). Transesophageal echocardiogram and contrast-enhanced computed tomography revealed a 9-mm pedunculated mobile mass in the LA next to the LA appendage, which was suspected to be the source of emboli (Fig. 2A). LA mass and partial LA wall resection were performed.
Images of Case 2. A Transesophageal echocardiogram and contrast-enhanced computed tomography revealed a 9 mm pedunculated mobile mass on the left atrial wall next to the left atrial appendage. B Pathology of the left atrial mass showed diffuse interstitial amyloid deposits (by Hematoxylin-Eosin and direct fast scarlet staining) positive for atrial natriuretic peptide, as well as nodular amyloid deposits positive for transthyretin. C 99mTechnetium-pyrophosphate scintigraphy showed no significant myocardial uptake, and cardiac magnetic resonance showed no ventricular late gadolinium enhancement but slight gadolinium enhancement in the left atrial walls
Pathology of the mass showed diffuse interstitial AANP amyloid deposits, as well as nodular ATTR amyloid deposits (Fig. 2B). Troponin T was normal (0.009 ng/ml) and plasma ANP was slightly elevated (66.3 pg/ml). 99mTc-PYP scintigraphy showed no atrial or ventricular uptake, and CMR showed no ventricular LGE but slight enhancement in the LA walls (Fig. 2C). The patient has been uneventful for 24 months since surgery and no follow up data have suggested ATTR-CA; echocardiogram with no LV hypertrophy and normal GLS (EF 64%, LVEDD/ESD 43/28 mm, IVS/PW 8/8 mm, GLS − 20.4%), and normal Trop T (0.012 ng/ml).
Case 3
A 78-year-old woman with a history of AF, pacemaker implantation, long standing hypertension and LV outflow tract obstruction (LVOTO) was admitted for dyspnea on exertion. Troponin T was normal (0.008 ng/ml), and BNP was elevated (261.4 pg/ml). Echocardiogram (Fig. 3A) showed LVEDD/ESD 42/27 mm, IVS/PWT 13/10 mm, LVOTO (provoked peak pressure gradient 92 mmHg) and low gradient moderate AS (peak velocity 2.6 m/s, mean pressure gradient 14 mmHg, AVA 1.23 cm2). Perioperative evaluations for LV hypertrophy included CMR showing asymmetric septal hypertrophy (septum thickness 15 mm) with no LGE (Fig. 3A), and right ventricular endomyocardial biopsy (RV-EMB) showing no significant amyloid in the myocardium, except for ATTR amyloid deposits on the vessel walls of small arteries (Fig. 3B). For drug refractory LVOTO with concomitant AS, SAVR and subaortic septal myectomy were performed.
Images of Case 3. A Transthoracic echocardiogram showed mild left ventricular hypertrophy and sigmoid septum showing significant left ventricular outflow tract obstruction, with concomitant low gradient aortic stenosis. Cardiac magnetic resonance also showed asymmetric septal hypertrophy (septum thickness 15 mm) with no significant late gadolinium enhancement. B Preoperative right ventricular endomyocardial biopsy showed no significant amyloid deposits in the myocardium, except for transthyretin amyloid deposits on the vessel walls of small arteries confirmed by Congo red staining with apple-green birefringence under polarized light microscopy and immunohistochemical staining for transthyretin (asterisks). C Pathology of the resected aortic valve showed patchy amyloid deposits confirmed by Congo red staining with apple-green birefringence under polarized light microscopy and immunohistochemical staining positive for transthyretin. D Pathology of resected myocardium from subaortic septal myectomy showed no significant amyloid deposits in the myocardium, except for transthyretin amyloid deposits on the vessel walls of small arteries confirmed by Congo red staining and immunohistochemical staining for transthyretin
Pathology of the aortic valve showed patchy ATTR amyloid deposits (Fig. 3C). The myocardium from subaortic myectomy showed no significant myocardial amyloid deposits, except for ATTR amyloid on the vessel walls of the small arteries (Fig. 3D), similar to the preoperative RV-EMB. The patient has been followed up for 5 years since surgery and no follow up evaluations have suggested ATTR-CA infiltrating the ventricles; mildly elevated BNP (407.7 pg/ml) but no LV dysfunction or LV hypertrophy on echocardiogram (EF 60%, LVEDD/ESD 40/25 mm, IVS/PW 10/10 mm at 5 years).
Discussion and conclusions
We report 3 cases of extraventricular ATTR amyloid deposits confirmed in surgically resected aortic valves and LA structures, all of which were unlikely to have ATTR amyloidosis infiltrating the ventricles as determined by multimodality evaluation and mid-term clinical course up to 5 years (summarized in Table 1). Our cases suggest the existence of extraventricular ATTR amyloid deposits localized in the aortic valve and LA structures.
AANP derived and ATTR derived amyloid deposits in the atrium
AANP amyloid deposits in the atrium, often referred to as isolated atrial amyloidosis (IAA) [8, 9], have been reported in surgically resected appendages and autopsy studies [4, 10,11,12,13,14,15,16]; however, very few histologically reports of ATTR amyloid in the atrium are published [4, 10,11,12]. Further, most previous studies were limited to evaluation of the atrium and did not evaluate the ventricles or other cardiac structures. Thus, the relationship between ATTR amyloid deposits in the atrium and ATTR-CA infiltrating the ventricles, and the clinical impact of atrial ATTR amyloid deposits remains unclear.
Di Bella et al. reported in 2018 that atrial involvement in ATTR-CA is an early stage of ATTR-CA [7]. However, recent reports show contradictory results [2, 4]. Ichimata et al. [4], in line with Di Bella et al., reported in a study of 44 autopsy cases of ATTR-CA evaluating multiple cardiac regions that atria-predominant ATTR amyloid deposition may precede TTR amyloidosis of the ventricles; however, by using cluster analysis from retrospective insights. On the other hand, Hussain et al. [2] recently reported in a study of 580 patients with 99mTc-PYP scintigraphy that 58 patients had atrial uptake without ventricular uptake, while 105 patients had ventricular uptake without atrial uptake, indicating that atrial involvement may not necessarily precede ventricular involvement.
As ATTR amyloids are believed to be derived and formed from circulating transthyretin protein synthesized by the liver, ATTR amyloid deposits in the atrium may be a part of systemic disease and ATTR amyloid deposits could be found in other tissue sites after long-term follow up. However, our findings support the possibility that they could be localized atrial ATTR amyloid deposits. While the clinical significance of atrial ATTR amyloid deposits has not been fully elucidated and long-term close follow-up may be justified at this point, our 2 cases of surgically resected ATTR amyloid deposits in the atrium with mid-term prospective follow up, the first to be reported with multimodality evaluations, suggest the possibility of extraventricular ATTR amyloid deposits localized in the atrium.
ATTR amyloid deposits in the aortic valve
While various types of amyloid deposits including light-chain (AL), amyloid A protein (AA) and Apo-AI have been reported in surgically resected aortic valves and autopsy studies, very few histological reports of ATTR amyloid in the aortic valve have been published [17,18,19], and their relationship with ATTR-CA infiltrating the ventricles is not fully understood. Recent studies have reported that ATTR-CA (infiltrating the ventricles) coexists in 11–16% of elderly patients with AS undergoing transcatheter aortic valve implantation [5, 6]. However, histological diagnosis is rarely confirmed in these patients, and the association among ATTR-CA, AS and aging has not been clarified.
Recently, Singal et al. studied 46 surgically resected aortic valves with concomitant ventricular biopsy and reported that 33 (71.7%) had aortic valvular amyloid deposits (including 19 ATTR derived); however, none had amyloid deposits in the ventricle, and they concluded that the majority were “isolated valvular ATTR amyloid deposits” [19]. In line with their report, our 2 surgical cases of ATTR amyloid deposits in the aortic valve with longer follow-up (up to 5 years) and multimodality evaluations support the possibility of localized ATTR amyloid deposits in the aortic valves.
Similar to the discussion with ATTR amyloid deposits in the atrium, deposition of ATTR amyloid is believed to be a systemic process, thus we could not rule out the possibility that valvular ATTR amyloid deposit is an early stage of ATTR-CA (infiltrating the ventricles) without long-term follow up. However, our cases suggest the possibility that they could be localized valvular ATTR amyloid deposits. Our findings also suggests that, to understand the pathophysiology of patients with concomitant AS and ATTR-CA, the existence of amyloid deposits localized in the valves should be taken into consideration.
Patient perspectives
While clinical implications of extraventricular ATTR amyloid deposits localized outside the ventricles are not fully elucidated, our cases are the first detailed report of surgically resected cases and with mid-term follow up (up to 5 years), which suggested the existence of extraventricular ATTR amyloid deposits localized in the aortic valve and the atrial structures. Diagnosis of amyloid deposits were confirmed by Congo red or direct fast scarlet staining, followed by immunohistochemistry staining for ATTR and AANP. Mass spectrometry or immunoelectron microscopy was unavailable in our patients, which might have provided further insights because of their proven superior sensitivity compared to immunohistochemistry [20, 21].
It could be hypothesized that our cases were localized amyloid deposits rather than an early ATTR-CA, and raises the possibility of localized “innocent” deposits not strictly related to systemic deposition as reported in literatures [10, 22,23,24]. However, non-cardiac manifestations or extracardiac ATTR amyloid deposits as in the case of carpal tunnel syndrome [25, 26] are believed to precede ATTR-CA by a period of years (although none of our 3 cases had history of carpal tunnel syndrome or lumber canal stenosis). Further long-term prospective studies will clarify the clinical implications of extraventricular ATTR amyloid deposits and help us understand whether they are useful for early diagnosis and treatment intervention of ATTR-CA [27].
Availability of data and materials
Data associated with this manuscript are not publicly available, but can be made available by the corresponding author upon reasonable request.
Abbreviations
- ANP:
-
Atrial natriuretic peptide
- AS:
-
Aortic stenosis
- CA:
-
Cardiac amyloidosis
- CMR:
-
Cardiac magnetic resonance
- EMB:
-
Endomyocardial biopsy
- IAA:
-
Isolated atrial amyloidosis
- LA:
-
Left atrium
- SAVR:
-
Surgical aortic valve replacement
- 99mTc-PYP:
-
99mTechnetium-pyrophosphate
- ATTR:
-
Transthyretin
References
Bandera F, Martone R, Chacko L, Ganesananthan S, Gilbertson JA, Ponticos M, et al. Clinical importance of left atrial infiltration in cardiac transthyretin amyloidosis. JACC Cardiovasc Imaging. 2022;15:17–29.
Hussain M, Krywanczyk A, Donnellan E, Martyn T, Hassan OA, Alkharabsheh S, et al. Association between atrial uptake on cardiac scintigraphy with technetium-99m-pyrophosphate labeled bone-seeking tracers and atrial fibrillation. Circ Cardiovasc Imaging. 2022;15:e013829.
Di Bella G, Cappelli F, Licordari R, Piaggi P, Campisi M, Bellavia D, et al. Prevalence and diagnostic value of extra-left ventricle echocardiographic findings in transthyretin-related cardiac amyloidosis. Amyloid. 2022;29:197–204.
Ichimata S, Hata Y, Hirono K, Yamaguchi Y, Nishida N. Clinicopathological features of clinically undiagnosed sporadic transthyretin cardiac amyloidosis: a forensic autopsy-based series. Amyloid. 2021;28:125–33.
Scully PR, Patel KP, Treibel TA, Thornton GD, Hughes RK, Chadalavada S, et al. Prevalence and outcome of dual aortic stenosis and cardiac amyloid pathology in patients referred for transcatheter aortic valve implantation. Eur Heart J. 2020;41:2759–67.
Ternacle J, Krapf L, Mohty D, Magne J, Nguyen A, Galat A, et al. Aortic stenosis and cardiac amyloidosis: JACC review topic of the week. J Am Coll Cardiol. 2019;74:2638–51.
Di Bella G, Minutoli F. Atrial impairment in transthyretin cardiac amyloidosis: an early marker of cardiac involvement and a prognostic factor. Amyloid. 2018;25:135.
Vergaro G, Aimo A, Rapezzi C, Castiglione V, Fabiani I, Pucci A, et al. Atrial amyloidosis: mechanisms and clinical manifestations. Eur J Heart Fail. 2022;24:2019–28.
van den Berg MP, Mulder BA, Klaassen SHC, Maass AH, van Veldhuisen DJ, van der Meer P, et al. Heart failure with preserved ejection fraction, atrial fibrillation, and the role of senile amyloidosis. Eur Heart J. 2019;40:1287–93.
Rocken C, Peters B, Juenemann G, Saeger W, Klein HU, Huth C, et al. Atrial amyloidosis: an arrhythmogenic substrate for persistent atrial fibrillation. Circulation. 2002;106:2091–7.
Fayyaz AU, Bois MC, Dasari S, Padmanabhan D, Vrana JA, Stulak JM, et al. Amyloidosis in surgically resected atrial appendages: a study of 345 consecutive cases with clinical implications. Mod Pathol. 2020;33:764–74.
Kawamura S, Takahashi M, Ishihara T, Uchino F. Incidence and distribution of isolated atrial amyloid: histologic and immunohistochemical studies of 100 aging hearts. Pathol Int. 1995;45:335–42.
Bhakhri K, Volpi S, Gori D, Goddard M, Ali JM, De Silva R. Isolated atrial amyloid: a potential contributor to morbidity and mortality following cardiac surgery. Interact Cardiovasc Thorac Surg. 2019;29:187–92.
Ariyarajah V, Steiner I, Hajkova P, Khadem A, Kvasnicka J, Apiyasawat S, et al. The association of atrial tachyarrhythmias with isolated atrial amyloid disease: preliminary observations in autopsied heart specimens. Cardiology. 2009;113:132–7.
Steiner I, Hajkova P. Patterns of isolated atrial amyloid: a study of 100 hearts on autopsy. Cardiovasc Pathol. 2006;15:287–90.
Larsen BT, Mereuta OM, Dasari S, Fayyaz AU, Theis JD, Vrana JA, et al. Correlation of histomorphological pattern of cardiac amyloid deposition with amyloid type: a histological and proteomic analysis of 108 cases. Histopathology. 2016;68:648–56.
Fujimoto T, Yamano T, Miyagawa-Hayashino A, Naiki H, Ueda M, Tasaki M, et al. Case with transthyretin amyloid cardiomyopathy complicated with rapidly progressive aortic stenosis possibly caused by amyloid deposition in the aortic valve. Circ Cardiovasc Imaging. 2021;14:e013357.
Hosoda Y, Ueda M, Takaki J, Okamoto K, Yamashita T, Fukui T. Early progression of aortic stenosis associated with iatrogenic variant transthyretin amyloidosis after domino liver transplantation. JACC Case Rep. 2020;2:1155–60.
Singal AK, Bansal R, Singh A, Dorbala S, Sharma G, Gupta K, et al. Concomitant transthyretin amyloidosis and severe aortic stenosis in elderly indian population: a pilot study. JACC CardioOncol. 2021;3:565–76.
Abildgaard N, Rojek AM, Moller HE, Palstrom NB, Nyvold CG, Rasmussen LM, et al. Immunoelectron microscopy and mass spectrometry for classification of amyloid deposits. Amyloid. 2020;27:59–66.
Benson MD, Berk JL, Dispenzieri A, Damy T, Gillmore JD, Hazenberg BP, et al. Tissue biopsy for the diagnosis of amyloidosis: experience from some centres. Amyloid. 2022;29:8–13.
Leone O, Boriani G, Chiappini B, Pacini D, Cenacchi G, Martin Suarez S, et al. Amyloid deposition as a cause of atrial remodelling in persistent valvular atrial fibrillation. Eur Heart J. 2004;25:1237–41.
Marcoux J, Mangione PP, Porcari R, Degiacomi MT, Verona G, Taylor GW, et al. A novel mechano-enzymatic cleavage mechanism underlies transthyretin amyloidogenesis. EMBO Mol Med. 2015;7:1337–49.
Mangione PP, Porcari R, Gillmore JD, Pucci P, Monti M, Porcari M, et al. Proteolytic cleavage of Ser52Pro variant transthyretin triggers its amyloid fibrillogenesis. Proc Natl Acad Sci U S A. 2014;111:1539–44.
Sperry BW, Reyes BA, Ikram A, Donnelly JP, Phelan D, Jaber WA, et al. Tenosynovial and cardiac amyloidosis in patients undergoing carpal tunnel release. J Am Coll Cardiol. 2018;72:2040–50.
Westin O, Fosbol EL, Maurer MS, Leicht BP, Hasbak P, Mylin AK, et al. Screening for cardiac amyloidosis 5 to 15 years after surgery for bilateral carpal tunnel syndrome. J Am Coll Cardiol. 2022;80:967–77.
Maurer MS, Schwartz JH, Gundapaneni B, Elliott PM, Merlini G, Waddington-Cruz M, et al. Tafamidis treatment for patients with transthyretin amyloid cardiomyopathy. N Engl J Med. 2018;379:1007–16.
Acknowledgements
Not applicable.
Funding
This work was supported by Grant-in-Aid for Early-Career Scientists from the Japan Society for the Promotion of Science (20K17171). The funder had no role in study design, data collection, analysis, interpretation of data, or manuscript writing.
Author information
Authors and Affiliations
Contributions
Conceptualization: AO, CI. Methodology: AO, CI. Investigation: AO, T.Kakuta, NT, ET, YM, T.Kitai, MA, HK, KOO, YI, SF, TF. Writing – Original Draft: AO. Writing – Review and Editing: SF, TF, CI. Supervision: KK, TN, CI. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the institutional review board of National Cerebral and Cardiovascular Center (R20090). The authors confirm that written informed consent for submission and publication of this case report has been obtained from the patients.
Consent for publication
Written informed consent was obtained from all patients for publication of this case report. Copies of the consent forms are available for review by the Editor of this journal.
Competing interests
AO reports grant and personal fees from Pfizer Inc. and personal fees from Alnylam Pharmaceuticals, outside the submitted work. Other authors have nothing to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Okada, A., Kakuta, T., Tadokoro, N. et al. Transthyretin derived amyloid deposits in the atrium and the aortic valve: insights from multimodality evaluations and mid-term follow up. BMC Cardiovasc Disord 23, 281 (2023). https://doi.org/10.1186/s12872-023-03319-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-023-03319-3