Abstract
Background
Hypertension has become an important health risk factor in the twenty-first century, especially for the elderly. Studies have confirmed that inflammation is involved in the development of hypertension and that the inflammatory marker C-reactive protein(CRP) is significantly associated with hypertension. Therefore, in this study, we aimed to explore the CRP correlation with hypertension in the elderly.
Methods
Serum CRP levels were measured in 196 hospitalized patients, and the CRP level was used as a criterion to divide them into the group with elevated CRP (> 10 mmol/L, n = 120) and the group with normal CRP (0 < CRP ≤ 10 mmol/L, n = 76). and the patient's baseline characteristics were collected and compared between the groups, and the correlation between CRP and other factors and hypertension in the elderly was analyzed by multi-factor logistic regression.
Results
The prevalence of hypertension, coronary artery disease and joint reactive inflammation was significantly higher in the group with elevated CRP. There was also a significant association between the use of alcohol, low density lipoprotein cholesterol (LDL-C) and steroids and elevated CRP; logistic regression showed that elevated CRP (OR = 2.13, 95% CI: 1.14–3.99, p = 0.019), body mass index (BMI) (OR = 1.10, 95% CI:1.01–1.90, p = 0.030), diabetes (OR = 2.68, 95% CI:1.24–5.79, p = 0.012) were positively associated with hypertension, while statins use was negatively associated with hypertension (OR = 0.49, 95% CI: 0.25–0.94, p = 0.013).
Conclusions
Elevated CRP, BMI, and diabetes are positively associated with hypertension in the elderly, and early screening for CRP and initiation of treatment may help prevent further inflammatory responses in hypertension.
Highlights
1. Inflammation plays an important role in vascular remodeling and myocardial remodeling in hypertension. Our study found that CRP, as a marker of systemic inflammation, was significantly positively correlated with hypertension in the elderly.
2. The most common phenomenon in elderly patients is co-morbidity. we found that the proportion of hypertension, coronary heart disease and arthritis in patients with elevated CRP was significantly higher than that in patients with normal CRP.
3. Inflammation is related to hypertension, and CRP is one of the inflammatory markers. Early screening and intervention of CRP may delay the progression of hypertension.
Similar content being viewed by others
Introduction
The incidence and mortality of cardiovascular and cerebrovascular diseases are.
increasing year by year. According to statistics, China has now become the country with the highest cardiovascular mortality [1]. Hypertension is an important risk factor for cardiovascular and cerebrovascular diseases. Due to the continuous progress of population aging, the prevalence of hypertension in the elderly over 65 years old is increasing, while the prevalence of hypertension in the elderly population over 80 years old is more than 90% [2, 3]. Therefore, hypertension has been an urgent problem to solve and prevent. Hypertension is considered to be an inflammatory disease [4, 5]. Inflammatory response plays an important role in vascular remodeling and myocardial remodeling in hypertension. In 2001, Bautista et al. [6] found that CRP levels remained strongly associated with hypertension and first clearly proposed CRP concentrations as an independent risk factor for hypertension, but this finding was numerous questioned due to the small sample size of their study and the fact that the prevalence of hypertension was as high as 46%, higher than the prevalence at that time. Subsequently, Sesso et al. [7], after following 20,525 normotensive women for an average of 7–8 years, observed a total of 5365 hypertensive patients, and baseline CRP concentrations were higher in these populations than in non-hypertensive populations, and even after adjusting for multiple risk factors, baseline CRP was still independently associated with hypertensive events, thus proposing CRP as an independent predictor of hypertension [8, 9]. Subsequently, scholars from home and abroad conducted cross-sectional and prospective studies on the association between CRP and hypertension, all of which confirmed that CRP was independently associated with hypertension and that CRP was one of the predictors of hypertension. However, most of the study subjects included in their experiment were young and middle-aged men and women, so the experimental results suggest that CRP is independently associated with hypertension in younger age groups. However, fewer experiments have been conducted nationally and internationally to study the correlation between CRP levels and hypertension in older adults over 65 years of age, especially in the elderly. Therefore, the main purpose of our study was to explore the relationship between CRP and hypertension in the elderly, and to provide support for the prevention of early hypertension and common diseases in the elderly.
Methodology
Study Sample
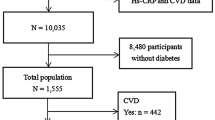
We selected 306 elderly (age ≥ 65 years) patients who visited the Hebei General Hospital between November 2020 and November 2021, and 196 cases with complete data and meeting the inclusion and exclusion criteria as the study population (Fig. 1). All study subjects were excluded from the use of anti-hypertensive drugs. The normal range of CRP in our hospital laboratory was 0 < CRP ≤ 10 mmol/L. Based on this criterion, we divided the study subjects into a group with elevated CRP (CRP > 10 mmol/L, N = 120) and a group with normal CRP (0 < CRP ≤ 10 mmol/L, N = 76). Diagnostic criteria for geriatric hypertension were performed according to the Chinese Guidelines for the Management of Geriatric Hypertension 2019 [3], That is, in elderly people aged ≥ 65 years, SBP ≥ 140 mmHg (1 mmHg = 0.133 kPa) and/or DBP ≥ 90 mmHg measured three times on different days without antihypertensive drugs can be diagnosed as geriatric hypertension. Older adults who have been diagnosed with hypertension and are receiving antihypertensive medication, although their blood pressure is < 140/90 mmHg, should be diagnosed with geriatric hypertension. In addition, All study subjects signed informed consent, and this study was approved by our hospital ethics committee.
Sample collection and analysis
We collected general information about the study subjects, including age, sex, height, weight, and calculated the corresponding BMI. We mainly collected the following data from the study subjects: (1) basic information: age, sex, height, weight, and calculated the corresponding BMI; (2) systolic and diastolic blood pressure; (3) personal history: history of smoking and alcohol consumption; (4) related diseases: hypertension, diabetes mellitus, hyperlipidemia, coronary heart disease, cerebrovascular disease, carotid artery stenosis, peripheral arterial disease, hypothyroidism, congestive heart failure, arthritis, other rheumatologic disorders, asthma, Liver disease.(4) History of medications, such as aspirin, non-steroidal anti-inflammatory drugs(NSAIDs), statins, steroids and immunosuppressive drugs; (5) Relevant laboratory tests: all study subjects fasted for 8–12 h before the morning collection of elbow venous blood, and the main collection included CRP, white blood cell count (WBC), total cholesterol (TC), LDL-C, high density lipoprotein cholesterol (HDL-C) and triglyceride (TG), etc. Immuno-dispersive turbidimetry was used to determine CRP.
Statistical methods
Statistical analysis was completed using IBM SPSS 26.0 software. For the 196 subjects included in this study, the statistics of normally distributed measures were expressed as mean ± standard deviation and analyzed by the independent samples t-test, while the non-normal distribution was expressed as median (interquartile spacing) and analyzed by the Mann–Whitney U test; the count data were expressed as percentages and the chi-square test was used for comparison between groups; To exclude the effect of confounding factors, we used multifactorial logistic regression to analyze the relationship between normal and elevated CRP, age, sex, BMI, statins, diabetes mellitus, chronic obstructive pulmonary disease, and asthma and hypertension in the elderly.
Results
Baseline characteristics of the study cohort
A total of 196 elderly patients were included in this study, 120 (61.2%) in the group with elevated CRP, of which 64 (53.3%) were men and 56 (46.7%) were women, aged 65–92 years, and 76 (38.8%) in the group with normal CRP, of which 45 (59.2%) were men and 31 (40.8%) were women, aged 65–94 years old. There were differences between the two groups in SBP, DBP and history of alcohol consumption, and the group with elevated CRP was larger than the normal group, with statistically significant differences (P < 0.05), while there were no significant differences between age, gender, BMI and history of smoking, with no statistically significant differences (P > 0.05).For laboratory indices, LDL-C levels were higher in the group with elevated CRP than in the normal group (P < 0.05), and there was no statistically significant difference between the two groups in TC, TG, HDL-C, and WBC (P > 0.05) (Table 1).
Comparison of drug use history
In terms of medication history, there was a difference between the two groups in taking steroid hormone drugs, with the elevated group (45.0%) being greater than the normal group (30.3%), with a statistically significant difference (P < 0.05); in taking aspirin, statins, non-steroidal anti-inflammatory drugs, and immunosuppressants, the difference was not statistically significant. (P > 0.05) (Table 2).
Comparison of co-morbidities
Analysis of co-morbidities showed that we found significant differences between the two groups suffering from hypertension, coronary heart disease, and arthritis, and the group with elevated CRP was larger than the normal group, with statistically significant differences (P < 0.05); between the two groups with diabetes, hyperlipidemia, cerebrovascular disease, carotid stenosis, peripheral arterial disease, hypothyroidism, congestive heart failure, other rheumatic diseases, psychosomatic diseases, chronic obstructive pulmonary disease, asthma, and liver disease, the differences were not statistically significant (P > 0.05) (Table 3).
To exclude the effect of confounding factors, we used multifactorial logistic regression to analyze the relationship between CRP and other related factors and hypertension, and the results showed that BMI (OR = 1.01,95%CI:1.01–1.19), elevated CRP (OR = 2.13,95%CI:1.14–3.99), diabetes mellitus (OR = 2.68,95% CI:1.24–5.79) were positively associated with hypertension (P < 0.05), statin use was a protective factor for hypertension (OR = 0.49, 95% CI: 0.25–0.94, P < 0.05), and age, gender, Chronic obstructive pulmonary disease and asthma were not significantly associated with hypertension (P > 0. 05) (Table 4).
Discussion
CRP as a sensitive inflammatory marker is involved in the non-specific inflammatory response of the body. Elevated CRP not only predicts a much higher probability of developing hypertension from normal blood pressure or prehypertension, but in patients with diagnosed hypertension, elevated CRP often indicates poor blood pressure control or the development of hypertensive complications, and in patients with high baseline blood pressure, both systolic and diastolic, CRP is mostly elevated [10]. Several cross-sectional and cohort studies have reported an association between CRP and hypertension, and their studies all support the association between CRP and hypertension, and CRP may serve as a predictor of hypertension [7, 9, 11,12,13]. Savoia et al. [14] found that high levels of CRP upregulate angiotensin receptor expression, promote plasminogen activator inhibitor-1 (PAI-1) production, and activate vascular smooth muscle, promote the release of inflammatory factors, attenuate the response of vascular endothelial cells to diastolic substances, reduce nitric oxide production, and increase vascular resistance. In our study, we found that in the elderly population, blood pressure levels were significantly higher in the group with elevated CRP than in the normal group, and the prevalence of hypertension was higher in the group with elevated CRP than in the normal group, with statistically significant differences (P < 0.05), and logistic regression also showed an independent positive association between elevated CRP and the risk of hypertension (OR = 2.13, 95% CI: 1.14–3.99, P < 0.05). In a study of the effect on the risk of hypertension in the US retired population, which included 2924 participants, logistic regression showed that CRP could be used as a predictor of hypertension in women [15]. In another study of CRP and hypertension in Japanese men [16], 2991 male workers without hypertension were evaluated, and the risk ratio (HR) for the occurrence of hypertensive events was estimated based on the quartiles of CRP, and 579 (19.4%) subjects developed hypertension during the 5-year follow-up period, and the incidence of hypertension increased with increasing levels of CRP, and the HR increased significantly with increasing CRP levels. This may imply that the development of hypertension involves a pathological process in which inflammation is involved and that the inflammatory response may be the direct cause of hypertension.
As we age, our physiological functions gradually decline. In addition to hypertension, the coexistence of various diseases such as coronary heart disease and diabetes is becoming more and more evident in the elderly population. According to a survey conducted by the Journal of the American Medical Family Council in 2013, about 2/3 of American senior citizens have co-morbidities [17]. A large body of evidence suggests that CRP is closely associated with dyslipidemia, diabetes, cardiovascular disease, and metabolic syndrome, and can be used as an indicator for early screening or long-term monitoring to provide some basis for patient prognosis [18,19,20]. CRP acts as a marker of inflammation and numerous studies have shown that CRP is significantly associated with cardiovascular disease. When an inflammatory response is generated, CRP is induced by interleukin 1 (IL-1), interleukin-6 (IL-6) and tumor necrosis factor (T NF-α), mainly by the liver. CRP is often elevated in nonalcoholic fatty liver disease, suggesting that the accumulation of hepatic adipose tissue is associated with enhanced inflammation-mediated oxidative stress. CRP induces a significant increase in the expression of intercellular adhesion molecule-1 (ICAM-1) and vascular cell adhesion molecule-1 (VCAM-1), which accelerates the inflammatory response in atherosclerosis. At the same time, high concentrations of CRP can promote thickening of the intima and atherosclerosis, leading to remodeling of hypertensive vessels [21, 22]. In addition, CRP stimulates endothelial cells, megalophils and polymorphonuclear cells to secrete endothelin-1 (ET-1), interleukin-6 (IL-6) and vasoconstrictor peptide, resulting in vasoconstriction [22]. Coronary artery disease was significantly associated with elevated CRP levels in this study, and serum LDL-C was also associated with elevated CRP, with statistically significant differences (P < 0.05). This is consistent with previous research[23]. In addition, CRP has been shown to be an independent predictor of the risk of myocardial infarction, stroke and peripheral vascular disease and can be used to predict future risk in patients with stable and unstable angina [24]. In addition, we found that the prevalence of diabetes was higher in the group with elevated CRP than in the normal group, and although it was not statistically significant, diabetes was positively associated with the development of hypertension (OR = 2.68,95%CI:1.24–5.79, P < 0.05). Studies have concluded that CRP concentrations tend to be higher in patients with type 2 diabetes and that CRP can disrupt insulin homeostasis and increase the risk of disease by blocking the major cascade of downstream insulin signaling [25], and in vitro studies have also shown an association between serum CRP levels and β-cell dysfunction and insulin resistance[26]. In addition, the development of arthritis is undoubtedly an important cause of reduced quality of life in elderly or even elderly patients, and arthritis as an inflammatory condition is closely associated with CRP. For example, patients with rheumatoid arthritis usually have persistently elevated CRP levels, with baseline CRP levels often exceeding 20 mg/L in randomized clinical trials of drugs for rheumatoid arthritis [16], however, retrospective and observational studies have found that many patients with rheumatoid arthritis have normal CRP levels despite exhibiting disease activity, suggesting that CRP levels only reflect signs of disease activity [27, 28].
Obesity as a risk factor for hypertension has become a globally recognized fact, and in this study, BMI was higher in the group with elevated CRP than in the normal group, and although the difference was not statistically significant (P > 0.05), studies have shown that pro-inflammatory proteins such as interleukin 6 (IL-6), which is broken down by adipose tissue in obese individuals, can increase CRP levels in the liver [28]. In 2003, Hotamisligil [29] proposed that obesity is a state of systemic chronic low-grade inflammation induced by different inflammatory factors. CRP, as a relatively sensitive marker of chronic inflammation, reflects the activity and amount of inflammatory factors, and is involved in the pathogenesis of obesity by regulating lipid metabolism, increasing the inflammatory response, decreasing tissue sensitivity to insulin, stimulating insulin secretion, and promoting lipid synthesis, further aggravating obesity [30]. We also found that steroid use was proportionally higher in the group with elevated CRP (p < 0.05). As an inhibitor of hydroxy-methyl-glutaryl coenzyme A reductase, statin not only reduces LDL-C levels, but also decreases inflammation, reduces oxidative stress, and has a protective effect on the cardiovascular system. For example, Rosuvastatin has been shown to be effective not only in improving lipids, but also in lowering CRP levels, reducing vascular inflammatory responses, and improving endothelial cell function, with positive effects on preventing and reducing cardiovascular clinical endpoints [31]. This study also showed that statin use was higher in the group with normal CRP than in the group with elevated CRP, and although not statistically significant, statin use reduced the risk of hypertension (OR = 0.49,95%CI: 0.25–0.94, p < 0.05) and was protective against hypertension. Earlier studies have suggested an association between alcohol consumption and CRP, but the form of the association is uncertain [32]. Our study found a higher proportion of alcohol consumption in the group with elevated CRP (P < 0.05), which is similar to the findings of a recent cohort study of Chinese men aged 50 years and older [33], which showed that compared with never and occasional drinkers (< 1 drink/week), daily (OR = 1.38, 95% CI: 1.24–2.65) and excessive drinkers (weekly ethanol intake ≥ 210 g, OR = 1.57, 95% CI: 1.22–2.02) had a higher risk of elevated CRP and a higher risk of cardiovascular disease, and therefore patients are advised to drink less or even abstain from alcohol.
As a retrospective study with elderly patients, the data were obtained from the electronic medical records of patients attending our hospital, based on the patients' admission, the collection of general data may lack accuracy, thus affecting the interpretation of the results. Furthermore, we included elderly patients, and because co-morbidity is common in elderly patients, it was not possible to set up a healthy population as a control group to assess the relationship between CRP and hypertension. Finally. our study, as a cross-sectional study, was unable to assess the relationship between CRP concentration and the severity of hypertension, with a small sample size, and further prospective analysis is needed in the future.
Conclusions
The present study showed that elevated CRP was positively associated with hypertension in the elderly, and in addition to CRP, BMI and diabetes mellitus were also shown to be risk factors for hypertension, and statin use may reduce the inflammatory response to some extent and have a protective effect on hypertension. In addition, alcohol consumption, LDL-C, coronary artery disease, arthritis, and steroid use are also associated with elevated CRP. The inflammatory response is involved in the development of hypertension, and early screening for CRP in the elderly population and early initiation of treatment may help prevent further development of the inflammatory response, and increasing the sample size will facilitate further research on whether CRP can be used to manage hypertension and other related diseases in the elderly.
Availability of data and materials
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
References
Roth GA, Mensah GA, Johnson CO, et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update From the GBD 2019 Study. J Am Coll Cardiol. 2020;76(25):2982–3021.
Wang Z, Chen Z, Zhang L. c: Status of Hypertension in China: Results From the China Hypertension Survey, 2012–2015. Circulation. 2018;137(22):2344–56.
Wang Z, Hao G, Wang X, et al. Clinical outcomes and economic impact of the 2017 ACC/AHA guidelines on hypertension in China. J Clin Hypertens (Greenwich). 2019;21(8):1212–20.
Wenzel UO, Bode M, Kurts C, Ehmke H. Salt, inflammation, IL-17 and hypertension. Br J Pharmacol. 2019;176(12):1853–63.
Agita A, Alsagaff MT. Inflammation, Immunity, and Hypertension. Acta Med Indones. 2017;49(2):158–65.
Bellelli G, Rozzini R, Battista Frisoni G, Trabucchi M. Is C-reactive protein an independent risk factor for essential hypertension? J Hypertens. 2001;19(11):2107.
Sesso HD, Buring JE, Rifai N, Blake GJ, Gaziano JM, Ridker PM. C-reactive protein and the risk of developing hypertension. JAMA. 2003;290(22):2945–51.
Bautista LE, Atwood JE, O’Malley PG, Taylor AJ. Association between C-reactive protein and hypertension in healthy middle-aged men and women. Coron Artery Dis. 2004;15(6):331–6.
Lakoski SG, Cushman M, Siscovick DS, et al. The relationship between inflammation, obesity and risk for hypertension in the Multi-Ethnic Study of Atherosclerosis (MESA). J Hum Hypertens. 2011;25(2):73–9.
Schillaci G, Pirro M. C-reactive protein in hypertension: clinical significance and predictive value. Nutr Metab Cardiovasc Dis. 2006;16(7):500–8.
Sung KC, Ryu S, Sung JW, et al. Inflammation in the Prediction of Type 2 Diabetes and Hypertension in Healthy Adults. Arch Med Res. 2017;48(6):535–45.
Mattace-Raso FU, Verwoert GC, Hofman A, Witteman JC. Inflammation and incident-isolated systolic hypertension in older adults: the Rotterdam study. J Hypertens. 2010;28(5):892–5.
Dauphinot V, Roche F, Kossovsky MP, et al. C-reactive protein implications in new-onset hypertension in a healthy population initially aged 65 years: the Proof study. J Hypertens. 2009;27(4):736–43.
Savoia C, Schiffrin EL. Inflammation in hypertension. Curr Opin Nephrol Hypertens. 2006;15(2):152–8.
Speer H, D’Cunha NM, Naumovski N, McKune AJ. Sex, Age, BMI, and C-Reactive Protein Impact the Odds of Developing Hypertension-Findings Based on Data From the Health and Retirement Study (HRS). Am J Hypertens. 2021;34(10):1057–63.
Kansui Y, Matsumura K, Morinaga Y, et al. C-reactive protein and incident hypertension in a worksite population of Japanese men. J Clin Hypertens (Greenwich). 2019;21(4):524–32.
Ornstein SM, Nietert PJ, Jenkins RG, Litvin CB. The prevalence of chronic diseases and multimorbidity in primary care practice: a PPRNet report. Journal of the American Board of Family Medicine : JABFM. 2013;26(5):518–24.
Shin SH, Lee YJ, Lee YA, Kim JH, Lee SY, Shin CH. High-Sensitivity C-Reactive Protein Is Associated with Prediabetes and Adiposity in Korean Youth. Metab Syndr Relat Disord. 2020;18(1):47–55.
Mazidi M, Toth PP, Banach M. C-reactive Protein Is Associated With Prevalence of the Metabolic Syndrome, Hypertension, and Diabetes Mellitus in US Adults. Angiology. 2018;69(5):438–42.
Wilson AM, Ryan MC, Boyle AJ. The novel role of C-reactive protein in cardiovascular disease: risk marker or pathogen. Int J Cardiol. 2006;106(3):291–7.
Ciobanu DM, Mircea PA, Bala C, Rusu A, Vesa Ş, Roman G. Intercellular adhesion molecule-1 (ICAM-1) associates with 24-hour ambulatory blood pressure variability in type 2 diabetes and controls. Cytokine. 2019;116:134–8.
Sproston NR, Ashworth JJ. Role of C-Reactive Protein at Sites of Inflammation and Infection. Front Immunol. 2018;9:754.
Dai W, Zhang Z, Zhao S. Baseline levels of serum high sensitivity C reactive protein and lipids in predicting the residual risk of cardiovascular events in Chinese population with stable coronary artery disease: a prospective cohort study. Lipids Health Dis. 2018;17(1):273.
Libby P. Inflammation in atherosclerosis. Nature. 2002;420(6917):868–74.
Bassuk SS, Manson JE. Epidemiological evidence for the role of physical activity in reducing risk of type 2 diabetes and cardiovascular disease. J Appl Physiol (1985). 2005;99(3):1193–204.
Pfützner A, Standl E, Strotmann HJ, et al. Association of high-sensitive C-reactive protein with advanced stage beta-cell dysfunction and insulin resistance in patients with type 2 diabetes mellitus. Clin Chem Lab Med. 2006;44(5):556–60.
Kay J, Morgacheva O, Messing SP, et al. Clinical disease activity and acute phase reactant levels are discordant among patients with active rheumatoid arthritis: acute phase reactant levels contribute separately to predicting outcome at one year. Arthritis Res Ther. 2014;16(1):R40.
Sokka T, Pincus T. Erythrocyte sedimentation rate, C-reactive protein, or rheumatoid factor are normal at presentation in 35%-45% of patients with rheumatoid arthritis seen between 1980 and 2004: analyses from Finland and the United States. J Rheumatol. 2009;36(7):1387–90.
Hotamisligil GS. Inflammatory pathways and insulin action. International journal of obesity and related metabolic disorders : journal of the International Association for the Study of Obesity. 2003;27(Suppl 3):S53-55.
Kawai T, Autieri MV, Scalia R. Adipose tissue inflammation and metabolic dysfunction in obesity. Am J Physiol Cell Physiol. 2021;320(3):C375-c391.
Rajagopalan S, Zannad F, Radauceanu A, et al. Effects of valsartan alone versus valsartan/simvastatin combination on ambulatory blood pressure, C-reactive protein, lipoproteins, and monocyte chemoattractant protein-1 in patients with hyperlipidemia and hypertension. Am J Cardiol. 2007;100(2):222–6.
Albert MA, Glynn RJ, Ridker PM. Alcohol consumption and plasma concentration of C-reactive protein. Circulation. 2003;107(3):443–7.
Xu SJ, Jiang CQ, Zhang WS, et al. Alcohol sensitivity, alcohol use and high-sensitivity C-reactive protein in older Chinese men: The Guangzhou Biobank Cohort Study. Alcohol (Fayetteville, NY). 2016;57:41–8.
Acknowledgements
Not applicable.
Funding
This work was supported by National Natural Science Foundation of China (81370316) and (81601858).
Author information
Authors and Affiliations
Contributions
Le He conceived the idea of the manuscript. Le He conducted the analysis and wrote the initial draft of the paper. Chenyang Fan provided important suggestions and ideas. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All methods used in our study comply with the relevant guidelines and regulations, and the study was approved by the Ethics Committee of Hebei General Hospital. However, all subjects signed an informed consent before participation. Results were delivered to participants, and counseling was given depending on diagnosis during evaluation.
Consent for publication
Not applicable.
Competing interests
The authors declare no confict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
He, L., Fan, C. & Li, G. The relationship between serum C-reactive protein and senile hypertension. BMC Cardiovasc Disord 22, 500 (2022). https://doi.org/10.1186/s12872-022-02948-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-022-02948-4