Abstract
Introduction
Hyponatremia is a common electrolyte abnormality that has been associated with poor outcomes in several conditions including acute myocardial infarction (AMI). However, those studies were performed in the era before percutaneous coronary intervention (PCI), focused mostly on ST-elevation myocardial infarction (STEMI), and sodium levels up to 72 h of admission. The purpose of this study was to identify the association between hyponatremia and clinical outcomes in patients with acute myocardial infarction.
Methods
We performed a retrospective analysis of patients with a diagnosis of non-ST-elevation myocardial infarction (NSTEMI) and STEMI presenting at our institution from March 2021 to September 2021. Our independent variables were sodium levels on the day of admission and up to 7 days later. Dependent variables were in-hospital mortality, 30-day mortality, length of hospital stay, intensive care admission, new heart failure diagnosis, and ejection fraction.
Results
50.2% of patients had hyponatremia up to 7 days of admission. Intensive care admission was higher in patients with hyponatremia up to7 days (69.7% vs 54.3%, P 0.019, OR 1.9), they had worse 30-day mortality (12.7% vs to 2.2%, P 0.004, OR 6.5), in hospital mortality (9.9% vs 1.1%, P 0.006, OR 9.9), and new heart failure diagnosis (31.5% vs 17.9%, P < 0.043, OR 2.1). Hyponatremia on admission was associated with in-hopital mortality (16.3% vs 3.8%, P 0.004, OR 4.9), 30-day mortality (18.4% vs 5.9%, P 0.017, OR 3.5).
Conclusions
This study suggests that hyponatremia on admission and at any point during the first seven days of hospitalization are associated with in-hospital and 30-day mortality.
Similar content being viewed by others
Introduction
Approximately 805,000 people in the United States have an event of AMI every year [1]. In the past, studies have attempted to assess various prognosticating factors in this patient population. Dysnatremias especially hyponatremia is regarded as the most common electrolyte abnormality seen in the hospital [2] and is a useful marker of water excess in the body [3]. Hyponatremia has been associated with increased mortality in patients with several cardiovascular conditions including heart failure [4,5,6].
Although the association between hyponatremia in patients with AMI with mortality and heart failure has been previously described [7,8,9,10]; most of the studies were focused on hyponatremia up to 72 h of admission, patients with STEMI, and were performed in the era before PCI. The cause for hyponatremia in patients with AMI has not been elucidated. It is likely a multifactorial phenomenon involving the sympathetic system, renin–angiotensin–aldosterone cascade, and vasopressin release [11, 12]. The effect of hyponatremia on cardiac function in this patient population remains unclear. It is hypothesized that low sodium levels may lead to downregulation of calcium channels in the myocyte leading to decreased contractility [13].
The purpose of this study was to identify the association between hyponatremia and clinical outcomes in patients with acute myocardial infarction.
Methods
Study design
We performed a single-center, cross-sectional, observational study of patients presenting to Upstate Medical University (Syracuse, NY). All patient hospital data was obtained utilizing the Slicer Dicer tool from EPIC®. This study was determined to be exempt from Institutional Review Board (IRB) by the Upstate Medical university IRB (ID: 1825224-1).
Study population and criteria for inclusion and exclusion
We included all patients 18 to 89 years old with ICD-10 and ICD-9 corresponding to STEMI or NSTEMI diagnosis from March 2021 to September 2021 at Upstate Medical University. Upon electronic medical record revision, the diagnosis of STEMI or NSTEMI was confirmed. Patients were excluded if there was no sodium level on admission, they were younger than 18 years old, and if they were older than 89 years old. The sodium level was corrected for hyperglycemia using the formula proposed by Hillier et al., corrected sodium = [Measured sodium + 2.4 * (Serum glucose − 100)]/100 [14].
Independent and dependent variable assessment
We aimed to identify the association between hyponatremia present on admission and up to 7 days of hospitalization in patients diagnosed with STEMI and NSTEMI to new heart failure development, length of hospital stay, intensive care admission, depressed ejection fraction, in-hospital mortality, and 30-day mortality.
Sodium levels included in the study were the first sodium level drawn at the hospital and the lowest sodium level during the first 7 days of hospitalization. The calculated ejection fraction from echocardiograms done during hospitalization was used, in case more than one echocardiogram had been performed the last measurement was used.
The independent variables were hyponatremia on admission (defined as sodium level < 135 mmol/L during the first blood test drawn in our hospital) and hyponatremia (sodium level < 135 mmol/L) present at any point during the first seven days of hospitalization. Delta sodium (∆Na) was defined as the difference between sodium on admission and the lowest sodium up to 7 days of hospitalization.
Our dependent variables were in-hospital mortality, 30-day mortality, length of hospital stay, intensive care admission, new heart failure diagnosis, and ejection fraction. 30-day-all-cause-mortality was defined as death for any reason up to 30 days from the moment of hospital admission.
Baseline covariates
We collected and analyzed age, smoking status, sex, past medical history including hypertension, diabetes, transient ischemic attack, peripheral vascular disease, cancer, heart failure, myocardial infarction, chronic kidney disease, previous percutaneous coronary intervention, and coronary artery bypass graft, as well as the use of diuretics ACEi, ARB, or ARNi to address and minimize confounding effects and frailty bias.
Statistical analysis
For this study, we present categorical variables as percentages and continuous variables as means (SD) for normally distributed data and median with interquartile range (IQR) for non-normally distributed data. A P value of ≤ 0.05 was considered statistically significant.
Baseline characteristics were analyzed using descriptive statistics. The statistical tools used to analyze categorical data were Fisher’s exact test, odds ratio (95% confidence interval (CI)), and logistic regression analysis with backward elimination. A P value of ≤ 0.05 was considered statistically significant. For continuous data, the Kolmogorov–Smirnov test was done to determine normality. If the data was found to be normally distributed, a t-test was utilized to determine if there was a significant P-value. For non-normally distributed data, Mann–Whitney U-test was done to evaluate for a significant P-value.
The variables initially entered for multivariate logistic regression analysis were age, sex, smoking status, past medical history including hypertension, diabetes, transient ischemic attack, peripheral vascular disease, cancer, heart failure, myocardial infarction, chronic kidney disease, previous percutaneous coronary intervention, and coronary artery bypass graft, as well as the use of diuretics, ACEi, ARB, or ARNi. All statistical analysis was performed using the IBM® SPSS® software version 28.0.
Results
Baseline characteristics
A total of 234 patients were included, of which 44.4% were females. The mean age was 64.86 years. 20.9% of the patients had hyponatremia on admission. Of the 185 patients who did not have hyponatremia on admission, 50.2% developed hyponatremia at some point during the first seven days of hospitalization. Baseline characteristics grouped by the presence of hyponatremia can be seen in Tables 1 and 2.
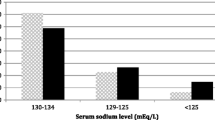
Hyponatremia was present on admission in 20.9% of the patients and 60.7% had hyponatremia during the first seven days of hospitalization. The median sodium level on admission was 137 mmol/L (IQR 135–140 mmol/L). The median sodium nadir during the first seven days of hospitalization was 133 mmol/L (IQR 130–136 mmol/L) (Table 2).
There was no significant difference for most of the baseline characteristics between patients presenting hyponatremia versus those who did not, except for patients with a history of diabetes mellitus (Table 1).
Outcomes
The median length of hospital stay was 4 days. Patients with hyponatremia on admission had a similar length of hospital stay compared to those without and were found to be similar on non-parametric tests (Table 3). In contrast, patients who had hyponatremia during the first seven days of hospitalization had a median length of hospital stay of 3 days (IQR 2–5) compared to 5 days (IQR 2–10) in the normonatremic group (Table 4).
In-hospital mortality was seen in 6.4% and 30-day mortality in 8.5% of our patients. In bivariate analysis, in-hospital mortality was seen in 9.9% compared to 1.1%, OR 9.95 (P 0.006) in those who had hyponatremia during the first 7 days of admission versus those without. Patients who had hyponatremia on admission also had a significant association with in-hospital mortality of 16.3% versus 3.78%, OR 4.9 (P 0.004) (Table 6).
30-day mortality was higher in patients with hyponatremia during the first 7 days of admission 12.7% versus 2.2%, OR 6.5 (P 0.004) (Table 5). In-hospital mortality was also associated with hyponatremia on admission 16.3% versus 3.8%, OR 3.5 (P 0.004) (Table 6).
Both hyponatremia on admission and during the first 7 days of admission was significantly associated with mortality even when depressed ejection fraction and heart failure diagnosis were included in logistic regression analysis.
Intensive care admission was higher in patients with hyponatremia up to 7 days of admission (69.7% vs 54.3%, OR 1.9, P 0.019). This association was not seen in patients with hyponatremia on admission only.
New heart failure diagnosis was not significantly associated with hyponatremia on admission. However, it was associated with patients that had hyponatremia during the first 7 days of hospitalization (31.5%. vs 17.9%, OR 2.1, P 0.043). Depressed ejection fraction was higher in those with hyponatremia during the first 7 days of hospitalization (50.7% vs 28.9%, P 0.002, OR 2.531) (Table 5). Both hyponatremia on admission and during the first seven days of hospitalization were significantly associated with lower left ventricular ejection fraction (Tables 3 and 4).
The median ∆Na was 3 with an IQR of 0 to 7. We did not find an association between ∆Na and any of the studied outcomes.
Discussion
Hyponatremia during the first seven days of hospitalization was seen in more than half the patients with AMI and was associated with poorer outcomes including 30-day and in-hospital mortality, ICU or CCU admission, new heart failure diagnosis, and depressed EF. Hyponatremia on admission was also associated with poorer outcomes. However, there was no significant association between ICU or CCU admission as well as new heart failure diagnosis.
Several studies have shown an association between hyponatremia up to 72 h of admission with short- and long-term mortality in patients with AMI [7, 8, 15]. More recently there has been conflicting evidence in patients with STEMI receiving percutaneous coronary intervention prompting the hypothesis that hyponatremia is a marker of disease severity and not an independent predictor of mortality [9]. This conflicting evidence could be, at least in part, explained by advances in PCI and medical therapy. Although less studied, NSTEMI also has been associated with short-term mortality [8, 15], but since these studies were performed before the PCI era. We found a significant association between hyponatremia on admission and up to 7 days of hospitalization with in-hospital and 30-day mortality. Although previous studies have demonstrated that hyponatremia conveys a worse prognosis in patients with heart failure [5, 6]. In those patients, correction of hyponatremia fails to improve mortality [6]. In patients with AMI, correction of hyponatremia might not have any mortality benefits as well [8].
Hyponatremia for up to 7 days was associated with new heart failure diagnosis. Other studies have reported an association between STEMI and heart failure in up to 30.2% of the patients [7, 10]. Qureshi et al. reported a higher prevalence of heart failure in patients with STEMI and NSTEMI that had persistent hyponatremia (6.4% and 14.3%) and hyponatremia only on admission (5.2% and 3.8%) compared to those without hyponatremia (1.8% and 2.1%). They found that patients with hyponatremia on admission had an increased risk of 30-day rehospitalization due to heart failure regardless of whether the sodium was corrected or not, it is important to highlight that in this study, 20.4% of patients underwent revascularization [8], compared to 42.7% in ours. In our study, hyponatremia on admission was not associated with heart failure, but it was significantly associated with hyponatremia up to 7 days of admission. A possible explanation for this finding is that hyponatremia might take some time to develop in patients with new-onset or acutely decompensated heart failure.
Although patients with hyponatremia appeared to have a more severe condition as evidenced by the higher admissions to ICU or CCU and lower EF% on echocardiograms. We did not find a statistically significant association with mortality between the levels of peak troponin and hyponatremia; our study may be underpowered to find this association. Further studies would be needed to discover if hyponatremia is also related to the size of myocardial involvement in patients with AMI.
The association between hyponatremia and mortality was significant even after accounting for depressed ejection fraction, heart failure diagnosis, and in-patient use of diuretics in the regression analysis. This could indicate that hyponatremia in patients with AMI is more than only a marker of heart failure in these patients.
Limitations of the study
This was a retrospective, single site, observational analysis that had a relatively small number of patients, thus it may have been underpowered to find certain differences. There might be other confounding factors that we did not take into consideration. Other causes of hyponatremia and BNP or NT-ProBNP levels might have a significant association with poorer outcomes, but this was not analyzed in the study.
Conclusions
This study suggests that hyponatremia on admission and at any point during the first seven days of hospitalization are associated with in-hospital and 30-day mortality.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its supplementary information files.
References
Fryar CD, Chen TC, Li X. Prevalence of uncontrolled risk factors for cardiovascular disease: United States, 1999–2010. NCHS Data Brief. 2012;103:1–8.
Anderson RJ, Chung HM, Kluge R, Schrier RW. Hyponatremia: a prospective analysis of its epidemiology and the pathogenetic role of vasopressin. Ann Intern Med. 1985;102(2):164–8. https://doi.org/10.7326/0003-4819-102-2-164 (PMID: 3966753).
Hoorn EJ, Zietse R. Hyponatremia revisited: translating physiology to practice. Nephron Physiol. 2008;108(3):p46–59. https://doi.org/10.1159/000119709.
Breen T, Brueske B, Sidhu MS, et al. Abnormal serum sodium is associated with increased mortality among unselected cardiac intensive care unit patients. J Am Heart Assoc. 2020;9(2): e014140. https://doi.org/10.1161/JAHA.119.014140.
Gheorghiade M, Abraham WT, Albert NM, et al. Relationship between admission serum sodium concentration and clinical outcomes in patients hospitalized for heart failure: an analysis from the OPTIMIZE-HF registry. Eur Heart J. 2007;28(8):980–8. https://doi.org/10.1093/eurheartj/ehl542.
Lee SE, Choi DJ, Yoon CH, et al. Improvement of hyponatraemia during hospitalisation for acute heart failure is not associated with improvement of prognosis: an analysis from the Korean Heart Failure (KorHF) registry. Heart. 2012;98(24):1798–804. https://doi.org/10.1136/heartjnl-2012-302334.
Goldberg A, Hammerman H, Petcherski S, et al. Prognostic importance of hyponatremia in acute ST-elevation myocardial infarction. Am J Med. 2004;117(4):242–8. https://doi.org/10.1016/j.amjmed.2004.03.022.
Qureshi W, Hassan S, Khalid F, et al. Outcomes of correcting hyponatremia in patients with myocardial infarction. Clin Res Cardiol. 2013;102(9):637–44. https://doi.org/10.1007/s00392-013-0576-z.
Lazzeri C, Valente S, Chiostri M, Attanà P, Picariello C, Gensini GF. Usefulness of hyponatremia in the acute phase of ST-elevation myocardial infarction as a marker of severity. Am J Cardiol. 2012;110(10):1419–24. https://doi.org/10.1016/j.amjcard.2012.07.004.
Tada Y, Nakamura T, Funayama H, et al. Early development of hyponatremia implicates short- and long-term outcomes in ST-elevation acute myocardial infarction. Circ J. 2011;75(8):1927–33. https://doi.org/10.1253/circj.cj-10-0945.
Palmer BR, Pilbrow AP, Frampton CM, et al. Plasma aldosterone levels during hospitalization are predictive of survival post-myocardial infarction [published correction appears in Eur Heart J. 2008;29(24):3068]. Eur Heart J. 2008;29(20):2489–96. https://doi.org/10.1093/eurheartj/ehn383.
Latini R, Masson S, Anand I, et al. The comparative prognostic value of plasma neurohormones at baseline in patients with heart failure enrolled in Val-HeFT. Eur Heart J. 2004;25(4):292–9. https://doi.org/10.1016/j.ehj.2003.10.030.
Movafagh S, Cleemann L, Morad M. Regulation of cardiac Ca(2+) channel by extracellular Na(+). Cell Calcium. 2011;49(3):162–73. https://doi.org/10.1016/j.ceca.2011.01.008.
Hillier TA, Abbott RD, Barrett EJ. Hyponatremia: evaluating the correction factor for hyperglycemia. Am J Med. 1999;106(4):399–403. https://doi.org/10.1016/s0002-9343(99)00055-8.
Singla I, Zahid M, Good CB, Macioce A, Sonel AF. Effect of hyponatremia (<135 mEq/L) on outcome in patients with the non-ST-elevation acute coronary syndrome. Am J Cardiol. 2007;100(3):406–8. https://doi.org/10.1016/j.amjcard.2007.03.039.
Acknowledgements
None.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
ACS: Analyzing data, conceptualizing, and writing the original draft. GS: Data gathering, analyzing data, writing the original draft. KB: Conceptualizing and writing the original draft. NA: Data gathering, writing the original draft. RM: Data gathering, writing the original draft. DC: Supervision, conceptualize, and review the original draft. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was determined to be exempt from Institutional Review Board (IRB) by the Upstate Medical university IRB (ID: 1825224-1). The need for written informed consent was waived by the SUNY Upstate IRB committee. All methods were performed in accordance with the relevant guidelines and regulations of the approved protocol.
Consent for publication
Nor applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Regression and sensitivity analysis.
Additional file 2.
Regression and sensitivity analysis cont'd.
Additional file 3.
Data.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cordova Sanchez, A., Bhuta, K., Shmorgon, G. et al. The association of hyponatremia and clinical outcomes in patients with acute myocardial infarction: a cross-sectional study. BMC Cardiovasc Disord 22, 276 (2022). https://doi.org/10.1186/s12872-022-02700-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-022-02700-y