Abstract
Background
Pulmonary hypertension in left heart disease (PH-LHD), which includes combined post- and precapillary PH (Cpc-PH) and isolated postcapillary PH (Ipc-PH), differs significantly in prognosis. We aimed to assess whether cardiopulmonary exercise testing (CPET) predicts the long-term survival of patients with PH-LHD.
Methods
A single-center observational cohort enrolled 89 patients with PH-LHD who had undergone right heart catherization and CPET (mean pulmonary arterial pressure > 20 mm Hg and pulmonary artery wedge pressure ≥ 15 mm Hg) between 2013 and 2021. A receiver operating characteristic curve was plotted to determine the cutoff value of all-cause death. Survival was estimated using the Kaplan–Meier method and analyzed using the log-rank test. The Cox proportional hazards model was performed to determine the association between CPET and all-cause death.
Results
Seventeen patients died within a mean of 2.2 ± 1.3 years. Compared with survivors, nonsurvivors displayed a significantly worse 6-min walk distance, workload, exercise time and peak oxygen consumption (VO2)/kg with a trend of a lower oxygen uptake efficiency slope (OUES) adjusted by Bonferroni’s correction. Multivariate Cox regression revealed that the peak VO2/kg was significantly associated with all-cause death after adjusting for Cpc-PH/Ipc-PH. Compared with Cpc-PH patients with a peak VO2/kg ≥ 10.7 ml kg−1 min−1, Ipc-PH patients with a peak VO2/kg < 10.7 ml kg−1 min−1 had a worse survival (P < 0.001).
Conclusions
The peak VO2/kg is independently associated with all-cause death in patients with PH-LHD. The peak VO2/kg can also be analyzed together with Cpc-PH/Ipc-PH to better indicate the prognosis of patients with PH-LHD.
Similar content being viewed by others
Introduction
Pulmonary hypertension (PH) due to left heart disease (LHD) is a major problem in patients with heart failure (HF) and the most common type of PH [1, 2]. The presence of PH suggests a poor prognosis and exercise capacity in patients with HF [1, 3] and LHD [4]. Recent studies have shown no treatment benefit in this population[2, 5]. PH-LHD is divided into combined post- and precapillary PH (Cpc-PH) and isolated postcapillary PH (Ipc-PH). Cpc-PH indicates the presence of precapillary components, which are associated with increased mortality [1]. The two subgroups are usually distinguished by several hemodynamic variables detected by a right heart catheterization (RHC). These variables include the transpulmonary gradient (TPG), pulmonary vascular resistance (PVR), and diastolic pressure gradient (DPG). Based on current guidelines in this field, PH-LHD defined as the mean pulmonary artery pressure (mPAP) > 20 mmHg and pulmonary artery wedge pressure (PAWP) > 15 mmHg at rest. Ipc-PH and Cpc-PH can be distinguished based on the PVR, Cpc-PH is characterized by an increased PVR of ≥ 3 WU [5].
Considering its invasiveness and the possibility of data distortion, RHC alone will likely be insufficient to assess PH-LHD patients [2]. In addition to RHC, other noninvasive techniques may be required in patients with PH-LHD. Modern CPET systems allow the analysis of gas exchange throughout exercise. An important practical significance of CPET is that it provides data concerning outcome prediction [6], which has usually been used to predict the severity and progression of HF [7]. The peak oxygen consumption (VO2) is the most well-established variable of CPET and has been considered a significant predictor of death in patients with HF [8]. A comprehensive analysis of the peak VO2, carbon dioxide output (VCO2), and ventilation (VE) is helpful to accurately predict the mortality of HF patients [9, 10].
PH-LHD is related to decreased exercise tolerance, and the degree of exercise impairment is directly correlated with disease severity [11]. However, CPET has not been widely used in clinical practice with PH-LHD, primarily due to poor knowledge of its potential and evidence. In the present study, we aimed to investigate whether the modified diagnostic criteria of hemodynamics for Ipc-PH and Cpc-PH were related to clinical outcomes, to study the incremental prognostic information provided by CPET, to estimate the prognostic value of these indices and to identify reliable prognostic factors for PH-LHD.
We present the following article in accordance with the STROBE reporting checklist.
Methods
Study design and patient population
We reviewed incident patients with suspected PH associated with LHD referred to our center between July 2013 and May 2020. Finally, 89 patients underwent CPET and RHC for hemodynamic evaluation were included. And all patients were followed up to January 31, 2021. The clinical characteristics and hemodynamic and CPET data were obtained during routine clinical care and were collected from hospital records. Demographic variables such as sex, age, body mass index, World Health Organization functional class (WHO FC), N-terminal pro-B type natriuretic peptide (NT-proBNP) and 6-min walk distance (6MWD) were obtained at baseline.
The patient inclusion criteria were as follows: (1) a diagnosis of LHD confirmed by experienced specialists according to the appropriate guidelines [5], including heart failure with a preserved left ventricular ejection fraction (LVEF) (HFpEF), heart failure with a reduced LVEF (HFrEF), valvular heart disease (VHD) and congenital/acquired cardiovascular conditions leading to postcapillary PH [5]; (2) After adequate medical treatment such as cardiotonic diuresis. RHC and CPET were performed (within one week) when patients were stable at not-acute decompensation period; and 3) PH-LHD defined as mPAP > 20 mmHg and PAWP > 15 mmHg at rest [7, 12]. Furthermore, PH-LHD was classified as Cpc-PH and Ipc-PH defined by PVR ≥ 3 Wood units (WU) and PVR < 3 WU, respectively [7, 12].
Patients were excluded for the following reasons: (1) a diagnosis of other PH groups as per the NICE criteria [13]; (2) no valid baseline CPET; (3) acute decompensated heart failure, severe cardiogenic shock requiring inotropic support or urgent mechanical circulatory support; (4) a lack of CPET or RHC; and (5) comorbidities such as severe chronic lung diseases and pulmonary embolism.
The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Ethics Committee of Shanghai Pulmonary Hospital approved the protocol (K16-317) and individual consent for this retrospective analysis was waived.
Procedures
Right heart catherization
RHC was performed as described previously using the Swan-Ganz catheter (7- or 7.5-Fr; Edwards Lifesciences LLC, Irvine, CA) [14]. The baseline hemodynamic variables evaluated included mPAP, right atrial pressure (RAP), PAWP, cardiac output (CO) and PVR. DPG = diastolic PAP—mean PAWP and TPG = mPAP—mean PAWP.
Cardiopulmonary exercise testing
CPET was performed using an electromagnetically braked cycle ergometer (Master Screen CPET, Jaeger Crop., Hoechberg, Germany), and gas exchange data were recorded over 10-s intervals via a breath-by-breath system. The protocol consisted of 3 min of rest, followed by 3 min of unloaded pedalling at 60 revolutions per minute, subsequently, a progressively increasing workload of 10–25 W/min to the maximum tolerance and finally 5 min of recovery. A test was terminated if any of the following conditions were observed: fatigue, dyspnea, chest tightness, or any other uncomfortable feeling reported by the patient. Measurements included the exercise time, workload, O2 consumption, oxygen pulse (O2 pulse), end-tidal partial pressure of CO2 (PET CO2), minute ventilation, carbon dioxide output, VE/VCO2, VO2/VE, oxygen uptake efficiency plateau (OUEP), and the oxygen uptake efficiency slope (OUES).
The VO2, PET CO2, VE/VCO2, VO2/VE, and O2 pulse values at peak exercise were measured according to the highest 30-s averaged value obtained during peak exercise. The lowest VE/VCO2 was calculated by averaging the 9 lowest consecutive 10-s-averaged data points of VE/VCO2. The VE/VCO2 slope was obtained from linear regression analysis of the relationship of VE with VCO2. The oxygen uptake efficiency plateau was at 90 s for the highest consecutive values of VO2 (ml/min)/VE (L/min) [15]. Using linear square regression, we computed the oxygen uptake efficiency slope according to the following equation: VO2 = a × lgVE + b (‘a’ is OUES) [15].
Outcome assessment
The primary outcome was all-cause death. All the patients were followed up until death or through January 31, 2021, whichever occurred first. Patients lost during follow-up were censored as alive on the last day of contact. We had an established PH database at our center. The data were obtained during follow-up or by telephone interview, and specific events were confirmed through medical records, death certificates or confirmation provided by immediate family members.
Statistical analysis
All the results were expressed as means ± SD or medians (and interquartile range) for continuous variables and as the absolute number for categorical variables. Comparisons in the two groups (survivors and nonsurvivors) were performed using independent-samples t-test and the Mann–Whitney U test for parametric and nonparametric data, respectively. Differences in categorical variables between groups were assessed using χ2 test. Comparisons in the four groups were performed using ANOVA and the Kruskal–Wallis test for parametric and nonparametric data, respectively.
The Cox proportional hazards model was performed to determine the associations between the clinical indices and survival with or without covariate adjustment. A receiver operating characteristic (ROC) curve was used to select the cutoff value for independent predictors with the maximum sensitivity and specificity. Correlations were assessed by Spearman’s correlation coefficient. The Kaplan–Meier method and log-rank test were used to perform survival analyses. The Bonferroni method for correcting the significance level for multiple comparisons was applied. For all analyses, statistical significance was indicated by a 2-sided P < 0.05. The data were analyzed using SPSS 19.0 (SPSS Inc., Chicago, IL, USA).
Results
Characteristics and hemodynamic parameters between nonsurvivors and survivors
A total of 89 eligible patients were included in this study, including 46 patients with Cpc-PH and 43 patients with Ipc-PH. The screening protocol is shown in Fig. 1. During a median follow-up of 3.0 (1.4, 4.2) years, all-cause mortality occurred in 17 (19.1%) patients. The follow-up rate was 95.5%. The patients had an average age of 64.0 (56.0, 72.5) years, and 35 patients (39.3%) were male. The demographics, baseline characteristics and hemodynamics were compared between survivors and nonsurvivors among the PH-LHD patients (Table 1). Significant differences were found between survivors and nonsurvivors regarding WHO-FC, 6MWD, NT-proBNP, renal function, PVR and DPG. However, when Bonferroni's correction of the significance level (P < 0.05) was applied, the adjusted significance level was 0.002. Compared with survivors, nonsurvivors walked a significantly shorter distance (P = 0.001).
Comparison of CPET between nonsurvivors and survivors
A significant difference was observed in the workload, peak O2 pulse, exercise time, peak VO2, lowest VE/VCO2, peak VE/VCO2, OUEP and OUES between nonsurvivors and survivors (Table 2). Regarding exercise capacity, nonsurvivors had a worse workload, exercise time and peak VO2 (the adjusted significance level was 0.004) after applying Bonferroni's correction of the significance level (P < 0.05). In terms of ventilatory and gas exchange efficiency, a trend was observed toward a lower OUES in nonsurvivors (P = 0.009).
Factors influencing survival
In the univariate Cox proportional hazards analysis (Table 3), age, 6MWD, Cpc-PH or Ipc-PH, exercise time, peak VO2/kg, lowest VE/VCO2, and OUES were significant predictors of death. Subsequently, all factors with a P value < 0.05 were included in the multivariate forward stepwise analysis, revealing that the peak VO2/kg was a significant independent predictor of all-cause death (hazard ratio: 0.487; 95% CI: 0.354–0.653; P < 0.001) after adjusting for Cpc-PH or Ipc-PH. The peak VO2/kg ≥ 10.7 ml kg−1·min−1 exhibited 76.4% sensitivity and 82.4% specificity with an area under the ROC curve of 0.8 (95% CI: 0.71 to 0.9; P < 0.001) (Fig. 2).
Correlation between CO, 6MWD, NT-proBNP and peak VO2/kg
As shown in Fig. 3, there was no significant correlation between peak VO2/kg and CO (r = 0.115, P = 0.282), peak VO2/kg was positively correlated with 6MWD (r = 0.507, P < 0.0001), and peak VO2/kg was negatively correlated with NT-proBNP (r = − 0.344, P = 0.001).
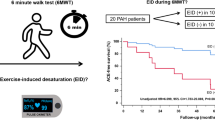
Kaplan–Meier survival analysis
Patients with a peak VO2/kg ≥ 10.7 ml kg−1·min−1 had a much better prognosis than those with a peak VO2/kg < 10.7 ml·kg−1 min−1 in PH-LHD patients (P < 0.0001) (Fig. 4A). Compared with Ipc-PH patients, Cpc-PH patients showed a worse survival (P < 0.05) (Fig. 4B). The prognosis of patients with a peak VO2/kg ≥ 10.7 ml kg−1 min−1 was better than that of those with a peak VO2/kg < 10.7 ml·kg−1 min−1 in Cpc-PH (P < 0.0001) (Fig. 4C). The prognosis of patients with a peak VO2/kg ≥ 10.7 ml kg−1 min−1 was better than that of patients with a peak VO2/kg < 10.7 ml·kg−1 min−1 in Ipc-PH (P = 0.001) (Fig. 4D). Additionally, hemodynamics and CPET parameters were significantly different among the above groups (Additional file 1: Table S1).
Kaplan–Meier analysis in PH-LHD, Cpc-PH and Ipc-PH patients stratified by peak VO2/kg. A Survival in PH-LHD patients between the peak VO2/kg ≥ 10.7 ml kg−1 min−1 and peak VO2/kg < 10.7 ml kg−1 min−1. B Survival in PH-LHD patients between Cpc-PH and Ipc-PH. C Survival in Cpc-PH patients between the peak VO2/kg ≥ 10.7 ml kg−1 min−1 and peak VO2/kg < 10.7 ml kg−1 min−1. D Survival in Ipc-PH patients between the peak VO2/kg ≥ 10.7 ml kg−1 min−1 and peak VO2/kg < 10.7 ml kg−1 min−1. Survival analyses were compared by the log-rank test. VO2, oxygen uptake; PH-LHD, pulmonary hypertension due to left heart disease; Cpc-PH, post- and precapillary pulmonary hypertension; Ipc-PH, isolated postcapillary pulmonary hypertension
Discussion
To our knowledge, there are few studies to explore the prosgnostic values of CPET for the mortality of patients with PH-LHD. For patients with PH-LHD, PVR is more significant to explain the prognosis based on peak VO2/kg. Our study demonstrated that the peak VO2/kg was independently associated with all-cause death in patients with PH-LHD. The peak VO2/kg can also be analyzed together with Cpc-PH/Ipc-PH, which can better indicate the prognosis of patients with PH-LHD. Nonsurvivors with PH-LHD had a worse 6MWD, workload, exercise and peak VO2/kg than survivors, revealing that PH-LHD patients with obvious exercise limitation had a poorer prognosis.
Although the current definition and classification of PH-LHD are based on hemodynamics, the application of hemodynamic parameters in prognostication is limited [16]. In addition to hemodynamic indices, other nonhemodynamic markers, including CPET profiles, can better determine the prognosis of patients with PH-LHD [5]. Further clinical studies are encouraged to better understand prognostic predictors. To the best of our knowledge, this study is the first to compare the invasive parameters of PH-LHD and CPET to study the predictors of mortality since the new standard was formulated in 2018 [16]. Significant differences were found in the CPET and hemodynamic parameters among the four groups according to the peak VO2/kg and Cpc-PH/Ipc-PH. Both the peak VO2/kg and Cpc-PH/Ipc-PH affected the prognosis, but the peak VO2/kg was better. The combination of the two could better predict the prognosis of patients with PH-LHD.
The presence of precapillary components in PH-LHD, defined as Cpc-PH, may consistently influence the prognosis [17]. However, using PVR alone to identify Cpc-PH, indicating the presence of precapillary components, remains controversial [5, 18]. Our previous study showed that DPG does not provide additional CPET information for patients with Cpc-PH beyond that provided by PVR [19], supporting those patients with Cpc-PH and Ipc-PH were differentiated according to PVR in the prognosis study of CPET. There have been conflicting results in the search for ideal prognostic indicators for patients with PH-LHD. PVR was considered to significantly, mildly or not predict the outcome in patients with PH-LHD [12, 16, 20, 21]. Our results showed that Cpc-PH with PVR ≥ 3 WU had a slight predictive effect on prognosis.
RHC plays an important role in distinguishing hemodynamic subtypes in patients with LHD, namely, Cpc-PH and Ipc-PH, but it is often inferior to CPET in accurately evaluating the functional status and prognostic information [22]. The data obtained from CPET have a recognized key role in the prognosis of HF [23], whether alone [24] or combined with non-CPET parameters [9, 25]. The application of an optimal CPET response in the risk stratification of mortality or other outcomes in patients with HF is controversial [26]. The peak VO2 describes the existence of functional impairment, its absolute value is used to grade the severity of exercise limitation in cardiac disease patients [22], and it is a well-established prognostic indicator in patients with HF. Some studies have shown that the VE/VCO2 relationship is a stronger predictor of mortality than the peak VO2 [9, 27,28,29]. In this study, we demonstrated that ventilatory and gas exchange CPET parameters predict survival in patients with PH-LHD. The more prognostic parameter is the VE/VCO2 rather than other parameters of ventilatory impairment. Different from the study of Mayer et al. [30], lowest VE/VCO2 was more meaningful than VE/VCO2 slope, but the VE/VCO2 related parameters were not as good as peak VO2. Among all CPET parameters, the peak VO2 was the best parameter to predict the death of patients with PH-LHD. This finding was similar to that reported in the HF population [31]. To our knowledge, few studies have explored the prognostic significance of the peak VO2 in invasively characterized PH-LHD. The peak VO2 is a broader marker of the severity and prognosis of heart and lung diseases.
Although peak VO2 has been studied for HF, no study has evaluated the impact of peak VO2 on the prognosis of Cpc-PH and Ipc-PH. In our study, there was no significant correlation between peak VO2 and cardiac output, but it was correlated with 6MWD and NT-proBNP, which indirectly supported that the decrease of peak VO2 in PH-LHD reflected more a general condition than simple hemodynamic disorder. Exercise capacity, whether assessed during CPET or walking tests (peak VO2 or 6MWD, respectively), is a recognized predictor of survival in HF and PAH [32]. The 6MWD contains important prognostic information [22, 33], similar to our results. Some studies have also shown that the 6MWD had only weak and nonsignificant prognostic power [34]. Groepenhoff et al.[32] found that the prognostic information of the 6MWD was better than that of the peak VO2 in PH patients, contrasting our results.
CPET parameters have become a new prognostic tool for PAH patients. Additionally, CPET provides a comprehensive pathophysiological assessment of patients with exercise restriction and dyspnea and is recommended for all patients with clinically stable PH [22]. In PAH patients, the peak VO2 and PVR are powerful independent prognostic indicators, and their combination can obtain the best risk stratification [34]. These different methods may be complementary in the risk stratification of PAH patients. Similarities and differences are observed among different types of PH. Our results also showed that the combination of the peak VO2 and Cpc-PH/Ipc-PH could better distinguish the significance of CPET and hemodynamic parameters and predict the prognosis. The peak VO2 is an independent and strong predictor of survival in PH-LHD patients. Cpc-PH/Ipc-PH, although also an accurate predictor, provides no independent prognostic information. This finding is similar to previous study findings on primary pulmonary hypertension, although the hemodynamic parameters are different [35]. Regardless of Ipc-PH or Cpc-PH, all PH-LHD patients with a peak VO2 < 10.7 ml·kg−1·min−1 at baseline had a higher risk of death. The peak VO2/kg < 10.7 ml·kg−1·min−1 is stronger than PVR ≥ 3WU in predicting prognosis, likely increasing the controversy of PVR alone. We suspect that mortality of PH-LHD is not only determined by hemodynamic factors caused by pulmonary hypertension, but also by the basic physical condition of patients. Peak VO2 is only an overall indicator of this pathophysiological state. Therefore, it is expected that the peak VO2 in PH-LHD is stronger than PVR in predicting the prognosis of PH-LHD.
Our study confirms that nonsurvivors of PH-LHD show a significantly decreased exercise capacity. Cpc-PH patients have a worse outcome than Ipc-PH patients. In our patient population, the prognostic value of the peak VO2 was better than that of the Cpc-PH/Ipc-PH, 6MWD and other CPET parameters. Our study suggests that hemodynamic variables need to be combined with assessment of cardiopulmonary exercise capacity when trying to determine individual risk in patients with PH-LHD.
Our study has some limitations. First, the prognostic effects of the peak VO2 and other CPET parameters were evaluated only once during the trial run. We did not evaluate any possible treatment changes during the follow-up or considered the impact of repeated CPET on the prognosis. Second, this study was performed at a single-center with a limited sample size, which may have provided less relevant evidence than a large sample and multicenter clinical research. Third, the retrospective design had selection bias, and this could have possibly led to a bias. The results of our study could have been influenced by the following selection bias. First of all, among the patients we excluded who did not undergo RHC, some refused invasive examination for fear or because echocardiography results were nearly normal after treatment. Others were too ill or old for invasive examination. For these patients with worse cardiopulmonary ability, our results may be overestimated. Secondly, among patients with other diseases excluded, such as severe lung diseases, these complications worsen patients' cardiopulmonary capacity, so our results may be overestimated. Finally, among the excluded patients without CPET or qualified CPET, they had the same standardized diagnosis and treatment procedure as the included patients. They may have similar age and sex distributions, with little possibility of selection bias. Prospective investigations of a large number of patients in the future will allow extensive and powerful multivariate analysis. Finally, we enrolled few patients with HFrEF in the present study, possibly leading to a survival bias.
Conclusions
The peak VO2/kg is independently associated with all-cause death in patients with PH-LHD. The peak VO2/kg can also be analyzed together with Cpc-PH/Ipc-PH to better indicate the prognosis of patients with PH-LHD.
Availability of data and materials
The data underlying this article will be shared on reasonable request to the corresponding author.
Abbreviations
- PH:
-
Pulmonary hypertension
- LHD:
-
Left heart disease (−)
- Cpc-PH:
-
Combined post- and precapillary PH
- Ipc-PH:
-
Isolated postcapillary PH
- CPET:
-
Cardiopulmonary exercise testing
- VO2 :
-
Oxygen consumption
- OUES:
-
Oxygen uptake efficiency slope
- HF:
-
Heart failure
- RHC:
-
Right heart catheterization
- TPG:
-
Transpulmonary gradient
- PVR:
-
Pulmonary vascular resistance
- DPG:
-
Diastolic pressure gradient
- mPAP:
-
Mean pulmonary artery pressure
- PAWP:
-
Pulmonary artery wedge pressure
- VCO2 :
-
Carbon dioxide output
- VE:
-
Ventilation
- WHO FC:
-
World Health Organization functional class
- NT-proBNP:
-
N-terminal pro-B type natriuretic peptide
- 6MWD:
-
6-Minute walk distance
- LVEF:
-
Left ventricular ejection fraction
- HFpEF:
-
Preserved LVEF
- HFrEF:
-
Reduced LVEF
- VHD:
-
Valvular heart disease
- WU:
-
Wood units
- RAP:
-
Right atrial pressure
- CO:
-
Cardiac output
- PET CO2 :
-
End-tidal partial pressure of CO2
- OUEP:
-
Oxygen uptake efficiency plateau
- ROC:
-
Receiver operating characteristic
References
Rosenkranz S, Gibbs JS, Wachter R, De Marco T, Vonk-Noordegraaf A, Vachiery JL. Left ventricular heart failure and pulmonary hypertension. Eur Heart J. 2016;37(12):942–54.
Al-Omary MS, Sugito S, Boyle AJ, Sverdlov AL, Collins NJ. Pulmonary hypertension due to left heart disease: diagnosis, pathophysiology, and therapy. Hypertension. 2020;75(6):1397–408.
Damy T, Goode KM, Kallvikbacka-Bennett A, Lewinter C, Hobkirk J, Nikitin NP, et al. Determinants and prognostic value of pulmonary arterial pressure in patients with chronic heart failure. Eur Heart J. 2010;31(18):2280–90.
Lee F, Mielniczuk LM. Pulmonary hypertension due to left heart disease: a practical approach to diagnosis and management. Can J Cardiol. 2020.
Vachiery JL, Tedford RJ, Rosenkranz S, Palazzini M, Lang I, Guazzi M, et al. Pulmonary hypertension due to left heart disease. Eur Respir J. 2019;53(1):1801897.
Tang Y, Yao L, Liu Z, Xie W, Ma X, Luo Q, et al. Peak circulatory power is a strong prognostic factor in patients with idiopathic pulmonary arterial hypertension. Respir Med. 2018;135:29–34.
Guazzi M, Arena R, Halle M, Piepoli MF, Myers J, Lavie CJ. 2016 Focused update: clinical recommendations for cardiopulmonary exercise testing data assessment in specific patient populations. Circulation. 2016;133(24):e694-711.
O’Neill JO, Young JB, Pothier CE, Lauer MS. Peak oxygen consumption as a predictor of death in patients with heart failure receiving beta-blockers. Circulation. 2005;111(18):2313–8.
Levy WC, Arena R, Wagoner LE, Dardas T, Abraham WT. Prognostic impact of the addition of ventilatory efficiency to the Seattle heart failure model in patients with heart failure. J Card Fail. 2012;18(8):614–9.
Myers J, Arena R, Dewey F, Bensimhon D, Abella J, Hsu L, et al. A cardiopulmonary exercise testing score for predicting outcomes in patients with heart failure. Am Heart J. 2008;156(6):1177–83.
Rao SD, Menachem JN, Birati EY, Mazurek JA. Pulmonary hypertension in advanced heart failure: assessment and management of the failing RV and LV. Curr Heart Fail Rep. 2019;16(5):119–29.
Palazzini M, Dardi F, Manes A, Bacchi Reggiani ML, Gotti E, Rinaldi A, et al. Pulmonary hypertension due to left heart disease: analysis of survival according to the haemodynamic classification of the 2015 ESC/ERS guidelines and insights for future changes. Eur J Heart Fail. 2018;20(2):248–55.
Simonneau G, Gatzoulis MA, Adatia I, Celermajer D, Denton C, Ghofrani A, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2013;62(25 Suppl):D34-41.
Jiang R, Ai ZS, Jiang X, Yuan P, Liu D, Zhao QH, et al. Intravenous fasudil improves in-hospital mortality of patients with right heart failure in severe pulmonary hypertension. Hypertens Res. 2015;38(8):539–44.
Tan X, Yang W, Guo J, Zhang Y, Wu C, Sapkota R, et al. Usefulness of decrease in oxygen uptake efficiency to identify gas exchange abnormality in patients with idiopathic pulmonary arterial hypertension. PLOS ONE. 2014;9(6):e98889.
Yamabe S, Dohi Y, Fujisaki S, Higashi A, Kinoshita H, Sada Y, et al. Prognostic factors for survival in pulmonary hypertension due to left heart disease. Circ J. 2016;80(1):243–9.
Assad TR, Hemnes AR, Larkin EK, Glazer AM, Xu M, Wells QS, et al. Clinical and biological insights into combined post- and pre-capillary pulmonary hypertension. J Am Coll Cardiol. 2016;68(23):2525–36.
Rosenkranz S, Lang IM, Blindt R, Bonderman D, Bruch L, Diller GP, et al. Pulmonary hypertension associated with left heart disease: updated recommendations of the cologne consensus conference 2018. Int J Cardiol. 2018;272S:53–62.
Zhong XJ, Tang J, Zhao QH, Gong SG, Jiang R, Liu JM, et al. Can the diastolic pulmonary pressure gradient provide cardiopulmonary capacity information in patients with pulmonary hypertension and left heart disease? Int J Cardiol. 2020;305:138.
Dragu R, Hardak E, Ohanyan A, Adir Y, Aronson D. Prognostic value and diagnostic properties of the diastolic pulmonary pressure gradient in patients with pulmonary hypertension and left heart disease. Int J Cardiol. 2019;290:138–43.
Tampakakis E, Leary PJ, Selby VN, De Marco T, Cappola TP, Felker GM, et al. The diastolic pulmonary gradient does not predict survival in patients with pulmonary hypertension due to left heart disease. JACC Heart Fail. 2015;3(1):9–16.
Farina S, Correale M, Bruno N, Paolillo S, Salvioni E, Badagliacca R, et al. The role of cardiopulmonary exercise tests in pulmonary arterial hypertension. Eur Respir Rev. 2018;27(148):170134.
Paolillo S, Veglia F, Salvioni E, Corra U, Piepoli M, Lagioia R, et al. Heart failure prognosis over time: how the prognostic role of oxygen consumption and ventilatory efficiency during exercise has changed in the last 20 years. Eur J Heart Fail. 2019;21(2):208–17.
Malhotra R, Bakken K, D’Elia E, Lewis GD. Cardiopulmonary exercise testing in heart failure. JACC Heart Fail. 2016;4(8):607–16.
Agostoni P, Paolillo S, Mapelli M, Gentile P, Salvioni E, Veglia F, et al. Multiparametric prognostic scores in chronic heart failure with reduced ejection fraction: a long-term comparison. Eur J Heart Fail. 2018;20(4):700–10.
Arena R, Myers J, Guazzi M. The clinical and research applications of aerobic capacity and ventilatory efficiency in heart failure: an evidence-based review. Heart Fail Rev. 2008;13(2):245–69.
Maiorana AJ, Naylor LH, Dongelmans S, Jacques A, Thijssen DH, Dembo L, et al. Ventilatory efficiency is a stronger prognostic indicator than peak oxygen uptake or body mass index in heart failure with reduced ejection fraction. Eur J Prev Cardiol. 2020;27(19):2095–8.
Arena R, Myers J, Aslam SS, Varughese EB, Peberdy MA. Influence of subject effort on the prognostic value of peak VO2 and the VE/VCO2 slope in patients with heart failure. J Cardiopulm Rehabil. 2004;24(5):317–20.
Arena R, Myers J, Aslam SS, Varughese EB, Peberdy MA. Peak VO2 and VE/VCO2 slope in patients with heart failure: a prognostic comparison. Am Heart J. 2004;147(2):354–60.
Myers J, Oliveira R, Dewey F, Arena R, Guazzi M, Chase P, et al. Validation of a cardiopulmonary exercise test score in heart failure. Circ Heart Fail. 2013;6(2):211–8.
Keteyian SJ, Patel M, Kraus WE, Brawner CA, McConnell TR, Pina IL, et al. Variables measured during cardiopulmonary exercise testing as predictors of mortality in chronic systolic heart failure. J Am Coll Cardiol. 2016;67(7):780–9.
Groepenhoff H, Vonk-Noordegraaf A, Boonstra A, Spreeuwenberg MD, Postmus PE, Bogaard HJ. Exercise testing to estimate survival in pulmonary hypertension. Med Sci Sports Exerc. 2008;40(10):1725–32.
Miyamoto S, Nagaya N, Satoh T, Kyotani S, Sakamaki F, Fujita M, et al. Clinical correlates and prognostic significance of six-minute walk test in patients with primary pulmonary hypertension. Comparison with cardiopulmonary exercise testing. Am J Respir Crit Care Med. 2000;161(21):487–92.
Wensel R, Francis DP, Meyer FJ, Opitz CF, Bruch L, Halank M, et al. Incremental prognostic value of cardiopulmonary exercise testing and resting haemodynamics in pulmonary arterial hypertension. Int J Cardiol. 2013;167(4):1193–8.
Wensel R, Opitz CF, Anker SD, Winkler J, Hoffken G, Kleber FX, et al. Assessment of survival in patients with primary pulmonary hypertension: importance of cardiopulmonary exercise testing. Circulation. 2002;106(3):319–24.
Acknowledgements
All authors wish to thank the technicians at the department of pulmonary function at shanghai pulmonary hospital.
Funding
The work was funded by the Program of National Natural Science Foundation of China (81700045, 81870042), the Three-year Action Plan to Promote Clinical Skills and Clinical Innovation in Municipal Hospitals (SHDC2020CR4021) and the Program of Shanghai Pulmonary Hospital (FKLY20005).
Author information
Authors and Affiliations
Contributions
Conception and design: XJZ, RJ and LY; Administrative support: JT, LW and JML; Provision of study materials or patients: RJ, QHZ and SGG; Collection and assembly of data: XJZ, CJL, HLQ and HTL; Data analysis and interpretation: PY, JH and RZ; Manuscript writing all authors. All authors have read and approved the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. The study was conducted in accordance with the Declaration of Helsinki (as revised in 2013). The study was approved by the Institutional Ethics Committee of Shanghai Pulmonary Hospital approved the protocol (K16-317) and individual consent for this retrospective analysis was waived.
Consent for publication
Not applicable.
Competing interests
All authors have completed the ICMJE uniform disclosure form. The authors have no competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Comparison of CPET and hemodynamics stratified by sex and Cpc-PH or Ipc-PH.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhong, XJ., Jiang, R., Yang, L. et al. Peak oxygen uptake is a strong prognostic predictor for pulmonary hypertension due to left heart disease. BMC Cardiovasc Disord 22, 137 (2022). https://doi.org/10.1186/s12872-022-02574-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-022-02574-0