Abstract
Background
A honeycomb-like structure (HLS) is a rare abnormality characterized by a braid-like appearance. Angiograph and intravascular examination, including coherence tomography and intravascular ultrasound (IVUS), can further confirm the multiple intraluminal channels or honeycomb structure, which can also be described as looking like ‘swiss cheese’, a ‘spider web’ or a ‘lotus root’. Previous studies have mostly reported this abnormality in coronary arteries, with a few cases in renal arteries. More information about the characteristics and development of HLS is needed.
Case presentation
A 69-year-old Han man with resistant hypertension received abdominal enhanced computerised tomography and was revealed to have left renal artery stenosis with the possibility of left renal infarction. Renal artery angiography confirmed a 95% stenosis located in the proximal segment of the left renal artery, and the middle segment was blurred with multi-channel-like blood flow. Further IVUS was performed and identified multiple channels surrounded by fibrous tissue. It was a rare case of HLS in the renal artery secondary to the thrombus, with organisation and recanalisation. Balloon dilatation and stent implantation at the proximal segment of the left renal artery were performed successfully. Blood pressure was well controlled after the procedure.
Conclusions
The IVUS findings are helpful for forming interventional therapeutic strategies for HLS lesions in the renal artery.
Similar content being viewed by others
Background
A honeycomb-like structure (HLS) was first described by Terashima et al. in a 26-year-old man with a history of Kawasaki disease at the proximal segment of the left anterior descending artery (LAD) [1]. This abnormality is rare in that its aetiology and characteristics are still unclear. In addition, compared to work on coronary arteries, studies concentrating on HLS involved in renal arteries are relatively scarce [2, 3]. Therefore, we herein describe the case of a 69-year-old man with HLS along with renal artery stenosis, secondary hypertension and suspected renal infarction treated with interventional treatment. To our knowledge, this is the first case of HLS on the basis of atherosclerosis in the renal artery.
Case presentation
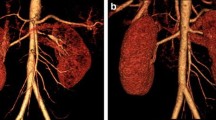
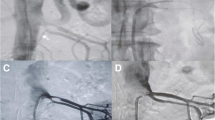
A 69-year-old Han man complained of chest distress and shortness of breath after stress for four months. He was diagnosed with hypertension for four months, and he felt that these symptoms were accompanied by high blood pressure. The maximum blood pressure measured was 200/110 mmHg. Benidipine hydrochloride (4 mg twice daily), metoprolol succinate (47.5 mg Qd), furosemide (20 mg Qd) and spironolactone (20 mg Qd) were applied to control blood pressure. In addition, he had a dull pain in his left waist for four months. Abdominal enhanced computerised tomography (CT) demonstrated a suspected left renal infarction. His past medical history included 10 years of diabetes mellitus and hyperlipidemia. During this hospitalization, he was diagnosed with resistant hypertension with chronic renal disease and renal dysfunction (creatinine 122 µmol/L, eGFR = 51.80 mL/min × 1.73 m2). Abdominal enhanced CT was reperformed and showed that his left renal artery was nearly occluded, his right renal artery had mild to moderate stenosis and his left kidney had atrophied. An invasive angiography with angiographic catheter JR 4.0 further demonstrated a 95% stenosis of the proximal segment of the left renal artery, and the middle segment was blurred with multi-channel-like blood flow (Fig. 1, Additional file 1). An RDC guiding catheter was used and run through across the lesion. The proximal lesion was pre-dilated by a 4.0 mm × 15 mm balloon at 10 atm. A commercially available IVUS system (iLAB, Boston Scientific Corporation, Marlborough, Massachusetts) was used to acquire IVUS images. A 40 MHz, 2.6 F imaging catheter (Atlantis SR Pro or Pro 2, Boston Scientific) was advanced distal to the lesion, and an automated pullback was performed at a speed of 0.5 mm/s. Multiple lumens and HLS were demonstrated by IVUS, and the cavity was surrounded by fibrous tissue (Fig. 2, Additional file 2). A lesion of the middle segment of the left renal artery was sequentially dilated by a 1.5 × 15 mm balloon, 2.5 × 10 mm balloon and 4.0 × 15 mm balloon at 8–12 atm, and an express SD 5.0 × 19 mm stent was implanted at 12 atm successfully, overlapping with the proximal segment of the left renal artery (Fig. 3, Additional file 3). The final angiogram showed restored flow to the distal renal artery. The patient recovered well and was discharged with atorvastatin (20 mg Qd), ezetimibe (10 mg Qd), aspirin (100 mg Qd), clopidogrel (75 mg Qd), Sacubitril Valsartan Sodium (25 mg Bid) and metoprolol succinate (47.5 mg Qd). Over three months of follow-up, the patient achieved complete remission of chest distress, shortness of breath and waist pain. Blood pressure was well controlled around 130/75 mmHg and renal function was recovered (creatinine 96 µmol/L, eGFR 69.21 mL/ (min × 1.73 m2).
Discussion and conclusions
HLS is considered a rare vascular lesion with a diffuse lesion or a braid-like appearance that can be detected by angiography, and further intravascular examination, such as IVUS and coherence tomography (OCT), helped to confirm the multiple intraluminal channels or honeycomb structure, which can also be described as having a ‘swiss cheese-’, a ‘spider web-’, or a ‘Lotus root-like’ appearance [4]. IVUS and OCT are helpful and essential for diagnosing HLS [5]. HLS was mostly reported in the coronary artery, but there were also some case reports of HLS being located in the carotid artery and renal artery [3, 5, 6]. The aetiology of HLS is still not clear. Previous studies have reported that it can be caused by spontaneous recanalisation after thrombotic events, including in situ thrombosis and embolic thrombus. Thrombosis can be secondary to vasculitis caused by Kawasaki disease, antiphospholipid syndrome and vasospasm [1, 7,8,9,10]. With the application and development of intravascular examination, more and more HLS was found, and most of its causes were thought to be recanalisation of the in situ thrombus and embolic thrombus [5]. Kazuoki et al. reported serial coronary angiography of a post-emergent coronary artery bypass grafting patient and found that occlusive thrombus in the left circumflex artery (LCX) was recanalised spontaneously after two years of follow-up. A lotus-root appearance was then confirmed by OCT, which provided the direct evidence that the multiple communicating channel structure represented spontaneous recanalised lesions after the thrombotic occlusions [11]. A similar manifestation was also found in an effort angina patient and confirmed by high-resolution intravascular ultrasound (HR-IVUS) [12]. Despite recanalization, most HLS lesions significantly affect blood flow, with an FFR value < 0.8 [2]. Therefore, positive intervention therapy was suggested for HLS lesions. Previous studies reported different treatment strategies, including drug-eluting stent (DES) implantation, drug-coating balloon and bioresorbable vascular scaffold [5, 13, 14]. However, stent implantation, which compresses both the septa and cavities, may be associated with side branch compromise or occlusion [2].
To our knowledge, this is the first case of HLS on the basis of atherosclerosis in the renal artery. The renal artery multiple luminal surrounded by fibrous tissue was demonstrated by IVUS, and no intact vascular wall of branches was shown in intravascular imaging. The properties of the lesions could not be fully identified. Upon consideration of multiple atherosclerotic risk factors, including age, diabetes and hyper-lipidaemia, we surmised that the stenosis of the left proximal renal artery resulted from atherosclerosis. Based on serious stenosis of the proximal artery, the decreased velocity of distal blood flow led to thrombus formation, which was associated with renal infarction. The thrombus was recanalized and finally formed HLS in his renal artery as a result of mismanagement in the acute phase. In addition, three months of follow-up showed that the patient had no complaint after stent implantation, which also verified our previous speculations.
In conclusion, the mechanism and formation of HLS are still unclear. This malformation can be found not only in the coronary artery but also in the renal artery. Detailed patient histories, long-term follow-up, angiogram, and intravascular imaging data may offer a deeper understanding of HLS in future clinical practice.
Availability of data and materials
All data generated or analyzed during this study are included in this manuscript and its additional files.
Abbreviations
- HLS:
-
Honeycomb-like structure
- LAD:
-
Left anterior descending artery
- CT:
-
Computerized tomography
- IVUS:
-
Intravascular ultrasound
- OCT:
-
Coherence tomography
- LCX:
-
Left circumflex artery
- HR-IVUS:
-
High-resolution intravascular ultrasound
- DES:
-
Drug-eluting stent
References
Terashima M, Awano K, Honda Y, Yoshino N, Mori T, Fujita H, Ohashi Y, Seguchi O, Kobayashi K, Yamagishi M. “Arteries within the artery” after Kawasaki disease: a lotus root appearance by intravascular ultrasound. Circulation. 2002;106(7):887–887.
Xu T, Shrestha R, Pan T, Huang X, Xu H, Zhang J-J, Tao L, Han Y, Chen S-L. Anatomical features and clinical outcome of a honeycomb-like structure in the coronary artery: reports from 16 consecutive patients. Coron Artery Dis. 2020;31(3):222–9.
Nakazato K, Kobayashi A, Nodera M, Kamioka M, Suzuki H, Saitoh S-I, Takeishi Y. Lotus root sign in the renal artery in renovascular hypertension. Circ J. 2017;81:1234–5.
Fujino Y, Attizzani GF, Tahara S, Takagi K, Naganuma T, Nakamura S, Nakamura S. A honeycomb-like structure in chronic total occlusion demonstrated by frequency-domain optical coherence tomography. Int J Cardiol. 2015;186:239–40.
Lin M, Su Z, Li J, Nie R, Wang J. Honeycomb-like structure in the right coronary artery treated with a drug-eluting stent: a case report and literature review. J Int Med Res. 2018;46(5):2008–13.
Chang H, Yoon HJ, Hong J-H, Kim C-H, Sohn S-I, Lee C-Y. Republished: a lotus root-like appearance in carotid stenosis on optical coherence tomography. J Neurointervent Surg. 2016;8(6):e21–e21.
Kimura T, Itoh T, Fusazaki T, Nakamura M, Morino Y. A honeycomb-like structure in the right coronary artery visualized by three-dimensional optical coherence tomography. Coron Artery Dis. 2015;26(4):356–60.
Koyama K, Yoneyama K, Mitarai T, Kuwata S, Ishibashi Y, Kongoji K, Akashi YJ. In-stent protrusion after implantation of a drug-eluting stent in a honeycomb-like coronary artery structure: complete resolution over 6 months and the role of optical coherence tomography imaging in the diagnosis and follow-up. JACC Cardiovasc Interv. 2014;7(5):e39–40.
Suzuki S, Sotomi Y, Nakatani S, Hirata A, Hao H, Tsujimoto M, Tsuji H, Shiojima I, Sakata Y, Hirayama A. Histopathologic insights into the honeycomb-like structure in the coronary artery: in vivo multimodality imaging assessment with directional coronary atherectomy. JACC Cardiovasc Interv. 2018;11(19):e157–9.
Toutouzas K, Karanasos A, Stathogiannis K, Synetos A, Tsiamis E, Papadopoulos D, Stefanadis C. A honeycomb-like structure in the left anterior descending coronary artery: demonstration of recanalized thrombus by optical coherence tomography. JACC Cardiovasc Interv. 2012;5(6):688–9.
Dai K, Suruga K, Nakano T, Takemoto H, Hashimoto Y, Tomomori S, Higaki T, Oi K, Kawase T, Nakama Y. A lotus root-like appearance in a spontaneously recanalized lesion confirmed by serial coronary angiography: from optical coherence tomography study. Coron Artery Dis. 2019;30(2):150–1.
Kahata M, Satomi N, Otsuka M, Ishii Y. Honeycomb-like structure in spontaneous recanalized coronary thrombus demonstrated by serial angiograms: a case report. Eur Heart J Case Rep. 2020;4(5):1.
Watanabe Y, Fujino Y, Ishiguro H, Nakamura S. Recanalized thrombus treated with a paclitaxel-coated balloon: Insights from optical coherence tomography. JACC Cardiovasc Interv. 2016;9(6):618–20.
Gómez-Monterrosas O, Regueiro A, Santos A, Otsuki S, Scalone G, Fernández-Rodríguez D, Sabaté M. Recanalized thrombus treated with bioresorbable vascular scaffold: insights from optical coherence tomography. JACC Cardiovasc Interv. 2014;7(12):1453–5.
Acknowledgements
We thank all the cardiologists involved in the study.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
WS and YJ guided the study. CC and YZ drafted the manuscript. DY and YL finished the figures. YC and YL collected the data. All authors have read and approved the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable. Study approval was not necessary as this is a case report and consent for publication was taken from the patients.
Consent for publication
Written informed consent was obtained from the patient for the publication of this case report. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1. Pre-operation renal artery arteriography.
Additional file 2. IVUS for honeycomb-like structure in left renal artery.
Additional file 3. Post-operation renal artery arteriography.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, C., Zhang, Y., Yin, D. et al. Refractory hypertension secondary to renal artery stenosis with a honeycomb-like structure. BMC Cardiovasc Disord 21, 606 (2021). https://doi.org/10.1186/s12872-021-02428-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-021-02428-1