Abstract
Background
Systematic investigation and analysis of cardiovascular health status (CVHS) of Chinese women is rare. This study aimed to assess CVHS and atherosclerotic cardiovascular disease (ASCVD) burden in the Chinese women physicians (CWP) and community-based non-physician cohort (NPC).
Methods
In this prospective, multicenter, observational study, CVHS using the American Heart Association (AHA) defined 7 metrics (such as smoking and fasting glucose) and ASCVD risk factors including hypertension, hyperlipidemia and type-2 diabetes were evaluated in CWP compared with NPC.
Results
Of 5832 CWP with a mean age of 44 ± 7 years, only 1.2% achieved the ideal CVHS and 90.1% showed at least 1 of the 7 AHA CVHS metrics at a poor level. Total CVHS score was significantly decreased and ASCVD risk burden was increased in postmenopausal subjects in CWP although ideal CVHS was not significantly influenced by menopause. Compared to 2596 NPC, fewer CWP had ≥ 2 risk factors (8% vs. 27%, P < 0.001); CWP scored significantly higher on healthy factors, a composite of total cholesterol, blood pressure, fasting glucose (P < 0.001), but, poorly on healthy behaviors (P < 0.001), specifically in the physical activity component; CWP also showed significantly higher levels of awareness and rates of treatment for hypertension and hyperlipidemia, but, not for type-2 diabetes.
Conclusion
Chinese women’s cardiovascular health is far from ideal and risk intervention is sub-optimal. Women physicians had lower ASCVD burden, scored higher in healthy factors, but, took part in less physical activity than the non-physician cohort. These results call for population-specific early and improved risk intervention.
Similar content being viewed by others
Background
Atherosclerotic cardiovascular disease (ASCVD) remains the leading cause of mortality worldwide and affects 6.6 million US women annually [1, 2]. However, a recent report showed that nearly 45% of women in the United States were unaware that ASCVD is the leading cause of death, and only 52% considered themselves at risk of myocardial infarction (MI) although most of them had ≥ 3 risk factors [3]. The awareness of ASCVD risk factors in Chinese women, where the ASCVD has substantially increased in recent years [4, 5], remains unknown.
To address the urgent need for primordial prevention of cardiovascular disease (CVD), the American Heart Association (AHA) proposed 7 health metrics, also referred to as Life’s Simple 7, including 4 health behaviors (smoking, body mass index (BMI), physical activity, and healthy diet) and 3 health factors (total cholesterol (TC), blood pressure (BP), and fasting blood glucose (FBG)) [6]. Three stages for each metric were created to reflect “ideal,” “intermediate,” and “poor” cardiovascular health status (CVHS) [6]. A number of studies [7,8,9] have evaluated CVHS and its association with ASCVD and a recent meta-analysis of 9 prospective cohort studies involving 12,878 participants reported that achieving the most ideal cardiovascular health metrics was associated with lower risk of all-cause mortality (RR = 0.55; 95% CI: 0.37–0.80), cardiovascular mortality (RR = 0.25; 95% CI: 0.10–0.63), CVD (RR = 0.20; 95% CI: 0.11–0.37), and stroke (RR = 0.31; 95% CI: 0.25–0.38) [10]. However, CVHS has not been evaluated in Chinese women, especially in Chinese women physicians (CWP).
With the aim for systematic investigation and analysis of cardiovascular health status of Chinese women doctors, we designed a prospective cohort study of CWP for ASCVD risk assessment and for implementation of effective risk reduction strategies to improve CVHS. In the current report, CVHS and ASCVD risk burden, particularly the modifiable risk factors, in CWP were evaluated compared to a community-based non-physician cohort (NPC). The levels of awareness for the modifiable ASCVD risk factors (hypertension, hyperlipidemia and type-2 diabetes (T2D)) and proportion of taking interventional actions in CWP and NPC were analyzed. This study may improve CWP’s attention to CVD, understand their own cardiovascular health status, and provide a basis for understanding Chinese women's CVD risk factors, incidence trends, and formulating prevention and treatment recommendations.
Methods
Study population
The CWP cohort study was a prospective, multicenter, observational study aimed to investigate the current CVHS and ASCVD risk factors among women physicians. The sample size of the study was initially estimated as 5740 subjects using Epi Infor Software based on the incidence of major cardiovascular events (about 1.5%) in a 4-year follow-up period in China [11]. Between January 2015 and June 2017, a total of 9661 subjects aged ≥ 35 years were recruited with a cluster sampling method across 52 study centers of 21 provinces in China (Additional file 1). An online standardized questionnaire specifically designed for this study was used (Additional file 2). Those 997 subjects who did not answer the questionnaire and 2639 subjects who provided the questionnaires with insufficient data were considered to decline research participation and had to be excluded. We received questionnaires with complete data response from 6025 subjects, which correspond to a participation rate of 62.4%. The inclusion criteria were: (1) physicians at the study centers; (2) ≥ 35 years old; (3) free of prior ASCVD, cancer and other major illness. Of the 6025 enrolled, 5832 subjects were confirmed to be free of ASCVD and other major diseases and included in the present report (Fig. 1). The study protocol was approved by the Ethics Committee of the Chinese General PLA Hospital and was in accordance with standards set forth by the Declaration of Helsinki. All participants provided their written informed consent before officially entering in the study.
To better understand the levels of ASCVD risk in CWP who have the best knowledge on CVHS relative to other population, a community-based NPC was selected from PERSUADE study [12], which is an on-going prospective cohort study in which 9078 participants were recruited from the local community hospitals geographically located in Tangshan City in northern China between January 2013 and January 2015. The inclusion criteria were: (1) women aged ≥ 35 years old; (2) providing informed consent; (3) free of prior ASCVD, cancer and other major diseases. The subjects who meet the inclusion criteria were eligible for this study. Finally, 2596 non-physician women were included in the present study (Fig. 1).
Clinical and laboratory data collection
Participants’ demographic information, behavior characteristics (including diet, exercise, smoking status and alcohol consumption), medical history and current medications, and family history of ASCVD were collected by trained interviewers using a web-based standardized questionnaire specifically designed for this study. Body weight, height and blood pressure were obtained using the most recent annual physical examination records at each site. Laboratory measurements of lipids, FBG or glycated hemoglobin (HbA1C) were also obtained from routine annual physical examination lab reports.
Definitions of ASCVD risk
Hypertension was defined as having any of the following 3 criteria: (1) either systolic BP (SBP) ≥ 140 mmHg or diastolic BP (DBP) ≥ 90 mmHg; (2) use of hypertension medication; (3) established diagnosis of hypertension by physicians.
T2D was defined as meeting any of the following 4 conditions: (1) FBG ≥ 7 mmol/L (126 mg/dL); (2) HbA1C ≥ 6.5%; (3) use of diabetes medication(s); (4) established diagnosis of T2D by physicians.
Hyperlipidemia was defined as having any of the following 3 measurements or 2 clinical conditions: (1) TC ≥ 5.2 mmol/L (≥ 200 mg/dL), (2) low-density lipoprotein cholesterol (LDL-C) ≥ 4.1 mmol/L (≥ 160 mg/dL), (3) triglycerides (TG) ≥ 1.7 mmol/L (≥ 150 mg/dL), (4) history of hyperlipidemia with established diagnosis by physicians; or (5) taking any lipid-lowering medication(s). The abnormal stratified standards of blood lipids for the primary prevention population of ASCVD were determined based on the 2016 Chinese guideline for the management of dyslipidemia in adults [13].
Cardiovascular health status (CVHS) and score
CVHS was evaluated using the AHA 7 metrics including smoking, BMI, physical activity, healthy diet, TC, BP, and FBG [6]. CVHS was further classified into 3 categories: ideal, intermediate and poor.
Ideal CVHS required all 7 metrics at ideal conditions: (1) never smoked or stopped smoking for at least 12 months. (2) BMI < 24 kg/m2 for Chinese. (3) vigorous physical activity ≥ 75 min a week or moderate physical activity ≥ 150 min a week, or combination of both ≥ 150 min a week. Sodium and cereals intake could not be evaluated accurately due to a lack of such data collected. The ideal diet was modified in our study which included: (a) vegetables and fresh fruits ≥ 4.5 servings per day, (b) fish ≥ 3.5 oz servings per week, (c) sugar sweetened beverage consumed ≤ 450 kcal (36 oz or 4 glasses) per week, (d) meat consumed none or ≤ 2 servings per week. (5) untreated TC < 5.20 mmol/L (< 200 mg/dL). (6) untreated BP < 120/80 mmHg. (7) untreated FBG < 5.6 mmol/L (< 100 mg/dL).
Intermediate CVHS was defined as presence of any one of the 7 metrics at intermediate score and no others at poor. The criteria of intermediate CVHS included: (1) former smokers who quit less than 12 months. (2) BMI 24–27.9 kg/m2. (3) vigorous physical activity 1–74 min a week or moderate physical activity 1–149 min a week, or combination of both 1–149 min a week. (4) 2–3 ideal diet components. (5) TC 5.2–6.2 mmol/L (200–239 mg/dL) or treated to goal. (6) SBP 120–139 mmHg or DBP 80–89 mmHg or treated to goal. (7) FBG 5.6–7.0 mmol/L (100–125 mg/dL) or treated to goal.
Poor CVHS was defined as any of these metrics at poor levels, which included: (1) current smokers, (2) BMI ≥ 28 kg/m2, (3) no physical activity, (4) 0–1 diet components, (5) TC ≥ 6.20 mmol/L (≥ 240 mg/dL), (6) SBP ≥ 140 or DBP ≥ 90 mmHg, and (7) FBG ≥ 7 mmol/L (≥ 126 mg/dL).
In addition, a total score ranging from 0 to 14 was calculated as the sum of each individual component of the AHA 7 metrics (poor = 0 point, intermediate = 1 point, and ideal = 2 points) [14]. CVHS was evaluated using 6 available metrics in the community-based NPC because dietary information was not collected.
Statistical analysis
Continuous variables are described as mean ± SD and compared using two-sample t-tests. Categorical variables are expressed as percentages and compared using x2 tests. A two-sided P < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS 19.0 statistical software.
Results
Baseline characteristics in CWP and NPC
Figure 1 and Table 1 shows the characteristics of the 2 cohorts. Compared with NPC, CWP group were younger, with fewer smokers, lower prevalence of hypertension and T2D. However, hyperlipidemia was more prevalent in CWP than NPC. The percentage of CWP who developed ≥ 2 risk factors was lower than NPC. CWP also had lower BMI, TC and FBG, while TG and LDL-C in the CWP group and NPC group were not statistically different.
There were fewer post-menopausal subjects (14% vs 40%,P< 0.001); however, higher prevalence of the hormone replacement therapy (1.3% vs 0.5%,P< 0.001) in CWP than in NPC.
Cardiovascular health status and score
Among 5832 CWP, only 71 (1.2%) participants had all 7 metrics at the ideal level, 502 (8.6%) at the intermediate level, while most subjects (90.1%) had at least one metric at the poor level. Each CVHS metric was compared separately between the 2 cohorts except for the diet (Table 2). In terms of the 4 healthy behaviors, smoking was low overall, but there were more current smokers in NPC than in CWP (2% vs. 0.9%,P< 0.001). Ideal BMI was present in 72% of CWP and 56% of NPC (P < 0.001). Ideal physical activity was seen significantly less frequent in CWP than in NPC (10% vs. 58%,P< 0.001). Furthermore, 84% of the physicians didn’t have any moderate or vigorous activity at all. Only 26% of CWP met the ideal diet definition.
As shown in Table 2, among the healthy factors, the prevalence of ideal BP and TC were higher in CWP compared to NPC (59% vs. 38%, 78% vs. 68%, separately,P< 0.001), and ideal FBG was same between the 2 cohorts (P = 0.84). CWP had a lower total score without diet information than NPC (9.0 ± 1.4 vs. 9.2 ± 1.9, P 0.001). As for healthy factors, CWP did better than NPC (5.1 ± 1.0 vs. 4.6 ± 1.1, P < 0.001); however, for healthy behaviors, CWP performed worse than NPC (P < 0.001), which was primarily due to poor physical activity (84% vs. 35%, P < 0.001).
Influence of menopause on risk burden and CVHS in CWP
Overall, 838 (14%) subjects reported being post-menopause, 833 (14%) subjects were going through menopause, and 4161 (72%) subjects were pre-menopause. As shown in Table 3, the risk factors presented a stepwise increasing trend from pre-menopause to menopause and to post-menopause: BMI (22 ± 2.7 vs. 23 ± 2.7 vs. 23 ± 2.8 kg/m2, P< 0.001), TC (4.3 ± 1.0 vs. 4.4 ± 1.1 vs. 4.9 ± 1.2 mmol/L, P < 0.001), LDL-C (2.5 ± 0.8 vs. 2.6 ± 0.9 vs. 2.8 ± 0.9, mmol/L, P < 0.001), TG (1.4 ± 0.9 vs. 1.5 ± 1.1 vs. 1.6 ± 1.0 mmol/L, P < 0.001), and FBG (5.1 ± 1.0 vs. 5.2 ± 1.0 vs. 5.3 ± 1.2 mmol/L, P< 0.001). Similar trends were seen in the risk burden (hypertension, hyperlipidemia, T2D, and number of subjects with ≥ 2 risk factors) from pre-menopause to menopause and to post-menopause. CVHS total score showed a significant stepwise decrease from pre-menopause to post-menopause (P < 0.001). However, CVHS distribution of ideal, intermediate and poor was not significantly different among the 3 menopause groups (P = 0.66). The ideal diet was significantly more frequent in post-menopausal subjects (24% vs. 25% vs. 33%, P< 0.001).
Level of awareness and rate of treatment for modifiable risk factors
Figure 2 presents the level of awareness and rate of intervention for hypertension, hyperlipidemia and T2D in CWP and NPC. As shown in Fig. 2a, CWP group showed a significant higher level of awareness for hypertension and hyperlipidemia than NPC (89% vs. 50%, P< 0.001 and 35% vs. 24%, P< 0.001), but, a lower level for T2D (51% vs. 67%, P< 0.001). Among subjects who were aware of these 3 modifiable conditions, treatment rates for hypertension and hyperlipidemia were higher in CWP than that in NPC (86% vs. 80%, P= 0.02 and 27% vs. 17%, P< 0.001), but, not significantly different for T2D between the 2 cohorts (74% vs. 82%, P= 0.2) (Fig. 2b).
Discussion
China is experiencing a substantial and rapid increase in ASCVD [4, 5]. Our study evaluated and compared CVHS and ASCVD risk burden in 2 populations of Chinese women, who were free from clinical ASCVD. We found that: (1) only 1.2% of CWP achieved the ideal CVHS and 90% showed at least 1 of the 7 AHA CVHS metrics at a poor level; (2) CVHS total score significantly decreased and ASCVD risk burden significantly increased in postmenopausal women although the ideal CVHS was not significantly influenced by menopause; (3) Compared with NPC, few CWP had ≥ 2 risk factors, and CWP scored significantly higher on healthy factors, a composite of TC, BP, and FBG, however, poorly on healthy behaviors, specifically in physical activity; (4) CWP also showed significantly higher levels of awareness and rates of treatment for hypertension and hyperlipidemia than NPC, but, not for T2D.
The extremely low ideal CVHS (1%) and high poor CVHS (90%) among CWP with a mean age of 44 years seen in our study are very alarming, although our observed ideal CVHS is somewhat better than that reported in previous studies [15, 16]. The younger age, medical education and health care profession in CWP may explain the differences regarding the number of subjects with ≥ 2 risk factors and CVHS healthy factor score between CWP and NPC. The results of our study complement previous findings from different populations [11, 17, 18].
It is established that healthy behaviors including non-smoking, healthy weight, diet and physical activity in CVHS are associated with lower risk of ASCVD [15, 16, 19, 20]. We found 84% of CWP with poor physical activity in our study, reporting no vigorous or moderate physical activity per week. This rate is several folds higher than the general populations in Europe (7–38%) and in the US (24% in 2005) [21, 22]. A heavy load of clinical work and physically inactive nature of the medical profession certainly add challenges for physicians to reach an ideal level of physical activity [23] By contrast, NPC in our study were more likely to be laborers as a profession which led to a lower rate (35%) of NPC with poor physical activity. Obviously, the difference between the 2 cohorts was due to professions not exercise. Nevertheless, physical inactivity among health care providers needs to be addressed for improved CVHS.
Hyperlipidemia was significantly more frequent in CWP than NPC. It is worth noting that the average level of LDL-C, 2.6 mmol/L (100 mg/dL), in our study is considered relatively normal for this population without clinical ASCVD based on current understanding. However, it is debatable whether this level of LDL-C is ideal. It has been reported that normal LDL-C levels were associated with subclinical atherosclerosis in absence of ASCVD risk factors [24]. Recently, Ference et al. [25] have suggested that plaque burden was accumulating from early age in life even with a normal LDL-C level and that ASCVD events begin to occur when LDL-C exposure threshold (Age × LDL-C mmol/L) moves beyond 129 mmol-years. To put this concept in contact with our data, mean age of 44 years and current average LDL-C level of 2.6 mmol/L in CWP; the current LDL-C exposure threshold is 113.5 mmol-years and will be higher than 129 mmol-years when CWP cohort reaches age of 50 years.
However, if the LDL-C level had been maintained at 1.8 mmol/L or lower (≤ 70 mg/dL), LDL-C exposure threshold would be 79.2 mmol-years now and would not go beyond 129 mmol-years until the cohort reaches an age of 71 years. Furthermore, previous intravascular imaging studies showed that coronary plaques may only stop progressing with the LDL-C level at ≤ 70 mg/dL [26, 27]. These data together strongly support a lower LDL-C level at a younger age.
For primary prevention of overall cardiovascular disease, AHA introduced “Life’s Simple 7”, which has been used as an effective tool for the promotion of cardiovascular disease prevention by previous studies [28, 29]. AHA definition of ideal TC is an untreated TC level less than 5.2 mmol/L (200 mg/dL) [6]. When more stringent guidelines were applied, goals of TC were even lower. The most recent consensus guidelines from the ESC/EAS established more stringent goals of ideal TC ≤ 4 mmol/L (≤ 155 mg/dl) [30]. Consistent with the 2016 Chinese guideline for the management of dyslipidemia [13] and AHA definition of ideal TC [6], our study set TC ≥ 5.2 mmol/L as one of the criteria signs for hyperlipidemia.
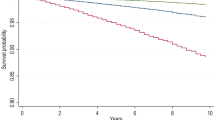
Another way to understand the future ASCVD risk in these 2 given populations is to project lifetime risk using the number of risk factors. Based on a published risk model in Chinese women [31], 8% and 12% cumulative ASCVD events over the next 10 years will be expected in CWP and NPC with ≥ 2 risk factors in our study.
Above and beyond aging, menopause plays an important role in increasing ASCVD risk in women [32, 33]. As shown in our study, CVHS total score decreased and ASCVD burden increased significantly during and post menopause. The ideal CVHS was not significantly influenced by menopause, because postmenopausal individuals were more conscious of healthy behaviors with better diet and maintained physical activity. A recent study has demonstrated that healthy lifestyle during menopause and midlife was associated with less subclinical atherosclerosis in women [34]. In addition, studies suggested that the follicle-stimulating hormone (FSH) rather than the estrogen may influence the 10-year ASCVD risk in post-menopausal women [35, 36].
It was estimated that promoting the overall population CVHS to ideal level will reduce deaths from ASCVD by 30% between 2010 and 2020 [37]. Our study showed that CWP had higher level of awareness and rate of treatment for hypertension than NPC and the general population [38]. The level of awareness for T2D was also higher in our study than the general population [39]. The low level of awareness and even lower rate of treatment for hyperlipidemia were consistent with those seen in the general population in China [40]. Moreover, in PERCRO-DOC survey [41], researchers found that the knowledge of current guidelines of physicians is not satisfactory and only 53.3% knew the LDL-cholesterol goal value for high-risk patients, which also reflects that physicians themselves may be not aware of the lipid profile of themselves at risk. Similarly, the awareness of CVD in public is insufficient in PERCO survey [42] in which only 43.3% knew their TC value, 30.9% knew what their target TC should be, and 53.2% of the general public have never discussed any CVD risk factor with their physicians. These results demonstrated the unmet need for ASCVD risk intervention and improved promotion of CVD prevention is warranted.
A major limitation of the present study is that the diet information was not collected in NPC, which made it impossible to fully evaluate the CVHS for NPC and to compare the health behavior between CWP and NPC. Nevertheless, our study has identified the similarities and differences in CVHS and ASCVD risk awareness and management. These findings will help to improve the precision of CVHS. Second, selection bias exists in our study such as the geographical restriction of the control cohort. Findings may not be generalizable to populations from different socio-geographic regions. In addition, cardiovascular metrics were obtained only at baseline, and changes over time were not accounted for in this study. The CWP cohort study is on-going and will evaluate ASCVD risk intervention and major events in its follow-up phase to address the importance of implementation of actions from the risk data to interventions.
Conclusions
The cardiovascular health status is far from ideal among Chinese women. Women physicians had lower ASCVD burden, scored higher in healthy factors, but, did poorly in physical activity than the non-physician cohort. The overall ASCVD risk intervention was sub-optimal although women physicians showed higher level of awareness and rates of treatment for hypertension and hyperlipidemia. These results call for necessary population-specific early and improved risk intervention.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ASCVD:
-
Atherosclerotic cardiovascular disease
- MI:
-
Myocardial infarction
- AHA:
-
American Heart Association
- CVHS:
-
Cardiovascular health score
- BMI:
-
Body mass index
- TC:
-
Total cholesterol
- BP:
-
Blood pressure
- FBG:
-
Fasting blood glucose
- CWP:
-
Chinese women physicians
- NPC:
-
Non-physician cohort
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- T2D:
-
Type-2 diabetes
- LDL-C:
-
Low-density lipoprotein cholesterol
- TG:
-
Triglycerides
References
GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet. 2017;390(10100):1151–210.
Mehta LS, Beckie TM, DeVon HA, Grines CL, Krumholz HM, Johnson MN, et al. Acute myocardial infarction in women: a scientific statement from the american heart association. Circulation. 2016;133(9):916–47.
Bairey Merz CN, Andersen H, Sprague E, Burns A, Keida M, Walsh MN, et al. Knowledge, attitudes, and beliefs regarding cardiovascular disease in women: the women’s heart alliance. J Am Coll Cardiol. 2017;70(2):123–32.
Moran A, Gu D, Zhao D, Coxson P, Wang YC, Chen CS, et al. Future cardiovascular disease in china: markov model and risk factor scenario projections from the coronary heart disease policy model-china. Circ Cardiovasc Qual Outcomes. 2010;3(3):243–52.
Yang G, Kong L, Zhao W, Wan X, Zhai Y, Chen LC, et al. Emergence of chronic non-communicable diseases in China. Lancet. 2008;372(9650):1697–705.
Lloyd-Jones DM, Hong Y, Labarthe D, Mozaffarian D, Appel LJ, Van Horn L, et al. Defining and setting national goals for cardiovascular health promotion and disease reduction: the American Heart Association’s strategic Impact Goal through 2020 and beyond. Circulation. 2010;121(4):586–613.
Guo L, Zhang S. Association between ideal cardiovascular health metrics and risk of cardiovascular events or mortality: a meta-analysis of prospective studies. Clin Cardiol. 2017;40(12):1339–46.
Dong C, Rundek T, Wright CB, Anwar Z, Elkind MS, Sacco RL. Ideal cardiovascular health predicts lower risks of myocardial infarction, stroke, and vascular death across whites, blacks, and hispanics: the northern Manhattan study. Circulation. 2012;125(24):2975–84.
Yang Q, Cogswell ME, Flanders WD, Hong Y, Zhang Z, Loustalot F, et al. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA. 2012;307(12):1273–83.
Fang N, Jiang M, Fan Y. Ideal cardiovascular health metrics and risk of cardiovascular disease or mortality: a meta-analysis. Int J Cardiol. 2016;214:279–83.
Wu S, Huang Z, Yang X, Zhou Y, Wang A, Chen L, et al. Prevalence of ideal cardiovascular health and its relationship with the 4-year cardiovascular events in a northern Chinese industrial city. Circ Cardiovasc Qual Outcomes. 2012;5(4):487–93.
Shan DK, Zhou Y, Wang YX, Gao X, Wang W, Yang JJ, et al. Population-based cohort study in outcome of phased progression of atherosclerosis in China (PERSUADE): objective, rationale and design. J Geriatr Cardiol. 2017;14(8):491–5.
Joint committee for guideline revision. 2016 Chinese guidelines for the management of dyslipidemia in adults. J Geriatr Cardiol. 2018;15(1):1–29.
Samieri C, Perier MC, Gaye B, Proust-Lima C, Helmer C, Dartigues JF, et al. Association of cardiovascular health level in older age with cognitive decline and incident dementia. JAMA. 2018;320(7):657–64.
Gardener H, Caunca M, Dong C, Cheung YK, Alperin N, Rundek T, et al. Ideal cardiovascular health and biomarkers of subclinical brain aging: the northern Manhattan study. J Am Heart Assoc. 2018;7(16):e009544.
Folsom AR, Yatsuya H, Nettleton JA, Lutsey PL, Cushman M, Rosamond WD. Community prevalence of ideal cardiovascular health, by the American Heart Association definition, and relationship with cardiovascular disease incidence. J Am Coll Cardiol. 2011;57(16):1690–6.
Gaye B, Canonico M, Perier MC, Samieri C, Berr C, Dartigues JF, et al. Ideal cardiovascular health, mortality, and vascular events in elderly subjects: the three-city study. J Am Coll Cardiol. 2017;69(25):3015–26.
Effoe VS, Carnethon MR, Echouffo-Tcheugui JB, Chen H, Joseph JJ, Norwood AF, et al. The American heart association ideal cardiovascular health and incident Type 2 diabetes mellitus among blacks: the jackson heart study. J Am Heart Assoc. 2017;6(6):e005008.
Zhou L, Zhao L, Wu Y, Wu Y, Gao X, Li Y, et al. Ideal cardiovascular health metrics and its association with 20-year cardiovascular morbidity and mortality in a Chinese population. J Epidemiol Commun Health. 2018;72(8):752–8.
Bennett DA, Du H, Clarke R, Guo Y, Yang L, Bian Z, et al. Association of physical activity with risk of major cardiovascular diseases in chinese men and women. JAMA Cardiol. 2017;2(12):1349–58.
Fransson EI, Heikkila K, Nyberg ST, Zins M, Westerlund H, Westerholm P, et al. Job strain as a risk factor for leisure-time physical inactivity: an individual-participant meta-analysis of up to 170,000 men and women: the IPD-Work Consortium. Am J Epidemiol. 2012;176(12):1078–89.
(CDC). CfDCaP. Trends in leisure-time physical inactivity by age, sex, and race/ethnicity--United States, 1994–2004. MMWR Morb Mortal Wkly Rep. 2005;54(39):991–4.
Chou LP, Tsai CC, Li CY, Hu SC. Prevalence of cardiovascular health and its relationship with job strain: a cross-sectional study in Taiwanese medical employees. BMJ Open. 2016;6(4):e010467.
Fernandez-Friera L, Fuster V, Lopez-Melgar B, Oliva B, Garcia-Ruiz JM, Mendiguren J, et al. Normal LDL-cholesterol levels are associated with subclinical atherosclerosis in the absence of risk factors. J Am Coll Cardiol. 2017;70(24):2979–91.
Ference BA, Graham I, Tokgozoglu L, Catapano AL. Impact of lipids on cardiovascular health: JACC health promotion series. J Am Coll Cardiol. 2018;72(10):1141–56.
Nissen SE, Nicholls SJ, Sipahi I, Libby P, Raichlen JS, Ballantyne CM, et al. Effect of very high-intensity statin therapy on regression of coronary atherosclerosis: the ASTEROID trial. JAMA. 2006;295(13):1556–65.
Nicholls SJ, Ballantyne CM, Barter PJ, Chapman MJ, Erbel RM, Libby P, et al. Effect of two intensive statin regimens on progression of coronary disease. N Engl J Med. 2011;365(22):2078–87.
Garg PK, O’Neal WT, Chen LY, Loehr LR, Sotoodehnia N, Soliman EZ, et al. American heart association’s life simple 7 and risk of atrial fibrillation in a population without known cardiovascular disease: the ARIC (atherosclerosis risk in communities) study. J Am Heart Assoc. 2018;7(8):e008424.
Younus A, Aneni EC, Spatz ES, Osondu CU, Roberson L, Ogunmoroti O, et al. A systematic review of the prevalence and outcomes of ideal cardiovascular health in US and Non-US populations. Mayo Clin Proc. 2016;91(5):649–70.
Catapano AL, Graham I, De Backer G, Wiklund O, Chapman MJ, Drexel H, et al. 2016 ESC/EAS guidelines for the management of dyslipidaemias. Eur Heart J. 2016;37(39):2999–3058.
Wang Y, Liu J, Wang W, Wang M, Qi Y, Xie W, et al. Lifetime risk for cardiovascular disease in a Chinese population: the Chinese Multi-Provincial Cohort Study. Eur J Prev Cardiol. 2015;22(3):380–8.
Atsma F, Bartelink ML, Grobbee DE, van der Schouw YT. Postmenopausal status and early menopause as independent risk factors for cardiovascular disease: a meta-analysis. Menopause. 2006;13(2):265–79.
Collins P, Webb CM, de Villiers TJ, Stevenson JC, Panay N, Baber RJ. Cardiovascular risk assessment in women - an update. Climacteric. 2016;19(4):329–36.
Wang D, Jackson EA, Karvonen-Gutierrez CA, Elliott MR, Harlow SD, Hood MM, et al. Healthy lifestyle during the midlife is prospectively associated with less subclinical carotid atherosclerosis: the study of women’s health across the nation. J Am Heart Assoc. 2018;7(23):e010405.
Wang N, Shao H, Chen Y, Xia F, Chi C, Li Q, et al. Follicle-stimulating hormone, its association with cardiometabolic risk factors, and 10-year risk of cardiovascular disease in postmenopausal women. J Am Heart Assoc. 2017;6(9):e005918.
Stefanska A, Ponikowska I, Cwiklinska-Jurkowska M, Sypniewska G. Association of FSH with metabolic syndrome in postmenopausal women: a comparison with CRP, adiponectin and leptin. Biomark Med. 2014;8(7):921–30.
Benjamin EJ, Blaha MJ, Chiuve SE, Cushman M, Das SR, Deo R, et al. Heart disease and stroke statistics-2017 update: a report from the American heart association. Circulation. 2017;135(10):e146–603.
Lu J, Lu Y, Wang X, Li X, Linderman GC, Wu C, et al. Prevalence, awareness, treatment, and control of hypertension in China: data from 1.7 million adults in a population-based screening study (China PEACE Million Persons Project). Lancet. 2017;390(10112):2549–58.
Wang L, Gao P, Zhang M, Huang Z, Zhang D, Deng Q, et al. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. JAMA. 2017;317(24):2515–23.
Huang Y, Gao L, Xie X, Tan SC. Epidemiology of dyslipidemia in Chinese adults: meta-analysis of prevalence, awareness, treatment, and control. Popul Health Metr. 2014;12(1):28.
Reiner Z, Sonicki Z, Tedeschi-Reiner E. Physicians’ perception, knowledge and awareness of cardiovascular risk factors and adherence to prevention guidelines: the PERCRO-DOC survey. Atherosclerosis. 2010a;213(2):598–603.
Reiner Z, Sonicki Z, Tedeschi-Reiner E. Public perceptions of cardiovascular risk factors in Croatia: the PERCRO survey. Prev Med. 2010b;51(6):494–6.
Acknowledgments
We would like to thank all the participants for volunteering their time to be involved in this study. We thank for Jun-Jie Yang for his assistance.
Funding
This study was supported by grants from “National Science-technology Support Plan Projects” (Item No. 2011BAI11B00) and “National Prevention and Control of Major Chronic Non-communicable Diseases” Project (Item No. 2016YFC1300304). The funder had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
YDC and XQZ have made substantial contributions to conception and design of the study; All authors contributed to acquisition, analysis, and interpretation of data; TWH, YQL, HWY, JJY, SSZ, JW, and FT contributed to statistical analysis; TWH, YQL, and XQZ wrote the manuscript; YDC, and XQZ revised the manuscript. All authors have read and approved the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Ethics Committee of the Chinese General PLA Hospital and was in accordance with standards set forth by the Declaration of Helsinki. All participants provided their written informed consent before officially entering in the study.
Consent for publication
All participants provided their informed consent.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1
. The 52 participating centers of this study.
Additional file 2
. Questionnaire on cardiovascular risk factors of female physicians.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Han, TW., Liu, YQ., Dong, W. et al. Poor cardiovascular health status among Chinese women. BMC Cardiovasc Disord 20, 497 (2020). https://doi.org/10.1186/s12872-020-01748-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-020-01748-y