Abstract
Objective
Coronary slow flow (CSF) is characterized by delayed opacification of distal epicardial coronary arteries without significant coronary stenosis. In addition, The changes of lipoprotein-associated phospholipase A2 (Lp-PLA2) as a significant predictive factor for CSF remain controversial. The study aims to investigate the association between plasma Lp-PLA2 and CSF.
Methods
In this retrospective study, 170 consecutive patients who underwent coronary angiography were enrolled in Beijing Anzhen Hospital from January 2017 to September 2019, and were divided into CSF group and normal control groups. According to coronary blood flow rate measured by the thrombolysis in myocardial infarction frame count (TFC) method, CSF was defined as TFC > 27. Serum Lp-PLA2 levels were measured in an enzyme-linked immunosorbent assay.
Results
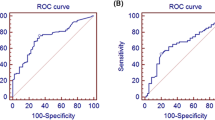
Lp-PLA2 levels were higher in the CSF group than in the control group (288.6 ± 50.3 versus 141.9 ± 49.7, P < 0.001) and were significantly correlated with the mean coronary artery thrombolysis in myocardial infarction (TIMI) frame count (r = 0.790, P<0.001). Logistic regression analysis showed that high Lp-PLA2 was independently associated with CSF after adjustment for conventional risk factors (OR = 1.040, CI = 1.022–1.059, P<0.001). Male sex (OR = 2.192, CI = 1.161–4.140, P = 0.016) and hypertension (OR = 1.965, CI = 1.034–3.736, P = 0.039) were also CSF risk factors. Receiver-operating characteristic curve (ROC) analysis showed that Lp-PLA2 levels can predict CSF severity; the predictive power was higher than the other risk factors.
Conclusion
Our study demonstrated that patients with CSF had higher circulating levels of Lp-PLA2 than normal controls. After adjustment for potential confounders, increased Lp-PLA2 was independently associated with presence of CSF.
Similar content being viewed by others
The coronary slow flow (CSF) phenomenon is a special phenomenon involving coronary microcirculation dysfunction, which is characterized by delayed distal vascular opacification without significant epicardial coronary stenosis. Studies have shown that slow blood flow is often associated with adverse cardiovascular events, including angina, myocardial infarction, malignant arrhythmias and even sudden cardiac death, suggesting a poor prognosis [1]. Although it has been 40 years since Tambe et al. first discovered slow blood flow [2], the exact mechanism of its pathogenesis remains unclear. A large number of studies have shown that the pathogenesis of CSF may involve vascular endothelial dysfunction, vascular inflammation, obesity, atherosclerosis and other factors [3,4,5]. However, there is a lack of effective biomarkers that specifically predict CSF. Recently, a vast majority of evidence has indicated that many inflammatory mediators such as interleukin-1, interleukin-10, and the lymphocyte to monocyte ratio, are associated with the pathogenesis of CSF, indicating the presence of a proinflammatory process occurring as a result of the phenomenon [6,7,8]. Thus, it is of value to identify the risk factors for CSF in order to detect and prevent CSF as early as possible.
Lipoprotein-associated phospholipase A2 (Lp-PLA2), a leukocyte-derived enzyme, is involved in the metabolism of low-density lipoprotein (LDL), propagating atherogenesis, and mediating the inflammatory process of the vascular wall [9]. Lp-PLA2 circulates in plasma in its active form with complexes of LDL and high density lipoprotein (HDL) [10]. Recent evidence suggests that Lp-PLA2 plays an important role in the pathophysiology of atherosclerosis and as a predictive biomarker for predicting future cardiovascular events [11]. According to its properties of proinflammation and atherogenesis, and the fact that increased Lp-PLA2 has been found to be closely associated with inflammation and atherosclerosis, we speculate that Lp-PLA2 may be associated with CSF [12]. Therefore, in this study, our aim was to evaluate the relationship between coronary blood flow and the Lp-PLA2 level.
Methods
Study patients
The retrospective study was carried out from January 2017 to September 2019 at Anzhen Hospital. A total of 170 patients who underwent coronary angiography with clinical chest pain and without significant coronary stenosis were consecutively enrolled in the observational study; 78 of the patients had slow coronary flow without any stenosis evidenced by coronary angiography, and 92 patients had normal coronary arteries and normal flow. Patients with prior evidence of coronary artery disease (acute coronary syndrome, coronary interventions history, coronary plaque and significant atherosclerotic lesions (stenosis above 40%), coronary ectasia, coronary calcification), congenital heart disease, valvular heart disease, cardiomyopathy, ischemic electrocardiogram, hematological system disease, tumors, heart failure, liver dysfunction, or kidney dysfunction or who had recently undergone surgery were excluded from the study. The study was approved by the Beijing An zhen Hospital Ethics Committee of Capital Medical University, and all patients provided informed consent.
Anthropometric and laboratory measurements
The study measured demographic characteristics, including age, sex, height, weight, body mass index (BMI) and waist circumference. Smoking, hypertension, diabetes mellitus and medication use were collected from electronic medical records. After fasting for at least 8 h, peripheral blood was collected on the morning of the first day of admission and stored at − 70 °C. The plasma Lp-PLA2 activity was measured using an enzyme-linked immunoassay (PLAC™ test, DIADEXUS, USA). Glucose, urea, creatinine, total cholesterol (TC), triglyceride (TG), HDL, and LDL levels were measured using a chemiluminescence method with a Roche Diagnostics Cobas analyzer Cobas 8000, c702 module. High sensitivity C-reactive protein (hs-CRP) levels were also measured by the nephelometric method. All samples were tested in triplicate according to the manufacturer’s protocols.
Diagnostic criteria
ACS was diagnosed according to European Society of Cardiology guidelines in 2015 [13]. Cardiomyopathy was diagnosed by established histological, immunological, and immunohistochemical criteria according to the WHO classification [14]. The diagnostic criteria of diabetes mellitus was according to WHO guidelines or by indication for insulin or anti-diabetic medications [15]. Hypertension was defined as repeated systolic pressure ≥ 140 mmHg and/or diastolic pressure ≥ 90 mmHg at least twice, or previously diagnosed hypertension [16].
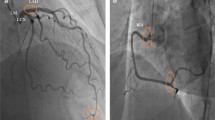
Coronary angiography protocols
CSF was defined according to the thrombolysis in myocardial infarction (TIMI) frame count (TFC) method. Coronary angiogram was performed using a digital subtraction angiography system (Allura Xper FD20; Philips Medical Systems, Best, the Netherlands), which used the standard Judkins technique to obtain images at the rate of 30 frames/s. The injection rate was 4–5 ml/s in the left coronary artery and 3–4 ml/s in the right coronary artery (RCA). The left coronary artery was injected with 8-10 ml contrast agent and RCA was injected with 6-8 ml contrast agent. The left anterior descending coronary artery (LAD) was imaged as the right anterior oblique projection with an angle of 20–25°, the left circumflex coronary artery (LCX) was imaged as the right anterior oblique projection with an angle of 20–25°, and the RCA was imaged as the positive projection with an angle of 30°. The first frame was defined when the contrast agent touched two medial walls of the coronary artery and advanced steadily with a diameter of more than 70%, and the last frame was defined when the leading edge of the contrast agent reached the end of the branches of the coronary artery. The frame counts in the LAD were divided by a factor of 1.7 to correct for its longer length. According to Gibson et al., any frame count over 27 is considered abnormal and indicates significant CSF [17]. All patients were carefully monitored for pulse and blood pressure during coronary angiogram.
Statistical analysis
Data were analyzed with IBM SPSS software version 23.0. Categorical variables were presented as frequencies and percentages, and continuous variables were expressed as the mean and standard deviation. Continuous variables with a normal distribution were compared using Student’s t-test. Kruskal-Wallis test and one-way ANOVA were used to analyze the differences between groups. The categorical variables were tested by chi-square test. Spearman ρ test correlation analysis was used to examine the correlation between Lp-PLA2 and other risk factors. We used multivariate logistic regression analysis to assess the value of Lp-PLA2 in predicting the presence of CSF with adjustment for risk factors. Additionally, a receiver operating characteristic (ROC) curve was plotted for the plasma Lp-PLA2 level to evaluate the ability of the variable to classify the severity of CSF. The ROC curve were calculated in an area under the curve (AUC) and 95% confidence intervals. A P value< 0.05 (two tailed) was considered significant.
Results
Patient characteristics
The baseline clinical characteristics of the study participants are shown in Table 1. We enrolled 170 patients (mean age 61.6 ± 9.7, 60.6% male) who underwent coronary angiography; the sample was composed of 78 patients (mean age 60.2 ± 9.7, 70.5% male) with CSF and 92 patients (mean age 62.7 ± 9.5, 52.1% male) with normal coronary flow (NCF). As shown in Table 1, men were more prevalent in the CSF group than in the NCF group (70.5% versus 52.1%, P = 0.018). However, the other demographic factors, such as age, BMI, waist circumference, prevalence of hypertension, prevalence of diabetes and current smoking, did not differ significantly between the CSF and NCF groups. Except for TGs, TC, and high-density lipoprotein cholesterol (HDL-c), the two groups showed no significant differences in most laboratory tests. The levels of HDL-C and TC were lower in the CSF group than in the NCF group (1.15 ± 0.07 versus 1.49 ± 0.29, P<0.001; 4.32 ± 0.85 versus 4.76 ± 1.01, P = 0.003), and the TG level was significantly higher in the CSF group (1.97 ± 1.57 versus 1.51 ± 0.66, P = 0.020).
Lp-PLA2 levels in the CSF group were significantly higher than those in the control group (288.6 ± 50.3 versus 141.9 ± 49.7, P < 0.001) (Table 1,Fig. 1). The TFC values of the two groups of coronary arteries were calculated respectively. The mean TFCs of LAD, LCX and RCA were significantly higher in CSF patients than in NCF patients (p < 0.001 for each coronary artery, Table 2, Fig. 2).
The spearman analysis, shown in Table 3, showed that the plasma Lp-PLA2 level was positively correlated with mean TFC (r = 0.790, P<0.001) and C-reactive protein (CRP), (r = 0.179, P = 0.019), and negatively correlated with HDL-C (r = − 0.693,P<0.001) and ejection fraction (r = − 0.164, P = 0.033) (Figs. 3, 4). Univariate and multivariate logistic regression analyses were used to explore the associations of risk factors with CSF. The results indicated that the level of Lp-PLA2 (OR = 1.049, CI = 1.034–1.064, P < 0.001), male sex (OR = 2.192, CI = 1.161–4.140, P = 0.016) and hypertension (OR = 1.965, CI = 1.034–3.736, P = 0.039) were risk factors for CSF. After adjustment for traditional confounders, we found that the Lp-PLA2 levels remained to be significantly and independently associated with the presence of CSF (OR = 1.040, CI = 1.022–1.059, P<0.001) (Table 4, Table 5, Fig. 5).
The ROC curve analysis (Fig. 6) showed that Lp-PLA2 (AUC values = 0.978; CI = 0.959–0.993; P < 0.0001) was better in predicting CFS than TC (0.621; CI = 0.537–0.706; P = 0.0064), TG (0.603; CI = 0.518–0.688; P = 0.021), male sex(0.592; CI = 0.506–0.677; P = 0.040)and hypertension (0.576; CI = 0.503–0.645; P = 0.036). The sum of the sensitivity and specificity for the prediction of the extent of CSF was maximal at a level of Lp-PLA2 ≥ 260.5 ng/ml (sensitivity = 76.9% [95% CI 66 to 85.71%], specificity =98.9% [95% CI 94.1 to 99%]).
Discussion
As far as we know, the present study demonstrated for the first time that there was an independent relationship between Lp-PLA2 and CSF phenomenon. The major finding was that Lp-PLA2 levels were positively correlated with CSF and significantly elevated in subjects with CSF. In addition, multivariate logistic regression analysis and ROC curves showed that Lp-PLA2 was still independently associated with the presence and severity of CSF. Male sex and hypertension also independently predicted the presence of the CSF phenomenon.
Although CSF has been found to be related to microvascular diseases, vascular endothelial dysfunction, coronary atherosclerosis, oxidative stress, insulin resistance, adipocytokines, and abnormal blood composition, the exact mechanisms are still unknown [18,19,20]. Tambe proposed that the CSF phenomenon might be related to abnormal microcirculation in 1972 [2]. Oğuzhan Çelik et al. identified a correlation between the extent of disruption in endothelial function and the CSF level using the flow-mediated dilation (FMD) method [21]. Several studies have found that the imbalance between endothelin-1 and nitric oxide in patients with CSF supports the involvement of endothelial dysfunction in CSF etiopathogenesis [22]. An intravascular ultrasound study demonstrated that diffuse coronary calcification was present in 88% of CSF patients, and statin therapy has been shown to improve coronary flow in CSF subjects [23]. Decreased fractional flow reserve in CSF patients has been demonstrated by intravascular ultrasound (IVUS) to result in increased resistance in the epicardial coronary artery due to diffuse atherosclerotic disease [24].
The role of chronic inflammation-mediated endothelial injury in CSF has been widely recognized. Muhammed Oylumlu et al. revealed that the platelet-to-lymphocyte ratio could be an important risk factor in patients with CSF [25]. Li et al. showed that plasma CRP and IL-6 as inflammatory markers were positively correlated with TIMI frame count in patients with CSF [26]. In our study, Lp-PLA2 was shown to be an independent predictor of CSF. Lp-PLA2, known as platelet-activating factor acetylhydrolase, is a calcium-independent serine lipase [10]. Lp-PLA2 is synthesized by macrophages and other inflammatory cells and circulates in the human blood mainly with LDL granules (80–85%) and less often with HDL [9]. Lp-PLA2 is involved in the oxidative modification of vascular wall LDL to generate oxidized phospholipids and oxidized non-esterified fatty acids, which can promote the development of vascular inflammation and atherosclerotic plaques [27]. Lp-PLA2 has been identified as an independent predictor of cardiovascular disease (CVD),and has been recommended as an adjunct to traditional risk assessment in patients with moderate and high 10-year risk of CVD as defined by Framingham risk scores [28]. In the REGARDS study, Lp-PLA2 activity was associated with coronary heart disease (CHD) risk over 5.3 years based on Cox proportional hazards regression [29]. Our study found that in the CSF group, with the increase in TFC, Lp-PLA2 levels exhibited an increasing trend, and there was a significant positive correlation between CSF and Lp-PLA2. Additionally multivariate logistic regression analysis showed that Lp-PLA2 could independently predict CSF. However, the mechanisms underlying the relationship between Lp-PLA2 and CSF are not entirely understood. The most reliable hypothesis seems to be that CSF is caused by increased microvascular resistance induced by endothelial dysfunction due to Lp-PLA2 mediated chronic inflammation.
Numerous studies have attempted to define the demographics, characteristics and independent predictors of patients with CSF. Arbey Y found that current smoking was associated with CSF [30]. Other studies have shown that BMI and hypertension were predictors of CSF phenomena [31]. Compared to other studies, our study did not find an association between BMI and CSF. Our study also shows that Lp-PLA2, male gender,c and hypertension are independent risk factor of the presence of CSF phenomena. Tsimikas found in his study that there was a significant correlation between Lp-PLA2 and LDL, non-HDL, and HDL [11]. However, we did not find any difference in LDL between the two groups, which may be related to the use of lipid-lowering drugs.
Limitations
Our study has some limitations: (1)This study was limited by a small and nonrandomized sample, which may restrict the generalizability of our results. (2)The study did not examine the ethnic background or socioeconomic status of the study population.(3)This study was also a single center, retrospective study. Multicenter randomized controlled trials must be conducted to explore the relationship between Lp-PLA2 and CSF. (4)The use of drugs, such as lipid-lowering drugs, may affect the results of experiments. (5)Finally, we determined only the mass of Lp-PLA2 instead of its activity due to our laboratory limitations.
Conclusion
In summary, the main finding was that Lp-PLA2 levels were positively correlated with CSF. The multivariate regression results showed that Lp-PLA2 was independently associated with the presence and severity of CSF. Currently, there is still no effective method to treat CSF. This study indicated the association between Lp-PLA2 and CSF, which may provide a new therapeutic target for the treatment of CSF. However, the exact pathophysiological mechanisms of Lp-PLA2 in CSF require further study to elucidate.
Availability of data and materials
The data and materials can be used with permission.
Abbreviations
- CSF:
-
Coronary slow flow
- Lp-PLA2 :
-
Lipoprotein-associated phospholipase A2
- TFC:
-
Thrombolysis in myocardial infarction frame count
- RCA:
-
Right coronary artery
- LCX:
-
Left circumflex coronary artery
- LAD:
-
Left anterior descending coronary artery
- CVD:
-
Cardiovascular disease
- TC:
-
Total cholesterol
- TG:
-
Triglyceride
- HDL-C:
-
High-density lipoprotein cholesterol
- LDL-C:
-
Low-density lipoprotein cholesterol
- HbA1c:
-
Glycosylated hemoglobin A1c
- FBG:
-
Fasting blood glucose
- BMI:
-
Body mass index
- CRP:
-
C-reactive protein
- ROC:
-
Receiver-operating characteristic curve
References
Horjeti B, Goda A. Acute ischemia manifestation in a patient with coronary slow flow phenomenon. J Electrocardiol. 2012;45(3):277–9.
Tambe AA, Demany MA, Zimmerman HA, Mascarenhas E. Angina pectoris and slow flow velocity of dye in coronary arteries--a new angiographic finding. Am Heart J. 1972;84(1):66–71.
Jin Z, Tan Q, Sun B. Telmisartan ameliorates vascular endothelial dysfunction in coronary slow flow phenomenon (CSFP). Cell Biochem Funct. 2018;36(1):18–26.
Yilmaz M, Korkmaz H, Bilen MN, Uku O, Kurtoglu E. Could neutrophil/lymphocyte ratio be an indicator of coronary artery disease, coronary artery ectasia and coronary slow flow? J Int Med Res. 2016;44(6):1443–53.
Hawkins BM, Stavrakis S, Rousan TA, Abu-Fadel M, Schechter E. Coronary slow flow--prevalence and clinical correlations. Circ J. 2012;76(4):936–42.
Yayla C, Akboga MK, Gayretli Yayla K, Ertem AG, Efe TH, Sen F, Unal S, Acar B, Ozcan F, Turak O, et al. A novel marker of inflammation in patients with slow coronary flow: lymphocyte-to-monocyte ratio. Biomark Med. 2016;10(5):485–93.
Mutluer FO, Ural D, Gungor B, Bolca O, Aksu T. Association of Interleukin-1 gene cluster polymorphisms with coronary slow flow phenomenon. Anatolian J Cardiol. 2018;19(1):34–41.
Shi GL, Cai XX, Su YM, Chen C, Deng XT, Pan HY, Fan MK, Zhu JH, Pan M. Interleukin-10 promotor -592A/C polymorphism is associated with slow coronary flow in Han Chinese. Int J Clin Exp Pathol. 2015;8(4):4091–8.
Silva IT, Mello AP, Damasceno NR. Antioxidant and inflammatory aspects of lipoprotein-associated phospholipase a(2) (Lp-PLA(2)): a review. Lipids Health Dis. 2011;10:170.
Stafforini DM. Plasma PAF-AH (PLA2G7): biochemical properties, association with LDLs and HDLs, and regulation of expression. Enzymes. 2015;38:71–93.
Acevedo M, Varleta P, Kramer V, Valentino G, Quiroga T, Prieto C, Parada J, Adasme M, Briones L, Navarrete C. Comparison of lipoprotein-associated phospholipase A2 and high sensitive C-reactive protein as determinants of metabolic syndrome in subjects without coronary heart disease: in search of the best predictor. Int J Endocrinol. 2015;2015:934681.
Ballantyne CM, Hoogeveen RC, Bang H, Coresh J, Folsom AR, Heiss G, Sharrett AR. Lipoprotein-associated phospholipase A2, high-sensitivity C-reactive protein, and risk for incident coronary heart disease in middle-aged men and women in the atherosclerosis risk in communities (ARIC) study. Circulation. 2004;109(7):837–42.
Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, Bax JJ, Borger MA, Brotons C, Chew DP, et al. 2015 ESC guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: task force for the Management of Acute Coronary Syndromes in patients presenting without persistent ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2016;37(3):267–315.
Richardson P, McKenna W, Bristow M, Maisch B, Mautner B, O'Connell J, Olsen E, Thiene G, Goodwin J, Gyarfas I, et al. Report of the 1995 World Health Organization/international society and Federation of Cardiology Task Force on the definition and classification of cardiomyopathies. Circulation. 1996;93(5):841–2.
Alberti KG, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part 1: diagnosis and classification of diabetes mellitus provisional report of a WHO consultation. Diab Med. 1998;15(7):539–53.
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the eighth joint National Committee (JNC 8). Jama. 2014;311(5):507–20.
Gibson CM, Cannon CP, Daley WL, Dodge JT Jr, Alexander B Jr, Marble SJ, McCabe CH, Raymond L, Fortin T, Poole WK, et al. TIMI frame count: a quantitative method of assessing coronary artery flow. Circulation. 1996;93(5):879–88.
Tasolar H, Eyyupkoca F, Akturk E, Karakus Y, Cansel M, Yagmur J, Ozyalin F, Altun B, Pekdemir H. Endothelial nitric oxide synthase levels and their response to exercise in patients with slow coronary flow. Cardiovasc J Afr. 2013;24(9–10):355–9.
Akboga MK, Canpolat U, Balci KG, Akyel A, Sen F, Yayla C, Cay S, Aras D, Aydogdu S. Increased platelet to lymphocyte ratio is related to slow coronary flow. Angiology. 2016;67(1):21–6.
Demir B, Caglar IM, Tureli HO, Pirhan O, Aciksari G, Serkan C, Cem O, Gedikbasi A, Zorkun C, Demir E, et al. Coronary slow flow phenomenon associated with high serum levels of soluble CD40 ligand and urotensin II: a multi-marker approach. Clin Lab. 2014;60(11):1909–20.
Li Y, Zhang H, Liang Y, Wang W, Xu T, Zhang J, Xiao W, Wang T. Effects of hyperbaric oxygen on vascular endothelial function in patients with slow coronary flow. Cardiol J. 2018;25(1):106–12.
Pekdemir H, Polat G, Cin VG, Camsari A, Cicek D, Akkus MN, Doven O, Katircibasi MT, Muslu N. Elevated plasma endothelin-1 levels in coronary sinus during rapid right atrial pacing in patients with slow coronary flow. Int J Cardiol. 2004;97(1):35–41.
Camsari A, Ozcan T, Ozer C, Akcay B. Carotid artery intima-media thickness correlates with intravascular ultrasound parameters in patients with slow coronary flow. Atherosclerosis. 2008;200(2):310–4.
Pekdemir H, Cin VG, Cicek D, Camsari A, Akkus N, Doven O, Parmaksiz HT. Slow coronary flow may be a sign of diffuse atherosclerosis. Contribution of FFR and IVUS. Acta Cardiol. 2004;59(2):127–33.
Oylumlu M, Dogan A, Oylumlu M, Yildiz A, Yuksel M, Kayan F, Kilit C, Amasyali B. Relationship between platelet-to-lymphocyte ratio and coronary slow flow. Anatolian J Cardiol. 2015;15(5):391–5.
Li JJ, Qin XW, Li ZC, Zeng HS, Gao Z, Xu B, Zhang CY, Li J. Increased plasma C-reactive protein and interleukin-6 concentrations in patients with slow coronary flow. Clin chim Acta. 2007;385(1–2):43–7.
Di Pietro N, Formoso G, Pandolfi A. Physiology and pathophysiology of oxLDL uptake by vascular wall cells in atherosclerosis. Vasc Pharmacol. 2016;84:1–7.
Davidson MH, Corson MA, Alberts MJ, Anderson JL, Gorelick PB, Jones PH, Lerman A, McConnell JP, Weintraub HS. Consensus panel recommendation for incorporating lipoprotein-associated phospholipase A2 testing into cardiovascular disease risk assessment guidelines. Am J Cardiol. 2008;101(12a):51f–7f.
De Stefano A, Mannucci L, Massoud R, Bernardini S, Cortese C. Performance characteristics of lipoprotein-associated phospholipase A2 activity assay on the dimension vista analyser and preliminary study of a healthy Italian population. Biochem Med. 2017;27(3):030701.
Arbel Y, Rind E, Banai S, Halkin A, Berliner S, Herz I, Mashav N, Thurm T, Keren G, Finkelstein A. Prevalence and predictors of slow flow in angiographically normal coronary arteries. Clin Hemorheol Microcirc. 2012;52(1):5–14.
Sanati H, Kiani R, Shakerian F, Firouzi A, Zahedmehr A, Peighambari M, Shokrian L, Ashrafi P. Coronary slow flow phenomenon clinical findings and predictors. Res Cardiovasc Med. 2016;5(1):e30296.
Acknowledgements
Not applicable.
Funding
This work was supported by grants 81573744, 81973841 from the China National Natural Scientific Foundation.
Author information
Authors and Affiliations
Contributions
Y-DD carried out the experiments, acquired the data and wrote the first draft of the paper; Y-QP carried out the experiments and wrote sections of the manuscript; Y-XZ, X-LL, HS and QM recruited the subjects, performed the patients assessments and critically reviewed the paper for intellectual content. Y-DD, Y-QP, R-W, J-XY and SZ performed the statistical analyses; H-LG conceived and designed the study and handled funding and supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Beijing Anzhen Hospital Ethics Committee of Capital Medical University, and all participants signed an informed consent form.
Consent for publication
All participants provided written informed consent before enrollment in this study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ding, Yd., Pei, Yq., Wang, R. et al. Increased plasma lipoprotein-associated phospholipase A2 levels are associated with coronary slow flow. BMC Cardiovasc Disord 20, 248 (2020). https://doi.org/10.1186/s12872-020-01463-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-020-01463-8