Abstract
Background
Complete heart blocks underwent to permanent pacemaker placement are a common complication of tricuspid valve replacement (TVR). If indicated, endocardial placement of a right ventricular (RV) lead is precluded in the presence of mechanical TVR.
Case presentation
A 20-year-old female patient firstly underwent metallic prosthetic valve operation with tricuspid valve endocarditis in 2014. Three years after the operation, echocardiography revealed dysfunction of the prosthetic valve thus reoperation was decided. In the second operation, the patient underwent a bioprosthesis valve and AV complete block developed in the postoperative period. Left ventricular ejection fraction (EF) was 45% was found on echocardiography. Pacemaker dependence of the patient, it was aimed to place two electrodes into the left ventricle. Electrodes were placed the target two branches in coronary sinus (CS) and right atrium. Univentricular bifocal pacing was enabled to work.
Conclusion
Electrode placement in the CS is a very good alternative to epicardial surgical lead placement in cases where endocardial lead placement from the right atrium to the RV is contraindicated. In patients with lower left ventricular EF who will be pacemaker dependent, the insertion of two electrodes into the CS to prevent pacemaker is a safe and effective treatment.
Similar content being viewed by others
Background
Complete heart blocks underwent to permanent pacemaker placement are a common complication of tricuspid valve replacement (TVR) [1]. If indicated, endocardial placement of a right ventricular (RV) lead is precluded in the presence of mechanical TVR [1]. For the procedure of endocardial lead placement, tilting disk valve prosthesis is the absolute contraindication due to the risk of acute valve failure, damage to the lead, and death [2]. In the routine clinical practice transvenous RV endocardial lead placement is performed. However, the tendency to replace ventricular lead is through away via the epicardial approach or via the coronary sinus (CS) in most of these cases [3]. Epicardial pacemaker lead implantation which is performed via thoracotomy is usually associated with high threshold occurrence [4]. We present an univentricular bifocal pacemaker implantation in a patient who underwent tricuspid valve surgery twice and developed complete AV block after the second operation.
Case presentation
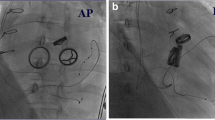
A 20-year-old female patient firstly underwent metallic prosthetic valve operation with tricuspid valve endocarditis in 2014. Three years after the operation, complaints of resistant ascites and dyspnea had been started. Electrocardiography (ECG) sinus rhythm revealed that the PR interval and QRS width were normal and there were no pathological ST-T wave changes. Echocardiography showed that the prosthetic tricuspid valve leaflets did not open and the maximum and mean gradients on the valve were 17 and 8 mmHg, respectively. Echocardiography revealed that prosthetic valve was dysfunctional thus reoperation was decided. In the second operation, a 27 mm St Jude Medical Epic porcine bioprosthetic valve was implanted in the patient and AV complete block developed in the postoperative period. Left ventricular ejection fraction (EF) was 45% and left ventricular dyssynchrony was found on echocardiography performed under transient pacemaker. Due to the low EF and pacemaker dependence of the patient, it was aimed to place two electrodes into the left ventricle and therefore reducing dyssynchrony. The patient underwent 3 left subclavian punctures and two simultaneous access systems were placed in the CS. In the CS angiography, lateral branch and middle cardiac veins were targeted (Fig. 1: a. Coronary sinus angiography, b. Two coronary sinus sheaths, c-d. Right atrium and coronary sinus electrodes). Electrodes were placed on the target two branches and right atrium. Threshold was below 1 V in both branches. When the CS was paced separately from the lateral branch and middle cardiac vein, the QRS duration was found as 200 ms. However, when the CS was paced simultaneously from the lateral branch and middle cardiac vein (univentricular bifocal pacing), the QRS duration was 160 ms (Fig. 2: Electrocardiography, a. Coronary sinus lateral branch pacing, b. Coronary sinus middle cardiac vein pacing, c. Univentricular bifocal pacing). Echocardiographic control at first month showed that EF was 50%. QRS width did not change during follow-up. Prosthetic valve function was normal in the 2-year follow-up of the patient, EF was around 55% and pacemaker measurements are within normal limits. Atrial pacing was not required in pacemaker control but there were intermittent episodes of paroxysmal atrial fibrillation, longest one being 46 h.
Discussion and conclusions
The permanent pacemaker is applied in less than 1% rates after coronary artery bypass grafting and in between 3 to 6% rates after valve interventions according to the type of operation [2]. Transvenous right ventricular endocardial pacing lead might complicate to acute valvular dysfunction in such mechanical tricuspid prosthetic valves, therefore it shouldn’t be preferred [5]. In the past methods epicardial lead implantation was commonly performed via the anterolateral thoracotomy or sternotomy [5]. It was widely known that these highly invasive methods had many surgical risks [5]. Additionally, in these cases the need for reoperation is associated with significant risks, longer hospital stay time, and a high lead failure rate [5]. It was reported that, the epicardial leads cause high pacing thresholds on follow-up [6]. Transvenous left ventricular epicardial lead implantation through coronary vein is much less invasive than the surgical epicardial implantation [6].
In various case reports, usage of great and middle cardiac vein for permanent pacing in cases with tricuspid prosthesis was written. Anagnostopoulos et al. made the first successful left ventricular permanent pacing by using the great cardiac vein in 1970 [7]. Successful outcome was reported by Hansky et al. for left ventricular pacing in seven patients having TVR and one patient after tricuspid valve repair. There were no complications seen, also all devices had proper function [5].
Sirinivasan et al. placed defibrillated lead into CS in a patient with TVR and implantable cardioverter defibrillator indication for ventricular tachycardia [8]. The RV lead that was present before the TVR and that remained behind the prosthetic valve was also used to be worked as a biventricular pace [8]. The patient’s QRS decreased from 186 ms to 142 ms [8].
Vijayakumar et al. placed a VVI pacemaker via electrode inserted into the CS, on a patient with TVR due to a high threshold of epicardial lead which was placed during the operation [4].
Jokinen et al. intervened 136 tricuspid valves over 15 years and followed the patients for 7.9 ± 4.1 years [2]. The incidence of pacemaker placement was 21% (28 of 136 patients) after TV operation. This rate was apparently higher than the other valve interventions [2]. Before hospital discharge 54% of cases (15/28 patients) had pacemaker implantation. Whereas after hospital discharge, nearly half of them (13/28 patients) underwent implantation [2].
Electrode placement in the CS is a very good alternative to epicardial surgical lead placement in cases where endocardial lead placement from the right atrium to the RV is contraindicated. Different case reports suggest that a VVI or DDD pacemaker can be safely implanted via CS in the presence of a mechanical TVR. Our case had undergone tricuspid valve operation twice and right ventricular pacemaker implantation was contraindicated for her. As the patient had 45% left ventricular EF, it was thought to be she would be pace-dependent and this univentricular pace could further impair left ventricular performance. Two electrodes were placed in the CS. It was enabled to work as a univentricular bifocal pacemaker. QRS was measured as 160 ms on ECG after the procedure.
In patients with lower left ventricular EF who will be pacemaker dependent, the insertion of two electrodes into the CS to prevent pacemaker syndrome and prevention of dyssynchrony is a safe and effective treatment.
Availability of data and materials
The data used İn the literature review are available from the corresponding author on reasonable request.
Abbreviations
- CS:
-
Coronary sinus
- ECG:
-
Electrocardiography
- EF:
-
Ejection fraction
- RV:
-
Right ventricle
- TVR:
-
Tricuspid valve replacement
References
Tavoosi A, Babvaynezhad M, Shamsali Z. A hybrid dual-chamber pacemaker in mechanical tricuspid valve prosthesis. J Innov Card Rhythm Manag. 2013;4:1264–5.
Jokinen JJ, Turpeinen AK, Pitkänen O, Hippeläinen MJ, Hartikainen JEK. Pacemaker therapy after tricuspid valve operations: implications on mortality, morbidity, and quality of life. Ann Thorac Surg. 2009;87:1806–15.
Coulson JD, Pitlick PT, Stinson EB, Shumway NE, Baum D. 122 heart block complicating tricuspid valve replacement in children. Pediatric Res. 1981;15:460–1.
Vijayakumar M, Kamath P, Pai PG. Permanent pacing in a patient with tricuspid prosthesis-widening therapeutic use of coronary sinus. Indian Heart J. 2013;65:611–3.
Lee PT, Chen JY, Tsai LM, Li YH, Lin LJ. Transvenous left ventricular Epicardial pacing in a patient with tricuspid mechanical prosthesis. Acta Cardiol Sin. 2011;27:207–9.
Ząbek A, Małecka B, Tomala I, Matusik P, Boczar K, Lelakowski J. Cardiac pacing in a patient with mechanical tricuspid valve. Pol Arch Med Wewn. 2015;125(1–2):89–91.
Anagnostopoulos CE, Patel B, Fenn JE, Stansel HC. Transvenous coronary sinus pacemaker: new primary approach to heart block in patients with tricuspid prostheses. Ann Thorac Surg. 1970;3:248–52.
Srinivasan NT, Segal OR. Biventricular pacing and coronary sinus ICD lead implantation in a patient with a mechanical tricuspid valve replacement. J Cardiol Cases. 2015;12:180–2.
Acknowledgements
Not Applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
This article is a single author. The whole treatment process and the writing of the manuscript were done by me. The author read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The patient has given a written consent of anonymous use of the clinical data for academic use, research purposes and publications.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent form is available.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Yolcu, M. Simultaneous pacing from two branches of coronary sinus in a patient with prosthetic tricuspid valve and complete heart block. BMC Cardiovasc Disord 20, 69 (2020). https://doi.org/10.1186/s12872-020-01373-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-020-01373-9