Abstract
Background
Previous randomized controlled trials (RCT)s showed similar outcomes in patients with atrial fibrillation (AF) and heart failure with reduced ejection fraction (HFrEF) treated with anti-arrhythmic drugs (AAD) compared to rate control therapy. We sought to evaluate whether catheter ablation is superior to medical therapy in patients with AF and HFrEF.
Methods
We searched electronic databases for all RCTs that compared catheter ablation and medical therapy (with or without use of AAD). We used random-effects models to summarize the studies. The primary end-point was all-cause mortality. Secondary outcomes included heart failure-related hospitalizations and change in left ventricular ejection fraction (LVEF).
Results
We retrieved and summarized 7 randomized controlled trials, enrolling 856 patients (429 in the catheter ablation arm and 427 in the medical therapy arm). Compared with medical therapy (including use of AAD), AF catheter ablation was associated with a significant reduction in mortality (risk ratio 0.50; 95% confidence interval [CI]: 0.34 to 0.74; P = 0.0005) and heart failure-related hospitalizations (risk ratio 0.56; 95% CI: 0.44 to 0.71; P < 0.0001). Furthermore, catheter ablation led to significant improvements in LVEF (weighted mean difference, 7.48; 95% CI: 3.71 to 11.26; P < 0.0001).
Conclusions
Compared to medical therapy, including use of AAD, catheter ablation for AF was associated with a significant reduction in mortality and heart failure-related hospitalizations as well as an improvement in LVEF in patients with HFrEF. Larger trials are needed to confirm whether rhythm control with ablation is superior to rate control in patients with AF and heart failure.
Similar content being viewed by others
Introduction
Atrial fibrillation (AF) and heart failure with reduced ejection fraction (HFrEF) are two of the most commonly encountered cardiac diseases and are inextricably linked [1]. They often occur concurrently [2], with each condition perpetuating the other and are both associated with significant morbidity and mortality [3]. AF may perpetuate HFrEF through decreased cardiac output, worsening the neurohormonal response, functional mitral annular enlargement with resultant mitral regurgitation as well as by tachycardia-induced cardiomyopathy [4,5,6,7,8].
Rhythm control with anti-arrhythmic drugs (AADs) did not improve outcomes compared to rate control in the AFFIRM trial [9]. Two large trials were performed comparing AAD to rate control in patients with AF and HFrEF [10, 11]. In the AF-CHF trial, compared to rate control rhythm control with amiodarone did not reduce cardiovascular mortality or hospitalization [11]. In the DIAMOND trial, dofetilide resulted in greater cardioversion to and maintenance of sinus rhythm compared to rate control medical therapy. Although dofetilide did not reduce mortality, patients in whom sinus rhythm was restored and maintained had improved survival compared to the other patients who remained in AF [10].
The degree of rhythm control achieved with AADs is suboptimal and AADs may have several side effects [12, 13]. Catheter ablation is superior to AADs in providing rhythm control in patients with AF [14,15,16,17]. In addition, catheter ablation has been shown to improve functional status and quality of life as well as reduce hospitalizations [14, 18] and health resource utilization [19]. Furthermore, catheter ablation is a relatively safe procedure with a low incidence of major adverse events [20]. The potential benefit of catheter ablation in patients with AF and HFrEF has not been fully elucidated. Several observational studies of catheter ablation in patients with HFrEF reported that maintenance of sinus rhythm by catheter ablation can improve left ventricular ejection fraction, functional status as well as reduce heart failure hospitalizations [21,22,23,24]. In a meta-analysis of observational studies, catheter ablation resulted in improved LVEF compared to rate control [25].
We aimed to assess the efficacy and safety of catheter ablation compared to medical therapy in patients with AF and HFrEF by performing a systematic review and meta-analysis of randomized controlled trials.
Methods
Search strategy
This systematic review was performed according to the guidelines described in the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) statement. We searched PubMed, Embase, and Cochrane Central Register of Clinical Trials using the terms: atrial fibrillation, persistent atrial fibrillation, ablation, catheter ablation, pulmonary vein isolation, heart failure, heart failure with reduced ejection fraction, congestive heart failure, left ventricular dysfunction, impaired left ventricular systolic function, reduced left ventricular systolic function, low ejection fraction, functional capacity, and quality of life. Our search was limited to human studies in peer-reviewed journals from inception to February 26th, 2018. No language restriction was applied. Hand searching with cross-references of retrieved publications, review articles and guidelines was also performed to ensure the inclusion of all relevant studies.
Study selection
The studies had to fulfil the following criteria to be included in the analysis: (i) the study was a randomized controlled trial; (ii) the intervention arm was composed of patients undergoing radio-frequency ablation or cryoablation for AF; (iii) included a control group of medical therapy. The medical therapy control group could be either rate control with medications or atrioventricular nodal ablation with pacing, or rhythm and rate control with amiodarone (iv) follow-up duration of at least six months; and (v) reported at least one outcome of interest. The use of amiodarone was included given guideline recommendations for its possible use for rate control in addition to its role as the main anti-arrhythmic drug for rhythm control in patients with HFrEF [26, 27].
Data extraction
Two investigators (A.A.T. and A.D.) independently performed the initial screening of titles and abstracts to identify potentially relevant articles. Review articles, case reports, meeting abstracts and duplicates were excluded. The full-text of selected articles was independently assessed by two inBCD90998vestigators (A.A.T. and A.D.) to determine relevance for inclusion. Conflicts were resolved by consensus and if necessary by additional discussion with a third author (R.P.). Extracted study and patient characteristics included data regarding study characteristics, baseline patient characteristics, procedural characteristics as well as the number of events for categorical outcomes in both arms and means and standard deviations for continuous outcomes. If this information was not reported in the published article, we contacted the corresponding author of the study for further details.
Quality assessment
We evaluated quality of included RCTs by using the Risk of Bias Tool developed by the Cochrane Collaboration. For each RCT, 2 reviewers (A.A.T. and A.D.) independently assigned a score of high, low, or unclear to each of the following domains: sequence generation; allocation concealment; blinding of participants, personnel, and outcome assessors; incomplete outcome data; selective outcome reporting; and other potential sources of bias. Disagreements were resolved by consensus. We included all eligible RCTs regardless of their assessed quality.
Primary and secondary outcomes
The primary end-point was all-cause mortality. Secondary outcomes included heart failure hospitalizations, change in LVEF, change in six-minute walk test distance and change in Minnesota living with heart failure (MLWHF score). Outcomes were collected at the end of study follow-up.
Statistical analysis
Descriptive statistics are presented as means and standard deviations (SD) for continuous variables or number of cases (n) and as percentages (%) for dichotomous and categorical variables. Publication bias was assessed visually using a funnel plot and quantified using Egger’s test for small study effects. Heterogeneity among studies was assessed using the inconsistency index (I2) statistic, which ranges from 0 to 100%. I2 is defined as the percentage of the observed inter-trial variability that is due to heterogeneity (true difference between trials) rather than chance for each outcome; I2 > 50% denotes significant heterogeneity. The results are presented as risk ratios with 95% confidence intervals (CIs) for calculated categorical outcomes using the total number of events reported in each included trial. For continuous outcomes weighted mean differences with 95% CIs were used using the means and standard deviations reported in each included trial. Data used was based on an intention to treat analysis. Random-effect models were used for all reported outcomes. All statistical analyses were performed with the use of STATA software version 14.3 (College Station, TX: StataCorp LP) and Statsdirect version 3 (England: StatsDirect Ltd. 2013). Two-tailed probability values of < 0.05 were considered significant.
Sensitivity analysis
Influence analyses using random-effects models were performed to assess the effect of each trial on metanalytic results. In addition, we performed a sensitivity analysis excluding trials that allowed AAD therapy in the comparison group. For LVEF assessment, we performed sensitivity analyses restricting follow up to 6–12 months as well as excluding the study that used a LVEF of less than 50% as an entry cut-off.
Results
Study selection
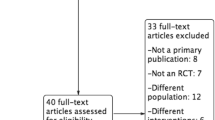
The search strategy identified 1868 abstracts, out of which 1822 were removed after title and abstract review (Fig. 1). Forty-six full-text manuscripts were assessed for eligibility. Seven studies (Table 1) fulfilled the inclusion criteria and were included in the present meta-analysis [28,29,30,31,32,33,34]. Thirty-nine studies were excluded from the final analysis because they did not meet the inclusion criteria: 30 were observational studies, four were review articles and five were meta-analyses.
Quality assessment
Overall there was a low risk of bias. The risks of bias of the included studies are shown in Table 2. No publication bias was suggested by the funnel plots or Egger’s test (Fig. 2 and Table 3). All were multicenter trials done according to the intention-to-treat principle.
Patient characteristics
The efficacy and safety of catheter ablation of AF in HFrEF was analyzed in seven randomized controlled studies that enrolled 856 patients including 429 in the catheter ablation arm and 427 in the rate control arm [28,29,30,31,32,33,34]. The mean age of patients included in the trials ranged from 57.4 ± 11.0 to 64 ± 8 years. The proportion of men in the studies was 84.4%. The mean proportion of patients with ischemic cardiomyopathy was 47.6%. Mean LVEF was 28% and mean NYHA class was 2.5. Baseline patient characteristics are summarized in Table 4.
Catheter ablation protocols
All studies used radiofrequency ablation exclusively except for one trial which left the ablation system to the discretion of the operator. One study incorporated contact force technology. Pulmonary vein isolation was the standard ablation strategy used. Six studies used additional linear lesions [28,29,30,31,32, 34], with two studies aiming for left atrial posterior wall isolation [28, 34], while in the remaining study the entire strategy was left to the discretion of operators, who were required to have performed at least 50 ablations previously [33].
Arrhythmia free survival
We assessed arrhythmia-free survival at the end of follow-up as the measure of success of catheter ablation in maintaining sinus rhythm. Six of the seven included trials reported arrhythmia-free survival. With the exception of the study by McDonald et al. [32], which reported an arrhythmia free survival of 50%, all other studies reported an arrhythmia free survival of over 70% at the end of follow-up [28,29,30,31, 33, 34]. The highest reported survival was 92% in the study reported by Hunter et al. [29]. At the longest reported follow-up, 37 months in CASTLE-AF, the arrhythmia free-survival rate was 75% in patients who underwent catheter ablation.
Clinical outcomes
All trials reported data on clinical outcomes, mortality and heart failure hospitalization, at the end of study follow-up. AF catheter ablation was associated with a significant reduction in mortality (risk ratio [RR] 0.50; 95% CI: 0.34 to 0.74; P = 0.0005) (Fig. 3) and heart failure hospitalizations (RR 0.56; 95% CI: 0.44 to 0.71; P < 0.0001) (Fig. 4) compared to a medical therapy strategy. No heterogeneity was detected (I2 = 0%) and there was no evidence of publication bias.
Left ventricular ejection fraction
Al trials reported data on change in LVEF. Compared with medical therapy including AAD, AF catheter ablation was associated with a significant increase in LVEF (weighted mean difference, 7.48; 95% CI: 3.71 to 11.26; P < 0.0001) (Fig. 5). These results were consistent across all seven trials. There was significant heterogeneity (I2 = 97%) but no evidence of publication bias. When restricted to 6–12 month follow up, catheter ablation was also associated with an increase in LVEF (weighted mean difference, 7.00; 95% CI: 5.02 to 8.99; P < 0.0001); there was no heterogeneity (I2 = 0%) when follow-up was restricted to 6–12 months. When only pure rate control strategies were considered (exclusion of comparison with any amiodarone use in Di Biase et al. [28] and Marrouche et al. [33]), five trials reported data and catheter ablation was associated with an increase in LVEF (weighted mean difference, 8.53; 95% CI: 6.54 to 10.51; P < 0.0001; I2 = 0%).
Functional capacity and quality of life
All trials reported on functional capacity using the 6MWT and five trials reported on quality of life using the MLWHF questionnaire. There was a significant improvement in 6MWT performance (weighted mean difference, 30.15; 95% CI: 10.47 to 49.84; P < 0.0001) (Fig. 6) and MLWHF questionnaire scores (weighted mean difference, − 9.53; 95% CI: –14.67 to − 4.38; P < 0.0001) (Fig. 7) in the AF catheter ablation group versus the medical therapy group.
Complications
Peri-procedural complications were reported by all seven trials. The overall incidence of was 7.3% (95% CI 3.4–11.3%), with bleeding complications occurring in 2.4% of the patients (95% CI 0.9–3.9%). Bleeding complications occurred in eight patients with pericardial effusion; five required immediate intervention and three patients with groin hematoma. Ablation related complications are summarized in Table 5.
Sensitivity analysis
The sensitivity analysis was consistent with the base-case analysis. An influence analysis with sequential exclusion of each study did not change the study outcomes of mortality, heart failure-related hospitalization, LVEF, 6MWT and MLWHF score. When trials that allowed AAD use in the medical therapy group were excluded (Di Biase et al. [28] and Marrouche et al. [33], there was no significant difference in mortality or heart failure-related hospitalization (although limited sample size with very low number of events to compare). In contrast, the improvement in LVEF, 6MWT and MLWHF score persisted.
Discussion
The primary finding of this meta-analysis, of patients with AF and ambulatory HFrEF with a mean NYHA of 2.5, is a significant reduction in all-cause mortality and heart failure hospitalizations in patients undergoing catheter ablation compared to those who receive medical therapy including AAD. In addition, there was a significant improvement in LVEF in patients who undergo catheter ablation. This benefit was consistent and similar in magnitude across all included trials including those with longer term follow up [28,29,30,31,32,33,34]. There was no heterogeneity in clinical outcomes but significant heterogeneity in LVEF and 6MWT assessment. This likely reflects the heterogeneity in testing as well as the varying degrees of follow-up. However, in all the included studies, the results for clinical outcome and change in LVEF functional assessment was consistently in favor of catheter ablation. The results of this study are in keeping with the current guidelines that state that catheter ablation of AF in patients with HF is an effective and acceptable therapeutic option and recommend its use for similar indications as for patients without HFrEF [35].
The deleterious effects of AF are well established, especially the increased risk of stroke. Recent evidence has shown that the complications of AF extend beyond stroke and include an increased risk of mortality, myocardial infarction as well as increased heart failure incidence and hospitalizations. In a large population-based administrative database, Ionescu-Ittu et al. showed that patients with a rhythm control strategy for AF had lower mortality over long-term follow-up [36]. In a large prospective cohort study of 15,400 patients with AF, 11% died at one-year follow-up, with heart failure being the commonest cause of death [37]. In a large meta-analysis of 104 studies involving 9,686,513 patients of whom 587,867 had AF, the presence of AF was associated with a two-fold increase in mortality and a five-fold increase in heart failure [38]. Therefore, given the increased risk of cardiovascular events in the HFrEF population and AF [39], the current meta-analysis suggest that restoring sinus rhythm by catheter ablation reduces mortality and heart failure-related hospitalizations.
The beneficial effect of catheter ablation on LVEF has been consistent across meta-analyses of observational studies and small randomized studies [25, 40]. We demonstrated a mean difference in LVEF improvement of 7.5%. This improvement was consistent across all RCTs and only marginally lower than 11.0% improvement seen in observational studies [25]. As mentioned, the high degree of heterogeneity is likely due to variants in LVEF measurement methods which may be observer dependent as well as due to the differences in duration of follow-up. This was corroborated by the analysis of the 5 trials with 12 months or less of follow-up which showed a similar improvement in LVEF but no heterogeneity. An influence analysis with exclusion of each trial did not change the results of our analysis. Furthermore, the similar results with exclusion of studies that used amiodarone or AV node ablation with ventricular pacing supported the validity of our results. While one study suggested an improvement in LVEF with pharmacological rhythm control [41], this was not corroborated in other studies [42, 43] nor in a meta-analysis [44]. Our finding of consistent improvement in LVEF with catheter ablation in all the RCTs evaluated is likely explained by the superiority of catheter ablation in maintenance of sinus rhythm in comparison to anti-arrhythmic drugs for LVEF [45]. Furthermore, the correlation between improvement in LVEF and clinical outcomes with catheter ablation, as well as the lack of improvement of LVEF and clinical outcomes with AAD, reinforces the value of LVEF as a surrogate marker for clinical outcomes [46, 47].
Interestingly, the proportion of patients who remained in sinus rhythm was relatively high especially considering that most patients had prior persistent AF. The proportions of patients who remained in sinus rhythm ranged from 80 to 90% at one year follow up to 70 and 63% at two and five years follow up respectively. This likely reflects the considerable improvement in technique and the ability of catheter ablation to maintain sinus rhythm even in cases with HFrEF and persistent AF. Furthermore, inasmuch as presence of heart failure favors maintenance of AF [48], the improvement in heart failure with restoration of sinus rhythm may also contribute to success of ablation by modifying the underlying electro-anatomical substrate [49] (i.e. possibly to a greater extent than achievable by ablation of long-standing persistent AF without heart failure). Success rates of catheter ablation of long-standing persistent AF without HFrEF, in a single center study, were 20 and 45% after single and multiple ablations respectively at five-year follow up [50]. Maintenance of sinus rhythm with AAD is especially difficult in HFrEF. In the AF-CHF trial, 21% abandoned rhythm control, 27% were in AF at the end of the 4-year follow up and 58% had experienced at least one episode of AF [11]. Loss of the atrial systole, a decreased diastolic filling interval and increased neurohormonal activation may be of particular hemodynamic consequence in this population [48]. In the DIAMOND AF study, patients who were able to maintain sinus rhythm had improved outcomes [10].
We found that catheter ablation is a safe procedure in patients with AF and HFrEF. The number of adverse events were relatively small and are comparable to those seen in patients with paroxysmal AF. In addition, the very low degree of side effects renders catheter ablation an attractive option for maintenance of sinus rhythm especially considering the low efficacy rate and higher degree of side effects of AADs.
Similar to a previous meta-analysis of randomized trials comparing AF catheter ablation to anti-arrhythmic drug therapy in patients without HFrEF [51], the current analysis demonstrated an improvement in functional status and quality of life in patients with HFrEF. Given the non-blinded nature of the intervention, the possibility that the improvements in functional status be due to a placebo effect cannot be excluded. However, the improvement in functional status mirrors that seen in LVEF and clinical outcomes. This association is well established in patients with HFrEF [52]. Furthermore, the six-minute walk distance is a recognized objective measure of functional status [53].
Of note, a major limitation of this analysis and the current literature is the absence of clinical trials with long-term clinical outcome assessment comparing catheter ablation with a pure rate control strategy i.e. excluding amiodarone use completely. As seen in the AF-CHF trial [11], use of amiodarone in the rhythm control group may have offset the benefit achieved from a relatively good degree of maintenance of sinus rhythm. Hence the RAFT-AF randomized trial (NCT01420393), which will assess the long-term outcome of catheter ablation in comparison to rate control therapy, excluding AAD use such as amiodarone, will shed important light on this important issue.
There were several other limitations to our meta-analyses. Firstly, the number of included studies and patients is relatively small, emphasizing the need for larger studies in this patient population. The small number of studies prevents an effective analysis of publication bias and meta-regression to better understand the factors associated with these results. Secondly, the absence of patient-level data prevented us from identifying patient characteristics that can be associated with improved outcomes. Thirdly, there was a significant variation in follow-up duration with only two studies with more than one year of follow-up. Therefore, we could not evaluate the benefit of catheter ablation beyond one-year follow-up. Fourthly, the mean NYHA class was 2.5 and the mean LVEF was 30%; therefore, it is unclear if these findings are applicable to patients with severely decreased LVEF and those with NYHA class III-IV. Fifthly, all patients included in the two largest trials reported by Di Biase et al. and Marrouche et al. included patients with an implantable-cardioverter-defibrillator [28, 33]. While this therapy is guideline based and allows continuous monitoring for arrhythmia recurrence, it remains unclear if catheter ablation is also beneficial in patients without an implantable-cardioverter-defibrillator especially given that it may no longer be indicated if the LVEF improves after catheter ablation. This clinical question should also be answered by the RAFT-AF study (NCT01420393). Data from the CABANA study (NCT00911508) specific to the heart failure population will also offer further insights. Finally, the results of our findings may only be applicable to large-volume centers of catheter ablation since most of the centers participating in the RCTs were institutions with expertise in this technique.
Conclusions
Compared to medical therapy including AAD, AF catheter ablation was associated with significant improvements in all-cause mortality, heart failure hospitalization, LVEF as well as functional status in patients with HFrEF and AF. Larger multicenter RCTs are needed to validate whether a rhythm control strategy with AF ablation is superior to rate control strategy (without use of AAD) in patients with AF and heart failure.
Abbreviations
- AAD:
-
Anti-arrhythmic drug
- AF:
-
Atrial fibrillation
- CA:
-
Catheter ablation
- HFrEF:
-
Heart failure with reduced ejection fraction
- LVEF:
-
Left ventricular ejection fraction
- MLWHF:
-
Minnesota living with heart failure
- RCT:
-
Randomized controlled trial
References
Anter E, Jessup M, Callans DJ. Atrial fibrillation and heart failure. Treatment Considerations for a Dual Epidemic 2009;119(18):2516–2525.
Malhi N, Hawkins NM, Andrade JG, Krahn AD, Deyell MW. Catheter ablation of atrial fibrillation in heart failure with reduced ejection fraction. J Cardiovasc Electrophysiol. 2018;29(7):1049–58.
Verma A, Kalman JM, Callans DJ. Treatment of patients with atrial fibrillation and heart failure with reduced ejection fraction. Circulation. 2017;135(16):1547–63.
Byrne M, Kaye DM, Power J. The synergism between atrial fibrillation and heart failure. J Card Fail. 2008;14(4):320–6.
Wasmund SL, Li JM, Page RL, Joglar JA, Kowal RC, Smith ML, et al. Effect of atrial fibrillation and an irregular ventricular response on sympathetic nerve activity in human subjects. Circulation. 2003;107(15):2011–5.
Gertz ZM, Raina A, Saghy L, Zado ES, Callans DJ, Marchlinski FE, et al. Evidence of atrial functional mitral regurgitation due to atrial fibrillation: reversal with arrhythmia control. J Am Coll Cardiol. 2011;58(14):1474–81.
Dandamudi G, Rampurwala AY, Mahenthiran J, Miller JM, Das MK. Persistent left ventricular dilatation in tachycardia-induced cardiomyopathy patients after appropriate treatment and normalization of ejection fraction. Heart Rhythm. 2008;5(8):1111–4.
Shinbane JS, Wood MA, Jensen DN, Ellenbogen KA, Fitzpatrick AP, Scheinman MM. Tachycardia-induced cardiomyopathy: a review of animal models and clinical studies. J Am Coll Cardiol. 1997;29(4):709–15.
The AFFIRM Investigators. A comparison of rate control and rhythm control in patients with atrial fibrillation. N Engl J Med. 2002;347(23):1825–33.
Pedersen OD, Bagger H, Keller N, Marchant B, Køber L, Torp-Pedersen C. Efficacy of Dofetilide in the treatment of atrial fibrillation-flutter in patients with reduced left ventricular function. A Danish Investigations of Arrhythmia and Mortality ON Dofetilide (DIAMOND) Substudy 2001;104(3):292–296.
Roy D, Talajic M, Nattel S, Wyse DG, Dorian P, Lee KL, et al. Rhythm control versus rate control for atrial fibrillation and heart failure. N Engl J Med. 2008;358(25):2667–77.
Roden DM. Risks and benefits of antiarrhythmic therapy. N Engl J Med. 1994;331(12):785–91.
Zimetbaum P. Antiarrhythmic drug therapy for atrial fibrillation. Circulation. 2012;125(2):381–9.
Haegeli LM, Calkins H. Catheter ablation of atrial fibrillation: an update. Eur Heart J. 2014;35(36):2454–9.
Morillo CA, Verma A, Connolly SJ, et al. Radiofrequency ablation vs antiarrhythmic drugs as first-line treatment of paroxysmal atrial fibrillation (raaft-2): a randomized trial. JAMA. 2014;311(7):692–700.
Wilber DJ, Pappone C, Neuzil P, et al. Comparison of antiarrhythmic drug therapy and radiofrequency catheter ablation in patients with paroxysmal atrial fibrillation: a randomized controlled trial. JAMA. 2010;303(4):333–40.
Essebag V, Wylie JV, Josephson ME. Effectiveness of catheter ablation of atrial fibrillation. Eur Heart J. 2006;27(2):130–1.
Amit G, Nyong J, Morillo CA. Efficacy of catheter ablation for nonparoxysmal atrial fibrillation. JAMA Cardiol. 2017;2(7):812–3.
Samuel M, Avgil Tsadok M, Joza J, Behlouli H, Verma A, Essebag V, et al. Catheter ablation for the treatment of atrial fibrillation is associated with a reduction in health care resource utilization. J Cardiovasc Electrophysiol. 2017;28(7):733–41.
Samuel M, Almohammadi M, Tsadok MA, Joza J, Jackevicius CA, Koh M, et al. Population-based evaluation of major adverse events after catheter ablation for atrial fibrillation. JACC Clin Electrophysiol. 2017;3(12):1425–33.
Ullah W, Ling L-H, Prabhu S, Lee G, Kistler P, Finlay MC, et al. Catheter ablation of atrial fibrillation in patients with heart failure: impact of maintaining sinus rhythm on heart failure status and long-term rates of stroke and death. EP Europace. 2016;18(5):679–86.
Chen MS, Marrouche NF, Khaykin Y, Gillinov AM, Wazni O, Martin DO, et al. Pulmonary vein isolation for the treatment of atrial fibrillation in patients with impaired systolic function. J Am Coll Cardiol. 2004;43(6):1004–9.
Hsu LF, Jais P, Sanders P, Garrigue S, Hocini M, Sacher F, et al. Catheter ablation for atrial fibrillation in congestive heart failure. N Engl J Med. 2004;351(23):2373–83.
Sacher F, Corcuff JB, Schraub P, Le Bouffos V, Georges A, Jones SO, et al. Chronic atrial fibrillation ablation impact on endocrine and mechanical cardiac functions. Eur Heart J. 2008;29(10):1290–5.
Dagres N, Varounis C, Gaspar T, Piorkowski C, Eitel C, Iliodromitis EK, et al. Catheter ablation for atrial fibrillation in patients with left ventricular systolic dysfunction. A systematic review and meta-analysis. J Card Fail. 2011;17(11):964–70.
January CT, Wann LS, Alpert JS, Calkins H, Cigarroa JE, Cleveland JC Jr, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association task force on practice guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014;64(21):e1–76.
Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37(38):2893–962.
Di Biase L, Mohanty P, Mohanty S, Santangeli P, Trivedi C, Lakkireddy D, et al. Ablation versus amiodarone for treatment of persistent atrial fibrillation in patients with congestive heart failure and an implanted device: results from the AATAC multicenter randomized trial. Circulation. 2016;133(17):1637–44.
Hunter RJ, Berriman TJ, Diab I, Kamdar R, Richmond L, Baker V, et al. A randomized controlled trial of catheter ablation versus medical treatment of atrial fibrillation in heart failure (the CAMTAF trial). Circ Arrhythm Electrophysiol. 2014;7(1):31–8.
Jones DG, Haldar SK, Hussain W, Sharma R, Francis DP, Rahman-Haley SL, et al. A randomized trial to assess catheter ablation versus rate control in the management of persistent atrial fibrillation in heart failure. J Am Coll Cardiol. 2013;61(18):1894–903.
Khan MN, Jais P, Cummings J, Di Biase L, Sanders P, Martin DO, et al. Pulmonary-vein isolation for atrial fibrillation in patients with heart failure. N Engl J Med. 2008;359(17):1778–85.
MacDonald MR, Connelly DT, Hawkins NM, Steedman T, Payne J, Shaw M, et al. Radiofrequency ablation for persistent atrial fibrillation in patients with advanced heart failure and severe left ventricular systolic dysfunction: a randomised controlled trial. Heart. 2011;97(9):740–7.
Marrouche NF, Brachmann J, Andresen D, Siebels J, Boersma L, Jordaens L, et al. Catheter ablation for atrial fibrillation with heart failure. N Engl J Med. 2018;378(5):417–27.
Prabhu S, Taylor AJ, Costello BT, Kaye DM, McLellan AJA, Voskoboinik A, et al. Catheter ablation versus medical rate control in atrial fibrillation and systolic dysfunction: the CAMERA-MRI study. J Am Coll Cardiol. 2017;70(16):1949–61.
Calkins H, Hindricks G, Cappato R, Kim YH, Saad EB, Aguinaga L, et al. 2017 HRS/EHRA/ECAS/APHRS/SOLAECE expert consensus statement on catheter and surgical ablation of atrial fibrillation. Heart Rhythm. 2017;14(10):e275–444.
Ionescu-Ittu R, Abrahamowicz M, Jackevicius CA, Essebag V, Eisenberg MJ, Wynant W, et al. Comparative effectiveness of rhythm control vs rate control drug treatment effect on mortality in patients with atrial fibrillation. Arch Intern Med. 2012;172(13):997–1004.
Healey JS, Oldgren J, Ezekowitz M, Zhu J, Pais P, Wang J, et al. Occurrence of death and stroke in patients in 47 countries 1 year after presenting with atrial fibrillation: a cohort study. Lancet. 2016;388(10050):1161–9.
Odutayo A, Wong CX, Hsiao AJ, Hopewell S, Altman DG, Emdin CA. Atrial fibrillation and risks of cardiovascular disease, renal disease, and death: systematic review and meta-analysis. BMJ. 2016;354.
Sartipy U, Dahlström U, Fu M, Lund LH. Atrial fibrillation in heart failure with preserved, mid-range, and reduced ejection fraction. JACC Heart Fail. 2017;5(8):565–74.
Al Halabi S, Qintar M, Hussein A, Alraies MC, Jones DG, Wong T, et al. Catheter ablation for atrial fibrillation in heart failure patients: a meta-analysis of randomized controlled trials. JACC Clin Electrophysiol. 2015;1(3):200–9.
Shelton RJ, Clark AL, Goode K, Rigby AS, Houghton T, Kaye GC, et al. A randomised, controlled study of rate versus rhythm control in patients with chronic atrial fibrillation and heart failure: (CAFÉ-II study). Heart. 2009;95(11):924–30.
Brignole M, Menozzi C, Gasparini M, Bongiorni MG, Botto GL, Ometto R, et al. An evaluation of the strategy of maintenance of sinus rhythm by antiarrhythmic drug therapy after ablation and pacing therapy in patients with paroxysmal atrial fibrillation. Eur Heart J. 2002;23(11):892–900.
Hohnloser SH, Kuck KH, Lilienthal J. Rhythm or rate control in atrial fibrillation--pharmacological intervention in atrial fibrillation (PIAF): a randomised trial. Lancet. 2000;356(9244):1789–94.
Sethi NJ, Feinberg J, Nielsen EE, Safi S, Gluud C, Jakobsen JC. The effects of rhythm control strategies versus rate control strategies for atrial fibrillation and atrial flutter: a systematic review with meta-analysis and Trial sequential analysis. PLoS One. 2017;12(10):e0186856.
Jais P, Cauchemez B, Macle L, Daoud E, Khairy P, Subbiah R, et al. Catheter ablation versus antiarrhythmic drugs for atrial fibrillation: the A4 study. Circulation. 2008;118(24):2498–505.
Anand IS, Florea VG, Fisher L. Surrogate end points in heart failure. J Am Coll Cardiol. 2002;39(9):1414–21.
Katsi V, Georgiopoulos G, Laina A, Koutli E, Parissis J, Tsioufis C, et al. Left ventricular ejection fraction as therapeutic target: is it the ideal marker? Heart Fail Rev. 2017;22(6):641–55.
Kotecha D, Piccini JP. Atrial fibrillation in heart failure: what should we do? Eur Heart J. 2015;36(46):3250–7.
Nattel S. Therapeutic implications of atrial fibrillation mechanisms: can mechanistic insights be used to improve AF management? Cardiovasc Res. 2002;54(2):347–60.
Tilz RR, Rillig A, Thum AM, Arya A, Wohlmuth P, Metzner A, et al. Catheter ablation of long-standing persistent atrial fibrillation: 5-year outcomes of the Hamburg sequential ablation strategy. J Am Coll Cardiol. 2012;60(19):1921–9.
Siontis KC, Ioannidis JPA, Katritsis GD, Noseworthy PA, Packer DL, Hummel JD, et al. Radiofrequency ablation versus antiarrhythmic drug therapy for atrial fibrillation. Meta-Analysis of Quality of Life, Morbidity, and Mortality 2016;2(2):170–180.
Zhang Y, Guallar E, Blasco-Colmenares E, Butcher B, Norgard S, Nauffal V, et al. Changes in follow-up left ventricular ejection fraction associated with outcomes in primary prevention implantable cardioverter-defibrillator and cardiac resynchronization therapy device recipients. J Am Coll Cardiol. 2015;66(5):524–31.
Guazzi M, Dickstein K, Vicenzi M, Arena R. Six-minute walk test and cardiopulmonary exercise testing in patients with chronic heart failure: a comparative analysis on clinical and prognostic insights. Circ Heart Fail. 2009;2(6):549–55.
Acknowledgements
none to declare
Funding
none to declare
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Contributions
AAT (Concept/design; data analysis/interpretation; drafting article; approval of article), RP (Concept/design; data analysis/interpretation; approval of article), AD (data analysis/interpretation; approval of article), HA (Data analysis/interpretation; approval of article), TH (Concept/design; critical review of article; approval of article), VE (Concept/design; critical review of article; approval of article). All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study used data from previously published studies that individually obtained ethics approval.
Consent for publication
Not applicable
Competing interests
Dr. Essebag has received honoraria from Abbott, biosense medical, boston scientific and Medtronic.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
AlTurki, A., Proietti, R., Dawas, A. et al. Catheter ablation for atrial fibrillation in heart failure with reduced ejection fraction: a systematic review and meta-analysis of randomized controlled trials. BMC Cardiovasc Disord 19, 18 (2019). https://doi.org/10.1186/s12872-019-0998-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-019-0998-2