Abstract
Background
The population of adolescents and young adults with congenital heart disease (CHD) is growing exponentially. These survivors are at risk of late cardiac complications and require lifelong cardiology care. However, there is a paucity of data on how to prepare adolescents to assume responsibility for their health and function within the adult health care system. Evidence-based transition strategies are required.
Methods
The Congenital Heart Adolescents Participating in Transition Evaluation Research (CHAPTER 2) Study is a two-site cluster randomized clinical trial designed to evaluate the efficacy of a nurse-led transition intervention for 16–17 year olds with moderate or complex CHD. The primary endpoint is excess time to adult CHD care, defined as the time interval between the final pediatric cardiology appointment and the first adult CHD appointment, minus the recommended time interval between these appointments. Secondary endpoints include the MyHeart score (CHD knowledge), Transition Readiness Assessment Questionnaire score, and need for catheter or surgical re-intervention. Participants are enrolled in clusters based on week of attendance in the pediatric cardiology clinic. The intervention consists of two one-hour individualized sessions between a cardiology nurse and study participant. Session One focuses on knowledge of the participant’s CHD, review of their cardiac anatomy and prior interventions, and potential late cardiac complications. Session Two focuses on self-management and communication skills through review and discussion of videos and role-play. The study will recruit 120 participants.
Discussion
Many adolescents and young adults experience a gap in care predisposing them to late cardiac complications. The CHAPTER 2 Study will investigate the impact of a nurse-led transition intervention among adolescents with CHD. Fidelity of the intervention is a major focus and priority. This study will build on our experience by (i) enrolling at two tertiary care programs, (ii) including a self-management intervention component, and (iii) evaluating the impact of the intervention on time to ACHD care, a clinically relevant outcome. The results of this study will inform pediatric cardiology programs, patients and policy makers in judging whether a structured intervention program provides clinically meaningful outcomes for adolescents and young adults living with CHD.
Trial registration
ClinicalTrials.gov ID NCT01723332
Similar content being viewed by others
Background
Major advances in the management of children with congenital heart disease (CHD) have evolved over the past three decades. As a consequence, over 90 % of these children reach adulthood and the population of adolescents and young adults with CHD is growing exponentially [1].However, this emerging “survivor” population has complex needs. These individuals are at risk of substantial cardiac morbidity [2, 3] and mortality [4, 5] in early-to-mid adult years. Unfortunately, 14–53 % of young adults are not successfully transferred to an adult CHD (ACHD) centre after graduating from a pediatric cardiac centre [6–8], and failure to attend an ACHD clinic results in excess cardiac morbidity [7, 9, 10]. Furthermore, adolescents and young adults with CHD have limited knowledge about their heart [11–13], limiting their ability to communicate confidently with health care providers [14].
At present there is a paucity of outcome data regarding the impact and effectiveness of CHD transition interventions. Indeed, there is a lack of transition outcome data for chronic pediatric conditions in general. This speaks to the urgency of developing evidence-based intervention programs that will optimize pediatric to adult health care transition using methods that can be readily adopted by clinical programs. The American Heart Association published a Scientific Statement on the subject of transition in 2011 that emphasized the relevance of this topic to the CHD community and acknowledged the lack of data on transition programming [15].
To address these knowledge gaps our team conducted the Congenital Heart Adolescents Participating in Transition Evaluation Research (CHAPTER 1) Study [16] to evaluate a single-session nurse-led transition education intervention, focusing on CHD knowledge, for youth 15–17 years of age. This study significantly improved patients’ knowledge of their CHD lesion in the intervention group at one month, which was sustained at 6 months. The intervention group also had higher self-management skills at six months, even though self-management skills were not the focus of the intervention. Limitations of this study include enrollment at a single center and use of surrogate outcomes (questionnaires) rather than participant behaviors such as attendance at an ACHD clinic. The current study was designed to build upon our experience with CHAPTER 1, specifically to include a self-management component of the intervention, to document time to first ACHD clinic appointment, and to assess generalizability of the intervention across more than one clinical program.
The primary aim of the CHAPTER 2 study is to determine the impact of a nurse-led intervention on time to first ACHD clinic attendance among youth graduating from one of two quaternary-care pediatric cardiology programs. We hypothesize that the transition intervention in combination with usual care will result in superior timing of the first ACHD clinic attendance compared to usual care alone. Secondary aims are to describe: 1) change in adolescent knowledge of their CHD, 2) change in self-management and self-advocacy skills using validated instruments [17, 18], 3) Incidence of cardiac procedures post enrollment, and 4) the frequency and content of verbal and written (email/text messaging) dialogue between nurse and participant.
Methods
Study design
The CHAPTER 2 Study is a two-center cluster randomized controlled trial of a nurse-led transition intervention versus usual care (see “usual care” section below). The intervention will consist of two individualized sessions lasting ~60 min each held two months apart, in or adjacent to the pediatric cardiology clinic. The study is registered with Clinical Trials.gov (ID NCT01723332) and will be conducted in accordance with CONSORT guidelines (Fig. 1) [19].
Study setting and participants
The study will be conducted at The Hospital for Sick Children (“SickKids”, Toronto, Canada) and the Stollery Children’s Hospital (Edmonton, Canada). These are the largest pediatric cardiology programs in Canada and offer the full range of cardiology and cardiac surgical subspecialty services. We will include 16–17 year olds with moderate or complex CHD (as previously defined) [20] who have not yet been transferred to adult care. Exclusion criteria will be (i) less than a Grade 6 level of reading and comprehension, based on parent report, and (ii) heart transplantation.
Transition intervention
The intervention will be conducted by one of two cardiology registered nurses (RNs) at each site (total 4 RNs) who are experienced working with teens. Youth will attend two one-on-one sessions with the same RN. Sessions will be youth-oriented, interactive, and engaging. Session One will occur immediately after a pediatric cardiology clinic visit to minimize study burden and to adhere with recommendations that transition interventions be delivered in clinical settings [21]. Individual sessions, in contrast to group sessions, allow the content to be patient-specific. Session Two will occur two months after Session One, in conjunction with another clinic appointment or as the sole purpose of a return visit. Individual participant flow through the study is illustrated in Fig. 2.
Immediately prior to Session One, the RN will review the cardiology chart to become familiar with the cardiac history including CHD diagnoses, names and dates of cardiac surgical procedures and cardiac catheterizations, and current cardiac medications and doses. Session One (1 h) will emphasize education; Session Two (1.0–1.5 h) will emphasize self-management. Details of each session are summarized in Table 1.
Treatment fidelity and quality assurance
Consistency of the intervention between study RNs and study participants is a priority of this study. Team education will start with an in-person two-day meeting in Toronto involving study RNs, led by the study investigator (GRR) who co-developed and conducted many of the interventions in the CHAPTER 1 study [16]. Professionally filmed video-tapes depicting Sessions One and Two were prepared for the RNs on how to conduct the sessions with a standardized patient. These teaching videos will be viewed by each study RN and role-playing will be performed for practice.
Audio recordings of sessions One and Two with study participants will be conducted if the participant agrees. Evaluation of treatment fidelity will be based on review of nursing logs and/or audiotapes by other study RNs and team members (ASM, GRR). Monthly conference calls involving all study RNs will be conducted to provide feedback and discuss issues related to the intervention as they arise.
After each session the RN will complete an intervention log. The RN will record completion of each intervention component as described in Table 1, and use field notes to record the participant’s knowledge, enthusiasm, and commitment to the intervention. All intervention logs and field notes will be reviewed monthly by team members (ASM, GRR, and RNs), as part of ongoing quality assurance.
Usual care
No transition program is formally in place at the Stollery site. Families receive written information about their child’s CHD, suggested timelines for increasing teens’ self-management of his/her CHD, and at the last pediatric visit a “graduation” package with information about the ACHD program is provided. At SickKids, usual care is similar. However, to account for potential differences in usual care, randomization will be stratified by site. With multiple pediatric cardiologists and clinic nurses at each site, clinician-led education is likely variable and constrained by limited clinic time. At both sites, pertinent medical records are sent to ACHD providers at the time of transfer. Both ACHD clinics send a welcome letter to patients indicating approximately when their first ACHD appointment will be. A second letter is sent one month prior to the first ACHD appointment with the date and time. Patients who do not attend are contacted by telephone to reschedule. All components of usual care will be tracked by the project coordinator at each site, and any change in usual care during the study will be documented.
Group allocation
Participants will be randomized by clusters defined by week of attendance in the pediatric cardiology clinic. As week (not study participant) is the unit of randomization, this is a cluster randomization design. This method of randomization: 1) prevents two adolescents in the same waiting room being allocated to different groups and 2) facilitates scheduling of study RNs, who will be available at short notice to provide the intervention during intervention weeks. Cardiologists will not be informed of group assignment, preventing potential bias by cardiologist co-intervention. We anticipate enrollment of 3–4 patients per week, i.e., cluster size will be ≤ 4. To determine which weeks are “intervention weeks” vs. “usual care weeks”, a biostatistician will prepare a randomization sequence.
A 1:1 ratio of intervention: usual care weeks will be used until midway through enrollment, when there will be a re-evaluation. If there is an imbalance, then there will be an adjustment of the ratio of intervention to usual care weeks.
Protecting against sources of bias
Participants, their parents, and the study RNs will be aware of group allocation as blinding is not feasible. However, clinical outcomes will be adjudicated by observers who are blind to group allocation (see Secondary outcomes #4 below). Furthermore, participants in both groups will be unaware of the primary outcome (excess time to attendance at first ACHD appointment) and therefore this outcome cannot be consciously influenced, though participants will be aware that the study will track information from the cardiology chart, including the first ACHD clinic visit. Clinic support staff and pediatric cardiologists will be blind to group allocation.
Outcome measures
Outcome measures correspond to aims as described above. The primary outcome will be the excess time between pediatric and ACHD care, defined as the time interval (in months) between the final pediatric visit and the first ACHD visit, minus the recommended time interval between these visits. The “recommended time” interval will be the interval suggested by the cardiologist at the final pediatric visit. For example, if the time between the final pediatric visit and first ACHD visit was 20 months but the pediatric cardiologist recommended this be 12 months, the excess time would be 8 months. If the first ACHD visit takes place before the recommended time, the excess time will be zero. For the rare study participant not having a documented “recommended time”, recommendations for frequency of care will be taken from published guidelines [22, 23]. Excess time to ACHD care is an objective and clinically meaningful outcome, as lapses between pediatric and ACHD care result in increased cardiac morbidity and need for re-intervention [9]. First ACHD appointments that occur 2 or more months later than had been recommended by the referring pediatric cardiologist will result in a review of medical records to identify potential participant or system factors, including a) ACHD waiting list too long to accommodate participant when recommended, b) ACHD team unaware of initial referral, or c) participant did not agree to an earlier appointment.
Secondary outcomes
Given the complex, multidimensional nature of the transition process, transition interventions need to consider multiple outcomes, including cognitive factors (e.g. CHD knowledge) and self-management behaviours. Therefore, several secondary outcomes are proposed. All baseline questionnaires will be completed in the pediatric clinic, and prior to Session One for those in the intervention arm.
-
1)
Change in MyHeart scores between baseline, 1, 6, 12 and 18 months. The MyHeart scale consists of eight questions that assess participant’s knowledge of their cardiac condition. The MyHeart scale was developed for the CHAPTER 1 study, with a significant improvement in score observed at 1 and 6 months post intervention, compared to participants in the usual care group [16].
-
2)
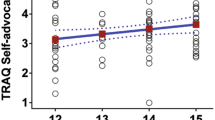
Change in Transition Readiness Assessment Questionnaire (TRAQ) score between baseline, 1, 6, 12, and 18 months. The TRAQ is the most rigorous transition readiness scale for adolescents. Sawicki et al. identified behaviours relevant to transition, tested item reliability and validity, and then field tested the items with 194 youth with special healthcare needs [18]. Scores range from 0 to 5. Principal component factor analysis revealed two domains explaining 68 % of the total variance: self-management (16 items, mean score 3.01 ± 1.02) assessing skills such as filling prescriptions, understanding treatment side effects, and arranging medical follow-up visits; and self-advocacy (13 items, mean score 3.67 ± 0.77) assessing communication skills with the healthcare team, managing activities of daily living, and use of school and community resources. Internal consistency is high, with Cronbach’s alpha of 0.92 (Self-management) and 0.82 (Self-advocacy). A ceiling effect is unlikely given the mean scores noted above. The reading level is Grade 5.7 and this instrument takes ~5 min to complete. The 12 and 18 month assessments will provide longitudinal data on evolution of self-management and self-advocacy skills and will allow participants in the intervention group sufficient time to apply the skills gained (e.g., to independently book a physician appointment).
-
3)
Change in the Williams’ Scale between baseline, 1, 6, 12, and 18 months. The Williams’ scale is a measure of medical self-management and transition readiness among adolescents with special health care needs, having high internal consistency (Cronbach’s alpha 0.89) [17]. This consists of 21 Likert-scaled items and has a grade 4.9 reading level.
-
4)
Assessment of patient engagement via a cardiologist questionnaire. This questionnaire will be completed by the participant’s primary cardiologist at the first cardiology clinic visit (pediatric or adult site), after month 3 post enrollment. This questionnaire will help determine if those participants in the intervention group were more engaged with their cardiologist then those in the usual care group. The single-page questionnaire consists of six items and takes 1–2 min to complete.
-
5)
Incidence of cardiac re-intervention (surgery or interventional catheterization). Chart review at 12 and 24 months post enrollment will be done independently by two RNs who will be blinded to group allocation. This review will ascertain cardiac hospitalizations and invasive cardiac procedures (since study enrollment), confirm attendance at ACHD clinic, and identify new or progressive complications (e.g., endocarditis, heart failure, stroke, thrombosis, systemic or pulmonary emboli, arrhythmia requiring drug or procedural intervention, renal or hepatic failure) [2]. Discrepant adjudication will be resolved by a cardiologist team member.
-
6)
Frequency and content of verbal and written (email/text messaging/telephone) dialogue between intervention nurse and participant. The intervention RN will complete detailed post-intervention field notes after each session. Telephone communication (phone calls, text messages) and emails will be encouraged from participants at any time; all will be recorded verbatim and analyzed (see Quantitative data analysis below).
Measurement of outcomes at follow-up
Documentation of first ACHD visit will be done at 12 and 24 month chart review and will include potential barriers to ACHD clinic attendance. Regarding secondary outcomes 1–3, participants will complete the follow-up questionnaires at home, independent of their parent(s). Adolescents not completing the follow-up questionnaires will be contacted by mail, email, or text (depending on their preference) every two weeks for a total of three times, and then telephoned once, to be reminded. A $25 gift certificate will be provided to participants at each of the 1, 6, 12, and 18 month time points to acknowledge their time and commitment to questionnaire completion.
Proposed sample size
The sample size is based on testing group differences in the primary outcome, excess time to ACHD care, with a two-sided log-rank test. A sample size of 60 patients per group (120 total) will allow detection of a difference between 90 and 70 %, the proportions that have attended their first ACHD clinic appointment by the end of the observation period in the intervention and usual care groups, respectively, with 80 + % power (Type I Error Probability [α] = 0.05), accounting for the “design effect” due to the cluster randomization of the trial. The proportion of 70 % in the usual care group is conservative, as published SickKids data suggests it may be as low as 50 % [8]. If the proportion of usual care participants attending the ACHD clinic is <70 %, the study power will be even higher. The difference between 90 and 70 % is the minimum clinically important difference, as a proportion <90 % attending ACHD care is unacceptably low [15]. Given that the most common reason for a lapse in care prior to first ACHD visit is a belief that cardiac follow-up is not required [9], a misconception that the intervention will address, we believe that a 90 % ACHD clinic attendance in the intervention group is achievable.
Quantitative data analysis
Intention-to-treat analysis will be used and all statistical tests will be two-sided. Baseline characteristics of the control (usual care) and intervention groups will be summarized using descriptive statistics (e.g., means, medians, standard deviations, frequencies, proportions). Kaplan-Meier plots will display excess time to first ACHD appointment by treatment group. Log-rank tests with a cluster-level bootstrap will test the difference in the excess time distribution between the intervention and control groups. The cluster sizes are likely to be 3–4. All statistical analyses will account for the cluster randomization. Participants who have not attended the ACHD clinic by the end of the study period (i.e., are censored) will still contribute to the primary outcome, as survival analysis is designed to accommodate censored data. We will assess differences in mean scores of each secondary outcome at baseline, 1, 6, 12, and 18 months, where applicable, by treatment group using general linear mixed models [24] that take both the cluster randomization and longitudinal nature of the data into account. Additional analyses will be stratified by a) study site (Edmonton versus Toronto) and b) attended first ACHD appointment (yes/no).
Qualitative data analysis
All field notes and text/email messages between the RN and participant will be saved, anonymized, and analyzed for codes, categories and subcategories as per qualitative deductive content analysis [25–27]. Data will be analyzed for manifest and latent content, latent content referring to the time that passes between each text message (or email), the word and sentence formations, and the (in)formality and use of language.
Discussion
The rapidly growing population of adolescent and young adult survivors of CHD is at risk of late cardiac and non-cardiac morbidity and premature mortality. Numerous barriers exist to delivering specialized ACHD care to this population, including a lack of ACHD providers in many developed countries [28, 29]. Unfortunately, few pediatric cardiology programs facilitate the transition of adolescents in their care [30], and many adolescents and young adults experience a gap in care [7, 8, 31] predisposing them to late cardiac complications [9]. To our knowledge, the single-centre CHAPTER 1 study is the only published controlled clinical trial of a transition intervention in the CHD population. The CHAPTER 2 study will build on our experience by (i) enrolling at two tertiary care programs, (ii) including a self-management intervention component, and (iii) evaluating the impact of the intervention on time to ACHD care, a clinically relevant outcome.
Potential limitations
Several threats to internal validity exist. These include: (i) co-intervention; awareness of the study and of the need for health care transition may influence what cardiologists say to participants, however both groups will benefit equally and this will not create a bias towards one study group. Cardiologists will be unaware of group allocation. (ii) Loss to follow-up; when patients miss appointments, both Edmonton and Toronto ACHD clinics routinely use all available contact information to arrange another appointment and keep patients in care. From the perspective of the study, participants who have not attended the ACHD clinic by the end of the study period will be censored and will still contribute to the primary outcome. (iii) Provider/system factors such as waiting lists may influence the primary outcome. However this will be equally true of participants in both groups. The time interval between the recommended date of first ACHD appointment and scheduled date of first ACHD appointment will be recorded to capture provider/system factors. The mean wait time for non-urgent referrals to Canadian ACHD clinics is only 4 ± 2 months [29], so we do not anticipate this to be an issue. (iv) Responsiveness of the Williams’ transition readiness scale to intervention is not yet known, though this is just one of six secondary endpoints. Both the TRAQ and MyHeart scale are responsive to an educational intervention [16].
In summary, the CHAPTER 2 study is a two-center cluster randomized clinical trial of a nurse led transition intervention for 16–17 year olds with moderate or complex CHD. Fidelity of the intervention is a major focus and priority. We will evaluate time to first ACHD appointment, CHD knowledge, transition readiness, need for catheter and surgical re-intervention, and qualitative outcomes. The results of this study will inform pediatric cardiology programs, patients and policy makers in judging whether a structured intervention program provides clinically meaningful outcomes for adolescents and young adults living with CHD.
Abbreviations
ACHD, adult congenital heart disease; CHAPTER, congenital heart adolescents participating in transition evaluation research; CHD, congenital heart disease; RN, research nurse; TRAQ, transition readiness assessment questionnaire
References
Marelli AJ, Ionescu-Ittu R, Mackie AS, Guo L, Dendukuri N, Kaouache M. Lifetime prevalence of congenital heart disease in the general population from 2000 to 2010. Circulation. 2014;130:749–6.
Warnes CA. The adult with congenital heart disease: born to be bad? J Am Coll Cardiol. 2005;46:1–8.
Perloff JK, Warnes CA. Challenges posed by adults with repaired congenital heart disease. Circulation. 2001;103:2637–43.
Khairy P, Ionescu-Ittu R, Mackie AS, Abrahamowicz M, Pilote L, Marelli AJ. Changing mortality in congenital heart disease. J Am Coll Cardiol. 2010;56:1149–57.
Billett J, Majeed A, Gatzoulis M, Cowie M. Trends in hospital admissions, in-hospital case fatality and population mortality from congenital heart disease in England, 1994 to 2004. Heart. 2008;94:342–8.
Goossens E, Stephani I, Hilderson D, Gewillig M, Budts W, Van Deyk K, Moons P. Transfer of adolescents with congenital heart disease from pediatric cardiology to adult health care: an analysis of transfer destinations. J Am Coll Cardiol. 2011;57:2368–74.
Wray J, Frigiola A, Bull C. Loss to specialist follow-up in congenital heart disease; Out of sight, out of mind. Heart. 2013;99:485–90.
Reid GJ, Irvine MJ, McCrindle BW, Sananes R, Ritvo PG, Siu SC, Webb GD. Prevalence and correlates of successful transfer from pediatric to adult health care among a cohort of young adults with complex congenital heart defects. Pediatrics. 2004;113:e197–205.
Yeung E, Kay J, Roosevelt GE, Brandon M, Yetman AT. Lapse of care as a predictor for morbidity in adults with congenital heart disease. Int J Cardiol. 2008;125:62–5.
Iversen K, Vejlstrup NG, Sondergaard L, Nielsen OW. Screening of adults with congenital cardiac disease lost for follow-up. Cardiol Young. 2007;17:601–8.
Van Deyk K, Pelgrims E, Troost E, Goossens E, Budts W, Gewillig M, Moons P. Adolescents’ understanding of their congenital heart disease on transfer to adult-focused care. Am J Cardiol. 2010;106:1803–7.
Kantoch MJ, Collins-Nakai RL, Medwid S, Ungstad E, Taylor DA. Adult patients’ knowledge about their congenital heart disease. Can J Cardiol. 1997;13:641–5.
Dore A, de Guise P, Mercier LA. Transition of care to adult congenital heart centres: what do patients know about their heart condition? Can J Cardiol. 2002;18:141–6.
Clarizia NA, Chahal N, Manlhiot C, Kilburn J, Redington AN, McCrindle BW. Transition to adult health care for adolescents and young adults with congenital heart disease: perspectives of the patient, parent and health care provider. Can J Cardiol. 2009;25:e317–22.
Sable C, Foster E, Uzark K, Bjornsen K, Canobbio MM, Connolly HM, Graham TP, Gurvitz MZ, Kovacs A, Meadows AK, Reid GJ, Reiss JG, Rosenbaum KN, Sagerman PJ, Saidi A, Schonberg R, Shah S, Tong E, Williams RG, on behalf of the American Heart Association Congenital Heart Defects Committee of the Council on Cardiovascular Disease in the Young, Council on Cardiovascular Nursing, Council on Clinical Cardiology, and Council on Peripheral Vascular Disease. Best practices in managing transition to adulthood for adolescents with congenital heart disease: the transition process and medical and psychosocial issues: a scientific statement from the American Heart Association. Circulation. 2011;123:1454–85.
Mackie AS, Islam S, Magill-Evans J, Rankin KN, Robert C, Schuh M, Nicholas D, Vonder Muhll I, McCrindle BW, Yasui Y, Rempel GR. Healthcare transition for youth with heart disease: a clinical trial. Heart. 2014;100:1113–8.
Williams T, Sherman E, Dunseith C, Mah J, Blackman M, Latter J, Mohamed I, Slick D, Thornton N. Measurement of medical self-management and transition readiness among Canadian adolescents with special health care needs. Int J Child Adolesc Health. 2011;3:527–35.
Sawicki GS, Lukens-Bull K, Yin X, Demars N, Huang IC, Livingood W, Reiss J, Wood D. Measuring the transition readiness of youth with special healthcare needs: validation of the TRAQ--Transition Readiness Assessment Questionnaire. J Pediatr Psychol. 2011;36:160–71.
Boutron I, Moher D, Altman DG, Schulz KF, Ravaud P. Methods and processes of the CONSORT group: example of an extension for trials assessing nonpharmacologic treatments. Ann Intern Med. 2008;148:W60–6.
Warnes CA, Liberthson R, Danielson GK, Dore A, Harris L, Hoffman JI, Somerville J, Williams RG, Webb GD. Task force 1: the changing profile of congenital heart disease in adult life. J Am Coll Cardiol. 2001;37:1170–5.
Transition to adult care for youth with special health care needs. Position Statement, Canadian Paediatric Society. Paediatr Child Health. 2007;12:785–8.
Silversides CK, Marelli A, Beauchesne L, Dore A, Kiess M, Salehian O, Bradley T, Colman J, Connelly M, Harris L, Khairy P, Mital S, Niwa K, Oechslin E, Poirier N, Schwerzmann M, Taylor D, Vonder Muhll I, Baumgartner H, Benson L, Celermajer D, Greutmann M, Horlick E, Landzberg M, Meijboom F, Mulder B, Warnes C, Webb G, Therrien J. Canadian Cardiovascular Society 2009 consensus conference on the management of adults with congenital heart disease: executive summary. Can J Cardiol. 2010;26:143–50.
Warnes CA, Williams RG, Bashore TM, Child JS, Connolly HM, Dearani JA, del Nido P, Fasules JW, Graham Jr TP, Hijazi ZM, Hunt SA, King ME, Landzberg MJ, Miner PD, Radford MJ, Walsh EP, Webb GD. ACC/AHA 2008 Guidelines for the Management of Adults with Congenital Heart Disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2008;118:e714–833.
Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22.
Elo S, Kyngas H. The qualitative content analysis process. J Adv Nurs. 2008;62:107–15.
Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15:1277–88.
Simons L, Lathlean J, Squire C. Shifting the focus: sequential methods of analysis with qualitative data. Qual Health Res. 2008;18:120–32.
Fernandes SM, Khairy P, Fishman L, Melvin P, O’Sullivan-Oliveira J, Sawicki GS, Ziniel S, Breitinger P, Williams R, Takahashi M, Landzberg MJ. Referral patterns and perceived barriers to adult congenital heart disease care: results of a survey of U.S. pediatric cardiologists. J Am Coll Cardiol. 2012;60:2411–8.
Beauchesne LM, Therrien J, Alvarez N, Bergin L, Burggraf G, Chetaille P, Gordon E, Kells CM, Kiess M, Mercier L-, Oechslin EN, Stein J, Tam JW, Taylor D, Williams A, Khairy P, Mackie AS, Silversides CK, Marelli AJ. Structure and process measures of quality of care in adult congenital heart disease patients: a pan-Canadian study. Int J Cardiol. 2012;157:70–4.
Hilderson D, Saidi AS, Van Deyk K, Verstappen A, Kovacs AH, Fernandes SM, Canobbio MM, Fleck D, Meadows A, Linstead R, Moons P. Attitude toward and current practice of transfer and transition of adolescents with congenital heart disease in the United States of America and Europe. Pediatr Cardiol. 2009;30:786–93.
Mackie AS, Ionescu-Ittu R, Therrien J, Pilote L, Abrahamowicz M, Marelli AJ. Children and adults with congenital heart disease lost to follow-up: who and when? Circulation. 2009;120:302–9.
Funding
This study was funded by a Heart and Stroke Foundation of Canada Grant-in-Aid.
Authors’ contributions
ASM, AHK, EO, DN, RS, JME, SJA, MK, GRR and BWM designed the study, obtained peer-reviewed funding, contributed content expertise in pediatric to adult transition and critically reviewed the manuscript for important intellectual content. GRR trained the intervention nurses and reviewed interventions. KNR and AJ recruited subjects and oversaw all day-to-day aspects of running the study. SM, DD, EW, and MS conducted study interventions with participants. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
The study was approved by the Health Research Ethics Board at the University of Alberta and University of Toronto. Written informed consent was obtained from the participant and a parent or guardian in all cases.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Mackie, A.S., Rempel, G.R., Kovacs, A.H. et al. A cluster randomized trial of a transition intervention for adolescents with congenital heart disease: rationale and design of the CHAPTER 2 study. BMC Cardiovasc Disord 16, 127 (2016). https://doi.org/10.1186/s12872-016-0307-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-016-0307-2