Abstract
Background
The role of mechanical power on pulmonary outcomes after thoracic surgery with one-lung ventilation was unclear. We investigated the association between mechanical power and postoperative pulmonary complications in patients undergoing thoracoscopic lung resection surgery.
Methods
In this single-center, prospective observational study, 622 patients scheduled for thoracoscopic lung resection surgery were included. Volume control mode with lung protective ventilation strategies were implemented in all participants. The primary endpoint was a composite of postoperative pulmonary complications during hospital stay. Multivariable logistic regression models were used to evaluate the association between mechanical power and outcomes.
Results
The incidence of pulmonary complications after surgery during hospital stay was 24.6% (150 of 609 patients). The multivariable analysis showed that there was no link between mechanical power and postoperative pulmonary complications.
Conclusions
In patients undergoing thoracoscopic lung resection with standardized lung-protective ventilation, no association was found between mechanical power and postoperative pulmonary complications.
Trial registration
Trial registration number: ChiCTR2200058528, date of registration: April 10, 2022.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Postoperative pulmonary complications (PPCs) are common following lung resection surgery and remain a major determinant of postoperative morbidity and mortality [1]. Lung-protective ventilation strategies are strongly recommended during thoracic surgery to reduce the incidence of PPCs [2, 3]. Protective ventilation during one-lung ventilation (OLV) includes three parts: tidal volume (VT) 4–6 ml/kg of predicted body weight (PBW), positive end-expiratory pressure (PEEP) 5–10 cmH2O and the recruitment maneuver [4]. Nevertheless, the effect of isolated part on the pulmonary outcomes in the context of lung-protective ventilation remains controversial [5,6,7,8].
Recently, mechanical power (MP), that is the amount of energy per unit of time generated and converted to the respiratory system by the ventilator, combining volume, pressure, flow and respiratory rate (RR), has been proposed [9]. MP, as a single variable, has been hypothesized to help estimate the contribution of the different ventilator-related causes of lung injury and of their variations. Previous retrospective studies reported that exposure to higher MP was associated with increased risk of mortality in patients with acute respiratory distress syndrome (ARDS) [10,11,12]. Furthermore, MP normalized to lung size (MP normalized to PBW [norMP] or MP normalized to the compliance of respiratory system [MP/Crs]) has been suggested to have better discrimination power than the absolute MP value in ARDS patients [12, 13].
However, evidence regarding MP and postoperative pulmonary outcomes for surgical patients was rare and mixed with divergent conclusions [14,15,16,17]. A second analysis of a randomized clinical trial found that elevated MP during major noncardiothoracic surgery was independently correlated with increased risk of PPCs [15]. In contrast, a prospective observational trial (n = 30) suggested that there existed no link between MP and pulmonary complications after thoracic surgery [14].
Clinical trials exploring the effect of MP on PPCs after thoracic surgery are requested [18, 19]. Therefore, we designed a prospective, observational study to evaluate the association between MP during OLV and pulmonary complications after thoracoscopic lung resection surgery.
Methods
Study design
We performed a single-center, prospective observational study, which was approved by Ethical Committee of the West China Hospital of Sichuan University (Ethical Committee No.2021 (1580) and registered at the Chinese Clinical Trial Registry (ChiCTR2200058528, principal investigator: Hai Yu, date of registration: April 10, 2022. https://www.chictr.org.cn/showproj.html?proj=155531) before the first patient was enrolled. This report adhered to the applicable STrengthening the Reporting of OBservational studies in Epidemiology (STORBE) statement [20]. Written informed consent was obtained from all participants.
Participants
Adult patients (aged 18 years or older) undergoing elective thoracoscopic lung resection surgery with a duration of OLV ≥ 1 h were included. The exclusion criteria were: American Society of Anesthesiologists classification 4 or above; previous history of neuromuscular diseases or brain trauma or brain injury; acute lung injury or ARDS or severe chronic obstructive pulmonary diseases or previous lung surgery; severe hepatic insufficiency or renal failure requiring dialysis.
Perioperative management
Standard monitoring included electrocardiogram, non-invasive or invasive blood pressure, SpO2, end-tidal carbon dioxide (ETCO2), neuromuscular blockade and bispectral index (BIS) monitoring. Common or video double-lumen tube of the appropriate size (32–37 French) was chosen according to gender, height and chest radiograph. Correct placement of the common double-lumen tube was verified by fiberoptic bronchoscope both in the supine and lateral position. Intraoperative anesthetic management was at the discretion of the attending anesthesiologist according to routine practice. Anesthesia was maintained with volatile anesthetics or intravenous propofol targeting a BIS value between 40 and 60. The train-of-four (TOF) count was monitored every 15 min. Reversal of neuromuscular blockade was suggested with neostigmine of 0.04 mg/kg at a TOF count of at least 3. Multimodal analgesia including non-steroidal anti-inflammatory drugs, glucocorticoids, intercostal nerve blockade and patient-controlled intravenous analgesia was applied to maintain a numerical pain rating scale < 4 [21].
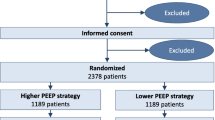
All participants were ventilated in volume control mode with a VT of 7 ml/kg of PBW during two-lung ventilation (TLV) and 5 ml/kg during OLV. Other parameters applied during mechanical ventilation were: PEEP level was determined by the attending anesthesiologist according to clinical guidelines (5–10 cmH2O) [22]; inspiratory pause of 20% to obtain the end-inspiratory plateau pressure (Pplat); inspiration: expiration ratio of 1:2; RR adjusted to maintain ETCO2 between 35 and 45 mmHg; inspiratory oxygen fraction 1.0 during TLV and 0.4–0.5 during OLV to maintain SpO2 > 92%. Manual recruitment maneuvers were performed immediately after tracheal intubation, the restart of TLV and the end of surgery with a continuous positive airway pressure of 30 cmH2O (TLV) or 20 cmH2O (OLV) for 15 s.
If hypoxemia occurred (defined as SpO2 < 92% or PaO2 < 60 mmHg without evidence of incorrect tube placement, airway obstruction, or hemodynamic impairment), immediate rescue recruitment maneuvers were performed on the ventilated lung. If this maneuver failed to enhance oxygenation, we incrementally increased the FiO2 and applied continuous positive airway pressure of 5 cmH2O to the nonventilated lung.
Outcome measures
The primary outcome was a composite of PPCs during hospital stay (respiratory infection, respiratory failure, pleural effusion, atelectasis, pneumothorax and bronchospasm) [23, 24]. Secondary outcomes included: the severity grade of pulmonary complications [25]; length of hospital stay; all-cause mortality during hospital stay and at postoperative day 30. The severity grade of PPCs was scored on a 0–5 scale, where 0 indicates no symptoms or signals of PPCs, grades 1–4 indicates successively worse forms of complications, and grade 5 indicates death before discharge (A description of the diagnosis of PPCs and the severity grade of PPCs is given in Appendix 1, Table S1 and Table S2).
Baseline characteristics, intraoperative surgery- and anesthesia-related data were recorded. Intraoperative mechanical ventilation parameters were collected at four timepoints: 1) T1-lateral position during TLV; 2) T2- lateral position after 10 min of OLV; 3) T3-lateral position after 1 h of OLV; 4) T4-TLV after surgery. Ventilation data was collected every hour during OLV. Outcomes were evaluated every afternoon by trained investigators during postoperative visits until discharge and at postoperative day 30 by telephone.
Exposure
The primary exposure was MP measured after 1 h of OLV (T3). The following equation was applied to calculate MP, norMP and MP/Crs:
Statistical analysis
Sample size was calculated using the rule of ten [26, 27]. Sample size = 10 × number of factors and cofactors/incidence of PPCs. On the basis of a 22% incidence of pulmonary complications after lung resection surgery [28, 29], 13 factors and a dropout rate of 5%, we estimated a sample size of 622 patients would be sufficient for this study.
Continuous variables were described as mean [standard deviation {SD}] or median [interquartile range {IQR}] and analyzed using the Student t test or the Mann–Whitney U test for normal or nonnormal distributions, respectively. Normality was tested using the Shapiro–Wilk test. Categorical variables were described as frequencies (percentages) and analyzed using Pearson’s test or Fisher’s exact tests. Data were analyzed with multivariable logistic regression, which provided odds ratios (OR) with 95% confidence intervals (CIs). Cofactors were included if they affected the outcome variable univariately (P < 0.1). If two factors were correlated (Variance inflation factor > 10), one of the factors would be excluded according to clinical considerations. Missing data were not addressed as < 5% of data for postoperative assessments were missing. A 2-tailed P value of < 0.05 was considered statistically significant. All analyses were conducted using IBM SPSS Statistics software (version 23.0).
Results
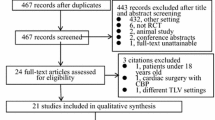
Between April 2022 and November 2022, we recruited 622 patients in total and 609 participants were analyzed in this study. Figure 1 illustrates details about the enrolled and excluded participants. Baseline characteristics of patients are shown in Table 1. In this study, median age was 55 years old and the majority of patients (68.1%) were female. Median duration of OLV was 90 min, thus ventilation parameters during OLV were only obtained twice in most patients. Ventilation characteristics of patients are presented in Table 2. The ventilation data at T4 of one patient were not collected. Ventilation parameters including MP at any study time-point were similar between patients with PPCs and patients without PPCs (Table 2). The distribution of MP during OLV is shown in Fig. 2.
The incidence of pulmonary complications after surgery during hospital stay was 24.6% (150 of 609 patients). The most common pulmonary complications were respiratory failure in 71 (11.7%) patients, atelectasis in 70 (11.5%) patients and respiratory infection in 18 (3.0%) patients. Results of the univariable analysis of the primary outcome are shown in Table 1. And there was no association between MP and in-hospital PPCs in the multivariable analysis (Fig. 3). In addition, MP was replaced by norMP and MP/Crs separately in multivariable analysis, and we did not detect association between norMP or MP/Crs and PPCs.
Odds ratio for postoperative pulmonary complications. ASA: American Society of Anesthesiologists; ARISCAT = Assess Respiratory Risk in Surgical Patients in Catalonia; FEV1/FVC: Forced expiratory volume in one second/Forced vital capacity; OLV: One-lung ventilation; MP: Mechanical power; Crs: Compliance of the respiratory system
During hospital stay, 14 and 6 patients experienced mild and moderate PPCs, respectively. The association between MP and the severity grade of PPCs cannot be assessed due to insufficient data. The length of hospital stay in patients with PPCs was longer than patients without PPCs (5[4–7] vs 4[4, 5], p < 0.001). There were no deaths during hospital stay and at postoperative day 30.
Discussion
In this study conducted in patients undergoing thoracoscopic lung resection surgery, there existed no link between MP and the incidence of PPCs during hospital stay in the context of lung-protective ventilation.
Ventilation characteristics keep changing over time during mechanical ventilation. According to the classical equation of MP proposed by Gattinoni et al. [9], the same MP can be achieved by different ventilation parameters, allowing MP a holistic indicator for monitoring mechanical ventilation. The effect of low tidal volume with or without PEEP on PPCs was uncertain, which indicated that MP was probably the determinant of pulmonary complications pathogenesis [5, 6].
Previous retrospective data suggested that elevated MP was associated with higher mortality in critically ill patients [11, 30,31,32]. Several clinical trials showed that the MP in ARDS patients receiving mechanical ventilation ranged from 15 to 29 J/min [11,12,13, 31]. Compared with ARDS patients, the absolute MP value was lower in surgical patients, though research about MP in surgical population was limited. Two clinical trials investigating general anesthesia outcomes reported that the MP in patients with PPCs or postoperative respiratory failure requiring reintubation was around 7.7 J/min [16, 17]. Karalapillai et al. [15] concluded that a higher MP was independently associated with higher risk of PPCs in surgical patients, and median MP of overall participants was 9.0 (7.0–11.4) J/min. However, so far, limited clinical data is available on the safe threshold of MP for developing PPCs in thoracic patients.
The incidence of PPCs in our study was 24.6%, which was on par with that observed in similar studies [23, 29]. Under lung-protective ventilation strategies including low tidal volume, optimal application of PEEP and recruitment maneuvers, we found MP was not associated with pulmonary complications after thoracoscopic lung resection surgery. However, Chiumello et al. [14] found that patients who developed PPCs had higher MP value during OLV (14.37 ± 8.19 vs 10.44 ± 2.82 J/min, p = 0.059) than patients without PPCs. Possible reasons for this discrepancy: 1) higher age (72 vs 55, y); 2) longer duration of OLV (137 vs 90, min); 3) patients with previous lung surgery (16.7% vs 0%); 4) larger VT and RR during OLV. In addition, the median MP during OLV in patients with PPCs in our study was 6.76 J/min. Notably, this value was significantly lower than the corresponding MP value reported in Chiumello’s study (14.37 J/min) [14] and in Suleiman’s study (9.8 J/min) [33]. In this study, four patients exhibited a MP exceeding 12 J/min, the threshold previously suggested as detrimental in ARDS patients [34]. Among these, two patients subsequently developed PPCs. Though a higher intensity of OLV measured by MP was dose-dependently associated with postoperative respiratory failure, high absolute MP value may not result in adverse outcomes [33].
Based on these above and existed evidence about high MP in ARDS patients, we suspected that MP is a beneficial indicator for critically ill patients or patients requiring long-time surgery. In other words, MP can evaluate precisely patients’ prognosis when there existed great previous lung injuries or injuries caused by the ventilator.
To our knowledge, this is the largest prospective observational study to explore the association between MP and PPCs in thoracic surgical patients. Our findings could be generalized to ventilation approaches in thoracoscopic lung resection surgery using OLV. The present analysis also has some limitations. First, MP was determined by several ventilation variables, and the interaction among these variables during mechanical ventilation may confuse the association between MP and postoperative outcomes. In our study, the ventilator settings were similar among all participants, however, manipulating a single variable (such as PEEP), which correlates with variations in delivered MP, is likely a better approach to delineating its impact as Schujit et al. [35] investigated. Second, the result may not be wholly generalizable to other practices because the participants in our center were relatively young with healthy and underwent procedures of relatively short duration. Third, measurements of esophageal pressure were lacking. Therefore, MP calculating in our study was delivered by the ventilator to the whole respiratory system rather than lung separately. We used airway pressure instead of transpulmonary pressure to calculate MP, which was more accordant with clinical practice.
Conclusions
In a population of patients undergoing thoracoscopic lung resection with standardized lung-protective ventilation, we did not detect an association between mechanical power and postoperative pulmonary complications.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ARDS:
-
Acute respiratory distress syndrome
- ARISCAT:
-
Assess Respiratory Risk in Surgical Patients in Catalonia
- ASA:
-
American Society of Anesthesiologists
- BIS:
-
Bispectral index
- CI:
-
Confidence interval
- ETCO2 :
-
End-tidal carbon dioxide
- IQR:
-
Interquartile range
- MP:
-
Mechanical power
- OLV:
-
One-lung ventilation
- OR:
-
Odds ratio
- PBW:
-
Predicted body weight
- PEEP:
-
Positive end-expiratory pressure
- PPCs:
-
Postoperative pulmonary complications
- RR:
-
Respiratory rate
- SD:
-
Standard deviation
- STORBE:
-
Strengthening the reporting of observational studies in epidemiology
- TLV:
-
Two-lung ventilation
- TOF:
-
Train of four
- VT :
-
Tidal volume
References
Shelley B, McCall P, Glass A, Orzechowska I, Klein A, Association of Cardiothoracic A, et al. Outcome following unplanned critical care admission after lung resection. JTCVS Open. 2022;9:281–90.
Batchelor TJP, Rasburn NJ, Abdelnour-Berchtold E, Brunelli A, Cerfolio RJ, Gonzalez M, et al. Guidelines for enhanced recovery after lung surgery: recommendations of the Enhanced Recovery After Surgery (ERAS(R)) Society and the European Society of Thoracic Surgeons (ESTS). Eur J Cardiothorac Surg. 2019;55(1):91–115.
Gao S, Barello S, Chen L, Chen C, Che G, Cai K, et al. Clinical guidelines on perioperative management strategies for enhanced recovery after lung surgery. Transl Lung Cancer Res. 2019;8(6):1174–87.
Young CC, Harris EM, Vacchiano C, Bodnar S, Bukowy B, Elliott RRD, et al. Lung-protective ventilation for the surgical patient: international expert panel-based consensus recommendations. Br J Anaesth. 2019;123(6):898–913.
Colquhoun DA, Leis AM, Shanks AM, Mathis MR, Naik BI, Durieux ME, et al. A lower tidal volume regimen during one-lung ventilation for lung resection surgery is not associated with reduced postoperative pulmonary complications. Anesthesiology. 2021;134(4):562–76.
Karalapillai D, Weinberg L, Peyton P, Ellard L, Hu R, Pearce B, et al. Effect of intraoperative low tidal volume vs conventional tidal volume on postoperative pulmonary complications in patients undergoing major surgery: a randomized clinical trial. JAMA. 2020;324(9):848–58.
Kiss T, Wittenstein J, Becker C, Birr K, Cinnella G, Cohen E, et al. Protective ventilation with high versus low positive end-expiratory pressure during one-lung ventilation for thoracic surgery (PROTHOR): study protocol for a randomized controlled trial. Trials. 2019;20(1):213.
Hemmes SN, de Abreu Gama M, Pelosi P, Schultz MJ. High versus low positive end-expiratory pressure during general anaesthesia for open abdominal surgery (PROVHILO trial): a multicentre randomised controlled trial. Lancet. 2014;384(9942):495–503.
Gattinoni L, Tonetti T, Cressoni M, Cadringher P, Herrmann P, Moerer O, et al. Ventilator-related causes of lung injury: the mechanical power. Intensive Care Med. 2016;42(10):1567–75.
Tonna JE, Peltan I, Brown SM, Herrick JS, Keenan HT. Mechanical power and driving pressure as predictors of mortality among patients with ARDS. Intensive Care Med. 2020;46(10):1941–3.
Serpa Neto A, Deliberato RO, Johnson AEW, Bos LD, Amorim P, Pereira SM, et al. Mechanical power of ventilation is associated with mortality in critically ill patients: an analysis of patients in two observational cohorts. Intensive Care Med. 2018;44(11):1914–22.
Zhang Z, Zheng B, Liu N, Ge H, Hong Y. Mechanical power normalized to predicted body weight as a predictor of mortality in patients with acute respiratory distress syndrome. Intensive Care Med. 2019;45(6):856–64.
Coppola S, Caccioppola A, Froio S, Formenti P, De Giorgis V, Galanti V, et al. Effect of mechanical power on intensive care mortality in ARDS patients. Critical care (London, England). 2020;24(1):246.
Chiumello D, Formenti P, Bolgiaghi L, Mistraletti G, Gotti M, Vetrone F, et al. Body position alters mechanical power and respiratory mechanics during thoracic surgery. Anesth Analg. 2020;130(2):391–401.
Karalapillai D, Weinberg L, Neto AS, Peyton P, Ellard L, Hu R, et al. Intra-operative ventilator mechanical power as a predictor of postoperative pulmonary complications in surgical patients: a secondary analysis of a randomised clinical trial. Eur J Anaesthesiol. 2022;39(1):67–74.
Santer P, Wachtendorf LJ, Suleiman A, Houle TT, Fassbender P, Costa EL, et al. Mechanical power during general anesthesia and postoperative respiratory failure: a multicenter retrospective cohort study. Anesthesiology. 2022;137(1):41–54.
Ball L, Volta CA, Saglietti F, Spadaro S, Di Lullo A, De Simone G, et al. Associations between expiratory flow limitation and postoperative pulmonary complications in patients undergoing cardiac surgery. J Cardiothorac Vasc Anesth. 2022;36(3):815–824.
Brochard L, Bersten A. Mechanical power: a biomarker for the lung? Anesthesiology. 2019;130(1):9–11.
de Abreu Gama M, Sessler DI. Mechanical Power: Correlate or Cause of Ventilator-induced Lung Injury? Anesthesiology. 2022;137(1):6–8.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet. 2007;370(9596):1453–7.
Shi W, Chen Y, Zhang M-Q, Che G-W, Yu H. Effects of methylprednisolone on early postoperative pain and recovery in patients undergoing thoracoscopic lung surgery: A randomized controlled trial. J Clin Anesth. 2021;75:110526.
Zhi XY, Liu LX, Writing Committee of Chinese Guidelines for Perioperative Airway Management in Thoracic Surgery(2020 edition). Chinese guidelines for perioperative airway management in thoracic surgery (2020 edition). Chin J Clin Thoracic Cardiovasc Surg. 2021;28(3):251–62.
Li XF, Jin L, Yang JM, Luo QS, Liu HM, Yu H. Effect of ventilation mode on postoperative pulmonary complications following lung resection surgery: a randomised controlled trial. Anaesthesia. 2022;77(11):1219–27.
Jammer I, Wickboldt N, Sander M, Smith A, Schultz MJ, Pelosi P, et al. Standards for definitions and use of outcome measures for clinical effectiveness research in perioperative medicine: European Perioperative Clinical Outcome (EPCO) definitions: a statement from the ESA-ESICM joint taskforce on perioperative outcome measures. Eur J Anaesthesiol. 2015;32(2):88–105.
Li XF, Jiang D, Jiang YL, Yu H, Zhang MQ, Jiang JL, et al. Comparison of low and high inspiratory oxygen fraction added to lung-protective ventilation on postoperative pulmonary complications after abdominal surgery: a randomized controlled trial. J Clin Anesth. 2020;67:110009.
Kirmeier E, Eriksson LI, Lewald H, Jonsson Fagerlund M, Hoeft A, Hollmann M, et al. Post-anaesthesia pulmonary complications after use of muscle relaxants (POPULAR): a multicentre, prospective observational study. Lancet Respir Med. 2019;7(2):129–40.
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR. A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol. 1996;49(12):1373–9.
de la Gala F, Piñeiro P, Reyes A, Vara E, Olmedilla L, Cruz P, et al. Postoperative pulmonary complications, pulmonary and systemic inflammatory responses after lung resection surgery with prolonged one-lung ventilation. Randomized controlled trial comparing intravenous and inhalational anaesthesia. Br J Anaesth. 2017;119(4):655–63.
Li XF, Hu JR, Wu Y, Chen Y, Zhang MQ, Yu H. Comparative effect of propofol and volatile anesthetics on postoperative pulmonary complications after lung resection surgery: a randomized clinical trial. Anesth Analg. 2021;133:949.
Jiang X, Zhu Y, Zhen S, Wang L. Mechanical power of ventilation is associated with mortality in neurocritical patients: a cohort study. J Clin Monit Comput. 2022;36(6):1621–8.
Parhar KKS, Zjadewicz K, Soo A, Sutton A, Zjadewicz M, Doig L, et al. Epidemiology, mechanical power, and 3-year outcomes in acute respiratory distress syndrome patients using standardized screening. An observational cohort study. Ann Am Thorac Soc. 2019;16(10):1263–72.
van Meenen DMP, Algera AG, Schuijt MTU, Simonis FD, van der Hoeven SM, Neto AS, et al. Effect of mechanical power on mortality in invasively ventilated ICU patients without the acute respiratory distress syndrome. Eur J Anaesthesiol. 2023;40(1):21–8.
Suleiman A, Azizi BA, Munoz-Acuna R, Ahrens E, Tartler TM, Wachtendorf LJ, et al. Intensity of one-lung ventilation and postoperative respiratory failure: a hospital registry study. Anaesth Crit Care Pain Med. 2023;42(5):101250.
Guerin C, Papazian L, Reignier J, Ayzac L, Loundou A, Forel JM, et al. Effect of driving pressure on mortality in ARDS patients during lung protective mechanical ventilation in two randomized controlled trials. Crit Care. 2016;20(1):384.
Schuijt MTU, Hol L, Nijbroek SG, Ahuja S, van Meenen D, Mazzinari G, et al. Associations of dynamic driving pressure and mechanical power with postoperative pulmonary complications–posthoc analysis of two randomised clinical trials in open abdominal surgery. eClinicalMedicine. 2022;47:101397.
Acknowledgements
The authors thank all the participants and all the research staff.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
HML analyzed the data, and prepared the manuscript. GWZ helped collect the data. Hong Yu helped design the study and revised the final version of the manuscript. XFL helped design the study, analyzed the data, and revised the manuscript. Hai Yu designed the study, revised and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by Ethical Committee of the West China Hospital of Sichuan University (Ethical Committee No.2021 (1580) and registered at the Chinese Clinical Trial Registry (ChiCTR2200058528, principal investigator: Hai Yu, date of registration: April 10, 2022) before the first patient was enrolled. This report adheres to the applicable STrengthening the Reporting of OBservational studies in Epidemiology (STORBE) statement.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, HM., Zhang, GW., Yu, H. et al. Association between mechanical power during one-lung ventilation and pulmonary complications after thoracoscopic lung resection surgery: a prospective observational study. BMC Anesthesiol 24, 176 (2024). https://doi.org/10.1186/s12871-024-02562-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-024-02562-1