Abstract
Background
Electronic health records (EHR) contain large volumes of unstructured free-form text notes that richly describe a patient’s health and medical comorbidities. It is unclear if perioperative risk stratification can be performed directly from these notes without manual data extraction. We conduct a feasibility study using natural language processing (NLP) to predict the American Society of Anesthesiologists Physical Status Classification (ASA-PS) as a surrogate measure for perioperative risk. We explore prediction performance using four different model types and compare the use of different note sections versus the whole note. We use Shapley values to explain model predictions and analyze disagreement between model and human anesthesiologist predictions.
Methods
Single-center retrospective cohort analysis of EHR notes from patients undergoing procedures with anesthesia care spanning all procedural specialties during a 5 year period who were not assigned ASA VI and also had a preoperative evaluation note filed within 90 days prior to the procedure. NLP models were trained for each combination of 4 models and 8 text snippets from notes. Model performance was compared using area under the receiver operating characteristic curve (AUROC) and area under the precision recall curve (AUPRC). Shapley values were used to explain model predictions. Error analysis and model explanation using Shapley values was conducted for the best performing model.
Results
Final dataset includes 38,566 patients undergoing 61,503 procedures with anesthesia care. Prevalence of ASA-PS was 8.81% for ASA I, 31.4% for ASA II, 43.25% for ASA III, and 16.54% for ASA IV-V. The best performing models were the BioClinicalBERT model on the truncated note task (macro-average AUROC 0.845) and the fastText model on the full note task (macro-average AUROC 0.865). Shapley values reveal human-interpretable model predictions. Error analysis reveals that some original ASA-PS assignments may be incorrect and the model is making a reasonable prediction in these cases.
Conclusions
Text classification models can accurately predict a patient’s illness severity using only free-form text descriptions of patients without any manual data extraction. They can be an additional patient safety tool in the perioperative setting and reduce manual chart review for medical billing. Shapley feature attributions produce explanations that logically support model predictions and are understandable to clinicians.
Similar content being viewed by others
Background
Machine learning and natural language processing (NLP) techniques, coupled with adoption of electronic health records (EHR), and widespread availability of high-performance computational resources offer new avenues for perioperative risk stratification whereby free-form text sources, such as medical notes, may be directly loaded into prediction models without the need to define, input or abstract predetermined data elements (e.g. diagnoses, medications, etc.). This offers the opportunity to use these techniques for preoperative assessment triage, flagging of critical/pertinent data in a voluminous electronic medical record, and a variety of other use cases based on clinician notes, which often contain narratives that richly and concisely describe a nuanced clinical picture of the patient while simultaneously prioritizing the clinician’s pertinent concerns. Unlike historical keyword-based approaches, modern NLP techniques using large pretrained language models are able to account for inter-word dependencies across the entire text sequence and have been shown to achieve state of the art performance on a variety of NLP tasks [1,2,3,4] including text classification [5, 6]. However, it is unknown whether these techniques can be successfully applied to perioperative risk stratification.
In this feasibility study, we hypothesize that NLP models can be applied to unstructured anesthesia preoperative evaluation notes written by clinicians to predict the American Society of Anesthesiologists Physical Status (ASA-PS) score [7, 8]. These preoperative evaluation notes are a pertinent summary of the patient’s medical and surgical history and describe why the patient is having surgery, all of which reflect the patient’s pre-anesthesia medical comorbidities that the ASA-PS aims to represent. In particular, we investigate four different text classification approaches that span the spectrum of historical and modern techniques: (1) random forest [9] with n-gram and term frequency-inverse document frequency (TFIDF) transform [10], (2) support vector machine [11] with n-gram and TFIDF transform, (3) fastText [12, 13] word vector model, and (4) BioClinicalBERT deep neural network language model. We also investigate the impact of using the entire note versus specific note sections. We compare the model’s prediction against the ASA-PS assigned by the anesthesiologist on the day of surgery and assess catastrophic errors made by one of these models. Finally, we use Shapley values to visualize which sections of note text were associated with the model’s predictions to explain these catastrophic errors. This approach shows that it is possible for clinicians to understand how complex NLP models are making their predictions, which is an important criteria for clinical adoption.
Methods
This retrospective study of routinely collected health records data was approved by the University of Washington Institutional Review Board with a waiver of consent. This study followed the Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis (TRIPOD) guideline [14] and other guidelines specific to machine learning projects [15,16,17]. Figure 1 depicts a flow diagram of study design.
Study cohort
Inclusion criteria were patients who had a procedure with anesthesia at the University of Washington Medical Center or Harborview Medical Center from January 1, 2016 – March 29, 2021 where the patient also had an anesthesia preoperative evaluation note filed up to 6 h after the anesthesia end time. This 6-h grace period reflects the reality that in some urgent or emergency situations or due to EHR behavior, text documentation may be time stamped out of order.
The anesthesia preoperative evaluation note must have contained the following sections: History of Present Illness (HPI), Past Medical and Surgical History (PMSH), Review of Systems (ROS), and Medications; notes missing at least one of these sections were excluded. No other note type was used. Cases must have had a recorded value for ASA-PS assigned by the anesthesiologist of record, a free-form text Procedure description, and a free-form text Diagnosis description; cases missing at least one of these values are excluded.
A unit of analysis is defined as a single case with an anesthesia preoperative evaluation note filed within 90 days of the procedure. This unit was chosen because ASA-PS is typically recorded on a per-case basis by the anesthesiologist to reflect the patient’s pre-anesthesia medical comorbidities at the time of the procedure. Likewise, preoperative evaluation notes filed > 90 days before the case may not reflect the patient’s current state of health, so are excluded. Data was randomly split 70%-10%-20% into training, validation, and test datasets respectively. Patients with multiple cases were randomized into a single data split to avoid information leakage between the three datasets. New case number identifiers were generated for this study and used to refer to each case.
Outcomes
The outcome variable is a modified ASA-PS with valid values of ASA I, ASA II, ASA III, ASA IV-V. ASA V cases are extremely rare, resulting in class imbalances that affect model training and performance. Thus ASA IV and V were combined into a compound class “IV-V”. ASA VI organ procurement cases are excluded. The final categories retain the spirit of the ASA-PS for perioperative risk stratification and resembles the original ASA-PS devised by Saklad in 1941 [7, 18]. The emergency surgery modifier “E” was discarded.
Predictors and data preparation
Free-form text from the anesthesia preoperative evaluation note is organized into many sections. Regular expressions are used to extract HPI, PMSH, ROS, and medications from the note. While diagnosis and procedure sections exist within the note, they were less frequently documented than in the procedural case booking data from the surgeon. Therefore, free-form text for these sections were taken from the case booking. Newline characters and whitespaces were removed from the text. Note section headers were excluded so that only the body of text from each section is included. We used text from each section to train models for ASA-PS prediction, resulting in 8 prediction tasks: Diagnosis, Procedure, HPI, PMSH, ROS, Medications (Meds), Note, Truncated Note (Note512). “Note” refers to using the whole note text as the predictor to train a model. When BioClinicalBERT is applied to the “Note” task, the WordPiece tokenizer [19,20,21] truncates input text to 512 tokens. This truncation does not occur for other models. For equitable comparison across models, we define the “Note512” task, which truncates the note text to the first 512 tokens used by the BioClinicalBERT model.
Statistical analysis and modeling
Four model architectures with different conceptual underpinnings were trained: (1) Random forest (RF) [9], (2) Support vector machine (SVM) [11], (3) fastText, [12, 13], and (4) BioClinicalBERT [22]. Each model architecture was trained on each of the 8 prediction tasks for a total of 32 final models.
Each model was trained on the training dataset. Model hyperparameters were tuned using Tune [23] with the BlendSearch [24, 25] algorithm to maximize Matthew’s Correlation Coefficient (MCC) computed on the validation dataset. The number of hyperparameter tuning trials was selected to be 20 times the number of model hyperparameters with early stopping if the MCC of the last 3 trials reaches a plateau with standard deviation < 0.001. The best model was then evaluated on the held-out test dataset. Details on the approach taken for each of the four model architectures is available in Supplemental methods.
Baseline models
Two baseline models were created for comparison: a random classifier model and an age & medications classifier model. The random classifier model generates a random prediction without using any features, thus serving as a negative control baseline. The age & medications classifier model serves as a simple clinical baseline model. It uses the patient’s age, medication list, and total medication count as input features to a multiclass logistic regression model with cross-entropy loss and L2 penalty for predicting the modified ASA-PS outcome variable. Defaults were used for all other model parameters. Both baselines were implemented using Scikit-learn.
Evaluation metrics
Final models were evaluated on the held-out test dataset by computing both class-specific and class-aggregate performance metrics. Class-specific metrics include: receiver operator characteristic (ROC) curve, area under receiver operator curve (AUROC), precision-recall curve, area under precision-recall curve (AUPRC), precision (positive predictive value), recall (sensitivity), and F1. Class-aggregate performance metrics include MCC and AUCμ, [26] a multiclass generalization of the binary AUROC. Additionally, macro-average AUROC, AUPRC, precision, recall and F1 were also computed. Each metric and model-task combination was computed with 1000 bootstrap iterations each with 100,000 bootstrap samples on the test set. For each metric, p-values were computed for all 400 pairwise model-task comparisons with the Mann–Whitney U test followed by Benjamini–Hochberg procedure to control false discovery rate with α = 0.01.
Model interpretability and error analysis
4-by-4 contingency tables were generated to visualize the distribution of model errors. Catastrophic errors were defined as cases where the model predicts ASA IV-V but the anesthesiologist assigned ASA I, or vice versa. For catastrophic errors made by the BioClinicalBERT model with the Note512 task, three new anesthesiologist raters independently assigned an ASA-PS based on only the input text from the Note512 task. These new ASA-PS ratings were compared against the original anesthesiologist’s ASA-PS as well as the model prediction’s ASA-PS.
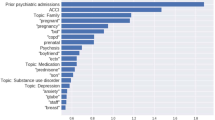
The SHAP [27] python package was used to train a Shapley values feature attribution model on the test dataset to understand which words support prediction of each modified ASA-PS outcome variable. An analysis of model errors with Shapley value feature attributions was reviewed for each of the catastrophic error examples with representative examples included in the manuscript. Shapley values for predicting each ASA-PS are visualized as a heatmap over text examples. Text examples are de-identified by replacing ages, dates, names, locations, and entities with pseudonyms to achieve data obfuscation while preserving structural similarity to the original passage.
Results
Our study comprised 38,566 patients undergoing 61,503 procedures with anesthesia care with 46,275 notes. Baseline patient, procedure, and note characteristics are described in Table 1. A flow diagram describing dataset creation is shown in Fig. 2. A total of 30 class-aggregate and class-specific metrics were computed; 400 pairwise comparisons exist for each metric resulting in 12,000 pairwise comparisons. Only 20 of these pairwise comparisons are not statistically significant (Supplemental Tables 7 and 8). All comparisons across the same model type and varying the task, or across the same task and varying model are statistically significant for reported metrics.
AUROC for each model architecture and task is shown in Table 2; AUPRC is shown in Table 3; AUCµ and MCC is shown in Supplemental Table 1. RF, SVM, and fastText perform best using the entire note compared to note sections. Tasks with longer text snippets yielded better performance–HPI, ROS and Meds sections result in better model performance as compared to Diagnosis, Procedure, and PMSH. On the Note task, fastText performs the best. On the Note512 task, BioCinicalBERT performs the best.
Direct comparison of models is most appropriate using the Note512 task since all models are given the same information content. For the Note512 task, BioClinicalBERT has better class-aggregate performance across AUROC, AUPRC, AUCμ, MCC, F1 (Supplemental Table 2) compared to other models. While F1 for both fastText and BioClinicalBERT are similar, fastText achieves this with higher macro-precision (positive predictive value) (Supplemental Table 3) whereas BioClinicalBERT achieves this with higher macro-recall (sensitivity) (Supplemental Table 4). Class-specific metrics show that fastText’s worse recall is due to imbalanced recall performance with higher recall for ASA II and III which are the most prevalent classes, but poor recall for ASA I and IV-V. Conversely BioClinicalBERT has worse precision than fastText on all classes except for ASA III. BioClinicalBERT has similar or better AUROC and AUPRC across all the ASA-PS classes. This is also seen in the ROC curves (Fig. 3) and the precision-recall curves (Fig. 4), in which the BioClinicalBERT model shows slightly better performance across most thresholds.
Figure 5 depicts 4-by-4 contingency tables to visualize distribution of model errors on the Note512 task. When erroneous predictions occur, they are typically adjacent to the ASA-PS assigned by the original anesthesiologist. In the analysis of 40 catastrophic errors made by the BioClinicalBERT model on the Note512 task, the mean absolute difference between the model prediction and a new anesthesiologist rater is 1.025 whereas the difference from the original anesthesiologist is 3 (Fig. 6). This disparity with the original anesthesiologist and greater concordance with the new anesthesiologist rater indicates that some of the “incorrect predictions” on the test set are not true failures of the model but issues with data quality documented in routine clinical care.
4-by-4 contingency tables for each model architecture on the Note512 task. The vertical axis corresponds to modified ASA-PS recorded in the anesthetic record by the anesthesiologist. The horizontal axis corresponds to the model predicted modified ASA-PS. Numbers in the table represent case count from the test set. Percentages are case counts normalized over the model predicted ASA-PS, representing the distribution of actual ASA-PS recorded in the anesthetic record for a specific model predicted ASA-PS. Cells outlined in red in the BioClinicalBERT contingency table correspond to our definition of catastrophic errors. The 21 cases where anesthesiologist assigned ASA I and BioClinicalBERT model predicted ASA IV-V comprise 1.7% of all cases. The 19 cases where anesthesiologist assigned ASA IV-V and BioClinicalBERT model predicted ASA I comprise 1.6% of all cases
Rater assignments of ASA-PS for catastrophic error examples from the BioClinicalBERT model on Note512 task. Top plot shows scenario where model prediction is ASA IV-V, but original anesthesiologist assigned case ASA I. Bottom plot shows scenario where model prediction is ASA I, but original anesthesiologist assigned case ASA IV-V. Three anesthesiologist raters were asked to read the input text from the Note512 task and assign an ASA-PS for each of the catastrophic error examples. For each case, a dot marks a rater’s ASA-PS assignment. The model’s prediction and original anesthesiologist ASA-PS is shown as a highlighted region overlaid on the plots. Shapley feature attribution visualizations are shown for cases #57482 (Fig. 7, Supplemental Fig. 2), #41739 (Supplemental Fig. 3), #11950 (Supplemental Fig. 4), #29054 (Supplemental Fig. 5)
Shapley values in Fig. 7 provide clinically plausible explanations for model explanations, highlighting the directional probability of how specific input text contributes to predicting a specific ASA-PS. These feature attributions often provide clinically plausible explanations for why a model is making a wrong prediction and allows the clinician to evaluate the evidence the model is considering. Additional examples shown in Supplemental Figs. 2, 3, 4 and 5.
Attribution of input text features to predicting modified ASA-PS for the BioClinicalBERT model on Note512 task. Shapley values for each text token is shown to compare feature attributions to ASA I (top) and feature attributions to ASA IV-V (bottom). Red tokens positively support predicting the target ASA-PS whereas blue tokens do not support predicting the target ASA-PS. The magnitude and direction of support is overlaid on a force plot above the text. The baseline probability of predicting each class in the test set is shown as the “base value” on the force plot. The base value + sum of Shapley values from each token corresponds to the probability of predicting the ASA-PS and is shown as the bolded number. For simplicity, feature attributions to ASA II and III are omitted in this figure, but a full-visualization with all outcome ASA-PS for this text snippet is available in Supplemental Fig. 2. Text examples are de-identified by replacing ages, dates, names, locations, and entities with pseudonyms to achieve data obfuscation while preserving structural similarity to the original passage
Discussion
In this study of ASA-PS prediction using NLP techniques, we found that more advanced models made fewer categorization errors. Further, an assessment of catastrophic errors made by the BioClinicalBERT model suggests that, in the majority of cases, expert review suggested the initial ASA-PS score assigned by the anesthesiologist was erroneous rather than the ASA-PS score assigned by the NLP model. Shapley value feature attributions enable a clinician to easily identify if the model predictions are erroneous or clinically plausible. From these feature attributions, we find NLP models are able to associate both obvious and subtle clinical cues to the patient’s illness severity.
Text classification techniques have undergone substantial evolution over the past decade. Most of these techniques will be unfamiliar to the practicing clinician. In brief, RF and SVM represent more rudimentary approaches that utilize bag-of-words and n-grams. These techniques are sensitive to word misspellings, cannot easily account for word order, have difficulty in capturing long-range references within sentences, and have difficulty in representing different meanings of a word when the same word appears in different contexts [28,29,30,31,32,33].
Modern NLP techniques have overcome many of these challenges with vector space representation of words [12, 13, 34,35,36] and subword components [13, 19, 20, 37] as seen in the fastText model, attention mechanism [38, 39], and pretrained deep autoregressive neural networks [40,41,42] such as transformer neural networks [43]. This has resulted in successful large language models such as BERT [21, 44] and the domain-specific BioClinicalBERT [22]. Perhaps the most widely known large language model is ChatGPT (OpenAI, San Francisco, CA), a general purpose chatbot based on the GPT-3 model which contains 175 billion parameters [45]. In contrast, BioClinicalBERT used in this feasibility study contains roughly 1500 times fewer parameters, but has been trained specifically on clinical notes which makes it well suited for the ASA-PS prediction task [46].
Longer text length provides more information for the model to make an accurate prediction. Even though text snippets such as Diagnosis or Procedure may have high relevance for the illness severity of the patient, the better performance on longer input text sequences indicate that more information is generally better. This is similar to what is observed in the multifaceted practice of clinical medicine–where a patient’s overall clinical status is often better understood as the sum of many weaker but synergistic signals rather than a single descriptor. The limited input sequence length for BioClinicalBERT creates a performance ceiling as it limits the amount of information available to the model. Comparing Note and Note512 tasks, all other models that can utilize the full note have better performance when this input length is lifted with fastText being the top performer. These findings suggest that future development of a large language model similar to BioClinicalBERT capable of accepting a longer input context would likely have superior performance characteristics. fastText requires significantly less compute resources for model training and inference compared to BioClinicalBERT and remains a good option in lower resource settings. RF and SVM were our worst performing models, confirming that modern word vector and neural network language model-based approaches are superior.
There is significant variability on the length and quality of clinical free-form text narrative written in the note, especially in the HPI section which is typically a clinician’s narrative of the patient’s medical status and need for the procedure. In some cases, the HPI section contains one or two words in length (Supplemental Fig. 4), whereas in other cases it is a rich narrative (Supplemental Figs. 2, 5). We believe that relatively poor performance in the ASA-PS prediction using HPI alone is a consequence of variability in documentation, as the model may have limited information for prediction if the note text does not richly capture the clinical scenario.
These models rarely made catastrophic errors. Erroneous predictions are typically adjacent to the ASA-PS assigned by the anesthesiologist, suggesting the model is making appropriate associations between freeform text predictors and the outcome variable (Fig. 5). Furthermore, when new anesthesiologist raters were asked to assign ASA-PS to the cases where catastrophic errors occurred from the BioclinicalBERT model on the Note512 task, there was greater concordance between the model predictions and the new anesthesiologist rather than the original anesthesiologist (Fig. 6). Shapley feature attributions for one of these catastrophic errors in Fig. 7 reveal that the original anesthesiologist may have made the wrong assignment, or may have written a note that does not reflect the true clinical scenario. In this example, the original anesthesiologist assigned the case ASA IV-V, but the model predicted I. Feature attributions show the BioClinicalBERT model correctly identifies pertinent negatives on trauma exam, normal hematocrit of 33, and normal Glasgow Coma Scale (GCS) of 15 to all support a prediction for ASA I and against ASA IV-V [47]. In this example, all new anesthesiologist raters agree with the model rather than the original anesthesiologist. These findings from our catastrophic error analysis suggest that the model performance may be underestimated by our evaluation metrics, as our ground truth test set contains imperfect ASA-PS assignments. It also illustrates how the model is robust against potentially faulty labels. Despite a noisy training and evaluation set, NLP models are still able to make clinically appropriate ASA-PS predictions.
Our exploration of Shapley feature attributions reveal that the model is able to identify indirect indicators of a patient’s illness severity. For example, subcutaneous heparin is often administered for bed-bound inpatients to prevent the development of deep vein thrombosis. Supplemental Fig. 4 depicts an example where the model learns to associate mention of subcutaneous heparin in the medication list with a higher ASA-PS, likely because hospitalized patients are generally more ill than outpatients who present to the hospital for same-day surgery. Similarly, the model learns the association between the broad spectrum antibiotic ertapenem with a higher ASA-PS as compared to narrow spectrum or prophylactic antibiotics such as metronidazole or cefazolin. These observations show that the model is able to identify and link these subtle indicators to a patient’s illness severity. Shapley value feature attributions prove to be an effective tool that enables clinicians to understand how a model makes its prediction from text predictors.
Limitations
Our dataset is derived from a real-world EHR used to provide clinical care and includes human and computer generated errors. These issues include data entry and spelling, the use of abbreviations, references to other notes and test results not available to the model, and automatically generated/inserted text as part of a note template. For this feasibility study we use the anesthesia preoperative evaluation note. This note is typically written days or weeks in advance for elective procedures, but is sometimes written immediately prior, during, or after the procedure in urgent or emergent scenarios. These notes are included because our goal is to study the factors that affect ASA-PS prediction using note text with NLP models. We have not conducted clinical validation of these models and we have not validated model performance across multiple institutions.
The BioClinicalBERT model is limited to an input sequence of 512 tokens; future investigation is needed to understand if longer-context large language models can achieve better performance. We also did not explore more advanced NLP models such as those that perform entity and relation extraction, which may further enhance the prediction performance. Larger model sizes such as GPT-3 have been shown to be correlated with improved model performance across a variety of tasks, but these models are not specialized for the clinical domain; we do not explore these models in our feasibility study and leave this exploration to future research [48].
Finally, the ASA-PS is known to have only moderate interrater agreement among human anesthesiologists [49, 50]. Consequently, a perfect classification on this task is not possible since the ground truth labels derived from the EHR encapsulate this interrater variability.
Conclusions
Our feasibility assessment suggests that NLP models can accurately predict a patient’s illness severity using only free-form text descriptions of patients without any manual data extraction. They can be automatically applied to entire panels of patients, potentially allowing partial automation of preoperative assessment triage while also serving as a measure of perioperative risk stratification. Clinical decision support tools could use techniques like these to improve identification of comorbidities, resulting in improved patient safety. These tools may also be used at the healthcare system level for population health analyses and for billing purposes. Predictions made by more advanced NLP models benefit from explainability through Shapley feature attributions, which produce explanations that logically support model predictions and are understandable to clinicians. Future work includes assessment of more advanced natural language models that have more recently become available, use of non-anesthesiologist clinician notes, and exploration of NLP-based prediction of other outcome variables which may be less subject to interrater variability.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available because the text dataset derived from electronic health records comprises personal identifiable information (PII) and protected health information (PHI). Data may be requested by contacting Vikas O’Reilly-Shah at voreill@uw.edu or the University of Washington Center for Perioperative & Pain Initiatives in Quality Safety Outcome (PPiQSO) at PPiQSO@uw.edu. Data access is contingent upon a data use agreement in accordance with UW Medicine policy. Code for experiments and results is publicly available at https://github.com/philipchung/nlp-asa-prediction.
Abbreviations
- NLP:
-
Natural Language Processing
- EHR:
-
Electronic Health Record
- ASA-PS:
-
American Society of Anesthesiologists Physical Status
- TFIDF:
-
Term Frequency Inverse Document Frequency
- TRIPOD:
-
Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis
- HPI:
-
History of Present Illness
- PMSH:
-
Past Medical Surgical History
- ROS:
-
Review of Systems
- Meds:
-
Medications
- Note512:
-
Note truncated to 512 tokens by the BERT WordPiece tokenizer
- RF:
-
Random Forest
- SVM:
-
Support Vector Machine
- MCC:
-
Matthew’s Correlation Coefficient
- AUROC:
-
Area Under Receiver Operating Characteristic
- AUPRC:
-
Area Under Precision-Recall Curve
- AUCμ:
-
Area Under Curve Multiclass U-statistic
- F1:
-
Harmonic Mean of Precision and Recall
- GPT:
-
Generative Pre-trained Transformer
- GCS:
-
Glasgow Coma Scale
References
Rajpurkar P, Zhang J, Lopyrev K, Liang P. SQuAD: 100,000+ Questions for Machine Comprehension of Text. In: Proceedings of the 2016 Conference on Empirical Methods in Natural Language Processing. Austin: Association for Computational Linguistics; 2016. p. 2383–92.
Zellers R, Bisk Y, Schwartz R, Choi Y. SWAG: A Large-Scale Adversarial Dataset for Grounded Commonsense Inference. In: Proceedings of the 2018 Conference on Empirical Methods in Natural Language Processing. Brussels: Association for Computational Linguistics; 2018. p. 93–104.
Wang A, Singh A, Michael J, Hill F, Levy O, Bowman S. GLUE: A Multi-Task Benchmark and Analysis Platform for Natural Language Understanding. In: Proceedings of the 2018 EMNLP Workshop BlackboxNLP: Analyzing and Interpreting Neural Networks for NLP. Brussels: Association for Computational Linguistics; 2018. p. 353–5.
Wang A, Pruksachatkun Y, Nangia N, Singh A, Michael J, Hill F, et al. SuperGLUE: a stickier benchmark for general-purpose language understanding systems. In: Proceedings of the 33rd International Conference on Neural Information Processing Systems. Red Hook: Curran Associates Inc.; 2019. p. 3266–80.
Zhang Z, Liu J, Razavian N. BERT-XML: Large Scale Automated ICD Coding Using BERT Pretraining. In: Proceedings of the 3rd Clinical Natural Language Processing Workshop. Online: Association for Computational Linguistics; 2020. p. 24–34.
Liu L, Perez-Concha O, Nguyen A, Bennett V, Jorm L. Automated ICD coding using extreme multi-label long text transformer-based models. arXiv [cs.CL]. 2022.
Mayhew D, Mendonca V, Murthy BVS. A review of ASA physical status - historical perspectives and modern developments. Anaesthesia. 2019;74:373–9.
Horvath B, Kloesel B, Todd MM, Cole DJ, Prielipp RC. The evolution, current value, and future of the American Society of Anesthesiologists Physical Status Classification System. Anesthesiology. 2021;135:904–19.
Breiman L. Random Forests. Mach Learn. 2001;45:5–32.
Buckley C, Lewit AF. Optimization of inverted vector searches. In: Proceedings of the 8th annual international ACM SIGIR conference on research and development in information retrieval. New York: Association for Computing Machinery; 1985. p. 97–110.
Boser BE, Guyon IM, Vapnik VN. A training algorithm for optimal margin classifiers. In: Proceedings of the fifth annual workshop on Computational learning theory. New York: Association for Computing Machinery; 1992. p. 144–52.
Joulin A, Grave E, Bojanowski P, Mikolov T. Bag of Tricks for Efficient Text Classification. In: Proceedings of the 15th Conference of the European Chapter of the Association for Computational Linguistics: Volume 2, Short Papers. Valencia: Association for Computational Linguistics; 2017. p. 427–31.
Bojanowski P, Grave E, Joulin A, Mikolov T. Enriching Word Vectors with Subword Information. Transactions of the Association for Computational Linguistics. 2017;5:135–46.
Collins GS, Reitsma JB, Altman DG, Moons KGM. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD Statement. BMC Med. 2015;13:1.
Doshi-Velez F, Perlis RH. Evaluating Machine Learning Articles. JAMA. 2019;322:1777–9.
Liu Y, Chen P-HC, Krause J, Peng L. How to read articles that use machine learning: users’ guides to the medical literature. JAMA. 2019;322:1806–16.
Yusuf M, Atal I, Li J, Smith P, Ravaud P, Fergie M, Callaghan M, Selfe J. Reporting quality of studies using machine learning models for medical diagnosis: a systematic review. BMJ Open. 2020;10:e034568.
Saklad M. Grading of patients for surgical procedures. Anesthesiology. 1941;2:281–4.
Wu Y, Schuster M, Chen Z, et al. Google’s neural machine translation system: bridging the gap between human and machine translation. arXiv:1609.08144 [cs]. 2016.
Schuster M, Nakajima K. Japanese and Korean voice search. In: 2012 IEEE International Conference on Acoustics, Speech and Signal Processing (ICASSP). 2012. p. 5149–52.
Devlin J, Chang M-W, Lee K, Toutanova K. BERT: Pre-training of Deep Bidirectional Transformers for Language Understanding. In: Proceedings of the 2019 Conference of the North American Chapter of the Association for Computational Linguistics: Human Language Technologies, Volume 1 (Long and Short Papers). Minneapolis: Association for Computational Linguistics; 2019. p. 4171–86.
Alsentzer E, Murphy J, Boag W, Weng W-H, Jindi D, Naumann T, et al. Publicly Available Clinical BERT Embeddings. In: Proceedings of the 2nd Clinical Natural Language Processing Workshop. Minneapolis: Association for Computational Linguistics; 2019. p. 72–8.
Liaw R, Liang E, Nishihara R, Moritz P, Gonzalez JE, Stoica I. Tune: a research platform for distributed model selection and training. arXiv [cs.LG]. 2018.
Wang C, Wu Q, Weimer M, Zhu E. FLAML: A Fast and Lightweight AutoML Library. In: Fourth Conference on Machine Learning and Systems (MLSys 2021). 2021.
Wang C, Wu Q, Huang S, Saied A. Economical Hyperparameter Optimization with Blended Search Strategy. In: The Ninth International Conference on Learning Representations (ICLR 2021). 2021.
Kleiman R, Page D. AUCmu: A Performance Metric for Multi-Class Machine Learning Models. Proceedings of Machine Learning Research. 2019;97:3439–47.
Lundberg SM, Lee S-I. A Unified Approach to Interpreting Model Predictions. Adv Neural Inf Process Syst. 2017;30.
Lewis DD. Representation and learning in information retrieval. Doctor of Philosophy. University of Massachusetts; 1992.
Lewis DD. Feature Selection and Feature Extraction for Text Categorization. In: Speech and Natural Language: Proceedings of a Workshop Held at Harriman, New York. 1992.
Cavnar WB, Trenkle JM. N-gram-based text categorization. Las Vegas: Nevada Univ; 1994.
Damashek M. Gauging similarity with n-Grams: language-independent categorization of text. science. 1995;267:843–8.
Yang Y, Pedersen JO. A Comparative Study on Feature Selection in Text Categorization. In: Proceedings of the Fourteenth International Conference on Machine Learning. San Francisco: Morgan Kaufmann Publishers Inc.; 1997. p. 412–20.
Bird S, Loper E. NLTK: The Natural Language Toolkit. In: Proceedings of the ACL Interactive Poster and Demonstration Sessions. Barcelona: Association for Computational Linguistics; 2004. p. 214–7.
Mikolov T, Chen K, Corrado G, Dean J. Efficient Estimation of Word Representations in Vector Space. In: Proceedings of Workshop at ICLR. 2013.
Mikolov T, Sutskever I, Chen K. Distributed representations of words and phrases and their compositionality. Adv Neural Inf Process Syst. 2013.
Pennington J, Socher R, Manning C. Glove: Global Vectors for Word Representation. In: Proceedings of the 2014 Conference on Empirical Methods in Natural Language Processing (EMNLP). Doha: Association for Computational Linguistics; 2014. p. 1532–43.
Sennrich R, Haddow B, Birch A. Neural Machine Translation of Rare Words with Subword Units. In: Proceedings of the 54th Annual Meeting of the Association for Computational Linguistics (Volume 1: Long Papers). Berlin: Association for Computational Linguistics; 2016. p. 1715–25.
Luong T, Pham H, Manning CD. Effective Approaches to Attention-based Neural Machine Translation. In: Proceedings of the 2015 Conference on Empirical Methods in Natural Language Processing. Lisbon: Association for Computational Linguistics; 2015. p. 1412–21.
Bahdanau D, Cho K, Bengio Y. Neural Machine Translation by Jointly Learning to Align and Translate. In: Proceedings of the 3rd International Conference on Learning Representations. 2015.
LeCun Y, Bengio Y, Hinton G. Deep learning. Nature. 2015;521:436–44.
Peters ME, Neumann M, Iyyer M, Gardner M, Clark C, Lee K, Zettlemoyer L. Deep Contextualized Word Representations. In: Proceedings of the 2018 Conference of the North American Chapter of the Association for Computational Linguistics: Human Language Technologies, Volume 1 (Long Papers). New Orleans: Association for Computational Linguistics; 2018. p. 2227–37.
Howard J, Ruder S. Universal Language Model Fine-tuning for Text Classification. In: Proceedings of the 56th Annual Meeting of the Association for Computational Linguistics (Volume 1: Long Papers). Melbourne: Association for Computational Linguistics; 2018. p. 328–39.
Vaswani A, Shazeer N, Parmar N, Uszkoreit J, Jones L, Gomez AN, et al. Attention is All you Need. In: Guyon I, Luxburg UV, Bengio S, Wallach H, Fergus R, Vishwanathan S, et al., editors. Advances in Neural Information Processing Systems. Curran Associates, Inc.; 2017.
Liu Y, Ott M, Goyal N, Du J, Joshi M, Chen D, Levy O, Lewis M, Zettlemoyer L, Stoyanov V. RoBERTa: a robustly optimized BERT pretraining approach. 2019. arXiv:1907.11692 [cs]. 2019.
Brown T, Mann B, Ryder N, Subbiah M, Kaplan JD, Dhariwal P, et al. Language models are few-shot learners. Adv Neural Inf Process Syst. 2020;33:1877–901.
Lehman E, Hernandez E, Mahajan D, Wulff J, Smith MJ, Ziegler Z, et al. Do We Still Need Clinical Language Models? In: Mortazavi BJ, Sarker T, Beam A, Ho JC, editors. Proceedings of the Conference on Health, Inference, and Learning. PMLR; 22 Jun--24 Jun 2023. p. 578–97.
Teasdale G, Jennett B. Assessment of coma and impaired consciousness A practical scale. Lancet. 1974;2:81–4.
Wei J, Tay Y, Bommasani R, et al. Emergent abilities of large language models. arXiv [cs.CL]. 2022.
Cuvillon P, Nouvellon E, Marret E, Albaladejo P, Fortier L-P, Fabbro-Perray P, Malinovsky J-M, Ripart J. American Society of Anesthesiologists’ physical status system: a multicentre Francophone study to analyse reasons for classification disagreement. Eur J Anaesthesiol. 2011;28:742–7.
Sankar A, Johnson SR, Beattie WS, Tait G, Wijeysundera DN. Reliability of the American Society of Anesthesiologists physical status scale in clinical practice. Br J Anaesth. 2014;113:424–32.
Pedregosa F, Varoquaux G, Gramfort A, et al. Scikit-learn: Machine Learning in Python. J Mach Learn Res. 2011;12:2825–30.
Fan R-E, Chang K-W, Hsieh C-J, Lin C-J. LIBLINEAR: a library for large linear classification. 2008. https://www.jmlr.org/papers/volume9/fan08a/fan08a.pdf. Accessed 5 Jan 2023.
Ng AY. Feature selection, L1 vs. L2 regularization, and rotational invariance. In: Proceedings of the twenty-first international conference on Machine learning. New York: Association for Computing Machinery; 2004. p. 78.
Crammer K, Singer Y. On the Algorithmic Implementation of Multiclass Kernel-based Vector Machines. J Mach Learn Res. 2001;2:265–92.
Ilya Loshchilov FH. Decoupled weight decay regularization. https://doi.org/10.48550/arXiv.1711.05101.
Wolf T, Debut L, Sanh V, Chaumond J, Delangue C, Moi A, et al. Transformers: State-of-the-Art Natural Language Processing. In: Proceedings of the 2020 Conference on Empirical Methods in Natural Language Processing: System Demonstrations. Online: Association for Computational Linguistics; 2020. p. 38–45.
Paszke A, Gross S, Massa F, et al. PyTorch: an imperative style, high-performance deep learning library. In: Proceedings of the 33rd International Conference on Neural Information Processing Systems. Red Hook: Curran Associates Inc.; 2019. p. 8026–37.
Falcon W. Pytorch lightning. GitHub. Note: https://github.com/PyTorchLightning. 2019.
Li L, Jamieson K, Rostamizadeh A, Gonina E, Ben-tzur J, Hardt M, et al. A system for massively parallel hyperparameter tuning. Proceedings of Machine Learning and Systems. 2020;2:230–46.
Acknowledgements
The authors would like to acknowledge: University of Washington Anesthesia Department’s Perioperative & Pain initiatives in Quality Safety Outcome group for assistance on data extraction and initial compute resources for data exploration, University of Washington Department of Medicine for computational environment support, Roland Lai and Robert Fabiano from University of Washington Research IT for creating a digital research environment within the Microsoft Azure Cloud where model development and experiments were performed, and the University of Washington Biomedical Natural Language Processing group for providing early feedback on experimental design and results.
Funding
Computational resources for this project were funded by the Azure Cloud Compute Credits grant program from the University of Washington eScience Institute and Microsoft Azure. The University of Washington Department of Anesthesiology and Pain Medicine Bonica Scholars program provided financial support for this work. Funding sources were not involved in design of the study, collection of data, analysis of data, interpretation of data or in writing the manuscript.
Author information
Authors and Affiliations
Contributions
P.C. conceived and designed this study, assisted in data acquisition, led model development, data analysis, data interpretation, and manuscript writing. C.F. led data acquisition, assisted in data interpretation, and revised the manuscript. A.W. assisted in data acquisition, data interpretation, and manuscript writing and revisions. M.Y. supervised experimental design, data analysis, data interpretation, and manuscript writing and revisions. V.O.R. supervised experimental design, data analysis, data interpretation, and manuscript writing and revisions. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This retrospective study of routinely collected health records data was approved by the University of Washington Institutional Review Board with a waiver of consent. All research methods were carried out in accordance to guidelines and regulations in the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 2: Supplemental Figure 1.
BioClinicalBERT Model Architecture with additional prediction heads for fine-tuning and prediction of modified ASA-PS. Supplemental Figure 2. Attribution of input text features to predicting modified ASA-PS for the BioClinicalBERT model on Note512 task. Model prediction is ASA I, Anesthesiologist assigned case ASA IV-V. Notable findings include the model focusing on pertinent negatives on trauma exam and imaging findings and a normal hematocrit of 33 all of which support predicting a ASA-PS I. The same pertinent negatives as well as a Glasgow Coma Scale (GCS) of 15 are negatively Shapley values for ASA-PS IV-V, which reduce the probability of predicting ASA IV-V. Despite the anesthesiologist’s assignment of ASA IV-V, the text description does not suggest the patient has severe systemic disease with constant threat to life (ASA IV) or is moribund and requires the operation to survive (ASA V). Text examples are de-identified by replacing ages, dates, names, locations, and entities with pseudonyms to achieve data obfuscation while preserving structural similarity to the original passage. Supplemental Figure 3. Attribution of input text features to predicting modified ASA-PS for the BioClinicalBERT model on Note512 task. Model prediction is ASA I, Anesthesiologist assigned case ASA IV-V. Notable findings include the model associating chest tube with ASA IV-V. The model has trouble with consistently attributing the multiple mentions of eyelid laceration with a specific ASA-PS. The model may be inappropriately assigning mention of left pneumothorax to ASAI. This example depicts a challenge for the model in which a relatively minor injury (eyelid laceration) is simultaneously present with a potentially severe injury (pneumothorax), though the severity of the pneumothorax is not mentioned and thus the text predominantly supports ASA I (healthy) or ASA II (mild systemic disease). This kind of mixed illness/injury example coupled with a narrative that does not clearly describe disease severity may be a struggle for the model. Text examples are de-identified by replacing ages, dates, names, locations, and entities with pseudonyms to achieve data obfuscation while preserving structural similarity to the original passage. Supplemental Figure 4. Attribution of input text features to predicting modified ASA-PS for the BioClinicalBERT model on Note512 task. Model prediction is ASA IV-V, Anesthesiologist assigned case ASA I. Notable findings include: young age associated with ASA I and ASA IV-V, but negatively associated with ASA II and III; diagnosis of perforated appendix and procedure of laparoscopic appendectomy negatively associated with ASA I and positively associated with higher ASA-PS; model identifying broad-spectrum antibiotics such as ertapenem to be associated with ASA IV-V, but narrower-spectrum antibiotics such as metronidazole, cefazolin to be heavily associated with ASA I; inpatient medications such as subcutaneous heparin and ondansetron negatively associated with lower ASA-PS and positively associated with higher ASA-PS. Text examples are de identified by replacing ages, dates, names, locations, and entities with pseudonyms to achieve data obfuscation while preserving structural similarity to the original passage. Supplemental Figure 5. Attribution of input text features to predicting modified ASA-PS for the BioClinicalBERT model on Note512 task. Model prediction is ASA IV-V, Anesthesiologist assigned case ASA I. Notable findings include medical conditions and interventions associated with higher ASA-PS such as cardiomyopathy, internal cardiac defibrillator (ICD) generator change, paroxysmal ventricular tachycardia, left ventricular assist device (LVAD), heart failure, possible transplantation, tricuspid valve repair, and patent foramen ovale (PFO) closure; history of chronic cigarette smoking and snoring associated with ASA IV-V. The text description is at least ASA III (severe systemic illness), and can be argued to be ASA IV (severe systemic disease with constant threat to life) if heart failure is progressively worsening. In this example the model appears to make a more appropriate ASA-PS prediction than the anesthesiologist. Text examples are de-identified by replacing ages, dates, names, locations, and entities with pseudonyms to achieve data obfuscation while preserving structural similarity to the original passage. Supplemental Table 1. (A) Matthew's correlation coefficient (MCC) and (B) AUCµ for each model architecture and task on the held-out test set compared to baseline models. MCC is a categorical analog of Pearson’s correlation coefficient. AUCµ is a multiclass generalization of AUROC and U statistic and is more theoretically grounded than macro-average AUROC, but less commonly reported. Standard errors are reported in parenthesis. Supplemental Table 2. (A) Macro-average F1 and (B) class specific F1 for each model architecture and task on the held-out test set compared to baseline models. Standard errors are reported in parenthesis. Supplemental Table 3. (A) Macro-average precision and (B) class-specific precision for each model architecture and task on the held-out test set compared to baseline models. Standard errors are reported in parenthesis. Supplemental Table 4. (A) Macro-average recall and (B) class-specific recall for each model architecture and task on the held-out test set compared to baseline models. Standard errors are reported in parenthesis. Supplemental Table 5. (A) Macro-average AUROC and (B) class-specific AUROC for each model architecture and task on the held-out test set compared to baseline models. Standard errors are reported in parenthesis. Supplemental Table 6. (A) Macro-average AUPRC and (B) class-specific AUPRC for each model architecture and task on the held-out test set compared to baseline models. Standard errors are reported in parenthesis. Supplemental Table 7. P-values for all pairwise comparisons which were not statistically significant. Reported p-values are corrected for multiple hypothesis testing using the Benjamini-Hochberg procedure with α =0.01.
Additional file 3: Supplemental Table 8.
Statistically Significant Pairwise Metric Comparisons.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chung, P., Fong, C.T., Walters, A.M. et al. Prediction of American Society of Anesthesiologists Physical Status Classification from preoperative clinical text narratives using natural language processing. BMC Anesthesiol 23, 296 (2023). https://doi.org/10.1186/s12871-023-02248-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-023-02248-0