Abstract
Background
Labor pain intensity is known to predict persistent postpartum pain, whereas acute postpartum pain may interfere with maternal postpartum physical, mental, and emotional well-being. Nevertheless, there is little research studying the association between labor pain intensity and acute postpartum pain. This study investigated the associations between labor pain intensity and psychological factors with acute postpartum pain.
Methods
We included women with American Society of Anesthesiologists (ASA) physical status II, having ≥ 36 gestational weeks and a singleton pregnancy. We investigated the association between labor pain intensity (primary exposure) and high acute postpartum pain at 0 to 24 h after delivery (Numeric Rating Scale (NRS) ≥ 3 of 10; primary outcome). Pre-delivery questionnaires including Angle Labor Pain Questionnaire (A-LPQ), Pain Catastrophizing Scale (PCS), Fear Avoidance Components Scale (FACS) and State Trait Anxiety Inventory (STAI) were administered. Demographic, pain, obstetric and neonatal characteristics were also collected accordingly.
Results
Of the 880 women studied, 121 (13.8%) had high acute postpartum pain at 0 to 24 h after delivery. A-LPQ total, PCS, FACS and STAI scores were not significantly associated with acute postpartum pain. Greater A-LPQ subscale on birthing pain (adjusted odds ratio (aOR) 1.03, 95% CI 1.01–1.05, p = 0.0008), increased blood loss during delivery (for every 10ml change; aOR 1.01, 95% CI 1.00–1.03, p = 0.0148), presence of shoulder dystocia (aOR 10.06, 95% CI 2.28–44.36, p = 0.0023), and use of pethidine for labor analgesia (aOR 1.74, 95% CI 1.07–2.84, p = 0.0271) were independently associated with high acute postpartum pain. “Sometimes” having nausea during menstruation before current pregnancy (aOR 0.34, 95% CI 0.16–0.72, p = 0.0045) was found to be independently associated with reduced risk of high acute postpartum pain.
Conclusions
Pre-delivery pain factor together with obstetric complications (shoulder dystocia, blood loss during delivery) were independently associated with high acute postpartum pain.
Trial registration
This study was registered on clinicaltrials.gov registry (NCT03167905) on 30/05/2017.
Similar content being viewed by others
Introduction
Despite being a natural process, labor and delivery may turn out to be a source of major trauma to the mother mentally and physically. It is reported that around 60% of nulliparous and 45% of multiparous women may experience severe pain during the first stage of labor [1]. Epidural analgesia is considered the gold standard to relieve labor pain, however some patients may have contraindications to this modality, limited or no access to its use, or opt for analgesia of lesser invasiveness. In addition, pain experiences during labor may differ among individuals and pregnancies, and is influenced by a multitude of physiological and psychosocial factors [1, 2]. Previous studies reported that psychological factors such as greater pain catastrophizing, anxiety sensitivity, and fear avoidance are associated with increased labor pain at early stage, and could lead to longer postpartum recovery [3,4,5]. Additionally, labor pain intensity in vaginal delivery is known to predict persistent postpartum pain [6]. Thus, a comprehensive multidimensional measurement of labor pain is critical for patient care and management to prevent long-term maternal morbidity.
Conventional pain measures (e.g., Visual Analog Scale (VAS), Numeric Rating Scale (NRS)) encompass a unidimensional assessment on pain intensity without considering other pain perception and experience. To address this issue, Angle et al. developed Angle Labor Pain Questionnaire (A-LPQ) that provides a comprehensive multidimensional scale that includes the psychological status, locations, and perception of labor pain that is specific to the context of labor and delivery [7]. A-LPQ is demonstrated to have good internal consistency and test-retest probability for both total and subscale scores, and is positively correlated with NRS and Verbal Rating Scale (VRS) scores [7]. A-LPQ is also linguistically validated, suitable for use among local population in Singapore [8].
Effective identification and management of acute postpartum pain is crucial in determining maternal outcomes and satisfaction. Eisenach et al. reported that severe acute postpartum pain is significantly associated with a 2.5-fold increase in risk of persistent postpartum pain and 3-fold increase in risk of postpartum depression [9]. Studies have also investigated the association between psychological factors (e.g., pain catastrophizing, fear avoidance, anxiety), but their association with acute postpartum pain is less known [3, 10, 11]. Furthermore, our previous data in nulliparous laboring women showed that those who had sub-acute pain after childbirth (SAPC; postpartum pain that lasts between four weeks to three months) was associated with receiving analgesia prior to neuraxial procedure (nitrous oxide/ meperidine), prolonged neuraxial procedure and multiple attempts, maternal anxiety and stress, and obstetric complications (e.g., blood loss during delivery, emergency cesarean delivery); yet their association with acute postpartum pain is unclear [12].
Despite the fact that both labor pain intensity and acute postpartum pain are reported to be associated with persistent postpartum pain, currently the association between these two factors has yet to be established. Exploring and understanding this association may improve peripartum pain management, leading to better patient outcomes. The primary aim of this study was to investigate the association between the labor pain intensity (measured via A-LPQ) and high acute postpartum pain at 0 to 24 h after delivery (measured via NRS ≥ 3 of 10). We would also evaluate the associations of other psychological and pain factors with high acute postpartum pain.
Methods
Patient recruitment
The patients recruited in this study were originally consented to participate in a randomized controlled trial on evaluating the association between labor epidural analgesia and postpartum depression (primary study), with the outcome being the incidence of postpartum depression at 6–10 weeks after delivery. Patient recruitment and follow-up for the primary study has been completed with ongoing data analysis. This study is the secondary analysis by using the trial as a platform to investigate the pain components, of which the pain outcomes were not relevant to the primary objective of the trial. The study was reviewed and approved by SingHealth Centralized Institutional Review Board (Ref no. 2017/2090) on 25/03/2017, with registration on Clinicaltrials.gov (NCT03167905) on 30/05/2017. All patients were recruited from June 2017 to July 2021 with written informed consent obtained from all participants on the primary trial, and patients were informed that the data obtained would be used for further analysis such as this study. This manuscript adheres to the Strengthening the Reporting of Observational studies in Epidemiology (STROBE) guidelines.
The study population included women with American Society of Anesthesiologists (ASA) physical status II [13], having ≥ 36 gestational weeks and a singleton pregnancy. Women who had multiple pregnancies, with non-cephalic fetal presentation, presence of obstetric and uncontrolled medical complications, or underwent elective cesarean delivery were excluded from the study. As this study involved the use of validated English questionnaires, participants who could not understand nor read English were also excluded.
Questionnaires and other collected data
A-LPQ is a 22-item multidimensional questionnaire assessing five subscales on labor pain experience: Uterine contraction pain, fear/ anxiety, back pain/ long haul, birthing pain, and the enormity of pain [7]. The questions are rated from a scale of 0 being none to 10 being worse possible or extremely. Subscale and total scores were calculated accordingly as continuous variable, with higher A-LPQ scores implying a higher labor pain. During the study, patients would receive A-LPQ questionnaire in a private ward setting prior to their labor process, and they were instructed to fill in the questionnaire once they experienced labor pain. Apart from A-LPQ, patients were also administered questionnaires on their psychological characteristics including:
-
(i)
Pain Catastrophizing Scale (PCS): A 13-item scale that measures one’s tendency of developing pain through negative thinking. The instrument comprises three subscales: rumination, magnification, and helplessness and are assessed on a 5-point Likert scale [14]. In this study, apart from studying the total and subscales scores as continuous variables, a cut-off score of 25 would also be used to categorize the patients into high and low pain catastrophizers groups [15]. This cut-off was adopted from a local study that investigated and showed the significant association between pre-delivery pain catastrophizing and increased risk of postpartum depression at 5 to 9 weeks after delivery [15].
-
(ii)
Fear-Avoidance Components Scale (FACS): An instrument to assess one’s fear avoidance associated with painful stimuli [16]. This questionnaire consists of 20 items on a 6-point Likert-like scale from zero (completely disagree) to five (completely agree). Higher FACS scores may indicate greater fear-avoidance of labor pain.
-
(iii)
State Trait Anxiety Inventory (STAI): A 40-item questionnaire that measures state anxiety (current anxiety state) and trait anxiety (susceptibility to perceive anxiety across many situations) [17].
Data on demographic characteristics (age, race, marital status, occupation, etc.) were also collected accordingly. After their delivery, patients were assessed on their pain as part of the routine practice. Data on acute postpartum pain (at rest) at 0 to 24 h were retrieved from electronic record, and was defined as NRS 0 being no pain to 10 being worse pain imaginable. Other data including pain (labor analgesia used), obstetric (mode of delivery, postpartum complications, blood loss, shoulder dystocia) and neonatal (infant weight and length, APGAR scores) characteristics were also recorded.
Statistical analysis
The primary objective was the association between labor pain intensity and acute postpartum pain at 0 to 24 h after delivery. The primary exposure of labor pain intensity (A-LPQ total and subscale scores) would be treated as continuous variable; whereas the primary outcome of acute postpartum pain would be in binary form: “high acute postpartum pain” for those who scored NRS ≥ 3 of 10 at 0 to 24 h after delivery, and “low acute postpartum pain” for those with NRS < 3 of 10. A NRS cut-off of 3 is considered clinically relevant as patients who score 3 and above would require medical intervention to relieve pain as per clinical practice, including our institution [18]. All demographic, pain, obstetric and neonatal characteristics were presented based on their acute postpartum pain status. Categorical and continuous variables were presented as frequency (proportion) and mean (standard deviation (SD)) respectively. Univariate and multivariable logistic regression were used to determine the potential factors associated with high acute postpartum pain. The quantitative associations derived from the logistic regression models were expressed as odds ratio (OR) with corresponding 95% confidence interval (95% CI). Variables with p < 0.15 with less than 10% of missing data in the univariate logistic regression analysis and clinically relevant were chosen for the subsequent multivariable logistic regression analysis [15, 19]. Stepwise variable selection method was used to finalize the final multivariable model. Statistical significance was set at p < 0.05 and all tests were two-tailed. All analyses were performed using SAS version 9.4 software (SAS Institute, Cary, North Carolina, USA).
Results
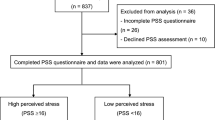
All patients from the primary study (n = 881) were included for this secondary analysis, and only one patient was excluded from the study before the administration of the questionnaires as she changed her mind to participate in the study (Fig. 1). Among the 880 who completed the pre-delivery questionnaires, 121 patients (13.8%) reported having NRS ≥ 3 (“high acute postpartum pain” group) and 759 (86.3%) reported having NRS less than 3 (“low acute postpartum pain”). There is no significant difference in demographic characteristics in both groups except housing status, whereby living in a rented house (OR 1.84, 95% CI 1.04–3.27, p = 0.0368) was significantly associated with high acute postpartum pain in univariate analysis (Table 1).
We examined the association between pre-delivery psychological measures with acute postpartum pain at 0 to 24 h after delivery (Table 2). Looking into the labor pain intensity, women with high acute postpartum pain had a mean (SD) A-LPQ total score of 130.8 (46.4), whereas those with low acute postpartum pain had a mean (SD) A-LPQ total score of 127.2 (50.2). However, no significant association was found between A-LPQ total score and acute postpartum pain (OR 1.00, 95% CI 1.00–1.01, p = 0.4738). Interestingly, A-LPQ subscale of birthing pain showed a significant association with high acute postpartum pain in univariate analysis (OR 1.03, 95% CI 1.01–1.04, p = 0.0022), and no other A-LPQ subscales demonstrated significant difference among the low and high acute postpartum pain groups. A total of 275 women were high catastrophizers (PCS ≥ 25), of whom 30.2% had high acute postpartum pain and 32.3% had low acute postpartum pain. Nevertheless, PCS total and subscale scores, together with FACS and STAI, did not show significant association with acute postpartum pain.
We also investigated patients’ pain, obstetric and neonatal characteristics as shown in Table 3. Being multiparous (OR 0.52, 95% CI 0.30–0.90, p = 0.0202) and “sometimes” having nausea during menstruation before current pregnancy (OR 0.46, 95% CI 0.22–0.97, p = 0.0404) was significantly associated with reduced risk of having high acute postpartum pain in univariate analysis. On the other hand, “always” having nausea during menstruation before current pregnancy (OR 2.80, 95% CI 1.10–7.11, p = 0.0309), use of pethidine for labor analgesia (OR 1.61, 95% CI 1.02–2.56, p = 0.0412), underwent instrumental delivery (OR 1.83, 95% Cl 1.08–3.08, p = 0.0237), longer duration of the second stage of labor (OR 1.004, 95% Cl 1.001–1.01, p = 0.0225), increased blood loss during delivery (OR 1.01, 95% Cl 1.00–1.02, p = 0.0161), increased placental weight (OR 1.002, 95% CI 1.001–1.004, p = 0.0030), increased infant weight (OR 1.001, 95% CI 1.00–1.001, p = 0.0047), increased infant length (OR 1.13, 95% CI 1.02–1.25, p = 0.0235) and presence of shoulder dystocia (OR 6.45, 95% CI 1.59–26.16, p = 0.0090) showed a higher risk of having high acute postpartum pain at 0 to 24 h after delivery.
The univariate factors selected for multivariable analysis (p < 0.15) are presented in Table 4. Independent association factors for acute postpartum pain were identified: greater A-LPQ subscale on birthing pain (adjusted OR (aOR) 1.03, 95% CI 1.01–1.05, p = 0.0008), increased blood loss during delivery (for every 10ml change; aOR 1.01, 95% CI 1.00–1.03, p = 0.0148), presence of shoulder dystocia (aOR 10.06, 95% CI 2.28–44.36, p = 0.0023), and use of pethidine for labor analgesia (aOR 1.74, 95% CI 1.07–2.84, p = 0.0271). Compared with “never” or “rarely having”, “sometimes” having nausea during menstruation before current pregnancy (aOR 0.34, 95% CI 0.16–0.72, p = 0.0045) was found to be independently associated with reduced risk of high acute postpartum pain. The area under the curve (AUC) for the multivariable model was 0.66 (95% CI 0.61–0.71) (Table 4).
Discussion
In this study, we found that labor pain intensity as assessed via A-LPQ total score was not associated with acute postpartum pain. However, greater A-LPQ subscale on birthing pain, increased blood loss during delivery, presence of shoulder dystocia, and use of pethidine for labor analgesia were independently associated with high acute postpartum pain in women who underwent labor process. In addition, “sometimes” having nausea during menstruation before current pregnancy was also found to be independently associated with reduced risk of high acute postpartum pain.
In the primary aim of the study, we found no association between overall labor pain intensity and acute postpartum pain; but looking into specific birthing pain revealed a significant association with high acute postpartum pain at 0 to 24 h after delivery. This may attribute to the timing of A-LPQ administration, where participants were given the choice to complete the A-LPQ at any time point after they experienced labor pain. The use of different labor analgesia and the retrospective completion of A-LPQ may further contribute to a subjective recollection of pain experience emotions and psychological state that could reduce the true representation of labor experience. In addition, other physiological domains (back pain/long haul, uterine contraction) did not show significant association with acute postpartum pain. It is notable that uterine contraction and low back pain are typically present during the first stage of labor, whereas perineal pain usually exists at the later second stage of labor [20]. After the delivery, uterine contraction pain is common within 48 h of delivery, while low back pain only persisted in 13.4% of a study cohort [18]. Thus, it is possible that uterine contraction and low back pain experiences are temporary and may not be a significant source to govern labor pain experience.
The association factors on presence of shoulder dystocia and increased blood loss during delivery may imply presence of perineal trauma or complicated birth experience in those having high acute postpartum pain. As one of the most common sources of postpartum pain, perineal pain typically arises from the stretching and tearing of perineal tissues (perineal trauma) during the period from complete cervical dilation to the delivery [21]. Several risk factors have been shown to be associated with perineal trauma, such as prolonged second stage of labor, instrumental delivery, decreased parity, larger infant birth weight, and shoulder dystocia [22, 23]. Similarly, a greater degree of perineal trauma may lead to increased blood loss during delivery, hence leading to maternal and neonatal complications and poorer postpartum recovery [24]. Our findings are in accordance with previous report that an increased degree of perineal and vaginal trauma as caused by shoulder dystocia could be associated with greater acute postpartum pain scores [22]. This highlights the importance of the early identification of individuals at risk of perineal pain and obstetric complications to allow earlier access to acute postpartum pain management.
We also identified the use of pethidine for labor analgesia as one of the association factors of high acute postpartum pain. Intramuscular pethidine is a commonly used opioid for labor pain relief; yet many studies have reported concerns regarding its use including the various side effects on nausea, vomiting, sedation, and respiratory depression [25, 26]. Studies have also concluded that pethidine is less efficacious in managing labor pain as well as acute postoperative and postpartum pain as compared with epidural and other analgesia [26, 27]. Notably, the use of pethidine during labor was independently associated with SAPC, implying that the use of pethidine during labor plays a similar role in the development of acute postpartum pain, which extends to experiencing SAPC [12, 28].
As part of the primary study assessment for perinatal mental health, we investigated the factors that could be associated with postpartum depression, which included symptoms in premenstrual syndrome (PMS) which has been reported to have positive association with postpartum depression [29]. “Sometimes” having nausea during menstruation before current pregnancy was found to be a protective factor against high acute postpartum pain as compared with those who “never” or “rarely” had nausea. The univariate analysis showed a reverse trend on this factor, such that “always” having nausea during menstruation before current pregnancy contributes to high acute postpartum pain. This may be attributed to other factors not analyzed in this study that may have mediated the association between nausea and acute postpartum pain. A plausible explanation could be the effects brought by hormonal changes, as evidence has shown that nausea during the menstrual cycle and pregnancy are linked to reproductive hormones (e.g., estrogen, progesterone) [30, 31]. Furthermore, having low estrogen levels may exacerbate pain, while a consistent mid-range or high level of estrogen may reduce pain in premenopausal women [32]. Future studies are needed to unravel the exact relationship between the gonadal hormones, nausea, and pain experience.
It was previously reported that pain catastrophizing may predict labor pain intensity and anticipation, leading to a greater risk of acute and persistent perineal postpartum pain and poorer postpartum maternal recovery and adjustment [3, 33, 34]. Similarly, fear-avoidance was shown to be a predictor of intrapartum pelvic girdle pain, genito-pelvic and lumbopelvic pain at 3- and 6-months postpartum [5, 10, 11]. Nonetheless, we did not find any significant association between pre-delivery pain catastrophizing and fear-avoidance with acute postpartum pain in this study. An explanation for our results could be the role of pain-related acceptance within the fear-avoidance model. Pain-related acceptance is the ability and willingness to experience pain, and is found to mediate the associations between pain, pain catastrophizing, and fear-avoidance beliefs [35, 36]. Previous study suggests that a higher level of pain-related acceptance may be protective against the development of fear-full catastrophic beliefs of pain and the maladaptive cognitive-behavioral cycle described in the model [36]. Thus, more research is needed to delineate the role of pain-related acceptance in childbirth and its effects on pain catastrophizing and fear-avoidance beliefs.
This study should consider several limitations. First, this study was conducted in a single maternity institution that offers treatment to predominantly English-speaking Asian population. A systematic review showed that Asians could have lower pain thresholds and different perceptions towards pain as compared with other populations, e.g., non-Hispanic whites, hence limiting the extrapolation of the study findings to other populations [37]. Secondly, other potential factors (religion, income, and socioeconomic status, postpartum analgesia (e.g., paracetamol, mefenamic acid, tramadol)) confounding to labor pain intensity and acute postpartum pain were not investigated in this study [38, 39]. Thirdly, as this was intended to be a secondary analysis, we did not include the sample size calculation in the manuscript. We did perform a post-hoc power calculation as below: Based on available sample size of 880 (121 in high and 759 in low acute postpartum pain groups) study has at least 80% power to reject the null hypothesis of conservative mean difference (Δ) of 14 points in mean A-LPQ scores between high and low acute postpartum pain groups with a common SD σ of 43 based on two-sided independent equal-variance t-test. The targeted A-LPQ score difference of Δ = 14 points is considered to be clinically meaningful and translates to a small effect size of Δ/σ = 14/43 = 0.33 [40]. Finally, the collected data largely rely on patient self-reporting especially the administered questionnaires before the delivery. Given the dynamic and subjective nature of the labor experience, the measurement of labor pain is particularly challenging as the use of self-reporting questionnaires may lead to recall bias or inconsistent results. Additionally, the lack of strict standardization for the exact timing of questionnaire administration may further affect the results as the participants may be in different physical or emotional states at the time of questionnaire response. We acknowledge this limitation, but we allowed women to provide their responses retrospectively for study compliance with reduced participation stress during painful laboring periods.
Conclusion
In summary, pre-delivery pain factor together with obstetric complications (shoulder dystocia, blood loss during delivery) were independently associated with high acute postpartum pain. Future studies are warranted to improve the performance of the model that could help to define the population at risk of high acute postpartum pain. Identification of modifiable pain and psychological factors could also enable healthcare professionals to implement pre-emptive interventions to improve perinatal and postpartum pain management.
Data availability
The datasets generated and/or analyzed during this study are not publicly available due to institutional policy on data confidentiality but are available from the corresponding author on reasonable request.
Abbreviations
- A-LPQ:
-
Angle Labor Pain Questionnaire
- aOR:
-
adjusted odds ratio
- ASA:
-
American Society of Anesthesiologists
- BMI:
-
body mass index
- CI:
-
confidence interval
- FACS:
-
Fear Avoidance Components Scale
- NRS:
-
Numeric Rating Scale
- PCS:
-
Pain Catastrophizing Scale
- PMS:
-
premenstrual syndrome
- SAPC:
-
sub-acute pain after childbirth
- SD:
-
standard deviation
- STROBE:
-
Strengthening the Reporting of Observational Studies in Epidemiology
- VAS:
-
Visual Analog Scale
- VRS:
-
Verbal Rating Scale
References
Melzack R. Labour pain as a model of acute pain. Pain. 1993;53(2):117–20.
Jones L, Othman M, Dowswell T, et al. Pain management for women in labour: an overview of systematic reviews. Cochrane Database Syst Rev. 2012;2012(3):CD009234.
Flink IK, Mroczek MZ, Sullivan MJL, Linton SJ. Pain in childbirth and postpartum recovery: the role of catastrophizing. Eur J Pain Lond Engl. 2009;13(3):312–6.
Curzik D, Jokic-Begic N. Anxiety sensitivity and anxiety as correlates of expected, experienced and recalled labor pain. J Psychosom Obstet Gynecol. 2011;32(4):198–203.
Rashidi Fakari F, Simbar M, Saei Ghare Naz M. The relationship between Fear-Avoidance Beliefs and Pain in pregnant women with pelvic Girdle Pain: a cross-sectional study. Int J Community Based Nurs Midwifery. 2018;6(4):305–13.
Kainu JP, Halmesmäki E, Korttila KT, Sarvela PJ. Persistent pain after cesarean delivery and vaginal delivery: a prospective cohort study. Anesth Analg. 2016;123(6):1535–45.
Angle P, Kurtz-Landy C, Djordjevic J, et al. The Angle Labor Pain Questionnaire: reliability, validity, sensitivity to Change, and responsiveness during early active labor without Pain Relief. Clin J Pain. 2017;33(2):132–41.
Tan CW, Tan HS, Lim LL, Sultana R, Sng BL. Translation and linguistic validation of the chinese version of angle labor pain questionnaire. Bali J Anaesthesiol. 2022;6(1):10–20.
Eisenach JC, Pan PH, Smiley R, Lavand’homme P, Landau R, Houle TT. Severity of acute pain after childbirth, but not type of delivery, predicts persistent pain and postpartum depression. Pain. 2008;140(1):87–94.
Glowacka M, Rosen N, Chorney J, Snelgrove Clarke E, George RB. Prevalence and predictors of genito-pelvic pain in pregnancy and postpartum: the prospective impact of fear avoidance. J Sex Med. 2014;11(12):3021–34.
Fernando M, Nilsson-Wikmar L, Olsson CB. Fear-avoidance beliefs: a predictor for postpartum lumbopelvic pain. Physiother Res Int. 2020;25(4):e1861.
Tan HS, Tan CW, Sultana R, et al. Peripartum factors associated with subacute pain after childbirth. Reg Anesth Pain Med. 2020;45:1017–8.
Committee on Economics, American Society of Anesthesiologists (ASA). ASA Physical Status Classification System. https://www.asahq.org/standards-and-guidelines/statement-on-asa-physical-status-classification-system (2020). Accessed 9 Jun 2023.
Sullivan MJL, Bishop SR, Pivik J. The Pain Catastrophizing Scale: Development and validation. Psychol Assess. 1995;7:524–32.
Zeng Y, Tan CW, Sultana R, et al. Association of Pain catastrophizing with postnatal Depressive States in Nulliparous Parturients: a prospective study. Neuropsychiatr Dis Treat. 2020;16:1853–62.
Neblett R, Mayer TG, Hartzell MM, Williams MJ, Gatchel RJ. The fear-avoidance components scale (FACS): development and psychometric evaluation of a New measure of Pain-related fear avoidance. Pain Pract Off J World Inst Pain. 2016;16(4):435–50.
Spielberger CD. State-trait anxiety inventory. In: Weiner IB, Craighead WE, editors. The Corsini Encyclopedia of psychology. John Wiley & Sons; 2010. pp. 1–1.
Fang X, Huan Y, Tao Y, Incidence, severity, and determinants of uterine contraction pain after vaginal delivery: a prospective observational study. Int J Obstet Anesth., Sandström S, Stephansson A et al. O.
Tan CW, Ozdemir S, Sultana R, Tan C, Tan HS, Sng BL. Factors associated with women’s preferences for labor epidural analgesia in Singapore: a survey approach. Sci Rep. 2022;12(1):10961.
Melzack R, Schaffelberg D. Low-back pain during labor. Am J Obstet Gynecol. 1987;156(4):901–5.
Duration of second stage. Of labor and instrumental delivery as risk factors for severe perineal lacerations: population-based study. BMC Pregnancy Childbirth. 2017;17(1):72.
Leeman L, Fullilove AM, Borders N, Manocchio R, Albers LL, Rogers RG. Postpartum perineal pain in a low episiotomy setting: association with severity of genital trauma, labor care, and birth variables. Birth Berkeley Calif. 2009;36(4):283–8.
Gauthaman N, Walters S, Tribe IA, Goldsmith L, Doumouchtsis SK. Shoulder dystocia and associated manoeuvres as risk factors for perineal trauma. Int Urogynecol J. 2016;27(4):571–7.
Stafford I, Dildy G, Clark S, Belfort M. Peripartum estimated blood loss: Effects of perineal laceration. Am J Obstet Gynecol. 2006;195(6):97.
Ullman R, Smith LA, Burns E, Mori R, Dowswell T. Parenteral opioids for maternal pain relief in labour. Cochrane Database Syst Rev. 2010;(9):CD007396.
Ching Wong SS, Cheung CW. Analgesic efficacy and adverse Effects of Meperidine in Managing Postoperative or Labor Pain: a narrative review of Randomized controlled trials. Pain Physician. 2020;23(2):175–201.
Sheiner E, Shoham-Vardi I, Sheiner EK, et al. A comparison between the effectiveness of epidural analgesia and parenteral pethidine during labor. Arch Gynecol Obstet. 2000;263(3):95–8.
Tan CW, Tan HS, Sultana R, Meaney MJ, Kee MZL, Sng BL. Association of pain, analgesic, psychological, and socioeconomic factors with sub-acute pain after childbirth: a prospective cohort study. J Clin Anesth. 2022;83:110978.
Amiel Castro RT, Pataky EA, Ehlert U. Associations between premenstrual syndrome and postpartum depression: a systematic literature review. Biol psychol. 2019;147:107612.
Matchock RL, Levine ME, Gianaros PJ, Stern RM. Susceptibility to nausea and motion sickness as a function of the Menstrual cycle. Womens Health Issues Off Publ Jacobs Inst Womens Health. 2008;18(4):328.
Tm G. Nausea and vomiting of pregnancy: an obstetric syndrome. Am J Obstet Gynecol. 2002;186(5 Suppl Understanding).
Maurer AJ, Lissounov A, Knezevic I, Candido KD, Knezevic NN. Pain and sex hormones: a review of current understanding. Pain Manag. 2016;6(3):285–96.
Soares ADS, Couceiro TC, de Lima M, Flores LC, Alcoforado FLL, de Filho EMB. Association of pain catastrophizing with the incidence and severity of acute and persistent perineal pain after natural childbirth: longitudinal cohort study. Braz J Anesthesiol. 2013;63(4):317–21.
Ferber SG, Granot M, Zimmer EZ. Catastrophizing labor pain compromises later maternity adjustments. Am J Obstet Gynecol. 2005;192(3):826–31.
LaChapelle DL, Lavoie S, Boudreau A. The meaning and process of pain acceptance. Perceptions of women living with arthritis and fibromyalgia. Pain Res Manag J Can Pain Soc. 2008;13(3):201–10.
Ravn SL, Vang ML, Vaegter HB, Andersen TE. Pain-Related Acceptance as a Mediator in the fear Avoidance Model of Chronic Pain: a preliminary study. Pain Med. 2018;19(9):1764–71.
Kim HJ, Yang GS, Greenspan JD, et al. Racial and ethnic differences in experimental pain sensitivity: systematic review and meta-analysis. Pain. 2017;158(2):194–211.
Defrin R, Eli I, Pud D. Interactions among sex, ethnicity, religion, and gender role expectations of pain. Gend Med. 2011;8(3):172–83.
Antony T, Merghani TH. The influence of demographic and psychosocial factors on the intensity of pain among chronic patients receiving home-based nursing care. Indian J Palliat Care. 2016;22(3):362–5.
Angle PJ, Kurtz Landy C, Djordjevic J, et al. Performance of the angle labor pain questionnaire during initiation of epidural analgesia in early active labor. Anesth Analg. 2016;123(6):1546–53.
Acknowledgements
We would like to thank Miss Agnes Teo (Senior Clinical Research Coordinator) and Miss Sili Tan (Clinical Research Coordinator) for their administrative support in this work.
Funding
CWT is supported by KKH Academic Medicine Research Start-Up Grant (ref no. KKH-AM/2022/01). NYT and SBL are awarded the Academic Medicine – Enhancing Training, Healthcare, Outcomes and Standards (AM-ETHOS) Duke-NUS Medical Student Research Fellowship Award year 2022-23 (ref no. AM-ETHOS01/FY2022/14-A14). SBL is supported by the National Medical Research Council (NRMC) Clinician Scientist award (ref no. CSAINV16may004). The funders had no roles in the study design, data collection and analysis, interpretation of data and the manuscript writing.
Author information
Authors and Affiliations
Contributions
CWT: Conceptualization, funding acquisition, methodology, investigation, formal analysis, writing – original draft, review and editing. NYT: Funding acquisition, methodology, formal analysis, writing – original draft, review and editing. RS: Methodology, formal analysis, writing – review and editing. HST: Conceptualization, methodology, formal analysis, writing – review and editing. BLS: Conceptualization, funding acquisition, methodology, investigation, formal analysis, writing – review and editing, supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
This study received approval by SingHealth Centralized Institutional Review Board (Ref no. 2017/2090) on 25/03/2017, with registration on Clinicaltrials.gov (NCT03167905) on 30/05/2017. Written informed consent was obtained from every patient by the investigators, and that this work was conducted in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
Ban Leong Sng is an editorial board member of BMC Anesthesiology. All other authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tan, C.W., Tan, N.YK., Sultana, R. et al. Investigating the association factors of acute postpartum pain: a cohort study. BMC Anesthesiol 23, 252 (2023). https://doi.org/10.1186/s12871-023-02214-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-023-02214-w