Abstract
Background
Primary viral myocarditis associated with severe acute respiratory syndrome coronavirus 2 (SARS-Cov2) infection is a rare diagnosis.
Case presentation
We report the case of an unvaccinated, healthy patient with cardiogenic shock in the context of a COVID-19-associated myocarditis and therapy with simultaneous veno-arterial extracorporeal membrane oxygenation (VA-ECMO) and percutaneous left ventricular decompression therapy with an Impella. The aim of this review is to provide an overview of therapeutic options for patients with COVID-19-associated myocarditis.
Conclusions
The majority of patients required a combination of two assist devices to achieve sufficient cardiac output until recovery of left ventricular ejection fraction. Due to the rapid onset of this fulminant cardiogenic shock immediate invasive bridging therapy in a specialized center was lifesaving.
Similar content being viewed by others
Background
COVID-19-associated myocarditis in non-mRNA-vaccinated patients without cardiovascular comorbidities has been reported recently [1]. However, the majority of described cases of myocarditis have been associated with mRNA (messenger ribonucleic acid) vaccinations in a younger population [2, 3].
A meta-analysis demonstrated myocardial impairment as measured by troponin I in up to 22% of critically ill COVID-19 (coronavirus disease) patients [4]. A study by Guarracino et al. gives an overview of cardiac involvement in critical COVID-19 patients based on echocardiography results [5]. Nevertheless, primary viral myocarditis associated with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection is a very rare, albeit a life-threatening, disease. While the cause of myocarditis associated with mRNA vaccination remains unclear, it is well known that several viral diseases can cause severe acute myocarditis. This was also observed for SARS-CoV-2. However, cardiac failure primary due to virus-associated myocarditis under COVID-19 infection must be distinguished from other causes of cardiac failure under COVID-19 infection [6].
COVID-19-associated myocarditis has been described several times and repeatedly led to fulminant biventricular failure [7, 8]. Cardiorespiratory assist devices such as veno-arterial extracorporeal membrane oxygenation (VA-ECMO) are frequently used in patients with cardiac failure under COVID-19 infection. These are mostly patients that require the use of cardiac assist devices due to complicating secondary organ failure (e.g., as a result of obstructive shock in pulmonary artery embolism) with pre-existing COVID-19 infection. However, we will report a case of primary COVID-19-associated myocarditis embedded in our literature review.
Due to the diverse causes of acute heart failure in critically ill COVID-19 patients other than myocarditis an appropriate distinction appears to be essential [9]. Unlike other causes, covid-19-associated myocarditis often leads to rapidly progressive cardiogenic shock. Due to severe biventricular heart failure which requires sophisticated use of multiple extracorporeal devices in a specialized center [10]. With our case report and a literature review, we aim to provide insight into the different treatment options and the available literature.
Case presentation
Case report
With the written consent of the patient we summarised the case data from the hospital’s internal documentation. The study and all methods were performed in accordance with the guidelines of the Declaration of Helsinki. We conducted our literature search for case reports and case series according to the PRISMA Guideline. This case report was conducted according to the CARE Guideline.
Clinical manifestation
A 38-year-old female patient (170 cm, 65 kg, body mass index (BMI) 22.5), without pre-existing comorbidities or a family history for cardiac pathologies, presented to the emergency department with cold-like symptoms and relapsing syncope. The unvaccinated patient had been diagnosed with SARS CoV-2 infection 5 days prior to admission.
Laboratory results showed an increased troponin T (140 pg/ml [reference range: < 14 pg/ml]; Fig. 1E) and a transthoracic echocardiography (TTE) revealed a severely impaired cardiac function. Electrocardiography (ECG) showed no signs of acute coronary syndrome. The SARS-CoV-2 RNA E-Gen cycling time was measured with 20.7 on day 2. Due to these clinical, laboratory and sonographic findings the suspected diagnosis of a COVID-19 associated myocarditis was uttered.
Clinical and laboratory findings Figure 1 depicts laboratory results, dosing, measurement results and ECMO settings. Abbreviations: MAP, mean arterial pressure; HR, heart rate; IVS, interventricular septum thickness; NTG, nitroglycerine; LPM, liter per minute; FiO2, inspirational oxygen concentration; TropT, troponin T; CKMB, Creatine kinase myocardial band; CK, Creatin kinase; pip/Taz, piperacillin tazobactam; Hb, Haemoglobin; RBC, red blood count; TC, thrombocyte count; FFP, fresh frozen plasma; PPSB, prothrombin complex concentrate; ASS, aspirin; aXa, anti-Xa activity; aPTT, activated partial thromboplastin time; IL-6, interleukin 6; CRP, C-reactive protein
On admission, the patient was awake, fully orientated, in a reduced general condition, cold sweating, with sinus tachycardia (122 /min) and without oxygenation disorder. TTE showed a severely impaired left ventricular ejection fraction (LVEF ~ 20%), signs of concentric left ventricular hypertrophy (interventricular septum thickness (IVS) 14 mm), a moderately reduced right ventricular function (TDI PW-doppler s-wave < 9.5 cm/s) and circular pericardial effusion (< 8 mm end-diastolic) (Fig. 2A). The patient swiftly deteriorated into cardiogenic shock with lactatemia (6.9 mmol/L) and severely impaired central venous oxygen saturation (ScvO2 36%). Lactatemia quickly disappeared under sufficient circulatory support. Transpulmonary thermodilution revealed a cardiac index < 1 L/min/m2.
Transthoracic echocardiography. A Day 1. Severely impaired cardiac function, left ventricular ejection fraction ~ 20%, interventricular septum thickness (IVS) 14 mm, circular pericardial effusion (< 8 mm end-diastolic). B Day 2. IVS 21 mm, lateral wall thickness 25 mm, pericardial effusion (11 mm). C Day 15. Normalized cardiac function, left ventricular ejection fraction 65%, IVS 8 mm, no pericardial effusion.
Drug and assist device Inotropy support
Inotropic support by means of epinephrine was initiated and awake femoro-femoral veno-arterial ECMO was provided (Cardiohelp; Getinge AB, Göteborg, Sweden) (Fig. 1 A+C). After initiation, aortic valve opening decreased severely. High dose vasopressors were needed to provide sufficient perfusion pressure (Fig. 1A). Due to reduced vigilance and ongoing hemodynamic instability the patient was intubated and ventilated (Fig. 1 A+C). In order to decompress the left ventricle (lv) and allow lv-unloading an Impella CP (Cardiac Power) device (ABIOMED; Danvers, Massachusetts, USA) was implemented (known as ECMELLA). Thereafter, hemodynamics initially stabilised. However, soon after re-admission from the heart catheter laboratory severe bleeding from the Impella cannulation site evolved, necessitating for differential coagulation analysis (thrombelastometry, impedance aggregometry) and differential therapy with colloids, crystalloids, blood products and coagulation factors (Fig. 1 B + D + F). During day 1 after ECMELLA initiation hemodynamic stabilisation could be achieved and vasopressor were reduced (Fig. 1A). Inotropic support with epinephrine was seized after ECMELLA initiation and 12.5 mg of levosimendan, was administered over a 24-hour period. Thereafter, tachycardia was treated with ivabradine 5 mg twice daily (Fig. 1A).
Cardiac function deteriorated with an increase in echocardiographic hypertrophy, most likely attributed to progressive myocardial edema (IVS 21 mm), an increase in pericardial effusion (11 mm) and a decrease in left and right ventricular contractility (Fig. 2B).
Increasing pleural effusions due to heart failure were drained. Pulmonary function remained unaffected with no clinical or radiological signs of SARS-CoV2-associated pneumonia. Figure 1 D depicts volume management, volume balance and urine production.
On day 6, a significant improvement in cardiac function, a decrease in myocardial edema and pericardial effusion was detected (Fig. 1 A+C). After gradual weaning of the extracorporeal support, the VA-ECMO was explanted on day 7 and the Impella on day 8 (Fig. 1 A+C). Based on the pulmonary gas exchange (Horovitz index: 460) the patient was extubated.
The patient recovered quickly, was transferred to the intermediate care unit on day 12 and finally discharged home on day 15. Transthoracic echocardiogram performed on discharge revealed a normalized cardiac function with no sign of persisting heart failure (Fig. 2C). ECG showed discordant terminal negative T-waves in leads V4–6 on day 13 with no change in echocardiographic function.
With appropriate rehabilitation the patient was able to fully reintegrate into her previous life.
Antiviral, antibacterial and immunomodulatory therapy
With stationary admission, the signs of inflammation were unremarkable (C-reactive protein 0.11 mg/dl, Interleukin-6 15.4 pg/ml and Procalcitonin 0.06 ng/ml; see Fig. 1G). The patient received dexamethasone as an immunomodulatory therapy in accordance with current guidelines (Fig. 1G) [11]. In addition, the patient received intravenous immunoglobuline (Pentaglobin, Biotest, Dreieich, Germany) 75 g over a period of 75 hours (Fig. 1G).
It is assumed that direct viral damage is the cause of COVID-19 associated myocarditis [12]. Therapy with SARS-CoV-2 specific monoclonal antibodies (1200 mg casivirimab/1200 mg imdevimab, Roche Pharma AG, Grenzach-Wyhlen, Germany) was initiated on day 2.
Serologic and PCR-testing showed no sign of viral or parasitic infection other than SARS-CoV-2. Microbial testing showed no sign of bacterial infection throughout the complete clinical course.
A myocardial biopsy was not performed because of proven suspected diagnosis, good response of therapy and the increased risk of bleeding under therapeutic anticoagulation.
Discussion and conclusions
Review of the literature
In order to evaluate the case, we conducted a search of the literature available.
We detected 13 cases of COVID-19 myocarditis requiring invasive cardiac organ support (Table 1) [13,14,15,16,17,18,19,20,21,22,23,24].
The literature search was performed (01.05.2022) by searching the MEDLINE, EMBASE, and PubMed databases using the search terms: “Myocarditis” AND “COVID-19” AND/OR “Device” AND/OR “ECMO” AND/OR “Impella” AND/OR “IABP” (intra-aortic balloon pump) were included. In a subsequent study selection we considered all case series and case reports that reported primary COVID-19 myocarditis. Case series and case reports that included myocarditis associated with mRNA vaccination against the novel COVID-19 virus were excluded.
In a secondary analysis only cases reporting severe events requiring cardiac replacement therapy were included.
Inclusion criteria
Mechanical heart support due to presumed severe COVID-19 associated myocarditis.
Exclusion criteria
-
1.
Myocarditis from a cause other than SARS-CoV-2 infection.
-
2.
Solely pharmacologic cardiogenic support
-
3.
Association with SARS-CoV-2 vaccination
The PRISMA flow diagram is shown in Fig. 3.
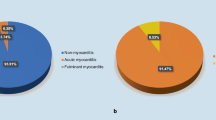
PRISMA flow diagram. Graphical representation of the systematic literature review according to the PRISMA reporting guideline. Abbreviations: SARS-CoV-2, severe acute respiratory syndrome coronavirus 2. Most of the patients in the case studies were male (m 10, f 3) and the median age was 42.6 years (interquartile range 22.5–56 years). Only three patients had reported cardiovascular risk factors diabetes and hypertension in their medical history. One of them already had two previously implanted permeable stents and an ischemic heart disease without chronic heart failure before COVID-19 myocarditis. Pulmonary manifestation in the form of pneumonia was only reported in one patient and acute respiratory distress syndrome (ARDS) was only reported in four patients of 13 cases [13,14,15,16, 21]. One of these four patients with ARDS requiring veno-arterio-venous ECMO (VAV-ECMO) due to ARDS [13].
The time between first symptoms and cardiogenic shock with device implantation varied between 4 and 14 days (median 7 days, interquartile range 4–11.75 days). Only in two patients myocarditis symptoms appeared after a prolonged period with 21 days and 8 weeks.
Echocardiography revealed severely impaired LVEF in all patients. An enlarged end-diastolic diameter was described in 3 patients and pericardial effusion was only described in 2 patients.
All patients required a cardiac assist device due to fulminant impaired left ventricular ejection fraction. 12 of 13 patients received VA-ECMO therapy with additional intra-aortic balloon pump (IABP) therapy in 5 patients and Impella-CP therapy in 3 patients. One of 13 patients only received Impella therapy without VA-ECMO support. Nine patients showed cardiac recovery with extracorporeal device explantation within 1 week (7 patients) or 2 weeks (2 patients) (median 6.5 days, interquartile range 4.5–8.5 days). Two patients also required an external pacemaker due to third degree atrioventricular block.
Four patients died in the course of the disease. Two of those showed full cardiac recovery but died due to fulminant sepsis. Both had a pulmonary manifestation in the form of ARDS. The other two patients died due to multi organ failure. One of them was diagnosed with ischemic heart disease before COVID-19 myocarditis and the other one had a pulmonary manifestation in the form of ARDS.
Discussion
We are reporting a characteristic case of an acute COVID-19-associated myocarditis. Although this form of COVID-19 disease is rare a differentiated consideration of the treatment options seems to be of high importance due to the great potential for recovery [7, 25]. If primary COVID-19 myocarditis is the main disease entity a foudroyant course with dramatic deterioration of cardiac function should be anticipated. From the previous reports, the development of a pronounced myocardial edema with lymphocytic infiltrate is evident [26]. This phenomenon could also be shown sonographically in the case treated at our clinic. This is typically associated with a marked restriction of the left ventricular ejection fraction. As in the case we described this can lead to the need for extracorporeal cardiovascular support [12, 27]. Accordingly, early allocation to a center with an appropriate expertise in cardiac assist device (VA-ECMO, Impella, IABP) should be considered. Thus, timely intervention with one or two ventricular assist devices is possible when conservative pharmacologic therapeutic approaches fail.
In the review we analyzed that total failure of left ventricular function occurred repeatedly. With single VA-ECMO therapy, inadequate aortic valve opening or lack of left ventricular ejection was reported several times, requiring dual cardiac assist devices such as VA-ECMO with Impella or VA-ECMO with IABP for adequate ventricular unloading. In the majority of the reported cases recovery was very quick, so that the inserted devices could be explanted within 1 week and the patients could leave the hospital with an almost completely normal cardiac function in the absence of complicating circumstances.
The occurrence of additional ARDS or bacterial superinfection appears to be of particular importance for the clinical outcome.
Although direct infection of myocytes through expressed ACE-2 receptors is possible, detection of viral RNA from the myocardium is usually not successful [28]. As long as pulmonary involvement is low the majority of patients survive with excellent recovery of left ventricular ejection fraction.
Conclusion
Refractory cardiogenic shock in patients with COVID-19-associated myocarditis is a rare condition and requires rapid invasive therapy in a specialized center.
The initially acute fulminant course of a myocarditis and the LVEF can recover within days. Therefore, rapid invasive bridging therapy may save lives in patients with a SARS-CoV-2 associated myocarditis.
Availability of data and materials
Data cannot be shared publicly. The dataset of the case report are not publicly available due to national data protection laws but are available upon reasonable request from the corresponding author, or via the data protection officer of the University Hospital Frankfurt. Requests regarding the data can thus be sent to the corresponding author: Florian.Raimann@kgu.de or Datenschutz@kgu.de.
Abbreviations
- ACE-2 receptors:
-
Angiotensin Converting Enzyme 2 receptors
- ARDS:
-
Acute respiratory distress syndrome
- AV block:
-
Atrioventricular block
- BMI:
-
Body mass index
- CT:
-
Computed tomography scan
- ECG:
-
Electrocardiography
- IABP:
-
Intra-aortic balloon pump
- Impella CP:
-
Impella Cardiac Power
- LAD:
-
Left anterior descending artery
- LVEF:
-
Left ventricular ejection fraction
- LV:
-
Left ventricle
- MRI:
-
Magnetic Resonance Imaging
- RBBB:
-
Right bundle branch block
- RNA:
-
Ribonucleic acid
- SARS-CoV-2:
-
Severe acute respiratory syndrome coronavirus 2
- TTE:
-
Transthoracic echocardiography
- VAV-ECMO:
-
Veno-arterial-venous extracorporeal membrane oxygenation,
- VA-ECMO:
-
Veno-arterial extracorporeal membrane oxygenation.
References
Agdamag ACC, Edmiston JB, Charpentier V, Chowdhury M, Fraser M, Maharaj VR, et al. Update on COVID-19 myocarditis. Medicina (Kaunas). 2020;56(12):678. https://doi.org/10.3390/medicina56120678.
Kim HW, Jenista ER, Wendell DC, Azevedo CF, Campbell MJ, Darty SN, et al. Patients with acute myocarditis following mRNA COVID-19 vaccination. JAMA Cardiol. 2021;6(10):1196–201. https://doi.org/10.1001/jamacardio.2021.2828.
Oster ME, Shay DK, Su JR, Gee J, Creech CB, Broder KR, et al. Myocarditis cases reported after mRNA-based COVID-19 vaccination in the US from December 2020 to august 2021. JAMA. 2022;327(4):331–40. https://doi.org/10.1001/jama.2021.24110.
Lippi G, Lavie CJ, Sanchis-Gomar F. Cardiac troponin I in patients with coronavirus disease 2019 (COVID-19): evidence from a meta-analysis. Prog Cardiovasc Dis. 2020;63(3):390–1. https://doi.org/10.1016/j.pcad.2020.03.001.
Guarracino F, Vetrugno L, Forfori F, Corradi F, Orso D, Bertini P, et al. Lung, heart, vascular, and diaphragm ultrasound examination of COVID-19 patients: a comprehensive approach. J Cardiothorac Vasc Anesth. 2021;35(6):1866–74. https://doi.org/10.1053/j.jvca.2020.06.013.
Bhatt AS, Adler ED, Albert NM, Anyanwu A, Bhadelia N, Cooper LT, et al. Coronavirus Disease-2019 and heart failure: a scientific statement from the Heart Failure Society of America. J Card Fail. 2022;28(1):93–112. https://doi.org/10.1016/j.cardfail.2021.08.013.
Mele D, Flamigni F, Rapezzi C, Ferrari R. Myocarditis in COVID-19 patients: current problems. Intern Emerg Med. 2021;16(5):1123–9.
Haroun MW, Patel SR, Sims D, Jorde UP, Goldstein DJ, Saeed O. Characteristics and outcomes of COVID-19 patients supported by Venoarterial or Veno-arterial-venous extracorporeal membrane oxygenation. J Cardiothorac Vasc Anesth. 2022;36:2935–41.
Bonow RO, Fonarow GC, O’Gara PT, Yancy CW. Association of Coronavirus Disease 2019 (COVID-19) with myocardial injury and mortality. JAMA Cardiol. 2020;5(7):751.
Venkataraman S, Bhardwaj A, Belford PM, Morris BN, Zhao DX, Vallabhajosyula S. Veno-arterial extracorporeal membrane oxygenation in patients with fulminant myocarditis: a review of contemporary literature. Med. 2022;58(2):215.
Malin JJ, Spinner CD, Janssens U, Welte T, Weber-Carstens S, Schälte G, et al. Key summary of German national treatment guidance for hospitalized COVID-19 patients. Infection. 2022;50(1):93–106. https://doi.org/10.1007/s15010-021-01645-2.
Siripanthong B, Nazarian S, Muser D, Deo R, Santangeli P, Khanji MY, et al. Recognizing COVID-19–related myocarditis: the possible pathophysiology and proposed guideline for diagnosis and management. Heart Rhythm. 2020;17(9):1463–71.
Tavazzi G, Pellegrini C, Maurelli M, Belliato M, Sciutti F, Bottazzi A, et al. Myocardial localization of coronavirus in COVID-19 cardiogenic shock. Eur J Heart Fail. 2020;22(5):911–5. https://doi.org/10.1002/ejhf.1828.
Salamanca J, Díez-Villanueva P, Martínez P, Cecconi A, González de Marcos B, Reyes G, et al. COVID-19 “fulminant myocarditis” successfully treated with temporary mechanical circulatory support. Cardio. Imag. 2020;13(11):2457–9.
Richard I, Robinson B, Dawson A, Aya A, Ali R. An atypical presentation of fulminant myocarditis secondary to COVID-19 infection. Cureus. 2020;12(7):e9179.
Jacobs W, Lammens M, Kerckhofs A, Voets E, Van San E, Van Coillie S, et al. Fatal lymphocytic cardiac damage in coronavirus disease 2019 (COVID-19): autopsy reveals a ferroptosis signature. ESC Heart Fail. 2020;7(6):3772–81.
Albert CL, Carmona-Rubio AE, Weiss AJ, Procop GG, Starling RC, Rodriguez ER. The enemy within: sudden-onset reversible cardiogenic shock with biopsy-proven cardiac myocyte infection by severe acute respiratory syndrome coronavirus 2. Circ. 2020;142(19):1865–70.
Gauchotte G, Venard V, Segondy M, Cadoz C, Esposito-Fava A, Barraud D, et al. SARS-Cov-2 fulminant myocarditis: an autopsy and histopathological case study. Int J Legal Med. 2021;135(2):577–81.
Othenin-Girard A, Regamey J, Lamoth F, Horisberger A, Glampedakis E, Epiney J-B, et al. Multisystem inflammatory syndrome with refractory cardiogenic shock due to acute myocarditis and mononeuritis multiplex after SARS-CoV-2 infection in an adult. Swiss Med Wkly. 2020;45.
Verma AK, Olagoke O, Moreno JD, Rezaee N, Ma P, Liu J, et al. SARS-CoV-2–associated myocarditis: a case of direct myocardial injury. Circ. Heart Fail. 2022;15.
Zeng J-H, Liu Y-X, Yuan J, Wang F-X, Wu W-B, Li J-X, et al. First case of COVID-19 complicated with fulminant myocarditis: a case report and insights. Infect. 2020;48(5):773–7.
Papageorgiou J-M, Almroth H, Törnudd M, van der Wal H, Varelogianni G, Lawesson SS. Fulminant myocarditis in a COVID-19 positive patient treated with mechanical circulatory support–a case report. Eur Heart J-Case Rep. 2021;5.
Marcinkiewicz K, Petryka-Mazurkiewicz J, Nowicki MM, Kuriata J, Dzielińska Z, Demkow M, et al. Acute heart failure in the course of fulminant myocarditis requiring mechanical circulatory support in a healthy young patient after coronavirus disease 2019. Kardio Pols (Pol Heart J). 2021;79(5):583–4.
Kim J, Ganguli S, Yamane D, Pocock E, Mazhari R, Hawkins K. 112: COVID-19-associated myocarditis treated with ECPELLA and glucocorticoid therapy: a CASE series. Crit Care Med. 2022;50(1):39.
Tschöpe C, Ammirati E, Bozkurt B, Caforio ALP, Cooper LT, Felix SB, et al. Myocarditis and inflammatory cardiomyopathy: current evidence and future directions. Nat Rev Cardiol. 2021;18(3):169–93. https://doi.org/10.1038/s41569-020-00435-x.
Fox SE, Falgout L, Vander Heide RS. COVID-19 myocarditis: quantitative analysis of the inflammatory infiltrate and a proposed mechanism. Cardiovasc Pathol. 2021;54:107361.
Irabien-Ortiz Á, Carreras-Mora J, Sionis A, Pàmies J, Montiel J, Tauron M. Fulminant myocarditis due to COVID-19. Rev Esp de Cardiol (English Edition). 2020;73(6):503–4.
Halushka MK, Vander Heide RS. Myocarditis is rare in COVID-19 autopsies: cardiovascular findings across 277 postmortem examinations. Cardiovasc Pathol. 2021;50:107300.
Acknowledgements
Not applicable.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
SN contributed to the manuscript in conceptualization, methodology, data collection, formal data analysis, drafting, visualization and writing the manuscript as well as critical revision. ANF contributed to the manuscript in conceptualization, methodology, data collection, formal data analysis, drafting, visualization and writing the manuscript as well as critical revision. SF helped with manuscript drafting and conducted a critical revision of the manuscript. KZ helped with manuscript drafting and conducted a critical revision of the manuscript. MS contributed to the manuscript in methodology, data collection, formal data analysis, drafting and writing the manuscript as well as critical revision. FJR contributed to the manuscript in conceptualization, methodology, data collection, formal data analysis, drafting, visualization and writing the manuscript as well as critical revision. ANF and SN: Both authors contributed equally to this manuscript and should both be regarded as first author. FJR and MS: Both authors contributed equally to this manuscript and should both be regarded as senior author. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This investigation was approved by the local ethical review board (No. #20–643) of the University Frankfurt. Written consent from the patient, in accordance the guidelines of the Declaration of Helsinki, was obtained before the case report was drafted.
Consent for publication
Written informed consent was obtained from the patient prior to publication.
Competing interests
ANF received speaker fees from P.J. Dahlhausen & Co. GmbH, Colone, Germany and received the Sedana Medical Research Grant 2020. FJR received speaker fees from Helios Germany, university hospital Würzburg and Keller Medical GmbH. FJR received financial support by HemoSonics LLC, pharma-consult Petersohn and Boehringer Ingelheim. KZ has received honoraria for participation in advisory board meetings for Haemonetics and Vifor and received speaker fees from CSL Behring and GE Healthcare. He is the Principal Investigator of the EU-Horizon 2020 project ENVISION (Intelligent plug-and-play digital tool for real-time surveillance of COVID-19 patients and smart decision-making in Intensive Care Units) and Horizon Europe 2021 project COVend (Biomarker and AI-supported FX06 therapy to prevent progression from mild and moderate to severe stages of COVID-19). SN, SF and MS stated that they had no interests which might be perceived as posing a conflict or bias.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Noone, S., Flinspach, A.N., Fichtlscherer, S. et al. Severe COVID-19-associated myocarditis with cardiogenic shock – management with assist devices – a case report & review. BMC Anesthesiol 22, 385 (2022). https://doi.org/10.1186/s12871-022-01890-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-022-01890-4