Abstract
Background
The present study aimed to investigate whether intratracheal dexmedetomidine combined with ropivacaine reduces the severity and incidence of postoperative sore throat after tracheal intubation under general anaesthesia.
Methods
Two hundred patients with American Society of Anaesthesiologists physical status I-II who were subjected to general anaesthesia were randomly divided into four groups, namely, Group D, Group R, Group DR and Group S; these groups received intratracheal dexmedetomidine (1 µg/kg), 0.8% ropivacaine (40 mg), dexmedetomidine (1 µg/kg) combined with 0.8% ropivacaine (40 mg) and normal saline before endotracheal intubation, respectively. The primary outcomes were the incidence and grade of sore throat and hoarseness at 2 h and 24 h after surgery. Moreover, the modified Observer's Assessment of Alertness/Sedation Scale results were recorded at each time point. The secondary outcomes were intraoperative haemodynamic fluctuations, intraoperative anaesthetic drug requirements, and adverse reactions during and after surgery. The patients’ vital signs before induction, before superficial anaesthesia, after superficial anaesthesia, before intubation, after intubation, and 1 min after intubation were recorded. The use of anaesthetic drugs and occurrence of adverse effects were also recorded.
Results
The incidence and severity of sore throat were significantly lower in Group DR than in the other three groups 2 h after the operation, but they were only significantly lower in Group DR than in the control group 24 h after the operation. Moreover, compared with Group S and Group D, Group DR exhibited more stable haemodynamics during intubation. The doses of remifentanil and propofol were significantly lower in Group DR than in the other groups.
Conclusion
The combined use of dexmedetomidine and ropivacaine for surface anaesthesia before intubation significantly reduced the incidence and severity of postoperative sore throat. This treatment also decreased anaesthetic drug requirements and intraoperative haemodynamic fluctuations and caused no adverse effects.
Trial registration
This clinical research was registered at the Chinese Clinical Trial Registry (ChiCTR1900022907, Registration date 30/04/2019).
Similar content being viewed by others
Background
Endotracheal intubation is a common procedure used during spinal surgery under general anaesthesia that provides effective mechanical ventilation. However, endotracheal intubation is the prominent cause of airway mucosal injury, which may result in postoperative sore throat (POST) [1]. Even though POST is a minor adverse event during anaesthesia recovery [2], it causes discomfort for the patient and reduces patient satisfaction with anaesthesia. POST was recently reported to have an incidence of up to 62% after general anaesthesia [3]. The incidence of POST is correlated with age, sex, tracheal tube size, endotracheal tube cuff pressure and other factors [4]. Various methods have been applied to reduce the incidence and severity of POST, including IV administration of lidocaine or dexamethasone [5, 6]; replacement of a double-lumen tube with an endobronchial blocker [7]; and prophylactic use of nebulised ketamine, magnesium, or corticosteroids [8, 9].
Dexmedetomidine is a highly selective adrenergic α-2 receptor agonist that is used for sedation, analgesia, and anxiety inhibition [10]. Ropivacaine is a sodium channel blocker that can affect sensory-motor block. Ropivacaine exhibits good liposolubility and long-acting effects and reaches an acceptable blood concentration via the mucous membrane [11]. Topical ropivacaine anaesthesia can effectively reduce haemodynamic responses during intubation and extubation and reduce the incidence of postoperative throat pain and cough [12]. It was reported that intracheal dexmedetomidine administration 30 min before the end of surgery leads to a smooth extubation and balanced anaesthesia recovery [13]. Several studies have shown that the combination of dexmedetomidine with ropivacaine effectively improves the efficacy of analgesia and extends the duration of analgesia after surgery [14,15,16]. Therefore, we hypothesised that intratracheal dexmedetomidine combined with ropivacaine would decrease the incidence and severity of POST after tracheal intubation.
Methods
This study was a prospective, patient- and investigator-blinded, controlled clinical trial with equal randomization, and it was approved by the Ethics Committee of the Third Affiliated Hospital of Anhui Medical University (No. PJ2019–03–01, approval on 26/03/2019) and registered in the Chinese Clinical Trial Registry (www.chictr.org.cn, ChiCTR1900022907, Registration date 30/04/2019). The study took place at the Third Affiliated Hospital of Anhui Medical University, The First People’s Hospital of Hefei. Each patient provided written informed consent before participation in the study. All the methods were carried out in accordance with the Declaration of Helsinki.
American Society of Anaesthesiologists (ASA) I-II, airway Mallampati class I-II, 20- to 65-year-old patients scheduled for spinal surgery with general anaesthesia were recruited. The exclusion criteria were as follows: ASA ≥ III; body mass index (BMI) ≥ 30 kg·m−2; severe cardiovascular, liver, and kidney dysfunction; uncorrected vision or hearing impairment; difficult airway or history of maxillofacial and neck surgery; chronic use of opioids or sedatives; chronic respiratory disease; recent respiratory tract infection; chronic cough; anaesthesia time more than 4 h; time without extubation more than 1 h; and transfer to the intensive care unit while still intubated.
Subjects were randomised to Group D, Group R, Group DR or Group S with an allocation ratio of 1:1:1:1 according to a computer-generated random number table. The details of the group assignments were sealed in sequentially numbered opaque envelopes. The anaesthesia nurses were given the sealed envelopes and asked to prepare the experimental drugs in syringes according to the group assignments; there was no difference in appearance among the groups. All the patients and anaesthesiologists were blinded to group assignments. An anaesthesiologist administered the drugs to the patient according to the coding number after anaesthetic induction. Another anaesthesiologist recorded intraoperative data and interviewed the patient about sore throat and hoarseness after the surgery.
Electrocardiography (ECG), blood oxygen saturation (SpO2), heart rate (HR), invasive blood pressure (IBP), and respiratory rate (RR) were monitored after the patients were admitted to the operating room. IBP and HR were recorded as the basal blood pressure and basal heart rate after 10 min of resting. The vein channel was established with an 18-gauge indwelling needle. Anaesthesia induction was performed by a senior anaesthesiologist. No subjects received preoperative medication. Oxygen was inhaled via a mask for 3 min, and all the patients received 0.3 μg/kg sufentanil, 1.5–2.5 mg/kg propofol and 0.2 mg/kg cisatracurium besilate via intravenous administration for induction. After the induction of general anaesthesia for 3 min, we used a disposable laryngo-tracheal mucosal atomization device (TUORen Medical Equipment Co., Henan, China; Fig. 1 A) to spray 5 ml of the treatment drug onto the tracheal mucosa and glottis to achieve uniform surface anaesthesia (Fig. 1 B and C). The drug treatments (diluted to 5 ml in each group) used in the four groups were as follows: Group D: dexmedetomidine (1 µg/kg); Group R: 0.8% ropivacaine (40 mg); Group DR: dexmedetomidine (1 µg/kg) combined with 0.8% ropivacaine (40 mg); Group S: saline. Next, endotracheal intubation was performed by two senior anaesthesiologists using a video laryngoscope after 2 min of assisted breathing, and we got successful intubation within 30 s at first time in all patients. The internal diameter of the endotracheal tube used was 6.5 mm for female patients and 7.0 mm for male patients. After successful intubation, mechanical ventilation was resumed, and the end-tidal carbon dioxide pressure was controlled at 35–45 mmHg.
Anaesthesia was maintained by 1% sevoflurane, 3–12 mg·kg−1 h−1 propofol, 0.1–0.3 μg·kg−1 min−1 remifentanil, and intravenous cisatracurium besilate intermittently to maintain a suitable depth of anaesthesia (bispectral index, BIS 40–60). Cuff pressure was maintained at 20–25 mmHg with the continuous monitoring of a pressure transducer [17]. Ondansetron (4 mg) was administered before the end of surgery. When anaesthesia was discontinued and the patients were restored to spontaneous respiration, 1 mg of neostigmine and 0.5 mg of atropine were administered to antagonise the muscle relaxants. The tracheal tube was removed when the patients were conscious, the RR was more than 12 breaths/min, the tidal volume was more than 6 ml/kg, there was swallowing and cough reflex recovery, and the SpO2 was ≥ 95%.
The primary outcome was the incidence and grade of sore throat and hoarseness at 2 h and 24 h after surgery, and the secondary outcome was intraoperative haemodynamic fluctuations, intraoperative anaesthetic drug requirements, and adverse reactions during and after surgery. The anaesthesia nurse recorded patient characteristics and assessed the ASA statuses, BMI values and Wilson risk sum scores of the patients on the day before the surgery. During the operation, the anaesthesiologist recorded the start time of anaesthesia, time of intubation, start time of the operation, end time of the operation, end time of anaesthesia and time of extubation. The patients’ systolic blood pressure (SBP), diastolic blood pressure (DBP), and HR before induction (T0), before superficial anaesthesia (T1), after superficial anaesthesia (T2), before intubation (T3), after intubation (T4), and 1 min after intubation (T5) were recorded. Moreover, the use of anaesthetic drugs (sufentanil, remifentanil, propofol, or cisatracurium besilate) and occurrence of adverse reactions during surgery and after surgery were recorded. The grading of sore throat was as follows [18, 19]: rating of 0, no sore throat; level 1, mild sore throat (complained of sore throat only when asked); level 2, moderate sore throat (self-reported sore throat); and level 3, severe sore throat (pain and discomfort in the pharynx that cause hoarseness or vocal change). Grade of hoarseness [19]: rating of 0, no hoarseness; level 1, mild hoarseness (complained of hoarseness only when asked); level 2, moderate hoarseness (self-reported hoarseness); level 3, severe hoarseness (change in voice was observed). The OAA/S score (0–5) was assessed as follows [20]: rating of 0, no response to squeezing of the trapezius; level 1, no response to mild pushing and shaking; level 2, response only to mild shoulder or head shaking; level 3, response only to loud or repeated name calling; level 4, indifference to normal intonation of names; and level 5, quick response to normal intonation. HR < 50 bpm was considered bradycardia, and an OAA/S score ≤ level 4 was considered an adverse reaction.
All the statistical analyses were performed using SPSS version 20.0. The one-sample Kolmogorov–Smirnov test was used to assess the normality of the quantitative data. Quantitative variables are presented as the mean ± standard deviation (SD) or mean ± standard error of the mean (SEM), and categorical variables are presented as numbers (n/%). Quantitative variables with normally distributed data were analysed using one-way ANOVA followed by the Bonferroni post hoc test. Categorical variables were assessed using χ2 or Fisher's exact test. Repeated measures analyses of variance (ANOVAs) were conducted to analyse differences in SBP, DBP and HR at different time points. Four separate two-way repeated-measures ANOVAs were conducted to identify within-subject effects of different groups. P < 0.05 was considered statistically significant.
In a pilot study, it was found that the incidence of sore throat 2 h after thoracolumbar spinal operation in 10 patients was 50%. In addition, we found that the incidence of sore throat 2 h after thoracolumbar spinal operation in patients who received laryngo-tracheal dexmedetomidine (1 µg/kg) combined with 0.8% ropivacaine (40 mg) spray was 20%. Through a two-sided test with α = 0.05 and β = 0.2, the sample size was 39 in each group, as calculated using G*Power V.3.1.9.4. Considering the 20% rate of patient exclusion, ultimately, a total of 200 ASA status I or II patients were enrolled in this study.
Results
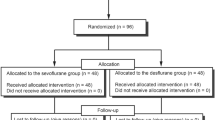
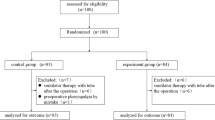
Two hundred twenty-two patients were assessed for eligibility, and of these patients, 22 were excluded; among these patients, 18 patients did not meet the criteria, and 4 refused to participate in the study. Therefore, in total, 200 patients were randomly assigned to Group D, Group R, Group DR and Group S. None of the patients were lost to follow-up (Fig. 2). There were no significant differences in patient characteristics, duration of surgery, duration of anaesthesia, retention time of the tracheal catheter or extubation time between the four groups (Table 1).
CONSORT flow diagram. Abbreviations: Group D: the patients received intratracheal dexmedetomidine (l µg/kg); Group R: the patients received intratracheal 0.8% ropivacaine (40 mg); Group DR: the patients received intratracheal dexmedetomidine (l µg/kg) combined with 0.8% ropivacaine (40 mg); Group S: the patients received intratracheal 5 ml normal saline (all group treatments were diluted to 5 ml)
The incidence and severity of sore throat was significantly lower in Group DR than in Group S, Group D and Group R (16% vs. 44%, P = 0.038, and 40%, P = 0.008 and 34%, P = 0.002, respectively) 2 h after the operation, but it was only significantly lower in Group DR than in Group S 24 h after the operation (10% vs. 28%, P = 0.022). In addition, no differences were detected in the grade of hoarseness (Table 2). Regarding the use of anaesthetic drugs, the doses of remifentanil and propofol were significantly lower in Group DR than in the other groups (P < 0.001). The doses of remifentanil and propofol were significantly lower in Group D than in Group S and Group R (P < 0.05 vs. Group R, P < 0.01 vs. Group S) (Table 3). Compared with Group S and Group D, Group R and Group DR had lower SBP and DBP at T4 and T5 (Fig. 3. A-B), while there was no statistically significant difference at other time points. Compared with Group S and Group R, Group D and Group DR had a lower HR at T3. Moreover, the HR in Group DR was lower than that in the other groups at T4 and T5 (Fig. 3. C). There were no complications associated with the treatment administration in any group during or after surgery.
Haemodynamics data are presented as the mean ± standard deviation (SD) or standard error of the mean (SEM). Time point: before induction (T0), before superficial anaesthesia (T1), after superficial anaesthesia (T2), before intubation (T3), after intubation (T4), and 1 min after intubation (T5). Compared with Group S and Group D, Group R and Group DR had lower SBP and DBP at T4 and T5 (A: SBP: T4*P = 0.001 and T4*P = 0.002, respectively; T4*P < 0.001 and T4*P = 0.001, respectively, SBP: T5*P < 0.001 and T5*P = 0.015, respectively; T5*P < 0.001 and T5*P < 0.001, respectively. B: DBP: T4*P < 0.001 and T4*P < 0.001, respectively; T4*P < 0.001 and T4*P < 0.001, respectively; DBP: T5*P < 0.001 and T5*P < 0.001, respectively; T5*P < 0.001 and T5*P < 0.001, respectively). Compared with Group S and Group R, Group D and Group DR had a lower HR at T3 (C: HR: T3*P < 0.001 and T3*P < 0.001, respectively; T3*P < 0.001 and T3*P < 0.001, respectively). Moreover, the HR in Group DR was lower than that in the other groups at T4 and T5 (C: HR: T4*P < 0.001, T4*P < 0.001, T4*P < 0.001, respectively; T5*P < 0.001, T5*P < 0.001, T5*P < 0.001, respectively)
Discussion
The findings of this study showed that intratracheal administration of dexmedetomidine combined with ropivacaine before intubation significantly reduced the incidence and severity of POST. This treatment also decreased anaesthetic drug requirements and intraoperative haemodynamic fluctuations and caused no adverse effects.
POST is a common complication of tracheal intubation under general anaesthesia. However, the exact cause of POST remains unclear. There are two main sources of sore throat: pain from supraglottic structures, possibly caused by direct laryngoscopy, and pain from infraglottic structures, presumably caused by the endotracheal tube or cuff [21]. Puyoet and colleagues further showed that patients with sore throat release mitochondrial DNA into the upper respiratory system and that their neutrophils are stimulated to release mediators associated with pain in a TLR9- and DNAse-dependent manner [22].
In this study, the incidence of sore throat was significantly lower in Group DR than in the other three groups at 2 h and was lower in Group DR than in the control group at 24 h after surgery. The reason may be that as an adjuvant for local anaesthetics, dexmedetomidine extended the duration of ropivacaine efficacy and improved the efficacy of analgesia after surgery. The possible mechanisms are as follows: dexmedetomidine is a highly selective and specific adrenergic α-2 receptor agonist that can be directly applied to the peripheral nervous system, inhibiting C-fibres and A α-fibres [23]; the most abundant α-2A area is the locus coeruleus, and dexmedetomidine acts on the locus coeruleus area, inhibiting nociceptive neurotransmission through the posterior horn of the spinal cord and terminating the propagation of pain signals, which leads to analgesia [24]; and dexmedetomidine promotes the release of acetylcholine from spinal interneurons, which increases the synthesis and release of nitric oxide and participates in the regulation of analgesia [25]. However, Brummett’s study reported that the increased duration of analgesia caused by combining dexmedetomidine with local anaesthetic results from inhibition of the hyperpolarization-activated cation current (Ih current) not from 2-adrenoceptor agonism [26]. Moreover, we hypothesised that the results might be related to the anti-inflammatory effect of dexmedetomidine. In rodent models, some research has revealed that dexmedetomidine decreases the expression of inflammatory mediators, microglial activation and nerve apoptosis [27,28,29,30]. A recent systematic review and meta-analysis that included 67 studies demonstrated that dexmedetomidine infusion during the perioperative period was associated with lower concentrations of stress hormones (epinephrine, norepinephrine, and cortisol), interleukin (IL)-6, tumour necrosis factor-α, and C-reactive protein after surgery [31]. To some extent, this mechanism is similar to that of dexamethasone in reducing the inflammatory reactions caused by tissue damage [32], but side effects similar to those of dexamethasone, including hyperglycaemia, peptic ulcer and adrenal suppression [33], were not observed in our study.
To eliminate other risk factors for sore throat, we attempted to maintain the cuff pressure at 20–25 cmH2O with a pressure transducer to reduce direct trauma to the tracheal mucosa [34]. We also chose a relatively small tracheal tube, which may provide a better view of the tube through the larynx and decrease the damage associated with tube insertion [35]. Furthermore, intubation and extubation were performed by a senior anaesthesiologist, so no injury was caused by the anaesthetic technique.
We observed that intratracheal dexmedetomidine administration can significantly reduce the use of remifentanil and propofol and decrease intraoperative haemodynamic fluctuations, which was consistent with the results of Le et al. [36]. Intratracheal administration of dexmedetomidine, which is a hydrophilic small molecule, is believed to allow its rapid absorption through the bronchial and alveolar capillary network, facilitating its pharmacological effects, such as reducing sympathetic and laryngeal nerve sensitivity and inhibiting the increase in HR and BP during intubation [13]. In addition, it has been demonstrated that dexmedetomidine can prevent remifentanil-induced hyperalgesia and maintain global haemodynamic stability [37]. However, adverse haemodynamic complications of dexmedetomidine included hypotension, bradycardia and even cardiac arrest [38,39,40]. In the current study, the HR decreased with the application of dexmedetomidine, but only rare episodes of bradycardia requiring atropine were observed. Most likely, because these complications occur more often in elderly patients with cardiac disease or given high dosages of dexmedetomidine intravenously [3], we restricted enrolment to ASA I-II patients, and intratracheal administration resulted in slower effects than intravenous administration. Moreover, sedation scores were measured in the assessments of outcomes. All patients’ OAA/S scores were higher than level 4, and there was no postoperative delay in recovery.
Dexmedetomidine can be administered intravenously, intramuscularly, or intranasally in clinical practice. It has been suggested that intranasal administration is effective, convenient, and well tolerated [41] but has a later onset time [42, 43]. However, the use of dexmedetomidine combined with ropivacaine as an intratracheal spray was first reported.
This study has a number of weaknesses. First, our study was a single-centre investigation of spinal surgery patients; consequently, generalization of these results to other surgical patients should be conducted with caution. Large samples and multicentre clinical verification are essential in the future. Second, all the patients had ASA I-II status and were 20–65 years old, and their basic condition was good. Elderly critical patients were not analysed. Third, the incidence and severity of POST after intravenous dexmedetomidine administration were not assessed in this study. Finally, we merely observed the effect of intratracheal dexmedetomidine combined with ropivacaine within 24 h after surgery, and the long-term outcomes and adverse effects need to be evaluated.
Conclusion
Intratracheal dexmedetomidine (1 µg/kg) combined with 0.8% ropivacaine (40 mg) before intubation can significantly reduce the incidence and severity of POST within 24 h after surgery, decrease anaesthetic drug requirements and intraoperative haemodynamic fluctuations, and cause no adverse effects.
Availability of data and materials
The data used to support the findings of this study are available from the corresponding author upon reasonable request.
Abbreviations
- POST:
-
Postoperative sore throat
- ASA:
-
American Society of Anaesthesiology
- OAA/S:
-
Observer's Assessment of Alertness/Sedation Scale
- BMI:
-
Body mass index
- ECG:
-
Electrocardiography
- SpO2 :
-
Blood oxygen saturation
- HR:
-
Heart rate
- IBP:
-
Invasive blood pressure
- RR:
-
Respiratory rate
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
References
Thomas D, Bejoy R, Zabrin N, Beevi S. Preoperative ketamine nebulization attenuates the incidence and severity of postoperative sore throat: a randomized controlled clinical trial. Saudi J Anaesth. 2018;12(3):440–5.
Lehmann M, Monte K, Barach P, Kindler CH. Postoperative patient complaints: a prospective interview study of 12,276 patients. J Clin Anesth. 2010;22(1):13–21.
Chung CJ, Jeong SY, Jeong JH, Kim SW, Lee KH, Kim JH, Park SY, Choi SR. Comparison of prophylactic effect of topical Alchemilla vulgaris in glycerine versus that of dexamethasone on postoperative sore throat after tracheal intubation using a double-lumen endobronchial tube: a randomized controlled study. Anesth Pain Med (Seoul). 2021;16(2):163–70.
Scuderi PE. Postoperative sore throat: more answers than questions. Anesth Analg. 2010;111(4):831–2.
Yang SS, Wang NN, Postonogova T, Yang GJ, McGillion M, Beique F, Schricker T. Intravenous lidocaine to prevent postoperative airway complications in adults: a systematic review and meta-analysis. Br J Anaesth. 2020;124(3):314–23.
Kuriyama A, Maeda H. Preoperative intravenous dexamethasone prevents tracheal intubation-related sore throat in adult surgical patients: a systematic review and meta-analysis. Canadian Journal of Anesthesia/Journal canadien d’anesthésie. 2019;66(5):562–75.
Knoll H, Ziegeler S, Schreiber JU, Buchinger H, Bialas P, Semyonov K, Graeter T, Mencke T. Airway injuries after one-lung ventilation: a comparison between double-lumen tube and endobronchial blocker: a randomized, prospective, controlled trial. Anesthesiology. 2006;105(3):471–7.
Rajan S, Malayil GJ, Varghese R, Kumar L. Comparison of usefulness of Ketamine and Magnesium Sulfate nebulizations for attenuating postoperative sore throat, hoarseness of voice, and cough. Anesth Essays Res. 2017;11(2):287–93.
Yu J, Ren L, Min S, Yang Y, Lv F. Nebulized pharmacological agents for preventing postoperative sore throat: a systematic review and network meta-analysis. PLoS ONE. 2020;15(8): e0237174.
Paris A, Tonner PH. Dexmedetomidine in anaesthesia. Curr Opin Anaesthesiol. 2005;18(4):412–8.
Eng HC, Ghosh SM, Chin KJ. Practical use of local anesthetics in regional anesthesia. Curr Opin Anaesthesiol. 2014;27(4):382–7.
Fang P, Zong Z, Lu Y, Han X, Liu X. Effect of topical ropivacaine on the response to endotracheal tube during emergence from general anesthesia: a prospective randomized double-blind controlled study. BMC Anesthesiol. 2018;18(1):134.
Wang F, Zhong H, Xie X, Sha W, Li C, Li Z, Huang Z, Chen C. Effect of intratracheal dexmedetomidine administration on recovery from general anaesthesia after gynaecological laparoscopic surgery: a randomised double-blinded study. BMJ Open. 2018;8(4): e020614.
Abdallah FW, Dwyer T, Chan VW, Niazi AU, Ogilvie-Harris DJ, Oldfield S, Patel R, Oh J, Brull R. IV and perineural dexmedetomidine similarly prolong the duration of analgesia after interscalene brachial plexus block: a randomized, three-arm, triple-masked. Placebo-controlled Trial Anesthesiol. 2016;124(3):683–95.
Bangera A, Manasa M, Krishna P. Comparison of effects of ropivacaine with and without dexmedetomidine in axillary brachial plexus block: a prospective randomized double-blinded clinical trial. Saudi J Anaesth. 2016;10(1):38–44.
Rancourt MP, Albert NT, Cote M, Letourneau DR, Bernard PM. Posterior tibial nerve sensory blockade duration prolonged by adding dexmedetomidine to ropivacaine. Anesth Analg. 2012;115(4):958–62.
Rosero EB, Ozayar E, Eslava-Schmalbach J, Minhajuddin A, Joshi GP. Effects of increasing airway pressures on the pressure of the endotracheal tube cuff during pelvic laparoscopic surgery. Anesth Analg. 2018;127(1):120–5.
Stout DM, Bishop MJ, Dwersteg JF, Cullen BF. Correlation of endotracheal tube size with sore throat and hoarseness following general anesthesia. Anesthesiology. 1987;67(3):419–21.
Bagchi D, Mandal MC, Das S, Sahoo T, Basu SR, Sarkar S. Efficacy of intravenous dexamethasone to reduce incidence of postoperative sore throat: a prospective randomized controlled trial. J Anaesthesiol Clin Pharmacol. 2012;28(4):477–80.
Kasuya Y, Govinda R, Rauch S, Mascha EJ, Sessler DI, Turan A. The correlation between bispectral index and observational sedation scale in volunteers sedated with dexmedetomidine and propofol. Anesth Analg. 2009;109(6):1811–5.
Levin PD, Chrysostomos C, Ibarra CA, Ledot S, Naito D, Weissman C, Avidan A. Causes of sore throat after intubation: a prospective observational study of multiple anesthesia variables. Minerva Anestesiol. 2017;83(6):582–9.
Puyo CA, Peruzzi D, Earhart A, Roller E, Karanikolas M, Kollef MH, Krupnick AS, Kreisel D, Ibrahim M, Gelman AE. Endotracheal tube-induced sore throat pain and inflammation is coupled to the release of mitochondrial DNA. Mol Pain. 2017;13:1744806917731696.
Tang C, Xia Z. Dexmedetomidine in perioperative acute pain management: a non-opioid adjuvant analgesic. J Pain Res. 2017;10:1899–904.
Grewal A. Dexmedetomidine: new avenues. J Anaesthesiol Clin Pharmacol. 2011;27(3):297–302.
Liang F, Liu M, Fu X, Zhou X, Chen P, Han F. Dexmedetomidine attenuates neuropathic pain in chronic constriction injury by suppressing NR2B, NF-kappaB, and iNOS activation. Saudi Pharm J. 2017;25(4):649–54.
Brummett CM, Hong EK, Janda AM, Amodeo FS, Lydic R. Perineural dexmedetomidine added to ropivacaine for sciatic nerve block in rats prolongs the duration of analgesia by blocking the hyperpolarization-activated cation current. Anesthesiology. 2011;115(4):836–43.
Yeh CH, Hsieh LP, Lin MC, Wei TS, Lin HC, Chang CC, Hsing CH. Dexmedetomidine reduces lipopolysaccharide induced neuroinflammation, sickness behavior, and anhedonia. PLoS ONE. 2018;13(1): e0191070.
He H, Zhou Y, Zhou Y, Zhuang J, He X, Wang S, Lin W. Dexmedetomidine mitigates microglia-mediated neuroinflammation through upregulation of programmed cell death protein 1 in a Rat Spinal Cord Injury Model. J Neurotrauma. 2018;35(21):2591–603.
Zhang X, Wang J, Qian W, Zhao J, Sun L, Qian Y, Xiao H. Dexmedetomidine inhibits inducible nitric oxide synthase in lipopolysaccharide-stimulated microglia by suppression of extracellular signal-regulated kinase. Neurol Res. 2015;37(3):238–45.
Bell MT, Agoston VA, Freeman KA, Puskas F, Herson PS, Mares J, Fullerton DA, Reece TB. Interruption of spinal cord microglial signaling by alpha-2 agonist dexmedetomidine in a murine model of delayed paraplegia. J Vasc Surg. 2014;59(4):1090–7.
Wang K, Wu M, Xu J, Wu C, Zhang B, Wang G, Ma D. Effects of dexmedetomidine on perioperative stress, inflammation, and immune function: systematic review and meta-analysis. Br J Anaesth. 2019;123(6):777–94.
Zhao X, Cao X, Li Q. Dexamethasone for the prevention of postoperative sore throat: a systematic review and meta-analysis. J Clin Anesth. 2015;27(1):45–50.
Park SH, Han SH, Do SH, Kim JW, Rhee KY, Kim JH. Prophylactic dexamethasone decreases the incidence of sore throat and hoarseness after tracheal extubation with a double-lumen endobronchial tube. Anesth Analg. 2008;107(6):1814–8.
El-Boghdadly K, Bailey CR, Wiles MD. Postoperative sore throat: a systematic review. Anaesthesia. 2016;71(6):706–17.
Koh KF, Hare JD, Calder I. Small tubes revisited. Anaesthesia. 1998;53(1):46–50.
Le Guen M, Liu N, Tounou F, Auge M, Tuil O, Chazot T, Dardelle D, Laloe PA, Bonnet F, Sessler DI, et al. Dexmedetomidine reduces propofol and remifentanil requirements during bispectral index-guided closed-loop anesthesia: a double-blind, placebo-controlled trial. Anesth Analg. 2014;118(5):946–55.
Yuan Y, Sun Z, Chen Y, et al. Prevention of remifentanil induced postoperative hyperalgesia by dexmedetomidine via regulating the trafficking and function of spinal NMDA receptors as well as PKC and CaMKII level In Vivo and In Vitro. PLoS ONE. 2017;12(2): e0171348.
Zhang X, Schmidt U, Wain JC, Bigatello L. Bradycardia leading to asystole during dexmedetomidine infusion in an 18 year-old double-lung transplant recipient. J Clin Anesth. 2010;22(1):45–9.
Peng K, Ji FH, Liu HY, Zhang J, Chen QC, Jiang YH. Effects of perioperative dexmedetomidine on postoperative mortality and morbidity: a systematic review and meta-analysis. Clin Ther. 2019;41(1):138-54.e4.
Li X, Yang J, Nie XL, Zhang Y, Li XY, Li LH, Wang DX, Ma D. Impact of dexmedetomidine on the incidence of delirium in elderly patients after cardiac surgery: a randomized controlled trial. PLoS ONE. 2017;12(2): e0170757.
Yuen VM, Irwin MG, Hui TW, Yuen MK, Lee LH. A double-blind, crossover assessment of the sedative and analgesic effects of intranasal dexmedetomidine. Anesth Analg. 2007;105(2):374–80.
Iirola T, Vilo S, Manner T, Aantaa R, Lahtinen M, Scheinin M, Olkkola KT. Bioavailability of dexmedetomidine after intranasal administration. Eur J Clin Pharmacol. 2011;67(8):825–31.
Li A, Yuen VM, Goulay-Dufay S, Sheng Y, Standing JF, Kwok PCL, Leung MKM, Leung AS, Wong ICK, Irwin MG. Pharmacokinetic and pharmacodynamic study of intranasal and intravenous dexmedetomidine. Br J Anaesth. 2018;120(5):960–8.
Acknowledgements
The authors wish to thank American Journal Experts (AJE) for English language editing.
Funding
This work was supported by Anhui Medical University Foundation for Clinical Science (No. 2021xkj223).
Author information
Authors and Affiliations
Contributions
All the authors contributed to the study conception and design. Data collection and analysis were performed by JYN, RH, NY, YH, HS. JYN and RH contributed equally. JYN, RH, RDN and JMY wrote the paper. All the authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study protocol was approved by the Ethics Committee of the Third Affiliated Hospital of Anhui Medical University (The First People’s Hospital of Hefei) (No. PJ2019–03–01, approval on 26/03/2019) and registered in the Chinese Clinical Trial Registry (www.chictr.org.cn, ChiCTR1900022907, Registration date 30/04/2019). The study took place at the Third Affiliated Hospital of Anhui Medical University (The First People’s Hospital of Hefei). Each patient provided written informed consent before participation in the study. All the methods were carried out in accordance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no conflicts of interest for this work.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Niu, J., Hu, R., Yang, N. et al. Effect of intratracheal dexmedetomidine combined with ropivacaine on postoperative sore throat: a prospective randomised double-blinded controlled trial. BMC Anesthesiol 22, 144 (2022). https://doi.org/10.1186/s12871-022-01694-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-022-01694-6