Abstract
Background
Alveolar recruitment maneuvers (ARMs) is an important part of lung-protective ventilation strategies (LPVSs), but the optimal duration and interval Remain unclear.
Methods
Patients:252 patients who underwent holmium laser lithotripsy surgery and meet inclusion criteria were included and randomized into three groups based on the duration and frequency of ARMs (Regular, one 30 s ARM (RARMs); Improved and intermittent, three 10s ARMs (IARMs); and Control (C), no ARMs).Interventions: Groups R and I received ARMs at 20 cmH2O pressures every 30 min. All patients received the same anesthesia and mechanical ventilation. Measurements:Outcomes included heart rate and mean arterial pressure changes during ARMs and postoperative pulmonary complications (PPCs) within the first 7 postoperative days.
Main results
Incidences of PPCs in groups R(7.1%) and I (5.0%)were slightly lower than those in group C (8.9%).This indicated the potential to reduce lung injury. Heart rate and mean arterial pressure fluctuations during ARMs were significantly higher in groups R and I than in group C (P < 0.01). The rate of blood pressure decrease was significantly higher in group R than in group I (P < 0.01).
Conclusions
IARMs can reduce cycle fluctuations than RARMs in patients Undergoing holmium laser lithotripsy surgery with laryngeal mask general anesthesia. Low tidal volume ventilation and low PEEP combined with ARM did not significantly reduce the incidence of PPCs in healthy lung patients, but tended to reduce lung injury.
Trial registration
The study was registered on the Chinese Clinical Trial Registry.
(ChiCTR2000030815,15/03/2020). This study was approved by the ethics committee of Chengdu Fifth People’s Hospital with approval number(2020–005(Study)-1).
Similar content being viewed by others
Background
With the development of comfort medicine and enhanced recovery after surgery (ERAS), the application of laryngeal mask general anesthesia in ureteral calculi holmium laser lithotripsy has been widely used in China. Usually, the calculi move with respiration, leading to interference with surgery; to reduce the interference, the anesthesiologist often needs to reduce the tidal volume or briefly stop breathing during the operation. Although such respiratory management can effectively reduce the impact of breathing movement during surgery, it may also increase postoperative pulmonary complications (PPCs) such as hypoxemia, atelectasis, and hypercapnia [1, 2]. PPCs cause considerable harm to patients and are the main cause of related complications [3]. Studies have shown that lung protective ventilation strategies (LPVS) can improve postoperative lung function and reduce the incidence of PPCs in patients undergoing surgery,it include low tidal volume ventilation, positive end-expiratory pressure (PEEP), pulmonary re-extension, low inhaled oxygen concentrations, and permissible hypercapnia [4,5,6]. Low tidal volume ventilation can lead to atelectasis [2]; however, collapsed alveoli can be reversed by ARM [7], and appropriate PEEP can maintain open alveoli [8]. There is currently no standard for the duration of ARM, with prior procedures using durations of 10 to 50 s at different pressures [9,10,11,12,13]. Similarly, the use of laryngeal mask anesthesia for lung protection has rarely been studied. We hypothesized that patients undergoing laryngeal mask general anesthesia employed IARMs was safer and would reduce the incidence of PPCs.
Methods
Participants
The study was registered on the Chinese Clinical Trial Registry (ChiCTR2000030815,15/03/20). This study was approved by the ethics committee of Chengdu Fifth People’s Hospital with approval number(2020–005(Study)-1). The subject participant provided written consent. All methods were carried out in accordance with the relevant guidelines and regulations. Risk and benefits were discussed with patients and relatives, and informed consent forms were obtained from all participants prior to enrollment. 252 participants were selected from 653 participants for scheduled transurethral ureteroscopic holmium laser lithotripsy with general Anesthesia from April 2020 to December 2020. Inclusion criteria were age 18 to 65 years with ASA Class I–III, a BMI of 18–30 kg/m2, an expected operation time of 1–3 h, and no contraindications to laryngeal mask placement. Exclusion Criteria were a history of surgery or invasive mechanical ventilation within 2 weeks, respiratory failure or sepsis, heart failure, liver and kidney insufficiency,pregnancy, alcohol abuse, morphine addiction, and mental system disorders.
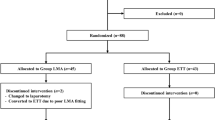
Withdraw Criteria were Laryngeal mask factor (experienced anesthesiologist failed to place 3 times,laryngeal mask leakage caused by various intraoperative factors), Surgery has changed,the experimental operation was not carried out for various reasons. Patients were randomized into three groups based on random numbers: One 30s ARM interval (Regular group, R, n = 84), three 10 s ARM intervals (Improved group, I, n = 84), and no ARM (Control group, C, n = 84). The random numbers were generated by a computer and randomly divided into three groups in a ratio of 1:1:1 into opaque, sealed envelopes, which were then passed by a non-participant investigator to the anesthesiologist, who administered the anesthetic for patients.
People including investigators, patients, staff in the ward and postoperative care units (PACU)) were unaware of the grouping. Postoperatively,all data were obtained by investigators who did not know the groups.
Anesthesia protocol
All patients fasted for 8 to 12 h prior to general anesthesia, and no preoperative medication was administered. Upper extremity intravenous (IV) access was established, and 5–10 ml/kg crystalloids were administered before anesthesia. Echocardiography (ECG), heart rate (HR), non-invasive blood pressure (NIBP), oxygen saturation (SpO2), and EtCO2 were monitored. A radial artery puncture catheter was placed under local anesthesia to monitor intraoperative arterial pressure and harvest samples for blood gas analysis. Anesthesia was induced by administering midazolam (0.03 mg/kg), sufentanil (0.3 ug/kg), propofol (1–1.5 mg/kg), and cisatracurium (0.15 mg/kg).
Laryngeal masks were selected based on weight: size 3 for <50 kg, size 4 for 50–70 kg, and size 5 for >70 kg. Mechanical ventilation was established after the oral insertion of the laryngeal mask. Sevoflurane was inhaled for sedation, and remifentanil maintenance infusion rate of 0.05 ~ 0.1 μg kg − 1 min − 1 for anesthesia maintenance. The Bispect ral index (BIS) value was maintained between 40–60 s, the average arterial pressure (MAP) was maintained between 70–100 mmHg, and HR was maintained between 50–100 beats per minute (bpm).Ringer’s fluid was instilled intravenously (5–10 ml/kg/h) to maintain body fluids. A blood transfusion was considered for blood loss >30% of the total blood volume or a hemoglobin level < 7 g/dl; otherwise, colloidal fluid was used to replace the volume of blood lost. All anesthetics were ceased after the double-J tube was placed. The laryngeal mask was removed when spontaneous breathing and swallowing reflexes were reestablished, normal tidal volume was recovered, and patients responded to verbal commands with their eyes open. The patient was transported back to the recovery ward after complete awakening, and all vital signs were normal.
Mechanical ventilation protocol
A tidal volume of 6 ml/kg, respiratory frequency of 12–18 breaths per minute, inspiration to expiration ratio of 1:2, and PEEP of 5 cmH2O were used in all groups. All patients were administered 50% oxygen at 2 L/min total flow, and respiratory rates were adjusted to maintain PaCO2 at 35–45 mmHg. Groups R and I received ARM every 30 min during surgery, whereas Group C did not receive ARM. ARMs were conducted by adjusting the pressure valve to 20 cmH2O, followed by adjusting the manually controlled breathing valve, and squeezing the air bag to maintain airway pressure. If the cyclic fluctuation during the period of the ARM exceeds 20% before ARM, the test will be terminated.
Outcomes
Primary outcomes included the incidence of PPCs within days, and changes in heart rate and mean arterial pressure during ARM. Secondary outcomes included the duration of postoperative hospital stay, patient satisfaction, and postoperative mortality within 30 days. We also recorded the mechanical ventilation duration and extubation time (from the end of the operation to the time of laryngeal mask removal), and analyzed arterial blood gases and airway peak pressure at T1 (preoperative), T2 (1 h after ventilation), and T3 (postoperative). We monitored postoperative symptoms including cough, expectoration, lung auscultation, fever, and complications associated with laryngeal mask placement.
Sample size and statistical methods
We used the excellent effect test for multiple proportion (provided by the Power Analysis and Sample Size,PASS) to calculate the sample size. According to the literature data, the incidence of PPCs was between 5 and 50% in different types of surgery and 30% relative reduction in PPCs would have clinical significance. However, the incidence of this type of surgery is rarely reported, so, we assume that the incidence of PPCs in the control group was 30 and 15% in the experimental group R and 10% in the experimental group I,and proportion among the groups was 1:1:1. The estimated sample size was 68 per group,which provide 80% power, with two-sided level ofα = 0.05. Taking into account the dropout rate of 20%, so we planned to enroll 252 patients (84 for each group) in all.
We analysed outcome data with SPSS version 26.0software.Statistical significance was set at P < 0.05.Statistical description was provided for baseline data,such as age, sex, BMI, ASA, smoking status, Chest X - ray examination. The quantitative data with a normal distribution were expressed as the mean ± standard deviation, data satisfying the homogeneity of variance were compared using one-way analysis of variance (ANOVA). Fisher’s least significant difference-t test (LSD-t test) was used for post hoc analysis. whereas non-parametric test were used for non- normally distributed. The categorical data were presented as the number (percentage) and used the chi-square test.
The estimated sample size was 84 cases in each group, and the sample size was finally included in the analysis (56, 60, 67). The reasons for some patients not included in the analysis were as follows: Duration of surgery<1 h;Laryngeal mask placement failed and was replaced with endotracheal intubation;Surgery has changed;the experimental operation was not carried out for various reasons;the experimental operation was not carried out for various reasons. If these patients were included in the analysis, it would affect the accuracy of our main outcome. Therefore, these patients were not included and we compared the dropout rates among the three groups, Chi-square test was performed and there was no significant difference (P = 0.156).
Results
Patients characteristics
Two hundred fifty two patients were randomized,following assessment with exclusion criteria, 183 individuals were included in the analysis (Fig. 1). There were no statistically significant differences among the three groups in terms of sex, age, body mass index (BMI), ASA class, history of smoking, and preoperative chest X-ray characteristics (Table 1).
Changes of the circulatory system
The decrease in mean arterial pressure was significantly higher in group R than in group I (6.18 ± 4.10 mmHg vs. 4.47 ± 3.35 mmHg, p < 0.01). Heart rate fluctuations during ARM has no significant difference between groupR and groupI (3.21 ± 2.15 bpm vs 3.07 ± 1.81 bpm, P = 0.114). Fluctuations in heart rate and blood pressure were not obvious in group C because ARMs were not performed, and the changes in heart rate and mean arterial pressure were significantly higher in groups R and I than in group C (P < 0.01). These results are presented in Table 2 and Fig. 2.
Postoperative follow-up and PPCs within the first 7 days after surgery
Thirteen patients developed PPCs (7.1%); four occurred in group R (7.1%), three occurred in group I (5.0%), and six occurred in group C (8.9%). The incidence of PPCs was slightly higher in group C than in groups R and I, but there was no significant difference in PPCs between groups (P > 0.05). There were no statistically significant differences between the groups with respect to complications of laryngeal mask placement and days in hospital. No deaths occurred during hospitalization (Table 3).
Other outcomes
There were no statistically significant differences among the groups with respect to intraoperative fluid administration or loss of body fluids, mechanical ventilation duration, or extubation time (Table S1).
There were no statistically significant differences among the three groups in terms of airway peak pressure or arterial blood gas analyses of PH, Oxygenation index (OI), and PaCO2 at T1, T2, and T3 (Table S2).
Discussion
Although there was no statistically significant improvement in PPCs after ARM, the incidence was lower in the improved group, indicating the potential to reduce lung injury. This result requires further confirmation in clinical studies with larger sample sizes. Nonetheless, the incidence of PPCs was lower than previously reported in the Literatures [14,15,16,17]. This could be attributed to the small sample size, differences in inclusion criteria, with the prior LPVS trials including patients with acute respiratory distress syndrome (ARDS) [18, 19], elderly patients [20], and patients undergoing thoracic surgery [21], versus the healthy lung patients in this study. Additionally, it is possible that the duration of mechanical ventilation was insufficient. In order to reduce retrograde infection, urethral injury, and water poisoning, the operation time for this type of surgery is typically less than 2 h in our hospital, meaning the mechanical ventilation duration is generally not more than 3 h. Fourth, diagnostic criteria may differ.
In this study, intermittent ARM (IARM) had less influence on circulation than continuous ARM. In clinical practice, intermittent ARM may be safer, but certain patients need to more time to open alveoli, including obese patients and patients undergoing thoracoscopic or laparoscopic procedures. Studies have shownthat the laryngeal mask has a protective effect on the lungs [22, 23]. The laryngeal mask is a supraglottic ventilation device that widely used in short operations and emergency airway rescue because it is simple to operate, has small injury risks, Does not require special positioning,and has good patient tolerance [23, 24]. The third-generation double-tube laryngeal mask used in this study includes a gastric tube, which greatly improves its effectiveness and safety. The laryngeal mask was successfully placed after anesthesia in 94% of patients, and there were no statistically significant differences in the number of complications associated with laryngeal mask placement and removal among the three groups.
The application of LPVS in this study included selection of an optimal tidal volume. The tidal volume should be chosen based on comprehensive consideration of patients’ lung function, lung compliance, thoracic compliance, and functional residual gas, and the tidal volume is calculated based on the patient’s predicted body weight (PBW) [25,26,27]. Excessive tidal volume can lead to excessive expansion of the alveoli and cause "volume injury" [26]. Excessive tidal volume also increases airway pressure, the possibility of gas entering the stomach, and air leakage. However,a low tidal volume can lead to insufficient ventilation resulting in atelectasis, ventilation/blood flow disorders, and respiratory acidosis [2]. Consensus among experts recommends a tidal volume of 6–8 mL/kg PBW, which was consistent with the tidal volume used in this study. Additionally, PEEP can maintain the alveoli in the open state during ventilation, and improve oxygen and pulmonary compliance.
Prior research indicates that PEEP ≥5 cmH2O can improve lung compliance, enhance patient oxygenation, and reduce the occurrence of PPCs [8]. Compared with PEEP ≤2 cmH2O, PEEP >12 cmH2O increased the risk of increased peak airway pressure and hemodynamic fluctuations [28]. Experts recommend at least 5 cmH2O, which was used in our study. Alveolar recruitment maneuvers performed at 30-min intraoperative intervals have been shown to improve trans-pulmonary pressure, reopen collapsed alveoli caused by insufficient ventilation, improve oxygen and lung compliance, and reduce the mortality of ARDS patients [29] .If the systolic blood pressure is less than 80 mmHg, or arrhythmia occurs, the ARM should be terminated [18].
There are several limitations associated with this study. It was a single-center study, with a small sample size, and only included healthy lung patients. Additionally, there was no comparison to other ventilation modalities, and strategies for perioperative lung protection should be multifactorial. The effectiveness of LPVS on PPCs was only assessed using one set of variables. A multicenter study with a substantially larger sample size is required to confirm our findings.
Conclusions
In conclusion, Low tidal volume ventilation and low PEEP combined with ARM did not significantly reduce the incidence of PPCs in healthy lung patients, but tended to reduce lung injury. IARMs can reduce cycle fluctuations than RARMs in patients Undergoing holmium laser lithotripsy surgery with laryngeal mask general anesthesia.
Availability of data and materials
The datasets used and analyzed in the current study are available from the corresponding author upon reasonable request.
Abbreviations
- ASA:
-
American Society of Anesthesiologists
- VILI:
-
Ventilation related lung injury
- LPVS:
-
Lung protective ventilation strategy
- PPCs:
-
Postoperative pulmonary complications
- PEEP:
-
Positive end-expiratory pressure
- ARMs:
-
Alveolar recruitment maneuvers
- IARM:
-
Improved alveolar recruitment maneuvers
- RARM:
-
Regular alveolar recruitment maneuvers
- ICU:
-
Intensive Care Unit
- BMI:
-
Body mass index
- PBW:
-
Predicted body weight
- OI:
-
Oxygenation index
- BIS:
-
Bispect ral index
- ECG:
-
Echocardiography
- HR:
-
Heart rate
- NIBP:
-
Non-invasive blood pressure
- SpO2:
-
Oxygen saturation
References
Kronenberg P, Somani B. Advances in Lasers for the Treatment of Stones—a Systematic Review [J]. Curr Urol Rep. 2018;19(6):1–11. https://doi.org/10.1007/s11934-018-0807-y.
Yang D, Grant MC, Stone A, et al. A meta-analysis of intraoperative ventilation strategies to prevent pulmonary complications: is low tidal volume alone sufficient to protect healthy lungs? [J]. Ann Surg. 2016;263(5):881–7. https://doi.org/10.1097/SLA.0000000000001443.
Fernandez-Bustamante A, Frendl G, Sprung J, et al. Postoperative Pulmonary Complications, Early Mortality, and Hospital Stay Following Noncardiothoracic Surgery: A Multicenter Study by the Perioperative Research Network Investigators [J]. JAMA Surgery. 2017;152(2):157–66. https://doi.org/10.1001/JAMASURG.2016.4065.
Young Christopher C, Harris Erica M. Vacchiano Charles,et al. Lung-protective ventilation for the surgical patient: international expert panel-based consensus recommendations.[J]. Br J Anaesth. 2019;123(6). https://doi.org/10.1016/j.bja.2019.08.017.
Spieth PM, Giildner A, Uhlig C, et al. Variable versus conventional lung protective mechanical ventilation during open abdominal surgery: Study protocol for a randomized controlled trial [J]. Trials. 2014;15:155–6. https://doi.org/10.1016/j.bja.2017.11.078.
Emmanuel Futier MD, Constantin J-M, et al. A Trial of Intraoperative Low-Tidal-Volume Ventilation in Abdominal Surgery [J]. New Engl J Med. 2013;369(5):428–37. https://doi.org/10.1097/01.sa.0000453220.13770.84.
Hartland BL, Newell TJ, Damico N. Alveolar recruitment maneuvers under general anesthesia:a systematic review of the literature [J]. Respir Care. 2015;60(4):609–20. https://doi.org/10.4187/respcare.03488.
de Jong MAC, Ladha Karim S, Vidal Melo Marcos F, et al. Differential Effects of Intraoperative Positive End-expiratory Pressure (PEEP) on Respiratory Outcome in Major Abdominal Surgery Versus Craniotomy [J]. Ann Surg. 2016;264(2):362–9. https://doi.org/10.1097/SLA.0000000000001499.
Aya K, Koichi S, Takashi J, Katsuaki T, Takashi M. Changes in corrected carotid flow time induced by recruitment maneuver predict fluid responsiveness in patients undergoing general anesthesia.[J]. J Clin Monitor Comput. 2021;30(7). https://doi.org/10.1007/S10877-021-00736-7.
Ismail S, Ufuk T, Selçuk A, Tarik U, Mefkur B, Ülgen ZS, et al. Effect of the "Recruitment" Maneuver on Respiratory Mechanics in Laparoscopic Sleeve Gastrectomy Surgery.[J]. Obes Surg. 2020;30(7):2684–92. https://doi.org/10.1007/s11695-020-04551-y.
Gulseren Y, Huseyin K, Aysu A, Ziya S. Low-pressure pulmonary recruitment maneuver: equal to or worse than moderate-pressure pulmonary recruitment maneuver in preventing postlaparoscopic shoulder pain? A randomized controlled trial of 72 patients[J]. Wideochir Inne Tech Maloinwazyjne. 2019;15(3):519–25. https://doi.org/10.5114/wiitm.2019.89831.
Bahattin T, Varlık E, Pınar Z. Effects of volume-controlled equal ratio ventilation with recruitment maneuver and positive end-expiratory pressure in laparoscopic sleeve gastrectomy: a prospective, randomized, controlled trial [J]. Turkish journal of medical sciences. 2018;48(4):768–76. https://doi.org/10.3906/sag-1712-12.
Kihlstedt PE, Ellen A. Pulmonary recruitment maneuver reduces pain after laparoscopic bariatric surgery: a randomized controlled clinical trial.[J]. Surg Obes Related Dis. 2018;14(3):386–92. https://doi.org/10.1016/j.soard.2017.11.017.
Prasad M, Sahay S, Varshney R, Jheetay G. Evaluation of risk factors for postoperative pulmonary complications after elective open upper abdominal surgery in chronic obstructive pulmonary diseases patients [J]. J Med Soc. 2019;33(1):47–51. https://doi.org/10.4103/jms.jms_42_18.
Dan H, Shujing Z, Zhangjie Y, Jie C, Hong X. Lung protective ventilation strategy to reduce postoperative pulmonary complications (PPCs) in patients undergoing robot-assisted laparoscopic radical cystectomy for bladder cancer: a randomized double blinded clinical trial.[J]. J Clin Anesth. 2021;71:110156. https://doi.org/10.1016/J.JCLINANE.2020.110156.
Fei LX, Dan J, Lian JY, Yu H, Qiu ZM, Li JJ, et al. Comparison of low and high inspiratory oxygen fraction added to lung-protective ventilation on postoperative pulmonary complications after abdominal surgery: a randomized controlled trial [J]. J Clin Anesth. 2020;67:110009. https://doi.org/10.1016/J.JCLINANE.2020.110009.
Junko N, Shoko N. Minami Toshiaki. Evaluation of alveolar recruitment Maneuver on respiratory resistance during general anesthesia: a prospective observational study.[J]. BMC Anesthesiol. 2020;20(1):01182–9. https://doi.org/10.1186/S12871-020-01182-9.
Kang H. Huqin Yang, Zhaohui Tong. Recruitment manoeuvres for adults with acute respiratory distress syndrome receiving mechanical ventilation: a systematic review and meta-analysis. [J]. J Crit Care. 2019;50:1–10. https://doi.org/10.1016/j.jcrc.2018.10.033.
Sachin S, Friedrich Jan O, Adhikari Neill KJ, Eddy F, Ferguson Niall D, Gordon G, et al. Comparative Effectiveness of Protective Ventilation Strategies for Moderate and Severe Acute Respiratory Distress Syndrome. A Network Meta-Analysis.[J]. Am J Respir Crit Care Med. 2021;203(11):1366–77. https://doi.org/10.1164/rccm.202008-3039OC.
Jo YY, Lee KC, Chang YJ, Jung WS, Park J, Kwak HJ. Effects of an alveolar recruitment maneuver during lung protective ventilation on postoperative pulmonary complications in elderly patients undergoing laparoscopy. Clin Interv Aging. 2020;15:1461–9. https://doi.org/10.2147/CIA.S264987.
Pule L, Xia K, Mengrong M, Jiaqiang Z. Individualized positive end-expiratory pressure (PEEP) during one-lung ventilation for prevention of postoperative pulmonary complications in patients undergoing thoracic surgery: a meta-analysis. Medicine. 2021;100(28):pe26638. https://doi.org/10.1097/MD.0000000000026638.
Hossein JM, Iman H, Farshid R-B, Shekoufeh B, Rouhollah AN, Elahe Y. The role of ventilation mode using a laryngeal mask airway during gynecological laparoscopy on lung mechanics, hemodynamic response and blood gas analysis.[J]. Int J Reprod Biomed (Yazd, Iran). 2016;14(12):775–60 https://pubmed.ncbi.nlm.nih.gov/28066834/.
Kang SH, Park MH. Comparison of early postoperative recovery between laryngeal mask airway and endotracheal tube in laparoscopic cholecystectomy arandomizedtrial [J]. KangandPark Med. 2019;98(25):pe16022. https://doi.org/10.1097/MD.0000000000016022.
Hashem J, Saeed K, Majid V, et al. Better Hemodynamic Profile of Laryngeal Mask Airway Insertion Compared to Laryngoscopy and Tracheal Intubation [J]. Iran Red Crescent Med J. 2015;17(8):e28615. https://doi.org/10.5812/ircmj.28615.
Linares-Perdomo O, East TD, Brower R, Morris AH. Standardizing predicted body weight equations for mechanical ventilation tidal volume settings [J]. Chest. 2015;148(1):73–8. https://doi.org/10.1378/chest.14-2843.
Güldner A, Kiss T, Neto AS, et al. Intraoperative Protective Mechanical Ventilation for Prevention of Postoperative Pulmonary Complications: A Comprehensive Review of the Role of Tidal Volume, Positive End-expiratory Pressure, and Lung Recruitment Maneuvers. [J]. Anesthesiology. 2015;123(3):692–713. https://doi.org/10.1097/ALN.0000000000000754.
Lorenzo B, Paolo P. Intraoperative mechanical ventilation in patients with non-injured lungs: time to talk about tailored protective ventilation? Ann Transl Med. 2016;4(1):17. https://doi.org/10.3978/j.issn.2305-5839.2015.12.30.
Hemmes Sabrine NT, de Abreu Marcelo G, Paolo P, et al. High versus low positive end-expiratory pressure during general anaesthesia for open abdominal surgery (PROVHILO trial):a multicentre randomised controlled trial.[J]. Lancet (London,England). 2014;384(9942). https://doi.org/10.1016/S0140-6736(14)60416-5.
Santos RS, Silva PL, Pelosi P, Rocco PR. Recruitment maneuvers in acute respiratory distress syndrome: the safe way is the best way [J]. World J Crit Care Med. 2015;4(4):278–86 CNKI:SUN:ZBJJ.0.2015-04-003.
Acknowledgements
We thankand all the re- search staff and all patients. We especially would like to thank Dr. Vikas Narang (Chief Operating Officer-Editage) for his valuable advice of the manuscript.
Funding
None.
Author information
Authors and Affiliations
Contributions
FB:Methodology, Supervision,Formal analysis, Writing - original draft. MY: Investigation,Data curation,Resources. HY: Formal analysis, Writing - review & editing. HL: Supervision, Data curation. WU: Conceptualization, Methodology, Writing - review & editing. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the ethics committee of Chengdu Fifth People’s Hospital with approval number(2020–005(Study)-1). After explaining the study protocol to the participants, we obtained written informed consent for study participation from all the participants. All methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Mechanical ventilation duration or extubation time.
Additional file 2: Table S2.
Intraoperative ventilation indexes of patients in three groups.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visithttp://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Bai, FR., Li, Hm., Yi, Ml. et al. The efficacy of different alveolar recruitment maneuvers in holmium laser lithotripsy surgery under general anesthesia using a laryngeal mask. BMC Anesthesiol 22, 134 (2022). https://doi.org/10.1186/s12871-022-01664-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-022-01664-y