Abstract
Background
This study aims to observe the effects of different target controlled plasma sufentanil concentrations on the minimum alveolar concentration (MAC) of sevoflurane for blocking adrenergic response (BAR) in patients undergoing laparoscopic cholecystectomy with carbon dioxide pneumoperitoneum stimulation.
Methods
Eighty-five patients undergoing laparoscopic cholecystectomy, aged 30–65 years, with American Society of Anesthesiologists physical status I-II, were enrolled in this study. All the patients were randomly divided into 5 groups (S0, S1, S2, S3, S4) with different sufentanil plasma target concentration (0.0, 0.1, 0.3, 0.5, 0.7 ng ml− 1). Anesthesia was induced by inhalation of 8% sevoflurane in 100% oxygen, and 0.6 mg kg− 1 of rocuronium was intravenously injected to facilitate the insertion of a laryngeal mask airway. The end-tidal sevoflurane concentration and sufentanil plasma target concentration were adjusted according to respective preset value in each group. The hemodynamic response to pneumoperitoneum stimulus was observed after the end-tidal sevoflurane concentration had been maintained stable at least for 15 min. The MACBAR of sevoflurane was measured by a sequential method. Meanwhile, epinephrine (E) and norepinephrine (NE) concentrations in the blood were also determined before and after pneumoperitoneum stimulus in each group.
Results
When the method of independent paired reversals was used, the MACBAR of sevoflurane in groups S0, S1, S2, S3, S4 was 5.333% (confidence interval [CI] 95%: 5.197–5.469%), 4.533% (95% CI: 4.451–4.616%), 2.861% (95% CI: 2.752–2.981%), 2.233% (95% CI: 2.142–2.324%) and 2.139% (95% CI: 2.057–2.219%), respectively. Meanwhile, when the isotonic regression analysis was used, the MACBAR of sevoflurane in groups S0, S1, S2, S3, S4 was 5.329% (95% CI: 5.321–5.343%), 4.557% (95% CI: 4.552–4.568%), 2.900% (95% CI: 2.894–2.911%), 2.216% (95% CI: 2.173–2.223%) and 2.171% (95% CI: 2.165–2.183%), respectively. The MACBAR was not significantly different between groups S3 and S4 when using 0.5 and 0.7 ng ml− 1 of sufentanil plasma target concentrations. No significant difference was found in the change of E or NE concentration between before and after pneumoperitoneum stimulation in each group.
Conclusions
The MACBAR of sevoflurane can be decreased with increasing sufentanil plasma target concentrations. A ceiling effect of the decrease occurred at a sufentanil plasma target concentration of 0.5 ng ml− 1. When the sympathetic adrenergic response was inhibited in half of the patients to pneumoperitoneum stimulation in each group, the changes of E and NE concentrations showed no significant differences.
Trial registration
The study was registered at http://www.chictr.org.cn (ChiCTR1800015819, 23, April, 2018).
Similar content being viewed by others
Background
With the development of minimally invasive techniques, laparoscopic surgery under inhalation anaesthesia has become increasing popular in general surgery [1,2,3]. However, inhalation anaesthetic used alone to provide all the necessary components of general anesthesia under laparoscopic surgery may increase the risk of cardiovascular inhibition and inhaled anaesthetic toxicity [4,5,6]. Many agents have been used to decrease the minimal alveolar concentration (MAC) of inhalation anaesthetics [7, 8]. Sufentanil, as an adjuvant, offers numerous advantages, including a reduced incidence of postoperative nausea and vomiting compared with the fentanyl [9], reduced opioid-induced hyperalgesia compared with the remifentanil [10], maintenance of stable hemodynamics, excellent analgesic effect. The MAC of sevoflurane for blocking the adrenergic response (BAR) at different sufentanil plasma target concentrations under laparoscopic pneumoperitoneum stimulus has not been reported. Therefore, our primary aim of this study is to observe the MACBAR of sevoflurane combined with different sufentanil plasma target concentrations in patients under carbon dioxide pneumoperitoneum stimulation. A secondary aim is to explore the concentrations of epinephrine and norepinephrine in the blood when the adrenergic response was inhibited in half of the patients.
Methods
Study design
The study was approved by the Ethics Committee of Affiliated Hospital of North Sichuan Medical College, Nanchong, China (Approved No. 2017/043). Written informed consents were obtained from all participants. All experiment procedures (blood collections and arterial catheterization) and data collection were conducted with prior informed consents. This study adhered to the applicable CONSORT guidelines and was registered with the Chinese Clinical Trials Registry at http://www.chictr.org.cn (ChiCTR1800015819, principal investigator: Yanxia Guo, date of registration: April 23, 2018).
The research was conducted between May 2018 and March 2019. Eighty five American Society of Anesthesiologists (ASA) physical status I-II, patients aged between 30 and 65 years, were randomly assigned to five groups (S0, S1, S2, S3, S4) according to a computer generated randomization. Patients in the five groups were anaesthetized by mask inhalation of sevoflurane and intravenous infusion of sufentanil with different plasma target concentrations: 0.0, 0.1, 0.3, 0.5, 0.7 ng ml− 1. Exclusion criteria included that: patients with a history of cardiovascular, lung, kidney or brain disease; long-term drug or alcohol abuse; recent take drugs known to affect the sympathetic adrenergic and cardiovascular systems; and body mass index (BMI) ≧30 kg m− 2. Withdrawal criteria included patients with mean arterial pressure (MAP) < 50 mmHg or heart rate (HR) < 50 bpm at any time during experimental observation; failing to achieve creation of the carbon dioxide pneumoperitoneum on the first attempt; or asking for adjustment of the pneumoperitoneal pressure above or below the preset value.
Anaesthesia administration
Induction
All patients were fasted at least for 8 h before surgery and without any preoperative medication. Before induction of anaesthesia, patient’s MAP, HR, electrocardiogram, and oxygen saturation were monitored as per routine with a PM-9000 express monitor (Mindray Medical International Limited, Shenzhen, China). Simultaneously, a peripheral intravenous catheter was inserted for infusion of Ringer’s solution at a rate of 10 ml kg− 1 h− 1. An arterial catheter was inserted into the left radial artery for monitoring patient’s arterial blood pressure and collecting blood samples. Anaesthesia was induced by inhalation of 8% sevoflurane with 100% oxygen until patients lost their consciousness, then 0.6 mg kg− 1 of rocuronium was intravenously injected to facilitate the insertion of laryngeal mask airway (Tuoren medical equipment group co. LTD, Henan, China) insertion. Then mechanical ventilation was begun using 100% oxygen with a tidal volume of 6 to 8 ml kg− 1. A normal end tidal carbon dioxide (CO2) tension (35 to 45 mmHg) was obtained by adjusting the respiratory frequency at 12 to 16 breaths min− 1. The end-tidal sevoflurane concentration and CO2 partial pressure were monitored continuously using the above-mentioned monitor. Depth of anaesthesia was monitored by the bispectral index (BIS) (Canwell Medical International Limited, Zejiang, China) which was placed before induction.
Measurement of MACBAR
After laryngeal mask airway insertion, sufentanil was administered by target-controlled infusion with Bovil pharmacokinetic model using a micro pump (TCI-I, ver 4.0, Guangxi VERYARK Technology Co., Ltd), and the plasma target concentration of sufentanil was 0.0, 0.1, 0.3, 0.5, 0.7 ng ml− 1 in groups S0, S1, S2, S3, S4, respectively. Simultaneously, the inhaled sevoflurane concentration was adjusted to obtain a stable preset end-tidal value according to our pilot study. In order to avoid a potential risk of intraoperative awareness, a higher initial end-tidal sevoflurane concentration was tested in the pilot study. The first patient in groups S0, S1, S2, S3 and S4 received a start end-tidal sevoflurane preset concentration of 5.0, 4.6, 3.0, 2.3 and 2.0% which was determined to be close to the MACBAR, respectively. An up-and-down sequential-allocation method was applied to determine the MACBAR of sevoflurane in each group as described in our previous studies [11, 12].
The CO2 pneumoperitoneum was created when the preset end-tidal sevoflurane concentration had been maintained stable at least 15 min. The creation of pneumoperitoneum was initiated using a Veress needle with the CO2 pressure set to 13 mmHg at umbilicus and the insufflation flow rate was set at 3 L/min. After the CO2 pneumoperitoneum had been created a 10-mm trocar replaced the Veress needle. Another 10-mm trocar and a 5-mm trocar were installed through a subxiphoid port and a port in the right subcostal area of the midclavicular line, respectively. HR and MAP were determined before induction, 3 and 1 min before CO2 pneumoperitoneum, and 1 and 3 min after three trocars were installed. Presence or absence of a sympathetic adrenergic response during the creation of the CO2 pneumoperitoneum was indicated by HR or MAP was recorded. Both the mean value of MAP and the mean value of HR measured 3 and 1 min before pneumoperitoneum stimulation were defined as the pre-pneumoperitoneum values, and the mean value of HR and the mean value of MAP measured 1 and 3 min after the trocars had been installed were defined as the post-pneumoperitoneum values. If the response was positive (an increase of patient’s HR or MAP > 20% of its pre-pneumoperitoneum value), the subsequent tested patient’s end-tidal sevoflurane concentration would be increased by 0.2%. If the response was absent i.e. HR and MAP change of < 20% of its pre-pneumoperitoneum value, the subsequent tested patient’s end-tidal sevoflurane concentration would be decreased by 0.2%. Patients with bradycardia (HR < 50 bpm) or hypotension (MAP < 50 mmHg) at any time during experimental observation were administered vascular active drugs such as atropine, ephedrine, and withdrawn from the study, a same tested end-tidal sevoflurane concentration was repeated in the following case. The study was continued until six crossing points of a negative versus positive response in the pre-and the next patient had occurred. The investigator responsible for recording the response of the patients to CO2 pneumoperitoneum was blinded to the plasma target controlled sufentanil concentrations and end-tidal sevoflurane concentration used in all the study patients. The MACBAR of sevoflurane in each group was calculated as the mean value of the end-tidal sevoflurane concentrations corresponding to the six crossing points.
After the above test was completed, the target controlled infusion of sufentanil was stopped in each group. The patients in group S0 received an i.v. bolus of 0.3 μg kg− 1 sufentanil. Furthermore, the inspired concentration of sevoflurane was adjusted to maintain the end-tidal concentrations at 1.4–1.7 MAC for maintaining the BIS value between 40 and 60. MAP was maintained between 60 and 85 mmHg intraoperatively. If the MAP increased by more than 20% compared with its preoperative value, a bolus of 10 μg sufentanil was administered. After surgery and removal of the laryngeal mask airway, patients were transported to the post- anaesthesia care unit (PACU). In the PACU, all patients were asked about whether there was any intraoperative awareness or not.
Analysis of blood samples
Arterial blood samples were collected 3 min before and after CO2 pneumoperitoneum and stored in sodium-heparin-containing tubes. Soon after, the plasma was separated and kept frozen at − 70 °C until analysis. The method used to measure the concentrations of E and NE in the current investigation have been described previously [12].
Statistical analysis
Statistical analysis was performed using SPSS 23.0 software. The MACBAR was estimated from the up-and-down sequences using the method of independent paired reversals, which enabled MACBAR with 95% CIs to be derived [13]. The sequences were also subjected to isotonic regression analyses. To compare the MACBAR from different groups more precisely, the 83% CIs were estimated using the isotonic regression analysis. The delta HR, delta MAP, delta E, delta NE value were calculated as the differences between their average values measured 1 and 3 min before and after CO2 pneumoperitoneum. The data are presented as mean (SDs or 95%CI). The preoperative data, including gender and ASA class were compared with X2 test. The preoperative data (age, BMI), the intraoperative data, the postoperative data, the MACBARS, the concentrations of E and NE, delta E, delta NE, MAP, delta MAP, HR, and delta HR were compared among the 5 groups using one-way analysis of variance (ANOVA). P value < 0.05 was considered as statistical significance.
Results
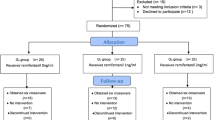
A total of 85 patients were recruited in this study. One case in group S0 and one case in group S3 both with MAP < 50 mmHg were removed from the study. Two cases with HR < 50 bpm in group S4 were also removed from the study. Ultimately, to obtain six crossing points, 14, 14, 18, 20 and 15 patients were used in groups S0-S4, respectively (Fig. 1), so that 81 patients completed the study. No significant differences were found in the patients’ preoperative data, operation time and rocuronium consumed among the 5 groups (Table 1). No intraoperative awareness was reported in the postoperative follow up.
Dixon up-and-down plots for each group. The plasma target concentration of sufentanil in groups S0, S1, S2, S3 and S4 was 0.0, 0.1, 0.3, 0.5 and 0.7 ng ml− 1, respectively. The empty (solid) circle represents the negative (positive) reaction to hemodynamics parameters, and the triangle indicates the intersection of negative and positive reactions. The ninth patient was given the same concentration of sevoflurane both in group S2 and group S3. To get six crossovers, 14, 14, 18, 20 and 15 patients were needed in groups S0-S4, respectively
The estimates of MACBAR of sevoflurane by the method of independent paired reversals and isotonic regression using the different plasma target concentration of sufentanil in groups S0-S4 are shown in Table 2. The 83% CIs were overlapped in group S3 and S4 using the isotonic regression analysis. For both methods, the MACBAR was not significantly different between group S3 and group S4 when using 0.5 and 0.7 ng ml− 1 of sufentanil plasma target concentrations. The HR and delta HR were similar among groups S2, S3, and S4, but significantly lower than groups S0 and S1 (P < 0.05, Table 3). No significant differences were found in the MAP, delta MAP, epinephrine and norepinephrine concentration, delta epinephrine and norepinephrine concentration among the 5 groups (Table 3). The total administered dose of sufentanil in both group S3 and group S4 was higher than in groups S0, S1, S2 (P < 0.05, Table 1). The spontaneous breathing recovery time, eye opening time and extubation time in group S4 was longer than those in the other 4 groups (P < 0.05, Table 1).
Discussion
The results of this study indicate that the reduction of the MACBAR of sevoflurane by sufentanil is dose-dependent. The overlapped 83% CIs in group S3 and S4 using the isotonic regression analysis indicate the MACBAR had no significant difference when using 0.5 and 0.7 ng ml− 1 of sufentanil plasma target concentrations. This suggests that a ceiling effect of the decrease of MACBAR of sevoflurane occurred when the sufentanil plasma target concentration increased to > 0.5 ng ml− 1 (Table 2). This ceiling effect of sufentanil is similar to the result measured by Brunner and colleagues [14] at the same plasma target concentration when they evaluated the reduction of isoflurane’s MAC by sufentanil in response to skin incision. Sufentanil is a μ receptor agonist, which can be saturated when its plasma target concentration is beyond a certain level [15]. We speculate that a similar ceiling effect will occur under a similar plasma target concentration of sufentanil no matter what kind of surgery or stimulus is selected. The ceiling plasma concentration of sufentanil (0.18 ng ml− 1) in Shun-Huang and colleague’s study [16] is significantly lower than that of our experiment result. We believe that is reasonably explained by the concomitant administration of 60% nitrous oxide [17, 18]. Several studies show that nitrous oxide can combine with the μ receptor and decrease the available binding sites of sufentanil in humans [19,20,21,22,23].
In this study, the MACBAR of sevoflurane (5.333%) under laparoscopic pneumoperitoneum stimulation is higher than that measured by Katoh and his colleagues (4.15%) under skin incision [24]. It suggests that the laparoscopic pneumoperitoneum stimulus is stronger than the skin incision stimulus, so that a higher concentration of sevoflurane is needed to inhibit the stress reaction in laparoscopic surgery, which is consistent with the results of our previous study [25]. The MACBAR of sevoflurane measured in this study is also significantly higher than the value (4.6%) reported in our previous study in gynecologic patients [12]. Although the same CO2 pneumoperitoneum stimulus was used, the MACBAR of sevoflurane could also be affected by the location of the perforation for establishing pneumoperitoneum, the patient’s age and gender [26, 27], the methods of measurement [25, 26] and the criterion of judgment for a positive or negative response [27, 28]. Dixon thought that the MACBAR values could be estimated as the mean of four independent crossovers of responses [28]. Paul and his colleagues thought that the reliability of the Dixon method increased with the number of pairs and six pairs was enough [29]. An increase of 15% or more from the baseline value of MAP or HR was taken as the criterion of a positive response in many studies [8, 30]. However, in clinic, the fluctuation of MAP or HR within the range of 20% is also acceptable and reasonable. Therefore, in our current study, an increase of 20% or more from pre-pneumoperitoneum stimulation values of MAP or HR was taken as the standard to judge a positive response.
Our results indicated the delta E or NE concentrations did not differ among all 5 groups (Table 3). This observation implies that when the sympathetic adrenergic response was inhibited in half patients to pneumoperitoneum stimulation in each group, the change of E or NE concentration would be similar, no matter the target controlled sufentanil concentration and the end tidal sevoflurane concentration. Our results also showed patients’ HR could be depressed to some degree with the increase of sufentanil plasma target concentration (Table 3). However, the decrease in HR did not result in a decrease of patients’ MAP, especially when a high concentration of sufentanil was administrated. It implies the hemodynamic safety range of sufentanil is large, which is consistent with the results of Fechner and his colleagues [31]. Our study did show that the use of sufentanil at a large dose results in a delay of anaesthesia recovery (Table 1). Therefore, the administration of larger dose sufentanil for short surgery such as laparoscopic cholecystectomy is not recommended.
There are several potential limitations to our study. First, we did not measure arterial blood gases during the pneumoperitoneum period. Although the end-expiratory CO2 partial pressure was maintained in the normal range by adjusting the ventilator, we did not measure the actual CO2 partial pressure to exclude the influence of hypercarbia on the sympathetic adrenergic response. Second, we did not measure the actual plasma sufentanil concentration. Although the Bovill pharmacokinetic model for target-controlled infusion has been shown to be safe in Asian people, it would have been desirable to measure the actual plasma sufentanil concentration to exclude individual error. Third, we did not monitor muscle relaxation. The level of neuromuscular blockade may influence the relaxation of the abdominal muscles, so as to affect the ease of creation of the pneumoperitoneum and thereby affect the adrenergic response during CO2 insufflation.
Conclusions
The MACBAR of sevoflurane can be decreased with increasing sufentanil plasma target concentrations. A ceiling effect of the decrease occurred at a sufentanil plasma target concentration of 0.5 ng ml− 1. When the sympathetic adrenergic response was inhibited in half patients to pneumoperitoneum stimulation in each group, the changes of E and NE concentrations showed no significant differences.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Change history
23 October 2020
An amendment to this paper has been published and can be accessed via the original article.
Abbreviations
- MACBAR :
-
Minimum alveolar concentration of sevoflurane for blocking adrenergic response
- E:
-
Epinephrine
- NE:
-
Norepinephrine
- CI:
-
Confidence interval
- BMI:
-
Body mass index
- ASA:
-
American Society of Anesthesiologists
- CO2 :
-
Carbon dioxide
- BIS:
-
Bispectral index
- MAP:
-
Mean arterial pressure
- HR:
-
Heart rate
- PACU:
-
Post-anesthesia care unit
References
Syn NL, Kabir T, Koh YX, Tan HL, Wang LZ, Chin BZ, et al. Survival advantage of laparoscopic versus open resection for colorectal liver metastases: A meta-analysis of individual patient data from randomized trials and propensity-score matched studies. Ann Surg. 2019. https://doi.org/10.1097/SLA.0000000000003672.
Siow SL, Goo ZQ, Mahendran HA, Wong CM. Laparoscopic versus open management of adult intussusception. Surg Endosc. 2019. https://doi.org/10.1007/s00464-019-07220-z.
Tanaka K, Misawa T, Baba Y, Ohashi S, Suwa K, Ashizuka S, et al. Surgical management of urachal remnants in children: open versus laparoscopic approach: A STROBE-compliant retrospective study. Medicine (Baltimore). 2019;98:e17480.
Ura T, Higuchi H, Taoda M, Sato T. Minimum alveolar concentration of sevoflurane that blocks the adrenergic response to surgical incision in women: MACBAR. Eur J Anesthesiol. 1999;16:176–81.
Wang Y, Sin SW, Zhang N, Zhao P. High-concentration sevoflurane exposure in mid-gestation induces apoptosis of neural stem cells in rat offspring. Neural Regen Res. 2018;13:1575–84.
Goyagi T. Dexmedetomidine reduced sevoflurane-induced neurodegeneration and long-term memory deficits in neonatal rats. Int J Dev Neurosci. 2019;75:19–26.
Liu Z, Wang JF, Meng Y, Fan XH, Deng XM, Li JB, et al. Effects of three target-controlled concentrations of sufentanil on MAC (BAR) of sevoflurane. CNS Neurosci Ther. 2012;18:361–4.
Albertin A, Casati A, Bergonzi P, Fano G, Torri G. Effects of two target-controlled concentrations (1 and 3 ng/ml) of remifentanil on MACBAR of sevoflurane. Anesthesiology. 2004;100:255–9.
Kim DK, Yoon SH, Kim JY, Oh CH, Jung JK, Kim J. Comparison of the effects of sufentanil and fentanyl intravenous patient controlled analgesia after lumbar fusion. J Korean Neurosurg Soc. 2017;60:54–9.
Ohnesorge H, Alpes A, Baron R, Gierthmühlen J. Influence of intraoperative Remifentanil and Sufentanil on sensory perception. A randomized trial. Curr Med Res Opin. 2016;32:1979–805.
Yang XL, Ma HX, Yang ZB, Zhang WS, Liu J. Comparison of MAC between intravenous injected isoflurane lipid emulsion and inhaled isoflurane in dogs. Anesthesiology. 2006;104:482–7.
Zou ZY, Zhao YL, Yang XL, Zhang GY, Zhou HG. Effects of different remifentanil target concentrations on MACBAR of sevoflurane in gynaecological patients with CO2 pneumoperitoneum stimulus. Br J Anaesth. 2015;114:634–9.
Polley LS, Columb MO, Naughton NN, Wagner DS, van de Ven CJM, Goralski KH. Effect of epidural epinephrine on the minimum local analgesic concentration of epidural bupivacaine in labor. Anesthesiology. 2002;96:1123–8.
Brunner MD, Braithwaite P, Jhaveri R, AI ME, Goodman DK, Smith LR, et al. MAC reduction of isoflurane by sufentanil. Br J Anaesth. 1994;72:42–6.
Leysen JE, Gommeren W, Niemegeers CJ. Sufentanil, a superior ligand for μ-opiate receptors: Binding properties and regional distribution in rat brain and spinal cord. Eur J Pharmacol. 1983;87:209–25.
Huang S, Zuo MZ. Target-controlled infusion of sufentanil reduces the capping effect of sevoflurane macbar during abdominal surgery. J Clin Res. 2012;29:889–92.
Dai YL, Chai XM, Zhu N, Wang KB, Bao WQ, Zhang XS, et al. Analgesia effect of premixed nitrous oxide/oxygen during the rehabilitation after total knee arthroplasty: a study protocol for a randomized controlled trial. Trials. 2019;20:399.
Gao LL, Yang LS, Zhang JJ, Wang YL, Feng K, Ma L, et al. A fixed nitrous oxide/oxygen mixture as an analgesic for trauma patients in emergency department: study protocol for a randomized controlled trial. Trials. 2018;19:527.
Emmanouil DE, Quock RM. Advances in understanding the actions of nitrous oxide. Anesth Prog. 2007;54:9–18.
Lewis VA, Gebhart GF. Evaluation of the periaque ductal central gray (PAG) as a morphine specific locus of action and examination of morphine induced and stimulation produced analgesia at coincident PAG loci. Brain Res. 1977;124:283–303.
Emmanouil DE, Ohgami Y, Chung E, Han S, Quock RM. Nitrous oxide (N2O) antinociception in the mouse abdominal constriction test is mediated by opioid receptors in the periaqueductal gray region of the brain. Proc West Pharmacol Soc. 2004;47:151.
Fang F, Guo TZ, Davies MF, Maze M. Opiate receptors in the periaqueductal gray mediate analgesic effect of nitrous oxide in rats. Eur J Pharmacol. 1997;336:137–41.
Hodges BL, Gagnon MJ, Gillespie TR, Breneisen JR, O'Leary DF, Hara S, et al. Antagonism of nitrous oxide antinociception in the rat hot plate test by site-specific mu and epsilon opioid receptor blockade. J Pharmacol Exp Ther. 1994;269:596–600.
Katoh T, Kobavashi S, Suzuki A, Iwamoto T, Bito H, Ikeda K. The effect of fentanyl on sevoflurane requirements for somatic and sympathetic responses to surgical incision. Anesthesiology. 1999;90:398–405.
Jiang PP, Yang XL, Guo YX, Xu J, Wang D. Comparison of sevoflarane MACBAR in normal liver function and grade b liver fJunction patients. Sichuan Med. 2019;40:137–41.
Mapleson WW. Effect of age on MAC in humans: a meta-analysis. Br J Anaesth. 1996;76:179–85.
Munoz HR, CortinezLI AFR, Dagnino JA. Remifentanil requirments during sevoflurane administration to block somatic and cardiovascular responses to skin incision in children and adults. Anesthesiology. 2002;97:1142–5.
Dixon WJ. Staircase bioassay: the up-and-down method. Neurosci Biobehav Rev. 1991;15:47–50.
Paul M, Fisher DM. Are estimates of MAC reliable. Anesthesiology. 2001;95:1362–70.
Dedola E, Albertin A, Poli D, Colla LL, Gandolfi A, Martani C, et al. Effect of nitrous oxide on desflurane MACBAR at two target-controlled concentrations of remifentanil. Minerva Anestesiol. 2008;74:165–72.
Fahlenkamp AV, Stoppe C, Cremer J, Biener IA, Peters D, Leuchter R, et al. Nausea and vomiting following balanced xenon anesthesia compared to sevoflurane: a post-hoc explorative analysis of a randomized controlled trial. PLoS One. 2016;11:e0153807.
Acknowledgements
Not applicable.
Funding
This study is supported by grant no. S15025 from the program of the Institution of Medicine of Sichuan Province, Chengdu, China, and partly supported by grant no. 18SXHZ0161 from the cooperation program of Municipal Government with College, Nanchong, Sichuan, China. The funding body did not partake in the design of the study, and collection, analysis, and interpretation of data, or in writing the manuscript.
Author information
Authors and Affiliations
Contributions
YX G and D W were the co-first authors of this article, conducted the study, collected and analyzed the data and writed the paper. XL Y was the corresponding authors of this article, helped with the study design and revision of the paper. PP J and J X helped with the clinical anaesthesia management. GY Z helped with the determination of blood samples. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Affiliated Hospital of North Sichuan Medical College, Nanchong, China (Approved No. 2017/043). Written informed consents were obtained from all participants. All experiment procedures (consisted of invasive manipulation) and data collection were conducted with prior informed consent.
Consent for publication
Not applicable.
Competing interests
All authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Guo, Y., Wang, D., Yang, X. et al. Effects of different sufentanil target concentrations on the MACBAR of sevoflurane in patients with carbon dioxide pneumoperitoneum stimulus. BMC Anesthesiol 20, 239 (2020). https://doi.org/10.1186/s12871-020-01160-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-020-01160-1