Abstract
Background
Preoperative airway assessment help anticipate a difficult airway. We hypothesized that a close association existed between difficult laryngoscopy and the neck circumference/inter-incisor gap ratio (RNIIG). Our aim was to determine its utility in predicting difficult laryngoscopy in cervical spondylosis patients.
Methods
Two hundred thirteen consecutive patients, aged 20–70 years, scheduled to undergo cervical spine surgery under general anesthesia, were recruited. Preoperative assessments included inter-incisor gap (IIG), thyromental distance (TMD), neck circumference (NC), NC/IIG ratio (RNIIG), NC/TMD ratio (RNTMD) and modified Mallampati test (MMT). Cormack–Lehane scales were assessed during intubation. The anesthesiologist was blinded to the airway assessments. RNIIG’s ability to predict difficult laryngoscopy was compared with that of established predictors.
Results
Difficult laryngoscopy incidence was 16.4%. Univariate analysis showed that male gender, increased age, weight, NC, RNIIG and RNTMD, decreased IIG and TMD, and MMT 3 and 4 were associated with difficult laryngoscopy. Binary multivariate logistic regression analyses identified only one factor that was independently associated with difficult laryngoscopy: RNIIG. The odds ratio and 95% confidence interval (95% CI) were 1.932 (1.504–2.482). RNIIG (≥9.5) exhibited the largest area under the curve (0.80; 95% CI 0.73–0.86) and the highest sensitivity (88.6%; 95% CI 78.1–99.1) and negative predictive value (96.6%; 95% CI 94.0–99.2), confirming its better predictive ability.
Conclusions
RNIIG is a new and simple predictor with a higher level of efficacy, and could help anesthetists plan for difficult laryngoscopy management in cervical spondylosis patients.
Trial registration
ChiCTR-OON-16008320 (April 19th, 2016).
Similar content being viewed by others
Background
Airway management is crucial in clinical anesthesia. The incidence of difficult laryngoscopy and intubation in various settings has ranged widely, from 1 to 15% [1–3]. For patients undergoing surgery for cervical spondylosis, they had impaired cervical mobility. Considering the fact that the best laryngoscopy view is achieved when the oral, pharyngeal, and laryngeal axes are most closely matched, it was difficult for an anesthesiologist to expose the glottis in cervical spondylosis patients. Therefore, compared with other patients, cervical spondylosis patients have a higher incidence of difficult laryngoscopy which causes a large proportion of unexpected difficult airways and significantly increases the morbidity and mortality rates [4]. Therefore, identifying a more reliable optimal predictor of difficult laryngoscopy in cervical spondylosis patients undergoing general anesthesia is desirable.
Suggested predictors for difficult laryngoscopy include increased neck circumference, high score of Mallampati test (MMT), small inter-incisor gap (IIG) and thyromental distance (TMD) [5]. All of these techniques are relatively quick bedside tests that are easy to perform with no special equipment. However, none of them alone has high diagnostic accuracy, particularly in cervical spondylosis patients.
Many studies found that modifications to bedside tests have shown improved predictive values. An example includes the ratio of neck circumference to TMD (RNTMD). When comparing independent predictors of difficult tracheal intubation in obese patients including the Mallampati test and the Wilson score, the RNTMD had the best predictive outcome [6]. IIG is a major single predictor for difficult airways. It reflects craniocervical extension, which is restricted in cervical spondylosis patients [7]. In our former study of cervical spondylosis patients [8], we found that IIG could predict difficult airway better than TMD. Therefore, our hypothesis was that the NC/IIG ratio (RNIIG) would be more useful than the previously reported indices for identifying difficult intubation in cervical spondylosis patients.
Methods
After institutional ethics committee approval (IRB00006761-2015021, Medical Ethics Committee of Peking University Third Hospital), informed written consent was obtained from all patients. We recruited 213 patients (20–70 years of age) undergoing cervical spine surgery with general anesthesia between April 2016 and October 2016. Patients met the following criteria: mentally competent adult and American Society of Anesthesiologists (ASA) score I–III; requirement for preoperative neck immobilization with a hard plastic collar; elective cervical spine surgery for severe cervical spondylosis. We excluded patients with pregnancy or oropharyngeal mass.
Clinical tests for the preoperative airway assessment and demographic information—gender, age, height, weight, body mass index (BMI)—were recorded 1 day before surgery by one anesthesiologist who was not involved in the anesthesia induction (to avoid inter-observer variability).
The difficulty of laryngoscopy was assessed with the Cormack–Lehane (C–L) scale, the results of which were recorded by another senior anesthetist. The C–L scale is graded in Table 1. Those with class III–IV and class I–II were defined as the difficult and easy laryngoscopy groups, respectively [9].
The IIG (distance between the upper and lower incisors at the midline) was measured by asking each patient to open the mouth to the maximum extent. The TMD (distance from the thyroid notch to the mentum) was measured with the neck extended. Neck circumference at the level of the cricoid cartilage was measured. The RNIIG and RNTMD were then calculated. The oropharyngeal view was assessed using a MMT classification. The patients were asked to sit, open their mouths fully, and protrude the tongue without phonation [10]. The cases were rated in Table 2.
No premedication was allowed. Preoperative routine monitoring included noninvasive blood pressure, heart rate, pulse oximetry, and electrocardiography. Anesthesia was induced with sufentanil (0.3 μg/kg) and propofol (2 mg/kg). Patients were manually ventilated following loss of consciousness. Neuromuscular blockade was achieved by injection of rocuronium (0.6 mg/kg). The C–L grade was determined during direct laryngoscopy, in all patients in the sniff position, by the same senior anesthesiologist not involved in the preoperative assessment. After that, tracheal intubation was then performed with the direct laryngoscope or alternative devices by the same anesthesiologist. In patients with difficult airway, intubation was completed following ASA guidelines [11].
Estimating a 10% incidence of difficult laryngoscopy [12], a sample size of 189 patients was calculated to have at least 90% power to detect a difference in predictors between the difficult and easy laryngoscopy groups estimated with PASS software (version 8.03; NCSS LLC, Kaysville, UT, USA). In consideration of the dropout, 213 patients were recruited in our study finally. SPSS software (version 21.0; IBM Corp, Armonk, NY, USA) was used for statistical analysis. Categorical variables were analyzed using the χ 2 test, and continuous variables were analyzed by an independent samples t-test. Binary multivariate logistic regression analyses were performed to identify multivariate predictors for difficult airways. A receiver operating characteristic (ROC) curve was used to describe the discrimination abilities of the predictive indicators. The area under the curve (AUC) was used as the quantitative index to describe the ROC curve. The 95% CI was calculated, and P < 0.05 was considered to indicate statistical significance.
Results
A total of 213 patients comprising 141 men (66.2%) and 72 women (33.8%) were included in the study. The overall incidence of difficult laryngoscopy was 16.4% (35/213). Univariate analysis demonstrated several risk factors that were associated with difficult laryngoscopy: male gender, increased age, weight, NC, RNIIG and RNTMD, decreased IIG and TMD, and MMT 3 and 4 (P < 0.05). The demographic variables and clinical tests for the study population are presented in Table 3.
Binary multivariate logistic regression (forward-Wald) analyses identified only one independent risk factor from the general condition and clinical tests that correlated best as a predictor of a difficult airway: RNIIG. The odds ratio (OR) and 95% CI were 1.932 (1.504–2.482) (Table 4).
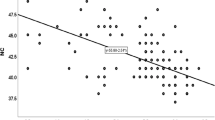
The AUC and standard error calculated for those clinical tests are shown in Table 5. We used the ROC curve and AUC to identify the predictive abilities of the clinical predictors. The AUC for RNIIG was higher than those obtained for RNTMD, IIG, NC, MMT, and TMD.
True-positive (TP), true-negative (TN), false-positive (FP), and false-negative (FN) results, together with the sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) calculated for those clinical tests are shown in Table 6. Compared with the other tests, RNIIG (≥9.5) had the highest sensitivity (88.6%; 95% CI 78.1–99.1) and negative predictive value (96.6%; 95% CI 94.0–99.2), confirming its better predictive ability.
Discussion
“An anaesthetist must assess the patient before anaesthesia and devise an appropriate plan of anaesthetic management” – The Good Anaesthetist, Royal College of Anaesthetists 2010 [13]. Airway assessment consists of taking a medical history, performing a physical examination, reviewing the clinical records and carring out additional tests. Successful identification of physical features that are suggestive of a difficult airway should direct planning toward safe airway management. Accordingly, many national airway guidelines emphasize the importance of a thorough and skilled assessment of all patients undergoing anesthesia [14, 15].
Certain single predictors such as Mallampati test and thyromental distance, performed at the bedside in seconds, can be used for routine screening in the general population, but are inadequate in patients undergoing surgery for cervical spondylosis. In these patients, there are a high incidence of difficult airway and few reliable tests to evaluate the difficult airway. In this study, the incidence of difficult laryngoscopy was 16.4%, which is higher than what has been reported in previous studies [2]. Bedside airway tests have been criticized for their poor predictive capability, the poor predictive capability relates to the high incidence of unanticipated difficulty airway. In this study, we found that RNIIG was a more accurate method for predicting difficult laryngoscopy in these patients.
Our data demonstrated that male gender, increasing weight and age were associated with difficult laryngoscopy. A significantly greater proportion of difficult tracheal intubations had been found in men and obesity patients [16, 17], which were attributed to differences in neck fat deposition between the genders [18]. An association between difficult laryngoscopy and older patients has also been reported [19]. Osteoarthritic changes, associated with decreased thyromental distance, cervical spine movement, interincisor distance, and grade of dentition, may be responsible for age-related increases in difficult laryngoscopy. Although patients in the difficult laryngoscopy group were heavier than those in the easy laryngoscopy group, BMI didn’t show statistically significant risk for difficult laryngoscopy. The results were in accordance with the study reported by Prakash et al. [20]. In a cohort study from the Danish Anesthesia Database of 91,332 consecutive patients, by examining the relative impact of weight and height, only weight was found as an independent risk factor for difficult tracheal intubation [21].
The Mallampati test [22] and thyromental distance [23] are all impaired by cervical spine limitation in cervical spondylosis patients which suggests the importance of adequate neck movement when trying to predict difficult airway. MMT could reflect oropharyngeal cavity volume, but it could not assess laryngeal condition. As for TMD, short TMD is a surrogate for inadequate head extension, rather than small submandibular space, when indicating possible difficult direct laryngoscopy. Both of MMT and TMD had lower AUC in our study. The results of the current study support those previous studies regarding poor sensitivity values for the MMT and TMD tests [24, 25].
The IIG has been demonstrated to be one of the most sensitive single predictors of a difficult airway in normal patients [26]. Craniocervical extension occurs during normal mouth opening, and nearly maximum mouth opening was obtained with 26° (95% CI 22–30) of craniocervical extension from the neutral position [7]. Craniocervical extension is an integral part of complete mouth opening in conscious subjects, whereas mouth opening may be restricted in patients with cervical spondylosis. However, the sensitivity of the IIG was not high enough (28.6%), suggesting that it was not reliable as a single predictor.
Ezri et al. reported that the abundance of pre-tracheal soft tissue at the level of the vocal cords was a good measure that fully distinguished an easy laryngoscopy from a difficult one in obese patients [16]. The accumulation of pre-tracheal soft tissue might cause difficult laryngeal exposure. The NC alone might not clearly indicate the amount of soft tissue at various topographical regions within the neck. Therefore, the NC might not be a perfect indicator. Our study also confirmed that NC was a moderate predictor, with 65.7% sensitivity and 0.689 AUC.
Kim et al. [6] found that RNTMD was a better indicator than either the NC or TMD alone. It was more difficult for patients with both a large neck circumference and a short neck to be given intubation than patients with a large neck circumference or a short neck alone. Previous studies have suggested that using a single screening test for difficult intubations only provides limited accuracy [27]. However, combinations of tests may increase the accuracy of diagnosis. The El-Ganzouri or Wilson scores [28, 29] are multivariate risk index systems, but they are time consuming as they contain multiple risk factors. Thus, combining two of the most valuable risk factors may add some incremental diagnostic value while not significantly increasing the burden of testing.
RNIIG is a new predictor of difficult laryngoscopy in cervical spondylosis patients, it contained two indicators: IIG and NC, which represented oropharyngeal cavity volume, craniocervical extension and laryngeal cavity volume. Compared with RNTMD, IIG, NC, MMT and TMD, RNIIG showed a relatively large AUC on the ROC curve which revealed that the RNIIG is highly predictive. The AUC for IIG was higher than TMD, so it might be the reason why RNIIG was better than RNTMD. RNIIG had higher sensitivity than any other test, thus providing fewer false-negative predictions. In other words, RNIIG missed the least number of difficult laryngoscopies. The failure of a test to predict a difficult case (false-negative result) could result in unanticipated difficult airway and life-threatening events. Binary multivariate logistic regression (forward-Wald) analyses identified only one independent risk factor from among the general condition and clinical tests that correlated best as a predictor of a difficult airway: RNIIG. The ORs and 95% CI were 1.932 (1.504–2.482). Wilson model is the most commonly used multivariate clinical model for predicting difficult airway. Naguib et al. [30] reported that the AUC and sensitivity of Wilson model were 0.79 (95% CI, 0.72–0.85) and 40.2% (95% CI, 30.0–50.0%). In our study, the AUC and sensitivity of RNIIG were 0.80 (95% CI, 0.73–0.86) and 88.6% (95% CI, 78.1–99.1%) suggesting that RNIIG showed better performance than Wilson model, and it could be more useful as a simple screening test for cervical spine surgery. In clinical practice, if we find the RNIIG of a cervical spondylosis patient is more than 9.5, it is suggested that we may encounter a difficult laryngoscopy. Therefore, we should follow the practice guidelines for management of the difficult airway recommended by the American Society of Anesthesiologists task force. Be sure that a senior anesthesiologist and visual tools (video laryngoscope, shikani optical stylet, fiberoptic bronchoscope, et al.) are all standby rather than rapid induction of general anesthesia with Macintosh laryngoscope for intubation.
Our study had some limitations. First, it was not completely blinded as the anesthesiologist could recognize the patients’ characteristics in the operating theater. It was thus impossible to maintain complete blindness during this study. Second, determination of the best cutoff point as a difficult laryngoscopy predictor, and its analysis as a measure of prediction, had both been performed on the same population. This might influence the statistical results to a certain extent. Third, we calculated the ideal cutoff values for RNIIG and RNTMD from the data obtained in the study, whereas the cutoff values for the other tests were obtained from the literature. Therefore, the ideal predictor (RNIIG) and its cutoff value should be tested in a future study.
Conclusions
We found a 16.4% incidence of difficult laryngoscopy in cervical spondylosis patients. RNIIG was the only independent risk factor for difficult laryngoscopy. RNIIG of ≥9.5 yielded moderate to high sensitivity, specificity, and negative predictive value. Thus, we consider a preoperative value of RNIIG ≥9.5 to be a good predictor of difficult laryngoscopy in cervical spondylosis patients.
Abbreviations
- 95% CI:
-
95% confidence interval
- AUC:
-
Area under the curve
- C–L scale:
-
Cormack–Lehane scale
- IIG:
-
Inter-incisor gap
- MMT:
-
Modified Mallampati test
- NC:
-
Neck circumference
- RNIIG:
-
NC/IIG ratio
- RNIIG:
-
The neck circumference/inter-incisor gap ratio
- RNTMD:
-
NC/TMD ratio
- ROC curve:
-
Receiver operating characteristic curve
- TMD:
-
Thyromental distance
References
De Jong A, Molinari N, Terzi N, Mongardon N, Arnal JM, Guitton C, Allaouchiche B, Paugam-Burtz C, Constantin JM, Lefrant JY, et al. Early identification of patients at risk for difficult intubation in the intensive care unit: development and validation of the MACOCHA score in a multicenter cohort study. Am J Respir Crit Care Med. 2013;187(8):832–9.
Fox WT, Harris S, Kennedy NJ. Prevalence of difficult intubation in a bariatric population, using the beach chair position. Anaesthesia. 2008;63(12):1339–42.
Adamus M, Fritscherova S, Hrabalek L, Gabrhelik T, Zapletalova J, Janout V. Mallampati test as a predictor of laryngoscopic view. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2010;154(4):339–43.
Shiga T, Wajima Z, Inoue T, Sakamoto A. Predicting difficult intubation in apparently normal patients: a meta-analysis of bedside screening test performance. Anesthesiology. 2005;103(2):429–37.
Gonzalez H, Minville V, Delanoue K, Mazerolles M, Concina D, Fourcade O. The importance of increased neck circumference to intubation difficulties in obese patients. Anesth Analg. 2008;106(4):1132–6. table of contents.
Kim WH, Ahn HJ, Lee CJ, Shin BS, Ko JS, Choi SJ, Ryu SA. Neck circumference to thyromental distance ratio: a new predictor of difficult intubation in obese patients. Br J Anaesth. 2011;106(5):743–8.
Calder I, Picard J, Chapman M, O’Sullivan C, Crockard HA. Mouth opening: a new angle. Anesthesiology. 2003;99(4):799–801.
Xu M, Li X, Wang J, Guo X. Application of a new combined model including radiological indicators to predict difficult airway in patients undergoing surgery for cervical spondylosis. Chin Med J (Engl). 2014;127(23):4043–8.
Krage R, van Rijn C, van Groeningen D, Loer SA, Schwarte LA, Schober P. Cormack-Lehane classification revisited. Br J Anaesth. 2010;105(2):220–7.
Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984;39(11):1105–11.
Frerk C, Mitchell VS, McNarry AF, Mendonca C, Bhagrath R, Patel A, O’Sullivan EP, Woodall NM, Ahmad I. Difficult Airway Society 2015 guidelines for management of unanticipated difficult intubation in adults. Br J Anaesth. 2015;115(6):827–48.
Etezadi F, Ahangari A, Shokri H, Najafi A, Khajavi MR, Daghigh M, Moharari RS. Thyromental height: a new clinical test for prediction of difficult laryngoscopy. Anesth Analg. 2013;117(6):1347–51.
Baker P. Assessment before airway management. Anesthesiol Clin. 2015;33(2):257–78.
Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, Hagberg CA, Caplan RA, Benumof JL, Berry FA, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013;118(2):251–70.
Law JA, Broemling N, Cooper RM, Drolet P, Duggan LV, Griesdale DE, Hung OR, Jones PM, Kovacs G, Massey S, et al. The difficult airway with recommendations for management--part 2--the anticipated difficult airway. Can J Anaesth. 2013;60(11):1119–38.
Ezri T, Gewurtz G, Sessler DI, Medalion B, Szmuk P, Hagberg C, Susmallian S. Prediction of difficult laryngoscopy in obese patients by ultrasound quantification of anterior neck soft tissue. Anaesthesia. 2003;58(11):1111–4.
Rose DK, Cohen MM. The airway: problems and predictions in 18,500 patients. Can J Anaesth. 1994;41(5 Pt 1):372–83.
Whittle AT, Marshall I, Mortimore IL, Wraith PK, Sellar RJ, Douglas NJ. Neck soft tissue and fat distribution: comparison between normal men and women by magnetic resonance imaging. Thorax. 1999;54(4):323–8.
Al Ramadhani S, Mohamed LA, Rocke DA, Gouws E. Sternomental distance as the sole predictor of difficult laryngoscopy in obstetric anaesthesia. Br J Anaesth. 1996;77(3):312–6.
Prakash S, Kumar A, Bhandari S, Mullick P, Singh R, Gogia AR. Difficult laryngoscopy and intubation in the Indian population: an assessment of anatomical and clinical risk factors. Indian J Anaesth. 2013;57(6):569–75.
Lundstrom LH, Moller AM, Rosenstock C, Astrup G, Wetterslev J. High body mass index is a weak predictor for difficult and failed tracheal intubation: a cohort study of 91,332 consecutive patients scheduled for direct laryngoscopy registered in the Danish Anesthesia Database. Anesthesiology. 2009;110(2):266–74.
Mashour GA, Stallmer ML, Kheterpal S, Shanks A. Predictors of difficult intubation in patients with cervical spine limitations. J Neurosurg Anesthesiol. 2008;20(2):110–5.
Qudaisat IY, Al-Ghanem SM. Short thyromental distance is a surrogate for inadequate head extension, rather than small submandibular space, when indicating possible difficult direct laryngoscopy. Eur J Anaesthesiol. 2011;28(8):600–6.
Lundstrom LH, Vester-Andersen M, Moller AM, Charuluxananan S, L’Hermite J, Wetterslev J. Poor prognostic value of the modified Mallampati score: a meta-analysis involving 177 088 patients. Br J Anaesth. 2011;107(5):659–67.
Khan ZH, Mohammadi M, Rasouli MR, Farrokhnia F, Khan RH. The diagnostic value of the upper lip bite test combined with sternomental distance, thyromental distance, and interincisor distance for prediction of easy laryngoscopy and intubation: a prospective study. Anesth Analg. 2009;109(3):822–4.
Yildiz TS, Solak M, Toker K. The incidence and risk factors of difficult mask ventilation. J Anesth. 2005;19(1):7–11.
Lee A, Fan LT, Gin T, Karmakar MK, Ngan Kee WD. A systematic review (meta-analysis) of the accuracy of the Mallampati tests to predict the difficult airway. Anesth Analg. 2006;102(6):1867–78.
Cortellazzi P, Minati L, Falcone C, Lamperti M, Caldiroli D. Predictive value of the El-Ganzouri multivariate risk index for difficult tracheal intubation: a comparison of Glidescope videolaryngoscopy and conventional Macintosh laryngoscopy. Br J Anaesth. 2007;99(6):906–11.
Wilson ME, Spiegelhalter D, Robertson JA, Lesser P. Predicting difficult intubation. Br J Anaesth. 1988;61(2):211–6.
Naguib M, Scamman FL, O’Sullivan C, Aker J, Ross AF, Kosmach S, Ensor JE. Predictive performance of three multivariate difficult tracheal intubation models: a double-blind, case-controlled study. Anesth Analg. 2006;102(3):818–24.
Acknowledgments
We sincerely thank all the staff of the Anesthesiology Department of Peking university third hospital for their help in this research.
Funding
The present study was supported by Hospital Medical Research Foundation from Peking University Third Hospital (No. BYSY2014019).
Availability of data and materials
The data during this study are available from the corresponding author on reasonable request.
Authors’ contributions
YH and MX designed and coordinated the study, recruited the patients, collected and interpreted data, and drafted the manuscript. ML, JW and XG participated in study design, CN analyzed the data and performed statistical analysis, YT participated in patient recruitment and data collection. All authors discussed the results, read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Written informed consent was obtained from the patient for publication of this article.
Ethics approval and consent to participate
The study was approved by Peking university third hospital medical ethics committee (IRB00006761-2015021) and each participant provided written informed consent.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Han, Yz., Tian, Y., Xu, M. et al. Neck circumference to inter-incisor gap ratio: a new predictor of difficult laryngoscopy in cervical spondylosis patients. BMC Anesthesiol 17, 55 (2017). https://doi.org/10.1186/s12871-017-0346-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-017-0346-y