Abstract
Background
Antibiotic-associated diarrhea (AAD) refers to symptoms of diarrhea that cannot be explained by other causes after the use of antibiotics. AAD is thought to be caused by a disruption of intestinal ecology due to antibiotics. Fecal Microbiota Transplantation (FMT) is a treatment method that involves transferring microbial communities from the feces of healthy individuals into the patient’s gut.
Method
We selected 23 AAD patients who received FMT treatment in our department. Before FMT, we documented patients’ bowel movement frequency, abdominal symptoms, routine blood tests, and inflammatory markers, and collected fecal samples for 16S rRNA sequencing to observe changes in the intestinal microbiota. Patients’ treatment outcomes were followed up 1 month and 3 months after FMT.
Results
Out of the 23 AAD patients, 19 showed a clinical response to FMT with alleviation of abdominal symptoms. Among them, 82.61% (19/23) experienced relief from diarrhea, 65% (13/20) from abdominal pain, 77.78% (14/18) from abdominal distension, and 57.14% (4/7) from bloody stools within 1 month after FMT. Inflammatory markers IL-8 and CRP significantly decreased after FMT, but there were no noticeable changes in WBC, IL-6, and TNF-α before and after transplantation. After FMT, the abundance of Bacteroides and Faecalibacterium increased in patients’ fecal samples, while the abundance of Escherichia-Shigella and Veillonella decreased.
Conclusion
FMT has a certain therapeutic effect on AAD, and can alleviate abdominal symptoms and change the intestinal microbiota of patients.
Similar content being viewed by others
Introduction
Antibiotic-associated diarrhea (AAD) refers to diarrhea symptoms that cannot be explained by other reasons after using antibiotics, often accompanied by abdominal pain, bloating, and bloody stools, and is a common complication in antibiotic treatment [1, 2]. The incidence of AAD varies with different antibiotics, and the incidence rate can be as high as 35% in patients receiving specific antibiotic treatment [3]. AAD is thought to be caused by dysbiosis of the gut due to antibiotics, which may lead to overgrowth of specific pathogens and changes in the function of the microbiome [3, 4]. It is estimated that only 15-25% of AAD cases are caused by overgrowth of Clostridioides difficile [5]. On the other hand, the occurrence of AAD may be related to the loss of beneficial metabolic activities of intestinal microorganisms. Changes in the composition and quantity of the gut microbiota (even without the overgrowth of pathogenic microorganisms) can lead to disturbances in overall colon metabolism, thereby causing AAD [6, 7]. Colonic microbiota such as Bacteroides, Bifidobacterium, and Lactobacillus can metabolize carbohydrates that the colon cannot absorb as a source of energy, producing short-chain fatty acids (SCFAs) [8]. Antibiotic treatment leading to a reduction in these bacteria can cause increased carbohydrate content in the colon, leading to osmotic diarrhea. In addition, butyric acid is an important energy source for the distal colonic mucosa [9]. A reduction in SCFAs production caused by a decrease in colonic anaerobic bacteria levels can directly cause colonic mucosal dysfunction and diarrhea [10].
Currently, the preventive intervention for AAD is the use of probiotics, which are defined as “live microorganisms that, when administered in adequate amounts, confer a health benefit on the host” [11]. Research has found that probiotics can reduce the overall risk of AAD during and 7 days after antibiotic treatment by restoring homeostasis in the gut [2]. Fecal Microbiota Transplantation (FMT) is a treatment method that involves transplanting the microbiota from a healthy person’s feces into a patient’s gut. This treatment aims to restore balance in the gut microbiota and improve a series of diseases related to the gut microbiota, such as recurrent Clostridioides difficile infection (rCDI) [12]. Therefore, research teams have begun to explore the efficacy of FMT on AAD [13]. FMT has been widely used in the treatment of rCDI, with an effective rate of up to 90%. Western countries have already included FMT in the first-line treatment of rCDI [14,15,16,17]. This article mainly explores the efficacy and safety of FMT for AAD, and analyzes the changes in the gut microbiota of AAD patients after FMT.
Materials and methods
Patient and data collection
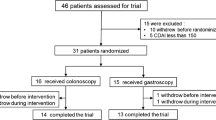
This study has been registered on Clinical Trials.gov as the NCT05990972 study. From July 2020 to April 2023, 23 patients with AAD who underwent Fecal Microbiota Transplantation (FMT) in our department were selected. The patient’s information is shown in Table 1. Before FMT, we recorded the patient’s bowel movement frequency, abdominal symptoms, routine blood tests, and inflammation indicators, and collected their stool samples for 16S rRNA sequencing. 1 month and 3 months after FMT, we followed up on the efficacy of the treatment.
Inclusion criteria: 1) Clear diagnosis of Antibiotic-associated diarrhea (AAD); 2) Stool samples were preserved during treatment; 3) Complete data on blood routine examination and inflammation factor checks; 4) Ineffective against conventional AAD treatments.
Exclusion criteria: 1) Suffering from other chronic gastrointestinal diseases; 2) History of malignant tumors; 3) History of gastrointestinal surgery; 4) Abnormal colonoscopy findings.
Results and definitions
Adverse Events (AEs) are recorded during hospitalization for FMT. AEs refer to any new symptoms, worsening of previous symptoms, and abnormal laboratory test results that occur during the FMT process. “Cure” is defined as a defecation frequency of less than or equal to three times per day, complete disappearance of abdominal symptoms, and no recurrence. “Relief” is defined as a defecation frequency of more than three times per day, but less than the frequency at admission, and less severe abdominal symptoms than at admission. Both “cure” and “relief” are collectively defined as a clinical response.
The donor screening
Donor selection should meet the following criteria: (1) Age between 18 and 30 years; (2) BMI of 18-25 kg/m^2; (3) No pathological signs during physical examination; (4) No history of infectious diseases; (5) No recent gastrointestinal, metabolic, neurological history, or other systemic diseases; (6) No recent use of drugs that could damage the composition of the gut microbiota; (7) Regular healthy diet, appropriate exercise, harmonious family environment, and no smoking or drinking habits; (8) Passing blood and stool tests before donating feces, including general blood and stool tests as well as potential pathogen or infectious disease screenings [18].
Preparation and procedure of FMT
Approximately 100 g of donated feces is collected into a sterile container, to which 300 mL of saline is added. The mixture is then stirred to allow it to pass through 2.0 mm and 0.5 mm mesh filters. Sterile glycerol is added to reach a final concentration of 10%, and the solution is stored at − 20 °C for 1-8 weeks until use. Patients receive a polyethylene glycol bowel lavage 12-24 hours before FMT. The fecal suspension is thawed in a 37 °C water bath and is infused into the patient through a nasoenteric tube placed in advance, within 6 hours after thawing [18, 19].
DNA extraction and 16 S rRNA gene sequencing
We used the PowerMax Extraction Kit (MoBio Laboratories, Carlsbad, CA, USA) to extract microbial genomic DNA from fecal samples according to the manufacturer’s instructions. After extraction, we employed agarose gel electrophoresis and NanoDrop ND-1000 spectrophotometer (Thermo Fisher Scientific, Waltham, MA, USA) to measure the concentration and purity of microbial DNA in the fecal samples. To amplify the V4 regions of 16S rRNA, we used two universal primers, specifically 515 Forward Primer (5′-GTGYCAGCMGCCGCGGTAA-3′) and 806 Reversed Primer (5′-GGACTACNVGGGTWTCTAAT-3′). The polymerase chain reaction (PCR) was performed in a 50 μl reaction system, with the PCR cycle consisting of pre-denaturation at 98 °C for 30 seconds, followed by 25 cycles of denaturation at 98 °C for 15 seconds, annealing at 58 °C for 15 seconds, and extension at 72 °C for 15 seconds, with a final extension at 72 °C for 1 minute. Subsequently, we used AMPure XP Beads (Beckman Coulter, Indianapolis, USA) to purify the PCR products and quantified the DNA concentration using the PicoGreen dsDNA Assay Kit (Invitrogen, Carlsbad, CA, USA). After quantitative analysis, the DNA library was sequenced on Illumina NovaSeq 6000 platform with 2 × 250 bp paired-end reads at Shanghai Bao Yuan Pharmaceutical Co., Ltd.
The 16S rRNA sequencing data of all participants in the study has been uploaded to the National Center for Biotechnology Information platform, with the accession number PRJNA1037722.
Data processing, analysis and visualization
The QIIME2 version 2023.5.0 [20] software was harnessed to implement DADA2 [21] processing on the raw sequencing data. Initially, the data was subjected to quality filtering, effectively eliminating adapter and barcode sequences. The information was also trimmed to an appropriate length to discard sequences that fell below an average quality score of 25. Subsequently, the sequences were dereplicated, scrutinized for sequence variants, merged, and underwent a standard DADA2 procedure for chimera checking. Any amplicon sequence variant (ASV) that had a frequency lower than 50 across all samples or appeared in less than three samples was filtered out. Filtered representative sequences and biom-formatted tables were later assigned using the Greengenes2 2022.10 database. The final result incorporated a table and taxonomy artifacts, which were exported as a biom table and a text file respectively, for future analysis after the addition of taxa data to the biom-formatted ASV table.
The “microeco” package was employed to generate several plots, including Principal Component Analysis (PCA), Principal Coordinate Analysis (PCoA), and Non-Metric Multidimensional Scaling (NMDS) plots based on Jaccard and Unweighted distances, alongside taxonomic composition bar plots, feature abundance box plots, Venn diagrams, and heatmap plots. As the microbiota was represented in relative abundance, Linear Discriminant Analysis (LDA) effect size (LEfSe) analysis [22] was used to observe differences in microbiota composition. After setting the alpha value to 0.05 and the LDA score threshold to 2, the LEfSe bar plot and corresponding cladogram were constructed using the “microeco” package.
The co-occurrence network was calculated using the “microeco” package by employing Spearman analysis for correlation coefficient computation. The P-value threshold was set to 0.01, while the coefficient threshold was automatically optimized. Subsequently, the cluster_fast_greedy method was utilized for network clustering, and visualization was conducted using Gephi (v0.10.1).
The Phylogenetic Investigation of Communities by Reconstruction of Unobserved States (PICRUSt2) (v2.5.1) [23] workflow was leveraged to predict the metagenome functions of the microbiota, and functional pathways were annotated using the Kyoto Encyclopedia of Genes and Genomes (KEGG) database [24,25,26,27].
Statistical analysis
In this study, all clinical characteristics are expressed as mean ± standard deviation (SD) or numbers and percentages. The clinical features between different groups were tested using rank sum test and chi-square test. A significance level of P < 0.05 was set, and SPSS version 26.0 was used as the statistical tool.
Results
Clinical outcomes of FMT treatment for AAD
A total of 23 patients underwent 42 fecal microbiota transplantation (FMT) procedures. Based on the frequency of bowel movements and abdominal symptoms, 82.61% (19/23) of patients responded clinically 1 month after FMT, of which the cure rate was 73.91% (17/23). The frequency of bowel movements significantly decreased. The clinical response rate 3 months after FMT was 78.26% (18/23), with a cure rate of 65.22% (15/23) (Table 2). As shown in Table 3, 65% (13/20) of abdominal pain, 77.78% (14/18) of bloating, and 57.14% (4/7) of bloody stools responded clinically within 1 month after FMT. According to the results of the inflammatory markers and routine blood tests before and after FMT in these 23 patients (Table 4), it was found that the inflammation indicators of AAD patients were higher than normal levels before FMT, and there was a decreasing trend after FMT, especially IL-8 and CRP. However, there was no significant change trend in WBC, IL-6, and TNF-α before and after transplantation.
The safety of FMT for AAD
During the in-hospital FMT period and the three-month follow-up period after FMT, 21.73% (5/23) of patients had eight cases of FMT-related adverse events (AEs) (Fig. 1). The most common AEs were abdominal pain and bloating, each with two cases (2/23, 8.7%), followed by one case (1/23, 4.3%) of nausea, vomiting, fever, and increased frequency of diarrhea. These AEs were all mild, with no FMT-related deaths.
The changes in the composition and structure of the gut microbiota before and after FMT
Figures 2A and 2B illustrate the composition of microbiota at different taxonomic levels. At the phylum level, the top four in terms of abundance after transplantation are Firmicutes, Proteobacteria, Bacteroidota, and Actinobacteriota. Among them, Firmicutes, Bacteroidota, and Actinobacteriota increase after transplantation, while Proteobacteria decreases. At the genus level, the abundance of Bacteroides and Faecalibacterium increase after transplantation, while the abundance of Escherichia-Shigella and Veillonella decrease.
The changes of intestinal microbiota before and after FMT. A Phylum level. B Genus level. C Gut microbiota difference between the before and after FMT were identified with a LEfSe analysis with LDA score threshold> 2.0. D The cladogram plot. Co-occurrence network analysis for the before and after FMT. E Before FMT. F After FMT. G KEGG level 2 annotation for the differently abundant function pathway before and after FMT
Next, we wanted to identify the differences between certain taxonomic groups before and after transplantation, so we conducted a LEfSe analysis, using effect size measurements to enrich bacterial groups with different abundances between the two groups. Under the significance threshold (p < 0.05) and LDA score > 2, Fig. 2C shows the taxonomic units of different abundances. We also generated a dendrogram from the LEfSe analysis to provide visual results of the phylogenetic distribution of these samples from the order to genus level. The size of each circle in the cladogram represents the abundance of certain taxonomic groups (Fig. 2D). To further explore the key groups before and after transplantation, we constructed a microbial co-occurrence network (Figs. 2E and 2F) using the Spearman correlation between different groups, where some specific species serve as key nodes in the network. From this network diagram, we can observe that compared to before FMT, after FMT, Prevotella and Bacteroides are important nodes connected to Faecalibacterium. As shown in Fig. 2G, genes related to lipid and carbohydrate metabolism are more enriched after transplantation.
Differences in the fecal microbiota between clinical responders and non-responders
Based on the efficacy after FMT, clinical response and non-response groups are divided. Figures 3A and 3B show the microbial composition at different classification levels. At the phylum level, compared with the non-response group, the response group had a lower abundance of Firmicutes and a higher abundance of Proteobacteria before transplantation, and the abundance of Firmicutes increased significantly and Proteobacteria decreased significantly after transplantation. At the genus level, compared with the non-response group, the response group had a higher abundance of Bacteroides and a lower abundance of Prevotella and Collinsella before transplantation. Figures 3C and 3D show the differences in some taxa between the two groups before and after transplantation at the genus level. There are significant differences in Veillonella, Neisseria, and Subdoligranulum. Using the Spearman correlation between different taxa, the co-occurrence networks of the four groups of microbes were constructed. They showed different microbial aggregation networks in different groups. Before and after FMT, the microbial interactions in the clinical non-response group were more closely related (Figs. 3E-3H). Among them, in the pre-FMT response group, Bacteroides, Veillonella, and Streptococcus are important nodes (Fig. 3E), while in the non-response group, Bacteroides, Megamonas, and Prevotella are important nodes (Fig. 3F). After FMT, Bifidobacterium and Fusobacterium are important nodes in the response group (Fig. 3G), while Prevotella, Paraprevotella, and Bacteroides are important nodes in the non-response group (Fig. 3H).
The difference of intestinal microbiota before and after FMT between clinical response group and non-response group. Box plots of microbiota abundance in two groups at different levels before and after FMT. A Phylum level. B Genus level. C Gut microbiota difference between the two groups before and after FMT were identified with a LEfSe analysis with LDA score threshold> 2.0. D The cladogram plot. Co-occurrence network analysis for the two groups before and after FMT. E Response group before FMT. F Non-response group before FMT. G Response group after FMT. H Non-response group after FMT
Discussion
In this study, 9 out of the 23 patients included were positive for CDI, which accounts for about 15-25% of AAD cases [5]. This is the most widely studied type in AAD [4]. There has been less research on other types of pathogens, which is why the clinical efficacy of FMT for AAD is lower than for CDI. However, in this study, whether there is a CDI infection does not affect the clinical efficacy of FMT for AAD. The clinical response rate for AAD patients who tested positive for CDI was 77.78% (7/9), and the clinical response rate for AAD patients who tested negative for CDI was 78.57% (11/14).
After FMT, we found significant changes in the abundance and diversity of the fecal microbiota, which has a certain correlation with the therapeutic effect of the disease. Studies have found a correlation between improvement in clinical efficacy and changes in the bacterial spectrum after FMT in patients [28, 29]. In rCDI patients who responded clinically, after FMT, there was an enrichment of Ruminococcaceae and Lachnospiraceae, a decrease in Enterobacteriaceae, more obvious colonization of donor microbiota, and alleviation of gut microbiota dysbiosis [30]. In IBS patients post-FMT, gastrointestinal symptom scores (IBS-SSS) decreased, quality of life scores (IBS-QOL) increased, dysbiosis index decreased, and 6 bacteria Alistipes, Bacteroides spp, Prevotella spp, parabobacteroides johnsonii, Firmicutes, Eubacterium biformme, and Faecalibacterium prausnitii, which were negatively correlated with the total IBS-SSS score, were identified [29]. It was also found that the changes in intestinal microbiota after FMT can predict clinical efficacy. Studies have found an index constructed based on Esherichia and Blautia after FMT can successfully predict the clinical outcomes of rCDI 8 weeks after treatment [30]. Changes in the relative abundance of Veillonella, Ruminococcaceae, Eggerthella and Lactobacillus, etc. in the short term (5 days) after treatment may be able to predict the long-term therapeutic effect of FMT on ulcerative colitis (UC) [31].
After FMT, at the genus level, Veillonella showed a significant reduction. Veillonella is a Gram-negative anaerobic coccus that can produce LPS, inducing an inflammatory response, and it is commonly seen in upper respiratory and intestinal infections. Veillonella and Streptococcus interact immunologically and often co-occur in ecosystems, suppressing the production of IL-12p70 while enhancing the response of IL-8, IL-6, IL-10, and TNF-α [32]. A study found that compared with the gut microbiota of healthy people, patients with autoimmune hepatitis (AIH) have reduced diversity and enriched genera such as Streptococcus and Veillonella [33]. In this study, the overall inflammation level of AAD patients after FMT showed a decreasing trend, which was negatively correlated with the changes in Veillonella. This is consistent with reports from other studies.
After FMT, the non-responsive group had a higher Sutturella timonensis than the responsive group. Some studies have found that Sutterella may play an important role in FMT treatment responses, where the abundance of Sutterella is negatively correlated with the remission degree of Ulcerative Colitis (UC) [34]; and in clinical cohort studies, it was found that the abundance of Sutterella is negatively correlated with the level of inflammatory cytokines (IL-12, IL-13, IFN-γ) [35]; in related experiments on AAD, high-throughput sequencing of fecal samples from 30 seven-week-old SPF male rats revealed that the relative abundance of the genus Sutterella is negatively correlated with the dose and positively correlated with the development of AAD [36]. At the same time, we found that the composition of the gut microbiota of patients before FMT is one of the main factors affecting clinical outcomes, which has been proven by numerous clinical studies [14]. For instance, in ulcerative colitis, higher fecal and mucosal microbial abundance before FMT treatment is associated with positive treatment outcomes, while the abundance of Clostridium and Sutterella is associated with FMT treatment failure [14, 34]. In Crohn’s disease, FMT failure is associated with the enrichment of different γ-Proteobacteria members (such as Klebsiella, Actinomyces, and Hemophilus) in the baseline recipient microbiota [37]. IBS patients who responded to FMT had a higher baseline abundance of streptococcal species and higher microbial diversity than non-responsive patients [38].
The limitations of this study include a small sample size and lack of controls. The fecal microbiota was only assessed using 16S rRNA sequencing, and there is a lack of related metabolomics data, so changes in metabolites related to short-chain fatty acids, bile acids, and lipids before and after FMT cannot be compared. Comprehensive microbial analysis may further deepen the understanding of the potential of precise strains and their specific functions as predictive factors for FMT success and failure. Therefore, we plan to increase the number of samples in subsequent studies, and perform metagenomic sequencing and related metabolomics sequencing on fecal samples.
Availability of data and materials
The 16S rRNA sequencing data of all participants in the study has been uploaded to the National Center for Biotechnology Information platform, with the accession number PRJNA1037722.
References
Liao W, Chen C, Wen T, et al. Probiotics for the prevention of antibiotic-associated diarrhea in adults: a Meta-analysis of randomized placebo-controlled trials. J Clin Gastroenterol. 2021;55(6):469–80.
Lukasik J, Dierikx T, Besseling-van der Vaart I, et al. Multispecies probiotic for the prevention of antibiotic-associated diarrhea in children: a randomized clinical trial. JAMA Pediatr. 2022;176(9):860–6.
McFarland LV. Antibiotic-associated diarrhea: epidemiology, trends and treatment. Future Microbiol. 2008;3(5):563–78.
Young VB, Schmidt TM. Antibiotic-associated diarrhea accompanied by large-scale alterations in the composition of the fecal microbiota. J Clin Microbiol. 2004;42(3):1203–6.
Bartlett JG. Clinical practice. Antibiotic-associated diarrhea. N Engl J Med. 2002;346(5):334–9.
Dunne C. Adaptation of bacteria to the intestinal niche: probiotics and gut disorder. Inflamm Bowel Dis. 2001;7(2):136–45.
Högenauer C, Hammer HF, Krejs GJ, et al. Mechanisms and management of antibiotic-associated diarrhea. Clin Infect Dis. 1998;27(4):702–10.
Cummings JH, Pomare EW, Branch WJ, et al. Short chain fatty acids in human large intestine, portal, hepatic and venous blood. Gut. 1987;28(10):1221–7.
Scheppach W, Müller JG, Boxberger F, et al. Histological changes in the colonic mucosa following irrigation with short-chain fatty acids. Eur J Gastroenterol Hepatol. 1997;9(2):163–8.
Topping DL, Clifton PM. Short-chain fatty acids and human colonic function: roles of resistant starch and nonstarch polysaccharides. Physiol Rev. 2001;81(3):1031–64.
Hill C, Guarner F, Reid G, et al. Expert consensus document. The international scientific Association for Probiotics and Prebiotics consensus statement on the scope and appropriate use of the term probiotic. Nat Rev Gastroenterol Hepatol. 2014;11(8):506–14.
Vindigni SM, Surawicz CM. Fecal microbiota transplantation. Gastroenterol Clin North Am. 2017;46(1):171–85.
Dai M, Liu Y, Chen W, et al. Rescue fecal microbiota transplantation for antibiotic-associated diarrhea in critically ill patients. Crit Care. 2019;23(1):324.
Danne C, Rolhion N, Sokol H. Recipient factors in faecal microbiota transplantation: one stool does not fit all. Nat Rev Gastroenterol Hepatol. 2021;18(7):503–13.
van Nood E, Vrieze A, Nieuwdorp M, et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med. 2013;368(5):407–15.
Hvas CL, Dahl Jørgensen SM, Jørgensen SP, et al. Fecal microbiota transplantation is superior to Fidaxomicin for treatment of recurrent Clostridium difficile infection. Gastroenterology. 2019;156(5):1324–1332.e1323.
Cammarota G, Masucci L, Ianiro G, et al. Randomised clinical trial: faecal microbiota transplantation by colonoscopy vs. vancomycin for the treatment of recurrent Clostridium difficile infection. Aliment Pharmacol Ther. 2015;41(9):835–43.
Cui J, Lin Z, Tian H, et al. Long-term follow-up results of fecal microbiota transplantation for irritable bowel syndrome: a single-center. Retros Study Front Med. 2021;8:710452.
Tian H, Ge X, Nie Y, et al. Fecal microbiota transplantation in patients with slow-transit constipation: a randomized, clinical trial. PloS One. 2017;12(2):e0171308.
Bolyen E, Rideout JR, Dillon MR, et al. Reproducible, interactive, scalable and extensible microbiome data science using QIIME 2[J]. Nat Biotechnol. 2019;37(8):852–7.
Callahan BJ, McMurdie PJ, Rosen MJ, et al. DADA2: high-resolution sample inference from Illumina amplicon data. Nat Methods. 2016;13(7):581–3.
Segata N, Izard J, Waldron L, et al. Metagenomic biomarker discovery and explanation. Genome Biol. 2011;12(6):R60.
Douglas GM, Maffei VJ, Zaneveld JR, et al. PICRUSt2 for prediction of metagenome functions. Nat Biotechnol. 2020;38(6):685–8.
Kanehisa M, Goto S, Sato Y, et al. KEGG for integration and interpretation of large-scale molecular data sets. Nucleic Acids Res. 2012;40(Database issue):D109–14.
Kanehisa M, Goto S. KEGG: Kyoto encyclopedia of genes and genomes. Nucleic Acids Res. 2000;28(1):27–30.
Kanehisa M. Toward understanding the origin and evolution of cellular organisms. Protein Sci. 2019;28(11):1947–51.
Kanehisa M, Furumichi M, Sato Y, et al. KEGG for taxonomy-based analysis of pathways and genomes. Nucleic Acids Res. 2023;51(D1):D587–d592.
El-Salhy M, Hatlebakk JG, Gilja OH, et al. Efficacy of faecal microbiota transplantation for patients with irritable bowel syndrome in a randomised, double-blind, placebo-controlled study. Gut. 2020;69(5):859–67.
El-Salhy M, Winkel R, Casen C, et al. Efficacy of fecal microbiota transplantation for patients with irritable bowel syndrome at 3 years after transplantation. Gastroenterology. 2022;163(4):982–994.e914.
Wei S, Bahl MI, Baunwall SMD, et al. Gut microbiota differs between treatment outcomes early after fecal microbiota transplantation against recurrent Clostridioides difficile infection. Gut Microbes. 2022;14(1):2084306.
Li Q, Ding X, Liu K, et al. Fecal microbiota transplantation for ulcerative colitis: the optimum timing and gut microbiota as predictors for long-term clinical outcomes. Clin Transl Gastroenterol. 2020;11(8):e00224.
van den Bogert B, Meijerink M, Zoetendal EG, et al. Immunomodulatory properties of Streptococcus and Veillonella isolates from the human small intestine microbiota. PloS One. 2014;9(12):e114277.
Goeser F, Münch P, Lesker TR, et al. Neither black nor white: do altered intestinal microbiota reflect chronic liver disease severity? Gut. 2021;70(2):438–40.
Paramsothy S, Nielsen S, Kamm MA, et al. Specific Bacteria and metabolites associated with response to fecal microbiota transplantation in patients with ulcerative colitis. Gastroenterology. 2019;156(5):1440–1454.e1442.
Kaakoush NO. Sutterella species, IgA-degrading Bacteria in ulcerative colitis. Trends Microbiol. 2020;28(7):519–22.
Lv W, Liu C, Ye C, et al. Structural modulation of gut microbiota during alleviation of antibiotic-associated diarrhea with herbal formula. Int J Biol Macromol. 2017;105(Pt 3):1622–9.
Sokol H, Landman C, Seksik P, et al. Fecal microbiota transplantation to maintain remission in Crohn's disease: a pilot randomized controlled study. Microbiome. 2020;8(1):12.
Holvoet T, Joossens M, Wang J, et al. Assessment of faecal microbial transfer in irritable bowel syndrome with severe bloating. Gut. 2017;66(5):980–2.
Acknowledgements
Not applicable.
Funding
This research was funded by the following two projects, which are respectively Shanghai Action Plan on Science Technology and Innovation 21Y11908300, and National Key R&D Program of China, 2022YFA1304101.
Author information
Authors and Affiliations
Contributions
Le Wang designed the whole project and wrote the main manuscript text , and Gongjing Guo revised the manuscript, and Yue Xu analyzed the microbiota data, and Long Li provided the design ideas, and Bo Yang and Di Zhao provided the sample information, and Hongliang Tian, Chen Ye, Zhiliang Lin and Jiaqu Cui collected information and samples from patients, Long Huang, Ning Li and Qiyi Chen supervised and revised the entire study.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethical Committee of Shanghai Tenth Hospital affliated to Tongji University with the ethical approval number SHSY-IEC-4.1/20-116/01. All participating patients signed an informed consent form.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, L., Guo, G., Xu, Y. et al. The effect of fecal microbiota transplantation on antibiotic-associated diarrhea and its impact on gut microbiota. BMC Microbiol 24, 160 (2024). https://doi.org/10.1186/s12866-024-03261-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12866-024-03261-0