Abstract
Background
Camels harbouring multidrug-resistant Gram-negative bacteria are capable of transmitting various microorganisms to humans. This study aimed to determine the distribution of anti-microbial resistance among Escherichia coli (E. coli) isolated from the feces of apparently healthy camels in Egyptian abattoirs. Additionally, we sought to characterize Shiga toxin-producing E. coli (STEC) strains, assess their virulence potential, and investigate the possibility of camels spreading carbapenem- and colistin-resistant E. coli.
Methods
121 fecal swaps were collected from camels in different abattoirs in Egypt. Isolation and identification of E. coli were performed using conventional culture techniques and biochemical identification. All isolates obtained from the examined samples underwent genotyping through polymerase chain reaction (PCR) of the Shiga toxin-encoding genes (Stx1 and Stx2), the carbapenemase-encoding genes (blaKPC, blaOXA−48, blaNDM, and blaVIM), and the mcr genes for mcr-1 to mcr-5.
Result
Bacteriological examination revealed 75 E. coli isolates. PCR results revealed that one strain (1.3%) tested positive for Stx1, and five (6.6%) were positive for Stx2. Among the total 75 strains of E. coli, the overall prevalence of carbapenemase-producing E. coli was 27, with 7 carrying blaOXA48, 14 carrying blaNDM, and 6 carrying blaVIM. Notably, no strains were positive for blaKPC but a high prevalence rate of mcr genes were detected. mcr-1, mcr-2, mcr-3, and mcr-4 genes were detected among 3, 2, 21, and 3 strains, respectively.
Conclusion
The results indicate that camels in Egypt may be a primary source of anti-microbial resistance (AMR) E. coli, which could potentially be transmitted directly to humans or through the food chain.
Similar content being viewed by others
Background
Camels play a vital role in the socioeconomic growth of many nations, particularly in Africa and the Middle East [1]. They provide essential resources and services that benefit local communities and economies, such as milk and meat production, transportation, and entertainment, particularly in Egypt’s tourism sector [2].
The impact of climate change and the rise in drought conditions have shifted livestock preferences in various regions worldwide, leading to a notable increase in the abundance of camels [3].
Camels in sub-Saharan Africa serve as a reservoir for various potentially zoonotic diseases and pathogens [4]. Carcass microbiological contamination primarily occurs during processing and handling stages, such as skinning, evisceration, preparation, storage, and distribution at abattoirs and retail shops [5].
Escherichia coli, or E. coli, is a rod-shaped bacterium in the intestinal tracts of humans and warm-blooded animals. While many strains of E. coli are harmless and coexist naturally, certain strains, such as Shiga toxin-E. coli (STEC), can result in foodborne illnesses. Some E. coli strains can also cause infections in the urinary and respiratory systems and other diseases [6].
In contrast, STEC in camels, capable of causing gastrointestinal illnesses such as non-bloody or bloody diarrhoea, haemorrhagic colitis (HC), and haemolytic uremic syndrome (HUS), has been rarely documented. However, STEC is responsible for approximately 2,801,000 cases of acute illnesses each year, posing a substantial global health burden [7].
E. coli produces numerous highly virulent genes, with Shiga toxin-producing E. coli (STEC) being the most significant serotype regarding public health toxins. The virulence factors of STEC are primarily derived from Shiga toxin genes (Stx1 and Stx2), which play a significant role in the manifestation of clinical symptoms [8]. Furthermore, Stx1 and Stx2 can have sequence variants, and a single STEC bacterium can produce multiple variants of these toxins [9].
The primary mode of transmission of STEC to humans is through consuming contaminated foods, including raw or undercooked ground meat products and unpasteurized milk. Additionally, cross-contamination during food preparation is another significant mode. Hand-to-mouth transfer involving direct contact with farm animals is also identified as a substantial transmission mode [10].
Antibiotic resistance (AMR) poses a significant threat to human and animal health, making the treatment of bacterial infections increasingly challenging. One of the essential AMR mechanisms in the Enterobacteriaceae family involves the production of extended-spectrum β-lactamases (ESBLs) and metallo-β-lactamases (MBLs), which can inactivate a wide range of antibiotics, including carbapenems, considered last-line therapies [11].
Gram-negative bacteria can resist antibiotics in several ways, such as by producing enzymes that destroy antibiotics, making it harder for antibiotics to enter the cell, or changing the cell membrane’s structure to prevent antibiotic penetration. These changes have been seen in many bacteria resistant to multiple drugs [12].
Carbapenems, important in human medicine as broad-spectrum beta-lactam antibiotics, are considered the last-line therapies for severe infections. The five most crucial carbapenemase enzymes are KPC, NDM, IMP, VIM, and OXA. These enzymes can break down carbapenems, conferring antibiotic resistance [13].
E. coli can resist many different types of antibiotics; the most common is beta-lactam resistance, including cephalosporins, aminoglycosides, and tetracyclines. E. coli achieves this by producing enzymes called beta-lactamases associated with genes such as blaTEM and blaCTX, which code for beta-lactamases [14].
Colistin, a potent antibiotic used in treating severe infections and often considered a last-resort antibiotic, faces the challenge of resistance, which can spread to other bacteria through mobile genetic elements, rapidly spreading this resistance within bacterial populations. A plasmid known as mcr-1, capable of transmitting colistin resistance to other bacteria [15, 16], can also be found on plasmids carrying other antibiotic-resistance genes, including those encoding carbapenemases and extended-spectrum beta-lactamases [17]. Many studies have demonstrated that using colistin as an antibiotic growth promoter (AGP) in livestock contributes to the emergence and spread of plasmid genes, conferring resistance to polymyxins, including colistin itself [18].
This study aimed to update our understanding of the prevalence of E. coli bacteria in camels in Egypt, characterize the strains of E. coli causing STEC infections, assess the potential of camels to spread E. coli bacteria resistant to carbapenem and colistin antibiotics, and evaluate the potential risk to human and animal health arising from the transmission of these strains to the environment.
Methods
Sample preparation: A total of 121 faecal swaps were collected from camels aged 3–5 years in different abattoirs in Cairo and Giza governorates (Al Waraq and Al Basateen abattoirs) during the period from January 2022 to June 2022. Subsequently, the swabs were placed in 2 ml of sterile saline (0.9% NaCl) and stored in an ice box until transported to the laboratory.
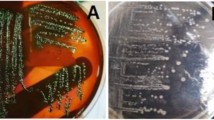
Bacterial isolation and identification: All samples were inoculated into brain-heart infusion broth tubes and incubated at 37 °C for 24 h. A loopful from the previously incubated tubes was streaked on eosin methylene blue agar (EMB) and incubated aerobically at 37 °C for 24–48 h. Suspected colonies were purified through subculture on EMB agar plates and subjected to traditional biochemical tests, including indole, methyl red, Voges-Proskauer, citrate utilization, and urease tests [19]. The isolates were stored at − 20 °C until further molecular analysis.
Molecular detection of virulence and antibiotic resistance genes in E. coli: All isolates obtained from the examined samples underwent genotyping using polymerase chain reaction (PCR), according to the protocol described by [20]. The template DNA used consisted of boiled lysates prepared from the isolates. In brief, a loopful of culture was suspended in 100 µl of sterile TE buffer, boiled for 10 min at 100 °C, and centrifuged for 5 min at 6000×g. The extracted DNA was stored at -20 °C until use.
All genomic DNA of the identified E. coli strains underwent PCR testing for Shiga toxin-encoding genes (Stx1 and Stx2) using multiplex PCR assays. The target genes, oligonucleotide primer sequences, and the expected product size in different PCR assays are outlined in Table 1.
To detect the carbapenemase-encoding genes (blaKPC, blaOXA−48, blaNDM, and blaVIM), multiplex PCR was performed using specific oligonucleotide primers for detecting blaKPC and blaNDM (Table 2). The PCR mixtures had a total reaction volume of 25 mL. All reaction mixtures were subjected to 30 cycles at 94 °C for 1 min, 55 °C for 1 min, and 72 °C for 2 min. Subsequently, 5 mL of the PCR product was electrophoresed on a 1% agarose gel to determine the size of the product [21]. Uniplex PCR was also conducted using a specific oligonucleotide primer to detect blaVIM (Table 2). The PCR mixtures had a total reaction volume of 25 mL. All reaction mixtures were subjected to 35 cycles at 94 ºC for 30 s, 55 ºC for 30 s, 72ºC for 1 min, and a final elongation at 72 ºC for 10 min. Then, 5 mL of the PCR product was electrophoresed on a 1% agarose gel to determine the size of the product [22].
The plasmid DNA served as the template for PCR. The primer pair used to detect the blaOXA−48 gene consisted of blaOXA−48 F(5ʹ-GCTTGATCGCCCTCGATT-3ʹ) and blaOXA−48 R (3ʹ-GATTTGCTCCGTGGCCGAAA-5ʹ). The thermal cycling process consisted of initial denaturation at 94 °C for 10 min, denaturation at 94 °C for 40 s, annealing at 60 °C for 40 s, extension at 72 °C for 1 min, and a final extension at 72 °C for 7 min. In total, 30 cycles were run. The amplified products were then subjected to gel electrophoresis [22].
Multiplex PCR was also performed using oligonucleotide primers for mcr-1 to mcr-5 (Table 3). The PCR conditions included denaturation at 94 °C for 5 min, followed by 25 cycles of denaturation at 94 °C for 30 s, annealing at 58 °C for 90 s, elongation at 72 °C for 60 s, and a final cycle of elongation at 72 °C for 10 min.
Results
Isolation and identification of E. coli strains:
The bacteriological examination of 121 camels’ faecal swaps showed the presence of 75 E. coli isolates (Table 4). Using multiplex PCR for the detection of Shiga toxin-encoding genes (Stx1 and Stx2) (Table 5), one E. coli strain (1.3%) tested positive for Stx1, and five strains (6.6%) were positive for Stx2.
Molecular findings of virulence and antibiotic resistance genes in E. coli:
In Table 5, the total prevalence of carbapenemase-producing E. coli was 27 strains: 7 carrying blaOXA−48, 14 carrying blaNDM, and 6 carrying blaVIM, while no strain carried blaKPC. Additionally, the total prevalence of colistin resistance genes in E. coli isolates was 29 strains, with mcr-1, mcr-2, mcr-3, mcr-4, and mcr-5 being 3, 2, 21, 3, and 0, respectively.
Discussion
Camels are susceptible to several infectious diseases, meaning eating camel meat or coming into contact with camels can pose a significant risk of zoonotic disease transmission [23]. In this study (Table 4), special consideration aligns with Jones et al. [24], who concluded that eating raw camel meat often leads to outbreaks of diarrheagenic E. coli, a type of bacteria that can cause diarrhea. This typically occurs due to rough handling procedures during slaughter and transportation. Additionally, many countries worldwide have reported a high incidence of pathogenic E. coli strains in fresh camel milk [25].
STEC is a type of bacteria that can cause food poisoning. It is a zoonotic pathogen responsible for mild to severe diarrhea, hemorrhagic colitis (bloody diarrhea), and hemolytic uremic syndrome (HUS) [26]. The distinguishing feature of STEC is the presence of one or more Shiga toxin (Stx) genes, which code for proteins that can damage the cells in the lining of the intestines. There are two main types of Shiga toxins: Stx1 and Stx2 [27].
Most E. coli bacteria live in the intestines of humans and animals without causing any harm. However, some E. coli bacteria produce toxins, leading to food poisoning. STEC infections are most common in ruminants. These animals can carry STEC bacteria in their intestines without getting sick. However, these bacteria can be spread to people through food or water contaminated with animal feces [28, 29]. This transmission occurs because the lining of their intestines lacks vascular receptors, preventing the toxins from being absorbed into the bloodstream and transported to other organs. As a result, the STEC bacteria can colonize the large intestine without causing symptoms [30].
The prevalence of Shiga toxin-encoding genes (Stx1 and Stx2) detected in this study was closely consistent with those reported by Erickson and Doyle [31] and Kintz et al. [32]. These studies focused on uncovering the source and transmission of STEC infections in the food chain and humans.
STEC can be transmitted to humans in several ways, including eating undercooked ground beef or other raw foods, such as lettuce, sprouts, or spinach, from manured gardens, drinking contaminated water or unpasteurized milk or juice, coming into direct contact with animal feces, or being infected with STEC [33].
Extended-spectrum beta-lactamase (ESBL)-producing Enterobacteriaceae (ESBL-E) are bacteria equipped with enzymes that can break down a wide range of beta-lactam antibiotics, including penicillin and cephalosporins. However, they are not resistant to carbapenem antibiotics [34]. ESBL-E bacteria pose a serious public health threat as they can be difficult or impossible to treat, leading to more extended hospital stays, more severe illnesses, and even death [35]. Infections caused by ESBL-producing Enterobacteriaceae (ESBL-E) are concerning for various reasons, including increased hospital costs, length of hospital stays, and mortality rates. ESBL-E infections can also be more deadly than other infections, necessitating treatment with last-resort antibiotics like carbapenems [36]. Recently, the effectiveness of carbapenems has been disposed of globally by the emergence of carbapenem-resistant bacteria. The resistance of Enterobacteriaceae to carbapenems includes numerous mechanisms, the most significant being the production of carbapenemases.
In Table 5, the prevalence of carbapenemase-producing E. coli was 27 strains: 7 carried blaOXA, 14 carried blaNDM, and 6 carried blaVIM, while no strain carried blaKPC. This result agrees with Tzouvelekis et al. [37], who concluded that the clinical intake of carbapenems has increased, leading to a rise in the number of pathogen isolates producing carbapenemases. The increased prevalence of bacterial species carrying ESBL genes, as reported worldwide, included community-acquired Escherichia coli isolates with the ability to produce ESBLs [38]. Moreover, this result agrees with Cantón et al. [39], who discussed that KPC, OXA, and NDM involve three of the ‘big five’ carbapenemases associated with nosocomial contagions. The global increase in carbapenemase-producing Enterobacteriaceae (CPE) has led to the overuse of colistin. This overuse has raised concerns about the emergence of colistin resistance (mcr) genes in bacteria [40], which are already resistant to many other antibiotics. Additionally, data on colistin-resistant E. coli and mcr genes in camels are lacking. Given the increasing use of camels for meat and milk production, this is a concern, raising the possibility that camels play a role in transmitting colistin-resistant bacteria to humans.
the present study showed a surprising occurrence of mcr genes in E. coli isolates where the total prevalence of colistin resistance genes in E. coli isolates was 29 (Table 5) and these findings was much higher than those obtained by Rhouma et al., who found no colistin resistance in E. coli isolated from camel feces in southern Tunisia [41].
Veterinarians working with camels face a significant challenge because there is no approved anti-microbial to treat bacterial infections in these animals. Anti-microbials approved for ruminants, horses, or other animal species to treat sick camels have proven ineffective due to the unique physiology of camels [42].
In a recent study in Egypt, Kamel et al. [43] investigated carbapenem-resistant Gram-negative bacteria isolated from febrile paediatric cancer patients from October 2014 to December 2016. The study revealed that blaOXA−48 was the most ubiquitous carbapenemase gene (58.62%), followed by blaNDM (27.58%), blaVIM (10.3%), and blaKPC (6.89%).
Evidence shows that camels could be a significant source of mcr gene contamination for Egypt’s local population and tourists. This is because camels and tourists often come into close contact, potentially spreading resistant bacteria globally.
New plasmid-mediated mcr genes have rapidly emerged in the past four years, compromising the therapeutic effectiveness of colistin, a last-resort antibiotic used to treat multidrug-resistant bacterial infections [44].
The mcr-1 and mcr-2 genes have engrossed worldwide consideration, heralding the polymyxin gap. However, in this study, the mcr-3 gene exhibited a prevalence of 28% compared with the mcr-1, mcr-2, mcr-4, and mcr-5 genes, which had prevalence rates of 4%, 2.6%, 45%, and 0%, respectively. These results agree with Yin et al. [45], who examined a colistin-resistant Escherichia coli isolate. The study yielded negative results for mcr-1 and mcr-2 and discovered a novel mcr-3. They found wide-ranging mcr-3 between Enterobacteriaceae and Aeromonas species initiating from clinical infections and environmental specimens across twelve countries on four continents.
E. coli, normal inhabitants of the intestines of humans and mammals, potentially represent a significant reservoir of AMR and play a vital role in gaining and propagating AMR mechanisms. Since colistin is widely used in veterinary medicine and is increasing in use in human medicine, it is crucial to continuously monitor the spread of mcr genes in both the agricultural and healthcare sectors. This can be achieved by tracking the presence of mobile colistin resistance determinants in colistin-resistant Gram-negative bacteria [46].
Conclusion
STEC is a significant foodborne zoonotic bacterium, and camels may play a role in transmitting E. coli, which resists many antibiotics to humans. These results recommend the need for careful veterinary practice of beta-lactams in the camel industry. For the first time in Egypt, camels could become a source of the mcr-3 gene. Therefore, the search for the mcr-3 gene should be immediately encompassed in investigating colistin-resistant Gram-negative bacteria from animals, humans, and the environment.
Data availability
No datasets were generated or analysed during the current study.
References
Ashour R, Hamza D, Kadry M, Sabry MA. The Surveillance of Borrelia species in Camelus dromedarius and Associated ticks: the first detection of Borrelia miyamotoi in Egypt. Veterinary Sci. 2023;10(2):141.
Ashour R, Hamza D, Kadry M, Sabry MA. Molecular detection of Babesia microti in dromedary camels in Egypt. Trop Anim Health Prod. 2023;55(2):91.
Watson EE, Kochore HH, Dabasso BH. Camels and climate resilience: adaptation in northern Kenya. Hum Ecol. 2016;44(6):701–13.
Baschera M, Cernela N, Stevens MJ, Liljander A, Jores J, Corman VM, Nüesch-Inderbinen M, Stephan R. Shiga toxin-producing Escherichia coli (STEC) isolated from fecal samples of African dromedary camels. One Health. 2019;7:100087.
Aynewa D, Gizaw Z, Haile AF. Assessment of bacteriological quality of sheep carcasses, effect level of 2.5% citric acid spray on bacterial contamination of meat, and hygiene practices of workers in a selected abattoir in Debrezeit town, central Ethiopia. Environ Health Insights. 2021;15:11786302211037555.
Lim JY, Yoon JW, Hovde CJ. A brief overview of Escherichia coli O157: H7 and its plasmid O157. J Microbiol Biotechnol. 2010;20(1):5.
Karch H, Tarr PI, Bielaszewska M. Enterohaemorrhagic Escherichia coli in human medicine. Int J Med Microbiol. 2005;295(6–7):405–18.
WHO. E. coli. 2018. Available via https://www.who.int/news-room/fact-sheets/detail/E-Coli [Ref list] /fact-sheets/detail/E-Coli [Ref list].
Sandvig K. The Shiga toxins: Properties and action on cells. Compr Sourceb Bacterial Protein Toxins. 2005;20:310–22.
Hunt JM. Shiga toxin–producing Escherichia coli (STEC). Clin Lab Med. 2010;30(1):21–45.
Kadry M, Nader SM, Elshafiee EA, Ahmed ZS. Molecular characterization of ESBL and Carbapenenemase Producing Salmonella spp. Isolated from Chicken and its Public Health Importance. Pakistan J Zool. 2021; 1;53(6).
Elshafiee EA, Kadry M, Nader SM, Ahmed ZS. Extended-spectrum-beta-lactamases and carbapenemase-producing Klebsiella pneumoniae isolated from fresh produce farms in different governorates of Egypt. Veterinary World. 2022;15(5):1191.
Munoz-Price LS, Poirel L, Bonomo RA, Schwaber MJ, Daikos GL, Cormican M, Cornaglia G, Garau J, Gniadkowski M, Hayden MK, Kumarasamy K. Clinical epidemiology of the global expansion of Klebsiella pneumoniae carbapenemases. Lancet Infect Dis. 2013;13(9):785–96.
Hammad AM, Eltahan A, Hassan HA, Abbas NH, Hussien H, Shimamoto T. Loads of coliforms and fecal coliforms and characterization of thermotolerant Escherichia coli in fresh raw milk cheese. Foods. 2022;11(3):332.
Ahmed ZS, Elshafiee EA, Khalefa HS, Kadry M, Hamza DA. Evidence of colistin resistance genes (mcr-1 and mcr-2) in wild birds and its public health implication in Egypt. Anti-microbial Resist Infect Control. 2019;8(1):1–8.
Liu YY, Wang Y, Walsh TR, Yi LX, Zhang R, Spencer J, Doi Y, Tian G, Dong B, Huang X, Yu LF. Emergence of plasmid-mediated colistin resistance mechanism MCR-1 in animals and human beings in China: a microbiological and molecular biological study. Lancet Infect Dis. 2016;16(2):161–8.
Zhang XF, Doi Y, Huang X, Li HY, Zhong LL, Zeng KJ, Zhang YF, Patil S, Tian GB. Possible transmission of mcr-1–harboring Escherichia coli between companion animals and human. Emerg Infect Dis. 2016;22(9):1679.
Dominguez JE, Redondo LM, Figueroa Espinosa RA, Cejas D, Gutkind GO, Chacana PA, Di Conza JA, Fernández Miyakawa ME. Simultaneous carriage of mcr-1 and other anti-microbial resistance determinants in Escherichia coli from poultry. Front Microbiol. 2018;9:1679.
Bhutia MO, Thapa N, Tamang JP. Molecular characterization of bacteria, detection of enterotoxin genes, and screening of antibiotic susceptibility patterns in traditionally processed meat products of Sikkim, India. Front Microbiol. 2021;11:599606.
Reischl U, Pulz M, Ehret W, Wolf HJ. PCR-based detection of mycobacteria in sputum samples using a simple and reliable DNA extraction protocol. Biotechniques. 1994;17(5):844–5.
Fan LC, Lu HW, Cheng KB, Li HP, Xu JF. Evaluation of PCR in bronchoalveolar lavage fluid for diagnosis of Pneumocystis Jirovecii pneumonia: a bivariate meta-analysis and systematic review. PLoS ONE. 2013;8(9):e73099.
Delidow BC, Lynch JP, Peluso JJ, White BA. Polymerase chain reaction: basic protocols. PCR protocols: current methods and applications. 1993:1–29.
Zhu S, Zimmerman D, Deem SL. A review of zoonotic pathogens of dromedary camels. EcoHealth. 2019;16:356–77.
Jones G, Lefèvre S, Donguy MP, Nisavanh A, Terpant G, Fougère E, Vaissière E, Guinard A, Mailles A, de Valk H, Fila M. Outbreak of Shiga toxin-producing Escherichia coli (STEC) O26 paediatric haemolytic uraemic syndrome (HUS) cases associated with the consumption of soft raw cow’s milk cheeses, France, March to May 2019. Eurosurveillance. 2019;24(22):1900305.
Bottichio L, Keaton A, Thomas D, Fulton T, Tiffany A, Frick A, Mattioli M, Kahler A, Murphy J, Otto M, Tesfai A. Shiga toxin–producing Escherichia coli infections associated with romaine lettuce—United States, 2018. Clin Infect Dis. 2020;71(8):e323–30.
Joseph A, Cointe A, Mariani Kurkdjian P, Rafat C, Hertig A. Shiga toxin-associated hemolytic uremic syndrome: a narrative review. Toxins. 2020;12(2):67.
Carvalho I, Tejedor-Junco MT, González-Martín M, Corbera JA, Silva V, Igrejas G, Torres C, Poeta P. Escherichia coli producing extended-spectrum β-lactamases (ESBL) from domestic camels in the Canary Islands: a one health approach. Animals. 2020;10(8):1295.
Ferens WA, Hovde CJ. Escherichia coli O157: H7: animal reservoir and sources of human infection. Foodborne Pathog Dis. 2011;8(4):465–87.
Gyles CL. Shiga toxin-producing Escherichia coli: an overview. J Anim Sci. 2007;85(suppl13):E45–62.
Nguyen Y, Sperandio V. Enterohemorrhagic E. Coli (EHEC) pathogenesis. Front Cell Infect Microbiol. 2012;2:90.
Erickson MC, Doyle MP. Food as a vehicle for transmission of Shiga toxin–producing Escherichia coli. J Food Prot. 2007;70(10):2426–49.
Kintz E, Brainard J, Hooper L, Hunter P. Transmission pathways for sporadic shiga-toxin producing E. Coli infections: a systematic review and meta-analysis. Int J Hyg Environ Health. 2017;220(1):57–67.
Fontaine O, Griffin P, Henao O. Diarrhea, acute. In: Heymann D.L., editor. Control of communicable diseases manual. 19th edition. American Public Health Association; Washington, DC: 2008; 179–195.
Castanheira M, Simner PJ, Bradford PA. Extended-spectrum β-lactamases: an update on their characteristics, epidemiology and detection. JAC-antimicrobial Resist. 2021;3(3):dlab092.
Paterson DL, Bonomo RA. Extended-spectrum β-lactamases: a clinical update. Clin Microbiol Rev. 2005;18(4):657–86.
Legese MH, Weldearegay GM, Asrat D. Extended-spectrum beta-lactamase-and carbapenemase-producing Enterobacteriaceae among Ethiopian children. Infection and drug resistance. 2017 Jan 25:27–34.
Tzouvelekis LS, Markogiannakis A, Psichogiou M, Tassios PT, Daikos GL. Carbapenemases in Klebsiella pneumoniae and other Enterobacteriaceae: an evolving crisis of global dimensions. Clin Microbiol Rev. 2012;25(4):682–707.
Blair JM, Webber MA, Baylay AJ, Ogbolu DO, Piddock LJ. Molecular mechanisms of antibiotic resistance. Nat Rev Microbiol. 2015;13(1):42–51.
Cantón R, Ruiz-Garbajosa P. Co-resistance: an opportunity for the bacteria and resistance genes. Curr Opin Pharmacol. 2011;11(5):477–85.
Liu YY, Wang Y, Walsh TR, Yi LX, Zhang R, Spencer J, Yu LF. Emergence of plasmid-mediated colistin resistance mechanism mcr-1 in animals and human beings in China: a microbiological and molecular biological study. Lancet Infect Dis. 2016;16:161–8.
Rhouma M, Bessalah S, Salhi I, Thériault W, Fairbrother JM, Fravalo P. Screening for fecal presence of colistin-resistant Escherichia coli and mcr-1 and mcr-2 genes in camel-calves in southern Tunisia. Acta Vet Scand. 2018;60(1):1–5.
Fadlelmula A, Al-Hamam NA, Al-Dughaym AM. A potential camel reservoir for extended-spectrum β-lactamase-producing Escherichia coli causing human infection in Saudi Arabia. Trop Anim Health Prod. 2016;48:427–33.
Kamel NA, El-Tayeb WN, El-Ansary MR, Mansour MT, Aboshanab KM. Phenotypic screening and molecular characterization of carbapenemase-producing Gram-negative bacilli recovered from febrile neutropenic pediatric cancer patients in Egypt. PLoS ONE. 2018;13(8):e0202119.
Ling Z, Yin W, Shen Z, Wang Y, Shen J, Walsh TR. Epidemiology of mobile colistin resistance genes mcr-1 to mcr-9. J Anti-microbial Chemother. 2020;75(11):3087–95.
Yin W, Li H, Shen Y, Liu Z, Wang S, Shen Z, Zhang R, Walsh TR, Shen J, Wang Y. Novel plasmid-mediated colistin resistance gene mcr-3 in Escherichia coli. MBio. 2017;8(3):10–28.
Rolain JM. Food and human gut as reservoirs of transferable antibiotic resistance encoding genes. Front Microbiol. 2013;4:173.
Müller D, Greune L, Heusipp G, Karch H, Fruth A, Tschäpe H, Schmidt MA. Identification of unconventional intestinal pathogenic Escherichia coli isolates expressing intermediate virulence factor profiles by using a novel single-step multiplex PCR. Appl Environ Microbiol. 2007;73(10):3380–90.
Gannon VP, King RK, Kim JY, Thomas EJ. Rapid and sensitive method for detection of Shiga-like toxin-producing Escherichia coli in ground beef using the polymerase chain reaction. Appl Environ Microbiol. 1992;58(12):3809–15.
Li B, Yi Y, Wang Q, Woo PC, Tan L, Jing H, Gao GF, Liu CH. Analysis of drug resistance determinants in Klebsiella pneumoniae isolates from a tertiary-care hospital in Beijing, China.
Dallenne C, Da Costa A, Decré D, Favier C, Arlet G. Development of a set of multiplex PCR assays for the detection of genes encoding important β-lactamases in Enterobacteriaceae. J Anti-microbial Chemother. 2010;65(3):490–5.
Li J, Hu Z, Hu Q. Isolation of the first IMP-4 metallo-β-lactamase producing Klebsiella pneumoniae in Tianjin, China. Brazilian J Microbiol. 2012;43:917–22.
Rebelo AR, Bortolaia V, Kjeldgaard JS, Pedersen SK, Leekitcharoenphon P, Hansen IM, Guerra B, Malorny B, Borowiak M, Hammerl JA, Battisti A. Multiplex PCR for detection of plasmid-mediated colistin resistance determinants, mcr-1, mcr-2, mcr-3, mcr-4 and mcr-5 for surveillance purposes. Eurosurveillance. 2018;23(6):17–00672.
Acknowledgements
The authors would like to express their sincere gratitude to all the slaughterhouse workers in the Egyptian abattoirs who participated in the study. Their kind cooperation made it possible to collect the necessary samples, and their contributions are greatly appreciated.
Funding
The authors declare that they received no funding or grants for this study.
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
MY, FK, MK and RE performed the collection of samples, the molecular detection of the target genes. MY, FK, MK, RE and ME performed the analysis and interpretation of the data and the writing of the manuscript. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The sample collection protocol adhered to the Institutional Animal Care and Use Committee (IACUC) guidelines of the Faculty of Veterinary Medicine, Cairo University, Egypt (VetCU08072023707). All experimental protocols were approved by the Institutional Animal Care and Use Committee (IACUC) of the Faculty of Veterinary. Medicine, Cairo University, Egypt.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
youseef, M., Karam, F., Kadry, M. et al. Escherichia coli and their potential transmission of carbapenem and colistin-resistant genes in camels. BMC Microbiol 24, 65 (2024). https://doi.org/10.1186/s12866-024-03215-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12866-024-03215-6