Abstract
Background
Cutaneous Leishmaniasis (CL) is a parasitic disease with diverse outcomes. Clinical diversity is influenced by various factors such as Leishmania species and host genetic background. The role of Leishmania RNA virus (LRV), as an endosymbiont, is suggested to not only affect the pathogenesis of Leishmania, but also impact host immune responses. This study aimed to investigate the influence of LRV2 on the expression of a number of virulence factors (VFs) of Leishmania and pro-inflammatory biomarkers.
Materials and methods
Sample were obtained from CL patients from Golestan province. Leishmania species were identified by PCR (LIN 4, 17), and the presence of LRV2 was checked using the semi-nested PCR (RdRp gene). Human monocyte cell line (THP-1) was treated with three isolates of L. major with LRV2 and one isolate of L. major without LRV2. The treatments with four isolates were administered for the time points: zero, 12, 24, 36, and 48 h after co-infection. The expression levels of Leishmania VFs genes including GP63, HSP83, and MPI, as well as pro-inflammatory biomarkers genes including NLRP3, IL18, and IL1β, were measured using quantitative real-time PCR.
Results
The expression of GP63, HSP83, and MPI revealed up-regulation in LRV2 + isolates compared to LRV2- isolates. The expression of the pro-inflammatory biomarkers including NLRP3, IL1β, and IL18 genes in LRV2- were higher than LRV2 + isolates.
Conclusion
This finding suggests that LRV2 + may have a probable effect on the Leishmania VFs and pro-inflammatory biomarkers in the human macrophage model.
Similar content being viewed by others
Introduction
Leishmaniasis is a vector-borne disease caused by an intracellular protozoan parasite of the Trypanosomatidae family [1,2,3]. Leishmaniasis has three clinical forms including cutaneous leishmaniasis (CL), visceral leishmaniasis (VL), and mucocutaneous leishmaniasis (MCL) [4,5,6].
CL is endemic in tropical and subtropical countries, with a global incidence ranging from 0.7 to 1 million new cases per year [7]. Iran is one of the endemic areas for CL and L. major, and L. tropica are responsible for approximately 80% and 20% of cases, respectively [4, 6, 8]. Clinical manifestations of CL are mostly limited to skin ulcers, however, atypical forms including disseminated, mucosal, and visceral involvements are also reported [9,10,11]. The severity of the disease seems to be multifactorial, depending on the host immune responses, Leishmania species, and sandfly factors [12, 13].
Recent evidence has highlighted the role of viruses as endosymbionts in the pathogenicity of certain protozoa [14,15,16,17]. Leishmania RNA virus (LRV) was firstly identified in L. guyanensis by Tarr et al. [18]. Based on the complete nucleotide sequence, LRVs are classified into two types: LRV1 (New World) and LRV2 (Old World), with less than 40% similarity in their genomes [19, 20]. The presence of LRV2 in Iran was mostly confirmed in L. major, and rarely in L. infantum and L. tropica [21,22,23]. However, the role of LRV in treatment failure, pathogenesis of Leishmania species, and immune responses have been investigated [24,25,26].
Leishmania virulence factors (VFs) play a crucial role in pathogenesis of the parasite by influencing the host’s immune responses [12, 27, 28]. This study examines the most important pathogenesis factors, contributing to the parasite pathogenesis and cytokine regulation.
Heat-shock proteins (HSP), glycoprotein phosphatase (GP63), and mannose phosphate isomerase (MPI) are the most important pathogenesis factors, which play crucial roles in the maturation of Leishmania spp., macrophage activation, immune modulation and growth of the parasite, respectively [29,30,31]. HSPs or stress proteins are highly evolutionarily conserved proteins that play important roles in vital activities of Leishmania, such as protection against stress and trivalent antimonials (HSP23), and the maintenance of the cell (HSP90) [16]. HSP90 (HSP83 homolog) is also considered as a viral protein in maturation of the parasite [29].
GP63, a prominent surface protein belonging to the metzincin class, is commonly expressed on the surface of Leishmania parasites. It is recognized as the primary membrane surface protein in these parasites. This activity of GP63 is related to the protection of Leishmania parasites against phagolysosomes of macrophages in hosts and digestive enzymes in the vector’s midgut [31]. Additionally, GP63 is one of the main factors, which is activated during macrophage infection that modulates immune responses [31, 42].
MPI is an enzyme playing a crucial role in the reversible conversion of fructose-6-phosphate and mannose-6-phosphate, which are essential for the biosynthesis of various glycoconjugates. The absence of MPI has been linked to prolonged growth time in Leishmania spp [14]. Additionally, Leishmania species produce significant amounts of mannose-containing glycolipids and glycoproteins, which contribute to the virulence factors of Leishmania spp [16].
Interleukin (IL) IL-1β and IL-18 are important pro-inflammatory cytokines during innate immune responses to leishmaniasis, which are mediated by activation of NOD-like receptors (NLRs) [32, 33]. The role of NLRP3 in leishmaniasis seems to be like a double-edged sword. Although NLRP3 is thought to be protective against leishmaniasis, there is evidence suggesting a synergistic role of this inflammasome in the pathogenesis of the parasite [34].
While several studies have investigated the role of LRV1 in the pathogenesis of Leishmania spp., there is few data on the effects of LRV2 in the pathogenesis of Old World Leishmania species [17, 35]. This study aimed to investigate the effects of a number of L. major (three LRV2 + and one LRV2-) isolates, collected from CL patients, on the expression of VFs (GP63, HSP83, and MPI) in Leishmania isolates, and pro-inflammatory biomarkers (NLRP3, IL18, and IL1β) on human monocyte cell line (THP-1).
Materials and methods
Sample collection and cultivation
Leishmania isolates were collected from CL patients whom were referred to the referral health centers in Golestan province, during December 2021 and May 2022. These patients were diagnosed based on the clinical characteristics and parasitology methods (including microscopic and culture detection). For parasitology diagnosis, suspected lesions to CL were scraped by using a sterile scalpel, and the exudate materials were stained with Giemsa, and microscopically checked. The scrapped materials were initially cultured on a two phasic medium containing Novy-MacNeal-Nicolle (NNN) medium and RPMI-1640 medium (Gibco, Germany) supplemented by 10% fetal bovine serum (FBS) (Gibco, Germany), with penicillin (100 U/mL) and streptomycin (100 µg/mL) (Sigma-Aldrich, St. Louis, USA). The culture media were incubated at 25˚C. After 6–8 days, the promastigotes were sub-cultured and incubated at 25 °C in RPMI-1640 medium, supplemented with 10% FBS and 1% penicillin/streptomycin, for 5 days [23].
Leishmania species identification
DNA was extracted according to the protocol of the commercial kit (Bioneer Company, Korea). To carry out the PCR, we used the primers Forward (LIN4, 5’ GGGGTTGGTGTAAAATAGGG 3’) and Reverse (LIN17, 5’ TTTGAACGGGATTTCTG 3’) to amplify identical 680 to 720-bp fragments of the kinetoplast (kDNA) gene in Leishmania isolates [36]. All the procedures were monitored by standard reference isolates of L. major (Acc. no. JN860745) and L. tropica (Acc. no. EF653267).
Leishmania RNA virus detection
RNA extraction and cDNA synthesis
Total RNA was extracted from 1 × 106 promastigotes according to the manufacturer’s protocol (YTZ, Favorgen, Taiwan). The purity of the extracted RNA was evaluated through agarose gel electrophoresis, based on the appearance of the specific bands. Additionally, the concentration of RNA was determined using a NanoDrop spectrophotometer at 260 nm (Thermo Scientific™ NanoDrop™ One Microvolume UV–Vis) (Suppl Fig. 1). The complementary DNA (cDNA) was synthesized from 100 ng of total RNA YTA kit (Favorgen, Taiwan) following the manufacturer’s protocol [17]. The amplified cDNA was stored at -20 °C till to be used for semi-nested PCR.
Semi-nested PCR
The initial PCR using an outer forward primer LRV F1 (5’ TGTAACCCACATAAACAGTGTGC 3’) and reverse primer LRV R (5’ATTTCATCCAGCTTGACTGGG 3’) was performed to amplify a 526-bp external partial sequence of the RdRp gene. The semi-nested PCR was performed on the primary PCR products. A pair of primers, forward primer LRV F2 (5’ AGGACAATCCAATAGGTCGTGT 3’) and reverse primer LRV R (5’ATTTCATCCAGCTTGACTGGG 3’) were used to amplify a 315-bp product of the RdRp gene of LRV2. The PCR program for two steps consisted of 35 cycles of 94 °C for 35 s, 60 °C for 35 s, and 72 °C for 1 min. The final extension of the strands consisted of 72 °C for 4 min. The PCR products were analyzed by electrophoresis on a 1.5% agarose gel stained with SYBR safe gel stain (Thermo Fisher Scientific, USA) next to the 100 bp DNA marker (Fermentas, Life Sciences) [17, 37].
In vitro assays
Macrophage differentiation
THP-1 cells were cultured in 25 cm2 culture flasks (SPL Life Science Co, Korea) in a complete medium containing RPMI 1640 with 25 mM HEPES, supplemented with 10% FBS and 1% penicillin (100 U/mL) and streptomycin (100 µg/mL) (Sigma-Aldrich, St. Louis, USA). The cells were incubated at 37 °C, with 5% CO2. The culture medium within the flasks was changed every 2–3 days. To differentiate THP-1 monocyte to macrophage, 5 × 105 cells/mL were transferred to a 6-well cell culture plate (SPL Life Sciences, Korea) containing RPMI-1640, supplemented with 50 ng/mL phorbol myristate acetate (PMA) (Santa Cruz Biotechnology). The cells were incubated at 37 °C and 5% CO2 for 48 h. Differentiated cells were identified by the presence of pseudopodia and adherence to the bottom of the wells, while non-adherent undifferentiated monocytes were washed away with RPMI 1640 media [38].
Leishmania culture
Promastigotes of four L. major isolates (three LRV2 + and one LRV2-) were sub-cultured in RPMI-1640 with 10% FBS and 1% penicillin-streptomycin every 5–6 days and kept at 25 °C.
Macrophage Infection
Prior to co-incubation, promastigotes of each Leishmania isolate were centrifuged at 2500 rpm for 7 min and the cell pellet was re-suspended with fresh RPMI 1640 medium with 10% FBS. THP-1 macrophages were infected with each Leishmania promastigotes isolate with a multiplicity of infection (MOI) = 3 and were incubated at 37 °C with 5% CO2. The expression analyzes of target genes were performed at zero (6 h after initial infection), 12, 24, 36, and 48 h after co-infection. All experiments were performed in duplicate.
RNA extraction and cDNA synthesis
Total RNA was extracted as described by the manufacturer (YTA, favorgen, Taiwan). The zero time-point was described as 6 h after the initial co-infection. The purity of the extracted RNA was assessed by agarose gel electrophoresis (based on the appearance of the specific bands on the gel) and the concentration of RNA was assessed using a NanoDrop spectrophotometer at 260 nm (Thermo Scientific™ NanoDrop™ One Microvolume UV-Vis). The cDNA was synthesized from 500 ng of total RNA using Superscript II Reverse Transcriptase “cDNA synthesis kit” (SMOBIO) following the manufacturer’s instructions. The amplified cDNA was stored at -20 °C till used for real-time quantitative PCR.
Quantification real-time PCR
Transcriptional analysis of the VFs genes (GP63, HSP83, and MPI) and pro-inflammatory biomarkers (NLRP3, IL18, and IL1β) was carried out compared to alpha-tubulin (ALT) and Beta-Actin (Β-ACT) genes, as housekeeping genes for Leishmania and pro-inflammatory biomarkers, respectively (Table 1).
A real-time PCR was performed in a 15-µl reaction containing: 0.5 µl forward, 0.5 µl reverse primers 7.5 µL 2X SYBR green master mix (Ampliqon, Denmark), 5.5 µl distilled water, and 1 µl cDNA from baseline pure culture or post-macrophage co-infection at zero, 12, 24, 36 and 48 h. The reaction was programmed with the following details: holding stage: at 90 °C/3 min, cycling stage: 45 cycles/15 sec at 95 °C and at 60 °C/35 sec, and melt curve stage: at 95 °C/15 sec, at 60 °C/60 sec and then at 95 °C/15 sec. Results were analyzed using the relative expression software tool (REST; https://www.gene-quantification.de/rest.html). The relative expression value of each gene was determined based on the threshold cycle (Ct) value of the target genes, calculated by normalization with ALT and Β-ACTIN constitutive gene Ct values. All experiments were duplicated and data are reported as the mean ± SD (standard deviations). The level of accepted statistically significance was 95% and P-value < 0.05.
Results
Leishmania characterization and LRV2 detection
In this study, four Leishmania isolates were selected from human CL patients based on the study’s objectives. All four isolates were identified as L. major (Suppl Fig. 2). Among these, one isolate (S1-) was LRV2 negative, while three isolates (S2+, S3+, and S4+) were positive for LRV2 using semi-nested PCR (Table 2). These isolates were further utilized for the analysis of VFs genes and pro-inflammatory biomarkers expression using RT-qPCR methods.
Virulence factors expression
GP63
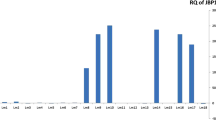
The real-time PCR results revealed significant changes in the expression of the GP63 gene for three LRV2 + isolates (S2+, S3 + and S4+) at the initial infection time of zero, compared to the S1- (LRV-). An upregulation was observed in S2+ (2.23; P-value = 0.0001), S3+ (9.21; P-value = 0.0001), and S4+ (3; P-value = 0.0001). Similarly, the expression of the GP63 gene was downregulated in S2+ (-2.3; P-value = 0.0001), S4+ (-3.7; P-value = 0.0001), but showed upregulation in S3+ (6; P-value = 0.0001) at 12 h. At the time points of 24, 36, and 48 h, all isolates were upregulated, with the highest gene expressions for GP63 gene in S3 + at 24 h (6.9; P-value = 0.0001), 36 h (9.9; P-value = 0.0001), and 48 h (4.3; P-value = 0.0001) (Fig. 1).
Gene expression of the GP63 gene in three LRV2 + isolates (S2+, S3+, and S4+) compared to LRV2- isolate (S1-) at different times after co-infection. Data analysis was done using two-way ANOVA for repeated measurements followed by the Tukey test. Bars represent mean ± SD. * Symbol represents the meaningful difference between groups. (*P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001, ****P ≤ 0.0001)
HSP83
The expression of HSP83 gene revealed significant upregulation at zero for S4+ (2.3; P-value = 0.01) compared to the S1- (LRV-). At 12 h after co-infection, significant downregulation was observed in all isolates compared to S1-. The expression of HSP83 gene after 24 h was upregulated in S2+ (2.5; P-value = 0.0001) and S3+, but was still downregulated in S4+ (-1.35; P-value = 0.0001). At 36 h, all isolates were upregulated, and at 48 h, except S2+, the expression of HSP83 was significantly upregulated compared to S1- (Fig. 2).
Gene expression of the HSP83 gene in three LRV2 + isolates (S2+, S3+, and S4+) compared to LRV2- isolate (S1-) at different times after co-infection. Data analysis was done using two-way ANOVA for repeated measurements followed by the Tukey test. Bars represent mean ± SD. * Symbol represents the meaningful difference between groups. (*P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001, ****P ≤ 0.0001)
MPI
The expression of the MPI gene was upregulated at zero time-point, with the highest expression in the S4 + isolate (4; P-value = 0.0001). At the 12 h time-point, significant upregulation was observed in the S3+ (9.4; P-value = 0.0001) and the S4+ (3.8; P-value = 0.0001) isolates. During the 24 h period after co-infection, an increase was observed in the S2+, S3+, and S4 + isolates. By the 36 h time-point, the expression of the MPI gene was significantly increased in all isolates. At 48 h, significant upregulation was observed in the S4 + isolate (2.1; P-value = 0.0176) (Fig. 3).
Gene expression of the MPI gene in three LRV2 + isolates (S2+, S3+, and S4+) compared to one LRV2- isolate (S1-) at different times after co-infection. Data analysis was done using two-way ANOVA for repeated measurements followed by the Tukey test. Bars represent mean ± SD. * Symbol represents the meaningful difference between groups. (*P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001, ****P ≤ 0.0001)
Pro-inflammatory biomarker
NLRP3
The expression of NLRP3 gene revealed significant upregulation at zero time-point for S1- (6.98; P-value = 0.0001) and S2+ (7.12; P-value = 0.0001) S3+ (5.48; P-value = 0.0001) and S4+ (8.31; P-value = 0.0001) compared to the control (un-infected macrophage). At 12, and 24 h, all isolates were significantly downregulated compared to the control. At 36 and 48 h, all LRV2 + isolates were upregulated compared to the LRV2- isolate and control groups. (Fig. 4).
The expression of the NLRP3 gene in three LRV2 + isolates (S2+, S3 + and S4+), and LRV2- isolate (S1-) compared to control (uninfected macrophage) at different times after co-infection. Data analysis was done using two-way ANOVA for repeated measurements followed by the Tukey test. Bars represent mean ± SD. * Symbol represents the meaningful difference between groups. (*P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001, ****P ≤ 0.0001)
IL-18
The results showed significant changes in the IL-18 gene expression at the time of zero compared to the control. The S1- and S2 + were upregulated, but S3 + and S4 + were downregulated. An upregulation was observed at time-point 12, in S2+, S3+, and S4+ (2.51; P-value = 0.01), (3.06; P-value = 0.001), (2.22; P-value = 0.05), respectively. The expression of the IL-18 gene during the time-points 24 and 36 h was upregulated, while the highest gene expressions of the IL-18 gene was at 36 h and in S4+ (2.61; P-value = 0.01). At the 48 h time-point, all isolates were significantly downregulated compared to control (Fig. 5).
The expression of the IL18 gene in three LRV2 + isolates (S2+, S3 + and S4+) and LRV2- isolate (S1-) compared to control (uninfected macrophage) at different times after co-infection. Data analysis was done using two-way ANOVA for repeated measurements followed by the Tukey test. Bars represent mean ± SD. * Symbol represents the meaningful difference between groups. (*P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001, ****P ≤ 0.0001)
IL-1β
The results of real-time PCR showed significant changes of the IL-1β gene at the time of zero compared to control. All isolates were significantly upregulated compared to control, but S1- revealed higher upregulation compared to LRV2 + isolates (3.6; P-value = 0.0001). At time-point 12 an upregulation was still observed in S1-, S2+, S3 + and S4+, but S2 + showed higher gene expression compared to other isolates (3.32; P-value = 0.0001). The expression of IL-1β gene during the time-points 24 and 36 h was significantly decreased in all isolates, but at 48 h, all isolates were significantly upregulated compared to other time point (Fig. 6).
The expression of the IL1β gene in three LRV2 + isolates (S2+, S3 + and S4+), and LRV2- isolate (S1-) compared to control (uninfected macrophage) at different times after co-infection. Data analysis was done using two-way ANOVA for repeated measurements followed by the Tukey test. Bars represent mean ± SD. * Symbol represents the meaningful difference between groups. (*P ≤ 0.05, **P ≤ 0.01, ***P ≤ 0.001, ****P ≤ 0.0001)
Discussion
The pathogenicity of Leishmania parasites is influenced by multiple factors, most importantly including Leishmania species, VFs expression, and the host’s immune responses [15, 16]. Recent findings have indicated that LRVs may intensify the severity of the disease, boost invasion of Leishmania parasite, and modulate immune responses [15, 17, 39, 40]. These findings suggest an association between LRVs and the clinical outcomes of leishmaniasis. The role of LRV1 in the pathogenesis of New World Leishmania species has been investigated [15, 16, 41]. However, there is limited data regarding the correlation between LRV2 and Old World Leishmania species [17]. Therefore, in this study, we evaluated the impact of LRV2 on the expression of VFs and pro-inflammatory biomarkers in response to L. major isolates, both LRV2 + and LRV2-, at different time points after co-infection.
GP63 is known to play a critical role in the attachment and entry of Leishmania promastigotes into macrophages. GP63 participates in other important processes, such as modulation of the host immune responses, degradation of host cell components, and further contributing to the pathogenesis of Leishmania infections [42, 43]. An in vivo study demonstrated that GP63-deficient L. major significantly reduces the development of CL lesions in mice, suggesting that GP63 does not significantly influence the pathogen-induced inflammatory cell recruitment, but may affect inflammatory cell activation and functions [43]. However, conflicting results have been released about the role of LRV in the expression of GP63. Kariyawasam et al. [16]. reported no significant difference in GP63 gene expression between LRV1 + and LRV1- groups. Our data revealed an increasing trend in the expression of GP63 in LRV2 + isolates compared to LRV2-. It is noteworthy that our findings on the expression of GP63 are closely aligned with the results reported by Rahmanipour et al. [17]. Therefore, it seems that the GP63 gene represents higher expression in LRV2 + isolates compared to LRV2-. Nevertheless, further studies are required to validate and confirm these results.
The expression of HSP83 gene in Leishmania-infected macrophages is upregulated. This upregulation plays a significant role in both parasite survival and replication [21]. It was shown that a higher concentration of HSP83 is associated with active mucosal and cutaneous ulcers, suggesting a positive correlation between HSP83 and the pathogenicity of Leishmania species [44, 45]. In this study, the expression of HSP83 gene showed an increase at all time-points in LRV2 + compared to LRV- isolates, although a downregulation was observed at 12 h in LRV2 + isolates. However, the outcome of the presence of LRVs on the expression of HSP-related genes is controversial. For example, Rahmanipour et al. [17]. observed higher levels of HSP70 gene expression in the initial hours for the LRV2 + strain, while it was downregulated at the final time-points. In contrast, Kariyawasm et al., [16] reported higher expression of HSP90 in LRV- strains compared to LRV1 + strains. Therefore, it seems that the role of species or strains of Leishmania and the presence of LRV may affect the expression of HSPs. Generally, HSP83 is thought to be constitutively expressed, which is consistent with our findings [16].
MPI is involved in the recruitment of other VFs including lipophosphoglycan (LPG) and GP63, and the lack of this protein has been associated with slow growth in Leishmania parasites [27]. Kariyawasm et al., [16] reported higher expression of MPI gene in LRV- strains compared to LRV1 + strains. In contrast, current findings have shown that the expression MPI gene was increased in all isolates of LRV2 + compared to LRV2-. Therefore, it may be concluded that LRV2 plays an important role in the upregulation of VFs genes. However, to validate this observation, further investigations are required. For this purpose, monitoring of the ulcer progression, response to treatment, and clinical presentation of CL lesions should be considered.
Different results have been reported regarding the role of cytokines and inflammasomes in the pathogenesis of CL [15, 34, 41, 46]. As an early response to Leishmania, activation of inflammasomes, particularly NLRP3, is a vital part of the immune response to the parasite. Upon stimulating NLRP3, caspase-1 is activated through auto-proteolysis, leading to the activation of pro-IL-18 and pro-IL-1β [47, 48]. Ives et al., [26] suggested that LRV may directly activate inflammatory signaling in macrophages, which leads to the activation of cytokines and chemokines. Therefore, LRV is a potential ligand for the activation of toll-like receptor (TLR) 3 and subsequent activation of the NLRP3 inflammasome [26]. Our results demonstrated that there was no difference in NLRP3 expression between LRV2 + and LRV2- isolates, during the initial hours, but at 48 h, LRV2 + isolates significantly increased the expression levels of NLRP3 gene compared to LRV2-. de Carvalho et al. [40]. reported an inverse association between inflammasome activation and the severity of leishmaniasis, supporting a protective role of the inflammasome during Leishmania infection. Therefore, it can be concluded that the presence of LRV1 dampens NLRP3 activation to favor infection and pathogenesis of Leishmania parasite. Nevertheless, the activation of the NLRP3 plays a crucial role in determining the outcome of leishmaniasis [34]. Hartley et al., [49] reported no significant difference in NLRP3 expression between LRV1 + and LRV1- in L. guyanensis. Therefore, they demonstrated that L. guyanensis evades inflammasome activation, regardless of the presence of LRV1. Indeed, there is limited understanding of the signaling pathways that trigger NLRP3 activation in response to Leishmania infection. Further research is needed to elucidate the specific mechanisms through which Leishmania parasites induce NLRP3 activation and the subsequent inflammatory responses [39].
The role of IL-1β and IL-18 in Leishmania infection has been the subject of numerous studies [39, 46, 48]. It was reported that IL-1β can modulate the immune responses, while IL-18 shifts the T-cell activation pathway towards Th2, however, both cytokines contribute to the progression of the disease [50, 51]. Notably, IL-1β has been identified as a significant signaling factor for host resistance against infection, as this cytokine transmits signals through IL-1R and myeloid differentiation primary response protein (MyD) 88, leading to the induction of NOS2-mediated nitric oxide (NO) production. In addition, it was suggested that IL-1β plays a role in increasing NO production, leading to reduced parasite proliferation and enhanced resistance to Leishmania infection. In our study, the expression of IL-1β gene was higher in the LRV- isolate than the LRV2 + isolates at the initial and final hours. In the line of our results, Kariyawasam et al., [15] and Carvalho et al., [40] reported similar findings, reporting higher expression of IL-1β gene in LRV1- compared to LRV1+. Hence, it appears that the presence of LRV plays a significant role in suppressing the activity of the immune system and the expression of pro-inflammatory cytokines. The expression of IL-1β in LRV2 + isolates was reported higher than in LRV- isolate during the early hours, but in contrast to our findings, the expression of IL-1β gene was lower in LRV- isolate compared to LRV2 + isolate at the final hours [17].
IL-18 is a pro-inflammatory cytokine that plays a protective role against pathogenesis factors of the Leishmania parasite and contributes to innate and adaptive immunity. Evidence suggests that IL-18 plays a critical role in modulating T cell responses during L. major infection [51,52,53]. Some studies indicate a positive role for IL-18 in promoting Th1 responses and resistance against Leishmania species infection, while conflicting results showed that IL-18 may enhance Th2-biased responses and causes susceptibility to the parasites [51, 52]. It was suggested that IL-18 may induce development of Th1 and natural killer (NK) cells and production of IFNγ via overexpression of IL-18R on Th1 and NK cells [54, 55]. In addition, IL-18 induces an IFNγ-independent immunity against Leishmania parasites [56]. In contrast, IL-18 seems to produce and release Th2 cytokines like IL-4 and IL-13 [57,58,59], which are protective against L. donovani, while induces susceptibility to L. major [58]. However, the role of IL-18 in Leishmania infections remains vague and depends to the Leishmania species and host genetics. In our study, we observed downregulation of IL-18 gene in the LRV2 + isolates compared to the LRV2- isolate in the early and middle hours, however, there was an upregulation during the final hour. However, it is necessary to fully elucidate the mechanisms behind the activation of the host’s immune responses in leishmaniasis, led by IL-18.
Conclusion
Our observations indicate that the presence of LRV2 + in L. major in comparison to LRV2- leads to an increase in the expression of VFs (GP63, HSP83, and MPI genes), while there is a declining trend in the expression of pro-inflammatory biomarkers (NLRP3, IL-18, and IL-1β genes). However, it is crucial to take into account the influence of various factors, including the host immune response, different Leishmania strains, the presence of VFs, and the expression of cytokines, in addition to the LRV status.
Collectively, the pathogenesis of Leishmania parasites is highly complex, particularly when attempting to establish a link between the pathogenesis and Leishmania viruses. Understanding the interplay between the parasite, the virus, and the host immune responses is a critical challenge, and further investigations and comprehensive studies are required to unravel the intricate mechanisms involved in the pathogenesis of Leishmania parasites and the potential influence of LRVs.
Data Availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Rioux J, Lanotte G, Serres E, Pratlong F, Bastien P, Perieres J. Taxonomy of Leishmania. Use of isoenzymes. Suggestions for a new classification. Ann Parasitol Hum Comp. 1990;65(3):111–25.
Bruschi F, Gradoni L. The leishmaniases: old neglected Tropical Diseases. Springer; 2018.
Torres-Guerrero E, Quintanilla-Cedillo MR, Ruiz-Esmenjaud J, Arenas R. Leishmaniasis: a review. F1000Research. 2017;6.
Firooz A, Mortazavi H, Khamesipour A, Ghiasi M, Abedini R, Balighi K, et al. Old world cutaneous Leishmaniasis in Iran: clinical variants and treatments. Dermatol Ther. 2021;32(7):673–83.
Ghatee MA, Taylor WR, Karamian M. The geographical distribution of cutaneous Leishmaniasis causative agents in Iran and its neighboring countries, a review. Front Public Health. 2020;8:11.
Mohebali M. Visceral Leishmaniasis in Iran: review of the epidemiological and clinical features. Iran J Parasitol. 2013;8(3):348.
Alvar J, Vélez ID, Bern C, Herrero M, Desjeux P, Cano J, et al. Leishmaniasis worldwide and global estimates of its incidence. PLoS ONE. 2012;7(5):e35671.
Norouzinezhad F, Ghaffari F, Norouzinejad A, Kaveh F, Gouya MM. Cutaneous Leishmaniasis in Iran: results from an epidemiological study in urban and rural provinces. Asian Pac J Trop Biomed. 2016;6(7):614–9.
Akilov OE, Khachemoune A, Hasan T. Clinical manifestations and classification of Old World cutaneous Leishmaniasis. Int J Dermatol. 2007;46(2):132–42.
Scorza BM, Carvalho EM, Wilson ME. Cutaneous manifestations of human and murine Leishmaniasis. Int J Mol Sci. 2017;18(6):1296.
Kakooei Z, Hajjaran H, Akhoundi B, Charehdar S, Elikaee S, Shafeghat Z, et al. Treatment failure in cutaneous Leishmaniasis patients referred to the School of Public Health, Tehran University of Medical Sciences during 2008–2017. J Arthropod Borne Dis. 2020;14(4):363.
Bifeld E, Clos J. The genetics of Leishmania virulence. Med Microbiol Immunol. 2015;204:619–34.
Lamotte S, Späth GF, Rachidi N, Prina E. The enemy within: Targeting host–parasite interaction for antileishmanial drug discovery. PLoS Negl Trop Dis. 2017;11(6):e0005480.
Mukkala AN, Kariyawasam R, Lau R, Valencia BM, Llanos-Cuentas A, Boggild AK. Elevated baseline expression of seven virulence factor RNA transcripts in visceralizing species of Leishmania: a preliminary quantitative PCR study. TAI. 2022;9:20499361221102665.
Kariyawasam R, Grewal J, Lau R, Purssell A, Valencia BM, Llanos-Cuentas A, et al. Influence of Leishmania RNA virus 1 on proinflammatory biomarker expression in a human macrophage model of American tegumentary Leishmaniasis. J Infect Dis. 2017;216(7):877–86.
Kariyawasam R, Mukkala AN, Lau R, Valencia BM, Llanos-Cuentas A, Boggild AK. Virulence factor RNA transcript expression in the Leishmania Viannia subgenus: influence of species, isolate source, and Leishmania RNA virus-1. Trop Med Int Health. 2019;47(1):1–9.
Rahmanipour M, Mohebali M, Koosha M, Kazemirad E, Yasami-Khiabani S, Mirjalali H et al. Effect of Leishmania RNA virus 2 on virulence factors and cytokines gene expression in a human macrophage infected with Leishmania major: a preliminary study. Exp Parasitol. 2022:108459.
Tarr PI, Aline RF Jr, Smiley BL, Scholler J, Keithly J, Stuart K. LR1: a candidate RNA virus of Leishmania. PNAS. 1988;85(24):9572–5.
Ogg MM, Carrion R, BOTELHO ACDC, Mayrink W, Correa-Oliveira R, Patterson JL. Quantification of leishmaniavirus RNA in clinical samples and its possible role in pathogenesis. Am J Trop Med Hyg. 2003;69(3):309–13.
Scheffter SM, Ro YT, Chung IK, Patterson J. The complete sequence of Leishmania RNA virus LRV2-1, a virus of an Old World parasite strain. Virol. 1995;212(1):84–90.
Saberi R, Fakhar M, Mohebali M, Anvari D, Gholami S. Global status of synchronizing Leishmania RNA virus in Leishmania parasites: a systematic review with meta-analysis. Transbound Emerg Dis. 2019;66(6):2244–51.
Hajjaran H, Mahdi M, Mohebali M, Samimi-Rad K, Ataei-Pirkooh A, Kazemi-Rad E, et al. Detection and molecular identification of Leishmania RNA virus (LRV) in Iranian Leishmania species. Arch Virol. 2016;161:3385–90.
Saberi R, Fakhar M, Hajjaran H, Ataei-Pirkooh A, Mohebali M, Taghipour N, et al. Presence and diversity of Leishmania RNA virus in an old zoonotic cutaneous Leishmaniasis focus, northeastern Iran: haplotype and phylogenetic based approach. IJID. 2020;101:6–13.
Hartley M-A, Bourreau E, Rossi M, Castiglioni P, Eren RO, Prevel F, et al. Leishmaniavirus-dependent metastatic Leishmaniasis is prevented by blocking IL-17A. PLoS Pathoge. 2016;12(9):e1005852.
Cantanhêde LM, da Silva Júnior CF, Ito MM, Felipin KP, Nicolete R, Salcedo JMV, et al. Further evidence of an association between the presence of Leishmania RNA virus 1 and the mucosal manifestations in tegumentary Leishmaniasis patients. PLoS Negl Trop Dis. 2015;9(9):e0004079.
Ives A, Ronet C, Prevel F, Ruzzante G, Fuertes-Marraco S, Schutz F, et al. Leishmania RNA virus controls the severity of mucocutaneous Leishmaniasis. Science. 2011;331(6018):775–8.
Atayde VD, Hassani K, da Silva Lira Filho A, Borges AR, Adhikari A, Martel C, et al. Leishmania exosomes and other virulence factors: impact on innate immune response and macrophage functions. Cell Immunol. 2016;309:7–18.
Omoruna O, Mukkala AN, Kariyawasam R, Shao E, Challa P, Klowak MA, et al. A systematic review of virulence factors in the Leishmania Genus. Am J Trop Med Hyg. 2019;101:566.
Rico AI, Angel SO, Alonso C, Requena JM. Immunostimulatory properties of the Leishmania infantum heat shock proteins HSP70 and HSP83. Mol Immunol. 1999;36(17):1131–9.
Larreta R, Soto M, Quijada L, Folgueira C, Abanades DR, Alonso C, et al. The expression of HSP83 genes in Leishmania infantum is affected by temperature and by stage-differentiation and is regulated at the levels of mRNA stability and translation. BMC Mol Biol. 2004;5(1):1–18.
Silva-Almeida M, Pereira BAS, Ribeiro-Guimarães ML, Alves CR. Proteinases as virulence factors in Leishmania spp. Infection in mammals. Parasit Vectors. 2012;5(1):1–10.
Drexler SK, Yazdi AS. Complex roles of inflammasomes in carcinogenesis. J Cancer. 2013;19(6):468–72.
Broderick L, De Nardo D, Franklin BS, Hoffman HM, Latz E. The inflammasomes and autoinflammatory syndromes. Annu Rev Pathol : Mech Dis. 2015;10:395–424.
Harrington V, Gurung P. Reconciling protective and pathogenic roles of the NLRP3 inflammasome in Leishmaniasis. Immunol Rev. 2020;297(1):53–66.
Zangger H, Hailu A, Desponds C, Lye L-F, Akopyants NS, Dobson DE, et al. Leishmania Aethiopica field isolates bearing an endosymbiontic dsRNA virus induce pro-inflammatory cytokine response. PLoS Negl Trop Dis. 2014;8(4):e2836.
Azizi K, Soltani A, Alipour H. Molecular detection of Leishmania isolated from cutaneous Leishmaniasis patients in Jask County, Hormozgan province, southern Iran, 2008. Asian Pac J Trop Med. 2012;5(7):514–7.
Farrokhi-Karibozorg M, Ghayour-Najafabadi Z, Hejazi SH, Ataei-Pirkooh A, Mohebali M, Teimouri P, et al. Molecular identification of Leishmania RNA virus in cutaneous Leishmaniasis patients and rodent reservoirs in Isfahan province. Iran Infect Genet Evol. 2022;98:105222.
Pazoki H, Rahimi HM, Mirjalali H, Niyyati M, Mosaffa N, Tabaei SJS et al. Soluble total antigen derived from Toxoplasma gondii tachyzoites increased the expression levels of NLRP1, NLRP3, NLRC4, AIM2, and the release of mature form of IL1β, but downregulated the expression of IL1β and IL18 genes in THP-1cell line. Microb. Pathog. 2021;158:105072.
Carvalho AM, Fernanda ON, Paixão CS, de Oliveira CI, Machado PRL, Carvalho LP, et al. Glyburide, a NLRP3 inhibitor, decreases inflammatory response and is a candidate to reduce pathology in Leishmania braziliensis Infection. JID. 2020;140(1):246.
de Carvalho RV, Lima-Junior DS, da Silva MVG, Dilucca M, Rodrigues TS, Horta CV, et al. Leishmania RNA virus exacerbates Leishmaniasis by subverting innate immunity via TLR3-mediated NLRP3 inflammasome inhibition. Nat Commun. 2019;10(1):5273.
Kariyawasam R, Lau R, Valencia BM, Llanos-Cuentas A, Boggild AK. Leishmania RNA virus 1 (LRV-1) in Leishmania (Viannia) braziliensis isolates from Peru: a description of demographic and clinical correlates. Am. J. Trop. Med. Hyg. 2020;102(2):280.
Yao C, Donelson JE, Wilson ME. The major surface protease (MSP or GP63) of Leishmania sp. Biosynthesis, regulation of expression, and function. Mol Biochem Parasitol. 2003;132(1):1–16.
Chan A, Ayala J-M, Alvarez F, Piccirillo C, Dong G, Langlais D, et al. The role of Leishmania GP63 in the modulation of innate inflammatory response to Leishmania major Infection. PLoS ONE. 2021;16(12):e0262158.
Skeiky Y, Benson DR, Guderian JA, Whittle JA, Bacelar O, Carvalho EM, et al. Immune responses of Leishmaniasis patients to heat shock proteins of Leishmania species and humans. Infect Immun. 1995;63(10):4105–14.
Kaufmann SH. Heat shock proteins and the immune response. Immunol Today. 1990;11:129–36.
Kihel A, Hammi I, Darif D, Lemrani M, Riyad M, Guessous F, et al. The different faces of the NLRP3 inflammasome in cutaneous Leishmaniasis: a review. Cytokine. 2021;147:155248.
Guarda G, Zenger M, Yazdi AS, Schroder K, Ferrero I, Menu P, et al. Differential expression of NLRP3 among hematopoietic cells. J Immunol. 2011;186(4):2529–34.
Jo E-K, Kim JK, Shin D-M, Sasakawa C. Molecular mechanisms regulating NLRP3 inflammasome activation. Cell Mol Immunol. 2016;13(2):148–59.
Hartley M-A, Ronet C, Zangger H, Beverley SM, Fasel N. Leishmania RNA virus: when the host pays the toll. Front Cell Infect Microbiol. 2012;2:99.
Aoki JI, Muxel SM, Zampieri RA, Müller KE, Nerland AH, Floeter-Winter LM. Differential immune response modulation in early Leishmania amazonensis Infection of BALB/c and C57BL/6 macrophages based on transcriptome profiles. Sci Rep. 2019;9(1):19841.
Gurung P, Karki R, Vogel P, Watanabe M, Bix M, Lamkanfi M, et al. An NLRP3 inflammasome–triggered Th2-biased adaptive immune response promotes Leishmaniasis. J Clin Investig. 2015;125(3):1329–38.
Monteforte GM, Takeda K, Rodriguez-Sosa M, Akira S, David JR, Satoskar AR. Genetically resistant mice lacking IL-18 gene develop Th1 response and control cutaneous Leishmania major Infection. J Immunol. 2000;164(11):5890–3.
Wei X-Q, Niedbala W, Xu D, Luo Z-X, Pollock KG, Brewer JM. Host genetic background determines whether IL-18 deficiency results in increased susceptibility or resistance to murine Leishmania major Infection. Immunol Lett. 2004;94(1–2):35–7.
Wei XQ, Leung BP, Niedbala W, Piedrafita D, Feng GJ, Sweet M et al. Altered immune responses and susceptibility to Leishmania major and Staphylococcus aureus infection in IL-18-deficient mice. J Immunol. 1999; 163:2821–8.
Nakanishi K, Yoshimoto T, Tsutsui H, Okamura H. Interleukin-18 regulates both Th1 and Th2 responses. Annu Rev Immunol. 2001;19:423–74. https://doi.org/10.1146/annurev.immunol.19.1.423.
Murray HW, Tsai CW, Liu J, Ma X. Responses to Leishmania Donovani in mice deficient in interleukin-12 (IL-12), IL-12/IL-23, or IL-18. Infect Immun. 2006;74:4370–4. https://doi.org/10.1128/IAI.00422-06.
Yoshimoto T, Tsutsui H, Tominaga K, Hoshino K, Okamura H, Akira S, et al. IL-18, although antiallergic when administered with IL-12, stimulates IL-4 and histamine release by basophils. Proc Natl Acad Sci USA. 1999;96:13962–6. https://doi.org/10.1073/pnas.96.24.13962.
Yoshimoto T, Mizutani H, Tsutsui H, Noben-Trauth N, Yamanaka K, Tanaka M, et al. IL-18 induction of IgE: dependence on CD4 + T cells, IL-4 and STAT6. Nat Immunol. 2000;1:132–7. https://doi.org/10.1038/77811.
Dayakar A, Chandrasekaran S, Kuchipudi SV, Kalangi SK. Cytokines: key determinants of resistance or Disease progression in visceral Leishmaniasis: opportunities for novel diagnostics and immunotherapy. Front Immunol. 2019;10:670. https://doi.org/10.3389/fimmu.2019.00670.
Acknowledgements
We would like to thankful to all authors that their valuable publications were included in this study.
Funding
This study was supported by Tehran University of Medical Science (TUMS), Tehran, Iran, (Code number: 53395)
Author information
Authors and Affiliations
Contributions
HH and MM designed the study. ZM contributed to manuscript writing, and EK, AKH, KS, and HM participated in the revising of the manuscript. RS contributed to sample collection. HMR and MK contributed to Real-Time PCR performing, prepared figures and analysis. All authors read and confirmed the final version of the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This research was approved by Tehran University of Medical Science (TUMS), Tehran, Iran, (Ethical code number: IR.TUMS.SPH.REC.1400.251). Written informed consent was obtained from the patients. All methods were carried out in accordance with relevant regulations and guidelines.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary Material 1:
Suppl Fig 1. The 1.5% gel electrophoresis of extracted RNA from isolated L. major. The presence of three 5s, 15s, and 28s confirmed the extraction of RNA from L. major sample.
Supplementary Material 2:
Suppl fig 2. The gel electrophoresis of conventional PCR for detection of Leishmania spp. Line 1: ladder 100 bp, Line 2: negative control; Line 3: positive control for L. tropica; Line 4: positive control for L. major, Line 5–8: samples.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mirabedini, Z., Mirjalali, H., Kazemirad, E. et al. The effects of Leishmania RNA virus 2 (LRV2) on the virulence factors of L. major and pro-inflammatory biomarkers: an in vitro study on human monocyte cell line (THP-1). BMC Microbiol 23, 398 (2023). https://doi.org/10.1186/s12866-023-03140-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12866-023-03140-0