Abstract
Background
Methicillin-resistant Staphylococcus aureus is linked to both nosocomial and community infections. One of the key virulence factors of S. aureus is Panton-Valentine leukocidin (PVL). The PVL genes are mostly associated with community-acquired MRSA (CA-MRSA). This study evaluates the prevalence of PVL genes as a marker for CA-MRSA at tertiary hospitals in Mansoura, Dakahlia, Egypt. S. aureus was isolated from clinical specimens obtained from different departments of tertiary hospitals, outpatient clinics, and hospital healthcare workers (HCWs). PCR was used to detect the mecA, PVL, and SCCmec genes among the recovered isolates. Standard broth microdilution method was used to determine the minimum inhibitory concentrations (MIC) of nine antibiotics against S. aureus.
Results
Two hundred S. aureus isolates were recovered and identified out of the total isolates (n = 320). The mecA gene was detected in 103 S. aureus isolates (51.5%). Among the MRSA isolates, 46.60% were PVL-positive. The incidence of the PVL genes of MRSA in nosocomial (HA), outpatient clinics (CA), and HCWs was 46.66%, 56.52%, and 42%, respectively. All MRSA isolates showed resistance to cefoxitin. The percentage of resistance to most tested antibiotics was high, except for ciprofloxacin (6.85%). Both antibiotic resistance and multidrug resistance among MRSA isolates were generally higher in PVL-positive isolates than in PVL-negative isolates in HA- and CA-MRSA isolates. While SCCmec type V was the most prevalent in PVL-positive MRSA stains, type I was the most prevalent in PVL-negative isolates.
Conclusion
This study revealed that PVL genes are generally highly prevalent among mecA-positive MRSA isolates, whether they are CA-MRSA, HA-MRSA, or HCW isolates. Therefore, PVL is not a valid marker for CA-MRSA in Mansoura, Dakahlia Governorate, Egypt, as has been reported in other countries. Further epidemiologic studies are required to track the incidence of PVL in HA-MRSA, CA-MRSA, and HCW isolates in other Egyptian governorates.
Similar content being viewed by others
Introduction
Staphylococcus aureus is the most aggressive species of staphylococci and causes a wide range of symptoms, from skin and soft tissue infections to potentially lethal pneumonia and toxin-related illnesses like toxic shock syndrome. It is also one of the most frequently isolated pathogens from hospitalised patients and the second-most frequently isolated pathogen from people in outpatient settings [1]. Although the discovery of penicillin in the 1940s helped to reduce the high mortality rate caused by S. aureus, this was short-lived because resistant isolates producing β-lactamases quickly evolved, and most S. aureus infections in hospitals became penicillin-resistant [2]. In the late 1950s, methicillin, which is a β-lactam antibiotic insensitive to beta-lactamases, offered a new option for treating resistant S. aureus infections. However, soon, methicillin-resistant S. aureus (MRSA) isolates appeared primarily in healthcare settings. MRSA isolates are resistant to all β-lactams, including penicillins and cephalosporins [2]. In addition to β-lactam resistance, MRSA isolates gradually developed resistance to other antibiotic classes [3]. Currently, multidrug resistance (MDR) is highly prevalent in MRSA isolates, and it is one of the most important current threats to public health [4].
MRSA resistance to β-lactam antibiotics is linked to the mecA gene, which encodes penicillin-binding protein 2a (PBP2a). PBP2a has a poor affinity for all β-lactams and maintains the transpeptidase activity in MRSA isolates in the presence of lethal amounts of β-lactams [5]. PBP2a is encoded by the mecA gene, which is contained in a movable genetic component known as the Staphylococcal chromosome cassette mec (SCCmec) [5, 6]. mecC MRSA is a recently identified subtype of MRSA that encodes a divergent mec gene and may colonise and infect a broad variety of host species, including humans. Although mecC MRSA isolates are currently uncommon and have been identified mainly in Europe, they could pose a diagnostic challenge when mecA or PBP2a/2′ detection is only used to diagnose MRSA [7]. Alongside their rise in nosocomial infections, MRSA isolates from community patients have become globally prevalent, and reports of serious and rapidly progressive fatal disease due to virulent community-acquired MRSA (CA-MRSA) have currently alarmed healthcare professionals [8].
S. aureus has a variety of virulence factors that enable it to evade the immune system and attach to and injure the host. These factors are related to the pathogenicity of the bacterium. One virulence factor of S. aureus that has a particular importance is Panton–Valentine leukocidin (PVL). It is composed of two separate proteins encoded by two adjacent genes, lukS-PV and lukF-PV [9]. The bicomponent toxin is a pore-forming leukotoxin that lyses leukocytes and has been initially associated with severe skin and soft tissue infections and necrotizing pneumonia [10].
The PVL genes were initially and frequently more associated with CA-MRSA isolates and were rarely found in hospital-acquired MRSA (HA-MRSA) isolates. However, subsequently, they were also detected among HA-MRSA isolates [11]. Therefore, in this study, we investigated the prevalence of PVL genes among HA-MRSA, CA-MRSA, and HCWs collected from Mansoura tertiary hospitals, Dakahlia Governorate, Egypt.
Materials and methods
Specimens’ collection
Non-duplicated specimens of pus, urine, blood cultures and nasal nares swabs were screened for S. aureus from April 2020 to February 2021. The specimens were collected from different hospital departments, at Mansoura University tertiary hospital labs that serve Dakahlia citizens. The specimens were obtained from 69 inpatients, 50 outpatient clinics and 81 HCWs. They were collected from eyes, pus, blood and urinary tract infections. Hospital-acquired S. aureus isolates were obtained from patients after admission to tertiary hospitals for more than 72 h. Community-acquired isolates were obtained from outpatient departments for patients who had not previously been hospitalised within the last 6 months. Nasal swaps were obtained from health care workers, including doctors, nurses, laboratory technicians, and housekeeping staff.
MRSA isolation and identification
Isolates were identified as S. aureus by standard methods. They were plated out on several culture media, including blood agar (Oxoid™, Thermo Scientific, USA), mannitol salt agar (Oxoid™, Thermo Scientific, USA), and nutrient agar (Oxoid™, Thermo Scientific, USA). Gram-staining, catalase and coagulase assays were used to confirm morphologically suspicious staphylococcal colonies [12]. The identified S. aureus isolates were kept at -80 °C in a tryptone-soy broth (Oxoid™, Thermo Scientific, USA) containing 20% glycerol, for subsequent testing. To primarily detect MRSA, S. aureus isolates were screened by disc diffusion susceptibility tests using 30 µg cefoxitin discs (Oxoid™, Thermo Scientific, USA) and Mueller-Hinton agar (Oxoid™, Thermo Scientific, USA) according to the CLSI guidelines [13].
Antibiotic susceptibility testing (AST)
Antibiotic susceptibility testing was performed by standardised broth microdilution for the determination of the minimal inhibitory concentration (MIC), according to the CLSI guidelines [13]. Briefly, bacterial turbidity was adjusted to 0.5 McFarland standard. Antibiotics were twofold serially diluted in Mueller-Hinton broth in microtiter plates. Wells were inoculated with bacterial suspensions in Muller-Hinton broth and incubated for 18 h. The MIC was calculated as the lowest concentration of the antibiotic that completely inhibited the growth of the tested organism in microtiter wells [13].
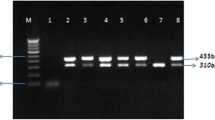
Screening isolates for mecA, PVL and SCC mec types (I-V) genes by polymerase chain reaction (PCR)
DNA was extracted from the MRSA isolates by boiling method [14]. The primers used for mecA, PVL and SCCmec genes (QIAGEN, USA), are listed in Table 1. For all genes, the thermocycler (FPROGO2D, Techni LTD, Oxford Cambridge, UK) was programmed for an initial denaturation at 94 °C for 4 min, followed by 30 amplification cycles and a final extension at 72 °C for 2 min. For mecA, the cycles were denaturation at 94 °C for 30s, annealing at 55 °C for 30s, and extension at 72 °C. For PVL the amplification cycle was denaturation at 94 °C for 45s, annealing at 56 °C for 45s and extension at 72 °C for 30s.
For SCCmec the cycles were denaturation at 94 °C for 30 s, annealing at 55 °C for 30s and extension at 72 °C for 60s. Seven µl of PCR products were analysed by electrophoresis at 100 V for 45 min on 1.5% agarose gel containing ethidium bromide (Sigma-Aldrich®, Germany) followed by visualisation using a UV transilluminator (Hoefer™, USA) at 312 nm.
Statistical analysis
The Chi-square test was used for the statistical evaluation of different parameters between two groups using SPSS, ver. 17. P-value of ≤ 0.05 was considered statistically significant.
Result
Isolation and identification of MRSA
A total of 200 S. aureus were isolated from different hospital departments, outpatient clinics, and nasal swabs of health care workers. The prevalence of MRSA among HCWs, outpatients, and inpatients was 43.5% (50/81), 46% (23/50), and 61.7% (30/69), respectively. As shown in Table 2, the PVL genes were relatively more prevalent in pus samples (64.28%), followed by blood (60.00%). The overall prevalence of the PVL genes among MRSA was 46.60% (48/103), distributed as follows: 46.60% HA-MRSA, 56.52% CA-MRSA, and 42% HCWs (Table 3).
Antibiotic susceptibility of MRSA
Cefoxitin resistance was demonstrated in all MRSA isolates (Table 4). A relatively high percentage of resistance was observed for PVL-positive than PVL-negative isolates. Resistances to clindamycin and gentamicin were statistically higher in PVL-positive than PVL-negative isolates (P < 0.05). All recovered MRSA isolates (n = 103) were multidrug-resistant (MDR). Out of the nine classes of tested antibiotics, PVL-negative isolates were resistant to 3–8 classes and PVL-positive isolates were resistant to 5–8 antibiotics classes (Table 5).
Most MRSA isolates (63.1%) were resistant to six to seven antibiotic classes. While the percentages of resistance to seven antibiotics in PVL-positive in HA, CA and HCWs isolates were 71.4%, 46.0% and 81.0%, respectively. In PVL-negative isolates, their percentages were 62.51%, 40.0%, and 62.7%, respectively (Table 5).
The most commonly observed resistance pattern in MRSA isolates was: Cef, Ere, Gen, Tet, Cli, TS, Fus. This pattern was detected in 18.44% of the MRSA isolates.
Detection of mecA, PVL and SCCmec genes
MRSA-positive isolates were screened for SCCmec types. The most common type among the PVL-positive isolates was type V. However, type I was the most prevalent among the PVL-negative isolates. The rate of type V SCCmec gene was significantly higher (p ≤ 0.05) in PVL-positive compared to PVL-negative. Type IV SCCmec gene was detected in 22.92% and 23.62% of PVL-positive and PVL-negative isolates, respectively. Type II SCCmec was not detected in any of the PVL-positive or negative isolates. The other unidentified SCCmec types were 22.92% and 27.26% in PVL-positive and PVL-negative isolates, respectively (Table 6).
Discussion
The widespread proliferation of MRSA is a major public health issue that challenges clinicians all over the world [15]. MRSA first emerged in the 1960s after being isolated from clinical specimens of hospitalised patients. Since the early nineties, MRSA has expanded quickly in communities all over the world. However, a decrease in the rates of MRSA infections has been reported in the UK and several developed countries [16]. On the contrary, the literature suggests an increase in MRSA infections in developing countries [17, 18]. However, there is a lack of a national surveillance system in Egypt to extrapolate the data obtained in different cities to have nationwide data. Reports described a general MRSA prevalence rate of 50–82% among patients hospitalised in two large Egyptian cities, Cairo and Alexandria, and a lower rate of 24% in the less populated City of Minia in southern Egypt [19]. The prevalence of CA-MRSA in Egypt ranges between 19 and 47% [20].
In this study, the overall incidence of MRSA was 51.5% (103/200), which is very high compared to the USA and Europe [23,24,25]. In addition, its incidence was relatively higher among HCWs (61.7%) compared to CA-MRSA (46%) and HA isolates (43.5%). The pathogenicity of S. aureus and its resistance to antibiotics are detrimental factors in the treatment of infections [21]. One of the key virulence factors of S. aureus is PVL, which increases the pathogenicity of S. aureus by accelerating apoptosis and destroying polymorphonuclear and mononuclear cells [10]. Generally speaking, the prevalence of PVL genes among MRSA isolates has been increasing in different countries [22,23,24]. However, it differs from one country to another [25, 26]. European countries with low overall rates of PVL-positive MRSA isolates include the United Kingdom (0.06%) [27], Germany (6.2%) [28], Ireland (1.8%) [29] and the Netherlands (15%) [30]. Low incidences were also reported in some Asian countries, like China (12.8%) [31] and Japan [11]. On the contrary, relatively higher rates of PVL-positive MRSA are common in Mediterranean countries like Turkey (18.3%) [32] and France (33.8%) [33].
In Egypt, there are a few studies on the molecular epidemiology of PVL-encoding MRSA isolates [34,35,36]. In the present study, the overall rate of detection of PVL genes was 46.60% (48/103) among MRSA isolates. This rate of prevalence of the PVL genes is higher than the rates in European, Asian, and Mediterranean countries. Previous reports from three different geographical locations in Egypt suggested different rates of prevalence of PVL genes. PVL-MRSA prevalence rates in Cairo and Ismailia were 19.04% and 92.2% in CA-MRSA, respectively, and 22.2% and 28.6% in HA-MRSA [34, 35]. On the other hand, the incidence of PVL genes was 16.67% in HCWs in the city of Fayoum [36]. In our study, a generally high incidence of PVL-positive MRSA in HA-MRSA, CA-MRSA, and HCWs was detected. The PVL-MRSA prevalence was 42.00%, 46.60%, and 56.52% in HA, CA, and HCWs, respectively.
The strikingly higher incidence of MRSA and PVL-MRSA in HA, CA, and HCWs in this study may be attributed to factors such as the excessive use of antibiotics due to the availability of antibiotics without prescription, the prescription of antibiotics for viral infections, as well as the absence of rapid and accurate methods for identification and decolonization of carries. On the other hand, one of the principal infection control measures for limiting the spread of nosocomial MRSA infection involves the performance of admission screening cultures for MRSA and the isolation of colonized or infected patients [37]. This protocol does not seem to be strictly implemented in tertiary hospitals of Mansoura. In addition, in tertiary hospitals in Egypt, there is a patient escort system. In this case, a person close to the patient stays with him in his room. So, the patient companions should also be screened for MRSA, otherwise, they contribute to the spread of CA-MRSA in hospitals. Therefore, it is not surprising that the incidence of MRSA isolates recovered from HCWs was 61.7%. and the incidence of PVL-positive isolates was 42%.
The high carriage rate of PVL-MRSA isolates in HCWs (42.0%) detected in this study suggests that they act as a reservoir for PVL-MRSA isolates and shed these isolates in both tertiary hospitals and the community. Therefore, strict control measures for the carriage of MRSA by patients admitted to hospitals and health care workers should be implemented.
Concerning antibiotic susceptibility testing, all recovered MRSA isolates (n = 103) were multidrug resistant, according to the European Centre for Disease Prevention and Control (ECDC) and the Centres for Disease Control and Prevention (CDC) [38]. All MRSA isolates were cefoxitin-resistant. The high levels of resistance rates for erythromycin, gentamicin, tetracycline, and clindamycin were observed (97.9%, 87.5%, 87.5% and 83.3%, respectively). This may be attributed to class I integrons, which are common in MRSA isolates from Egypt [39]. Class I integron has been associated with the resistance of staphylococci to several antibiotics, including erythromycin, gentamicin, tetracycline, and trimethoprim/sulfamethoxazole [40].
A lower overall resistance rate of 6.85% was observed for ciprofloxacin. This confirms a previous report of a low resistance rate for CA-MRSA in Mansoura [41]. It seems that ciprofloxacin is not very commonly prescribed at Mansoura, and therefore, MRSA isolates are still highly sensitive to it. In contrast, 96% of the MRSA isolates at Alexandria Main University Hospital are resistant to ciprofloxacin [42]. The overall rate of resistance to vancomycin in this study was 23.4%. Therefore, vancomycin can still be used for the treatment of MRSA isolates and should be guided by culture sensitivity testing. Ibrahiem et al. reported that among 127 MRSA isolates that were recovered from 268 clinical samples collected from different locations in Egypt, the percentage of vancomycin-resistant isolates was 23.62% [43]. Another study conducted in Egypt revealed that the prevalence of VRSA was 21.7% [44]. The former observations indicate an alarming increase in vancomycin resistance in different areas of Egypt that could be attributed to the overuse of vancomycin for treating MRSA infections. As a result, there is an urgent need to establish adequate surveillance for antibiotic resistance and implement a restricted antibiotic policy in Egyptian hospitals.
We screened the tested MRSA isolates for their SCCmec types (I–V) in the mecA-positive isolates. SCCmec types I, II, and/or III were reported in HA-MRSA isolates [45], whereas SCCmec-variant genes IV and V were detected in CA-MRSA isolates [46,47,48]. In the present study, type V SCCmec was the most prevalent among PVL-positive MRSA isolates (41.67%), compared to PVL-negative isolates (14.53%). The SCCmec gene variant type IV, which was commonly reported in CA-MRSA [49], was equally associated with PVL-positive (22.92%) and PVL-negative (23.62%) MRSA isolates. The most prevalent SCCmec type among the PVL-negative isolates was type I, as previously reported [50], and its incidence rate in our study is 29.09%. On the contrary, type II was not detected in any of the PVL-positive or negative isolates. PVL genes have been previously reported as markers for CA-MRSA [50].
In the current study, the carriage of MRSA isolates by HCWs was 61.7%, reflecting their major role in spreading MRSA in tertiary hospitals and the community of Dakahlia Governorate. Therefore, there is a need for rapid identification of MRSA and appropriate infection control measures for MRSA infection. Also, improving compliance, reducing antibiotic overuse, screening HCWs for carriage of S. aureus, and decolonization are necessary strategies. The high incidence of PVL-positive MRSA suggests that it is not a good marker for community MRSA in Egypt.
Conclusions and future perspectives
In conclusion, there is an alarmingly high prevalence of MDR in PVL-positive and negative MRSA in tertiary hospitals and in the community in Mansoura, Dakahlia Governorate. This necessitates the reduction of the excessive use of antibiotics and the implementation of MRSA control measures in tertiary hospitals in Dakahlia Governorate. The high incidence of PVL-MRSA in HA, CA, and HCWs in this study suggests that PVL is not a valid marker for CA-MRSA in Dakahlia Governorate, Egypt. Further epidemiologic studies using different molecular typing techniques should be conducted to identify the circulating MRSA clone complexes (CCs), and their sequence type and relate the isolates to their origin, whether CA or HA in Dakahlia Governorate, Egypt.
Data Availability
All data generated or analysed during this study are included in this published article.
References
Tong SYC, Davis JS, Eichenberger E, Holland TL, Fowler VG. Staphylococcus aureus Infections: epidemiology, pathophysiology, clinical manifestations, and management. Clin Microbiol Rev. 2015;28(3):603–61. https://doi.org/10.1128/CMR.00134-14. Pubmed:26016486.
Preeja PP, Kumar SH, Shetty V. Prevalence and characterization of methicillin-resistant staphylococcus aureus from community- and hospital-associated Infections: a tertiary care center study. Antibiot (Basel). 2021;10(2):1–10. https://doi.org/10.3390/antibiotics10020197. Pubmed:33670648.
Bush K, Bradford PA. β-lactams and β-lactamase Inhibitors: an Overview. Cold Spring Harb Perspect Med. 2016 1 Aug;6(8):a025247. https://doi.org/10.1101/cshperspect.a025247. PMID: 27329032. PMCID: PMC4968164.
European Food Safety Authority (EFSA), European Centre for Disease Prevention and Control (ECDC). The European Union Summary Report on antimicrobial resistance in zoonotic and indicator bacteria from humans, animals and food in 2020/2021. EFSA J. 2023;6(3):e07867. https://doi.org/10.2903/j.efsa.2023.7867.
Nikaido H. Multidrug resistance in bacteria. Annu Rev Biochem. 2009;78:119–46. https://doi.org/10.1146/annurev.biochem.78.082907.145923. Pubmed:19231985.
Hanssen AM, Kjeldsen G, Sollid JU. Local Variants of Staphylococcal Cassette Chromosome mec in Sporadic methicillin-Resistant Staphylococcus aureus and methicillin-Resistant coagulase-Negative Staphylococci: evidence of Horizontal Gene Transfer? Antimicrob Agents Chemother. 2004;48(1):285 – 96. https://doi.org/10.1128/AAC.48.1.285-296.2004, Pubmed:14693553.
Paterson GK, Harrison EM, Holmes MA. The emergence of mecC methicillin-resistant Staphylococcus aureus. Trends Microbiol. 2014;22(1):42–7. https://doi.org/10.1016/j.tim.2013.11.003. PMID: 24331435; PMCID: PMC3989053.
David MZ, Daum RS. Community-associated methicillin-resistant Staphylococcus aureus: epidemiology and clinical consequences of an emerging epidemic. Clin Microbiol Rev. 2010;23(3):616–87. https://doi.org/10.1128/CMR.00081-09. Pubmed:20610826.
Wójcik-Bojek U, Różalska B, Sadowska B. Staphylococcus aureus-A known opponent against Host Defense Mechanisms and Vaccine Development-Do we still have a chance to Win? Int J Mol Sci. 2022;23(2). https://doi.org/10.3390/ijms23020948. Pubmed:35055134.
Vandenesch F, Naimi T, Enright MC, Lina G, Nimmo GR, Heffernan H, et al. Community-acquired methicillin-resistant Staphylococcus aureus carrying panton-valentine leukocidin genes: worldwide emergence. Emerg Infect Dis. 2003;9(8):978–84. https://doi.org/10.3201/eid0908.030089. Pubmed:12967497.
Nakaminami H, Ozawa K, Sasai N, Ikeda M, Nemoto O, Baba N, et al. Current status of Panton–Valentine leukocidin-positive methicillin-resistant Staphylococcus aureus isolated from patients with skin and soft tissue Infections in Japan. J Dermatol. 2020;47(11):1280–6. https://doi.org/10.1111/1346-8138.15506. Pubmed:32696497.
El-Baghdady KZ, El-Borhamy MI, Abd El-Ghafar HA. Prevalence of resistance and toxin genes in community-acquired and hospital-acquired methicillin-resistant Staphylococcus aureus clinical isolates. Iran J Basic Med Sci. 2020;23(10):1251–60. https://doi.org/10.22038/ijbms.2020.40260.9534. Pubmed:33149856.
CLSI, Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing; twenty-fifth informational supplement. CLSI Doc. 2015;M100:25.
Sheneef A, Goda AM, Ftohy TE. Staphylococcal Cassette chromosome mec typing of community – acquired methicillin – resistant Staphylococcus aureus isolates in Sohag University Hospital, Egypt. Egypt EJMM. 2017;26(2):111–7. https://doi.org/10.12816/0046236.
Ferri M, Ranucci E, Romagnoli P, Giaccone V. Antimicrobial resistance: a global emerging threat to public health systems. Crit Rev Food Sci Nutr. 2017;57(13):2857–76. https://doi.org/10.1080/10408398.2015.1077192. Pubmed:26464037.
Kourtis AP, Hatfield K, Baggs J, Mu Y, See I, Epson E et al. Vital signs: epidemiology and recent trends in methicillin-resistant and in methicillin-susceptible Staphylococcus aureus bloodstream infections – United States. MMWR Morb Mortal Wkly Rep. 2019;68(9):214-9. https://doi.org/10.15585/mmwr.mm6809e1, Pubmed:30845118.
ECDC. ; 2017. ECDC: surveillance report. Surveillance of Antimicrobial Resistance in Europe 2016 [Internet]. https://ecdc.europa.eu/en/publications-data/antimicrobial-resistance-surveillance-europe-2016.
Schaumburg F, Alabi AS, Peters G, Becker K. New epidemiology of Staphylococcus aureus Infection in Africa. Clin Microbiol Infect. 2014;20(7):589–96. https://doi.org/10.1111/1469-0691.12690. Pubmed:24861767.
Alfeky AE, Tawfick MM, Ashour MS, El-Moghazy AA. High prevalence of multi-drug resistant methicillin-resistant Staphylococcus aureus in tertiary Egyptian hospitals. J Infect Dev Ctries. 2022;16(5):795–806. https://doi.org/10.3855/jidc.15833. Pubmed:35656950.
Abouelfetouh A. The status of methicillin resistance among Egyptian Staphylococcus aureus isolates: an overview. Infect Disord Drug Targets. 2017;17(1):67–9. doi: 10.2174/1871526516666160802111200, Pubmed:27488498.
Gould IM, David MZ, Esposito S, Garau J, Lina G, Mazzei T, Peters G. New insights into meticillin-resistant Staphylococcus aureus (MRSA) pathogenesis, treatment and resistance. Int J Antimicrob Agents. 2012;39(2):96–104. https://doi.org/10.1016/j.ijantimicag.2011.09.028, Pubmed:22196394.
Bhatta DR, Cavaco LM, Nath G, Kumar K, Gaur A, Gokhale S, Bhatta DR. Association of Panton Valentine Leukocidin (PVL) genes with methicillin resistant Staphylococcus aureus (MRSA) in Western Nepal: A matter of concern for community Infections (a hospital based prospective study). BMC Infect Dis. 2016;16(1):1–6. https://doi.org/10.1186/s12879-016-1531-1.
Linde H, Wagenlehner F, Strommenger B, Drubel I, Tanzer J, Reischl U et al. Healthcare-associated outbreaks and community-acquired infections due to MRSA carrying the Panton-Valentine leucocidin gene in southeastern Germany. Eur J Clin Microbiol Infect Dis. 2005;24(6):419 – 22. https://doi.org/10.1007/s10096-005-1341-7, Pubmed:15937659.
Scarnato F, Mallaret MR, Croizé J, Kouabenan DR, Dubois M, Maitre A, DeGaudemaris R. Incidence and prevalence of methicillin-resistant Staphylococcus aureus nasal carriage among healthcare workers in geriatric departments: relevance to preventive measures. Infect Control Hosp Epidemiol. 2003;24(6):456-8. https://doi.org/10.1086/502232, Pubmed:12828325.
Havaei SA, Moghadam SO, Pourmand MR, Faghri J. Prevalence of genes encoding bi-component leukocidins among clinical isolates of Methicillin Resistant Staphylococcus aureus. Iran J Public Health. 2010;39(1):8–14. Pubmed:23112984.
Miller LG, Perdreau-Remington F, Rieg G, Mehdi S, Perlroth J, Bayer AS et al. Necrotizing fasciitis caused by community-associated methicillin-resistant Staphylococcus aureus in Los Angeles. N Engl J Med. 2005;352(14):1445-53. https://doi.org/10.1056/NEJMoa042683, Pubmed:15814880.
Hora DK, Kamaraki M, Rao GG, Nielsen PB. How common is PVL positive MRSA in adult emergency admissions? Findings of the first UK study. J Infect. 2009;59(6). https://doi.org/10.1016/j.jinf.2009.10.027.
Klein S, Hannesen J, Zanger p, Heeg K. SB& D nurjadi1. Entry of Panton–Valentine leukocidin-positive methicillin-resistant Staphylococcus aureus into the hospital: prevalence and population structure in Heidelberg, Germany 2015–2018.
Rossney AS, Shore AC, Morgan PM, Fitzgibbon MM, O’Connell B, Coleman DC. The emergence and importation of diverse genotypes of methicillin-resistant Staphylococcus aureus (MRSA) harboring the panton-valentine leukocidin gene (pvl) reveal that pvl is a poor marker for community-acquired MRSA strains in Ireland. J Clin Microbiol. 2007;45(8):2554-63. https://doi.org/10.1128/JCM.00245-07, Pubmed:17581935.
Wannet WJB, Spalburg E, Heck MEOC, Pluister GN, Tiemersma E, Willems RJL et al. Emergence of virulent methicillin-resistant Staphylococcus aureus strains carrying panton-valentine leucocidin genes in the Netherlands. J Clin Microbiol. 2005;43(7):3341-5. https://doi.org/10.1128/JCM.43.7.3341-3345.2005, Pubmed:16000458.
Yu F, Chen Z, Liu C, Zhang X, Lin X, Chi S, et al. Prevalence of Staphylococcus aureus carrying Panton-valentine leukocidin genes among isolates from hospitalized patients in China. Clin Microbiol Infect. 2008;14(4):381–4.
Yılmaz S, Calikoglu EO, Kosan Z. for an Uncommon Neurosurgical Emergency in a Developing Country. Prevalence of obesity among adolescents in Eastern Turkey: a cross-sectional study with a review of the local literature. Niger J Clin Pract. 2019;22(8):1070-7. https://doi.org/10.4103/njcp.njcp_418_18, Pubmed:31417049.
van der Mee-Marquet N, Poisson DM, Lavigne JP, Francia T, Tristan A, Vandenesch F et al. The incidence of Staphylococcus aureus ST8-USA300 among French pediatric inpatients is rising. Eur J Clin Microbiol Infect Dis. 2015;34(5):935 – 42. https://doi.org/10.1007/s10096-014-2308-3, Pubmed:25575950.
Al sweify M, Aboul-Atta H, El-Hadidy G, Hessam W, Raheel A. Identification of CA-MRSA causing hospital-acquired Infections in Suez Canal University hospitals, Egypt, by detection of its major virulence determinants. Microbes Infect Dis. 2020;0:0. https://doi.org/10.21608/mid.2020.41062.1057.
Enany S, Yaoita E, Yoshida Y, Enany M, Yamamoto T. Molecular characterization of Panton-Valentine leukocidin-positive community-acquired methicillin-resistant Staphylococcus aureus isolates in Egypt. Microbiol Res. 2010;165(2):152–62. https://doi.org/10.1016/j.micres.2009.03.005. Pubmed:19616420.
Hefzy EM, Hassan GM, Abd El Reheem F. Detection of panton-valentine leukocidin-positive methicillin-resistant Staphylococcus aureus nasal carriage among Egyptian health care workers. Surg Infect (Larchmt). 2016;17(3):369–75. https://doi.org/10.1089/sur.2015.192.
Dow G, Field D, Mancuso M, Allard J. Decolonization of methicillin-resistant Staphylococcus aureus during routine hospital care: efficacy and long-term follow-up. Can J Infect Dis Med Microbiol. 2010;21(1):38–44. https://doi.org/10.1155/2010/590530. Pubmed:21358884.
Magiorakos AP, Srinivasan A, Carey RB, Carmeli Y, Falagas ME, Giske CG et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18(3):268 – 81. https://doi.org/10.1111/j.1469-0691.2011.03570.x, Pubmed:21793988.
El-Baz AM, Yahya G, Mansour B, El-Sokkary MMA, Alshaman R, Alattar A, El-Ganiny AM. The link between occurrence of class I integron and acquired aminoglycoside resistance in clinical MRSA isolates. Antibiotics (Basel). 2021;10(5):1–14. https://doi.org/10.3390/antibiotics10050488, Pubmed:33922421.
Xu Z, Li L, Shi L, Shirtliff ME. Class 1 integron in staphylococci. Mol Biol Rep. 2011;38(8):5261-79. https://doi.org/10.1007/s11033-011-0676-7, Pubmed:21258866.
Ali HA, El-Mahdy RH, Gaballah MA. Community-acquired methicillin-resistant Staphylococcus aureus colonization in atopic dermatitis patients in Mansoura, Egypt. Biomed Dermatol. 2019;3(1):1–5. https://doi.org/10.1186/s41702-019-0040-4.
Alseqely M, Newton-Foot M, Khalil A, El-Nakeeb M, Whitelaw A, Abouelfetouh A. Association between fluoroquinolone resistance and MRSA genotype in Alexandria, Egypt. Sci Rep. 2021;11(1):4253. https://doi.org/10.1038/s41598-021-83578-2. Pubmed:33608606.
Ibrahiem W, Rizk D, Kenawy H, Hassan R. Prevalence of Vancomycin resistance among clinical isolates of MRSA from different governorates in Egypt. Egypt J Med Microbiol. 2022;31(4):5–14. https://doi.org/10.21608/ejmm.2022.262673.
Mashaly M, El-Mashad N, El-deeb H. Detection of VanA type Vancomycin resistance among MRSA isolates from an emergency hospital in Egypt. Comp Clin Pathol. 2019;28(4):971–6. https://doi.org/10.1007/s00580-018-2858-3.
Ito T, Katayama Y, Asada K, Mori N, Tsutsumimoto K, Tiensasitorn C, Hiramatsu K. Structural comparison of three types of Staphylococcal Cassette chromosome Mec Integrated in the chromosome in Methicillin-Resistant Staphylococcus aureus. Antimicrob Agents Chemother. 2001;45(12):3677. https://doi.org/10.1128/AAC.45.12.3677-3677.2001.
Berglund C, Ito T, Ikeda M, Ma XX, Söderquist B, Hiramatsu K. Novel type of staphylococcal cassette chromosome mec in a methicillin-resistant Staphylococcus aureus strain isolated in Sweden. Antimicrob Agents Chemother. 2008;52(10):3512-6. https://doi.org/10.1128/AAC.00087-08, Pubmed:18676883.
Ito T, Ma XX, Takeuchi F, Okuma K, Yuzawa H, Hiramatsu K. Novel type V staphylococcal cassette chromosome mec driven by a novel cassette chromosome recombinase, ccrC. Antimicrob Agents Chemother. 2004;48(7):2637-51. https://doi.org/10.1128/AAC.48.7.2637-2651.2004, Pubmed:15215121.
Daum RS, Ito T, Hiramatsu K, Hussain F, Mongkolrattanothai K, Jamklang M, Boyle-Vavra S. A novel methicillin-resistance cassette in community-acquired methicillin-resistant Staphylococcus aureus isolates of diverse genetic backgrounds. J Infect Dis. 2002;186(9):1344-7. https://doi.org/10.1086/344326, Pubmed:12402206.
Wong H, Louie L, Lo RYC, Simor AE. Characterization of Staphylococcus aureus isolates with a partial or complete absence of staphylococcal cassette chromosome elements. J Clin Microbiol. 2010;48(10):3525-31. https://doi.org/10.1128/JCM.00775-10, Pubmed:20668131.
Boye K, Bartels MD, Andersen IS, Møller JA, Westh H. A new multiplex PCR for easy screening of methicillin-resistant Staphylococcus aureus SCCmec types I-V. Clin Microbiol Infect. 2007;13(7):725-7. https://doi.org/10.1111/j.1469-0691.2007.01720.x, Pubmed:17403127.
Lina G, Piémont Y, Godail-Gamot F, Le Bes M, Peter MO, Gauduchon V et al. Involvement of panton-valentine leukocidin-producing Staphylococcus aureus in primary skin infections and pneumonia. [cited 2022 11]; doi.Clin Infect Dis. 1999;29(5):1128-32. https://doi.org/10.1086/313461, Pubmed:10524952.
Acknowledgements
The authors extend their appreciation to the staff of Microbiology laboratory at Mansoura University Teaching Hospitals for facilitating the collection of the clinical isolates.
Funding
The authors declare that no funds, grants, or other support were received for the preparation of this manuscript.
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
Mohamed Shohayeb and Tarek El-Banna; Data curation, Maisra El-Bouseary and Lamis Elsawy; Formal analysis, Lamis Elsawy, Maisra El-Bouseary Mohamed Shohayeb and Tarek El-Banna; Methodology, Lamis Elsawy, Maisra El-Bouseary Mohamed Shohayeb and Tarek El-Banna; Visualization, Maisra El-Bouseary and Lamis Elsawy; Writing – original draft, Lamis Elsawy; Writing – reviewing & editing, Maisra El-Bouseary, Tarek El-Banna and Mohamed Shohayeb. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
The study was conducted in accordance with the Declaration of Helsinki and approved by the Research Ethics Committee Review Board (FPDU-REC), Faculty of Pharmacy, Tanta University (FPDU18/2022).
Consent to participate
Written informed consent was obtained from each participant.
Consent for publication
not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Shohayeb, M., El-Banna, T., Elsawy, L.E. et al. Panton-Valentine Leukocidin (PVL) genes may not be a reliable marker for community-acquired MRSA in the Dakahlia Governorate, Egypt. BMC Microbiol 23, 315 (2023). https://doi.org/10.1186/s12866-023-03065-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12866-023-03065-8