Abstract
Background
In 2018, about 10 million people were found infected by tuberculosis, with approximately 1.2 million deaths worldwide. Despite these numbers have been relatively stable in recent years, tuberculosis is still considered one of the top 10 deadliest diseases worldwide. Over the years, Mycobacterium tuberculosis has developed a form of resistance to first-line tuberculosis treatments, specifically to isoniazid, leading to multi-drug-resistant tuberculosis. In this context, the EU and Indian DBT funded project STriTuVaD—In Silico Trial for Tuberculosis Vaccine Development—is supporting the identification of new interventional strategies against tuberculosis thanks to the use of Universal Immune System Simulator (UISS), a computational framework capable of predicting the immunity induced by specific drugs such as therapeutic vaccines and antibiotics.
Results
Here, we present how UISS accurately simulates tuberculosis dynamics and its interaction within the immune system, and how it predicts the efficacy of the combined action of isoniazid and RUTI vaccine in a specific digital population cohort. Specifically, we simulated two groups of 100 digital patients. The first group was treated with isoniazid only, while the second one was treated with the combination of RUTI vaccine and isoniazid, according to the dosage strategy described in the clinical trial design. UISS-TB shows to be in good agreement with clinical trial results suggesting that RUTI vaccine may favor a partial recover of infected lung tissue.
Conclusions
In silico trials innovations represent a powerful pipeline for the prediction of the effects of specific therapeutic strategies and related clinical outcomes. Here, we present a further step in UISS framework implementation. Specifically, we found that the simulated mechanism of action of RUTI and INH are in good alignment with the results coming from past clinical phase IIa trials.
Similar content being viewed by others
Background
Tuberculosis (TB), a disease caused by Mycobacterium tuberculosis (MTB) infection, is still one of the top 10 causes of death worldwide, especially in emerging countries. According to the World Health Organization (WHO), in 2018 10 million people fell ill with tuberculosis, of which 5.7 million were men, 3.2 million women, and 1.1 million children [1]. TB spreads from person to person through aerosol transmission. As today, no one is immune or isolated from the risk of being affected by the disease [2], and no prophylactic vaccines are available. Recently, bedaquiline and delamanid were approved as new two anti‐TB drugs, while novel candidates and repurposed drug have been developed and are in the final stages of drug development process [3].
Commonly, first-line TB treatments (isoniazid (INH), rifampin (RIF), pyrazinamide (PZA), ethambutol (EMB) and streptomycin (SM) [4]) are used for active tuberculosis in order to reduce the bacterial load in the lungs and the probability of transmission. INH, already known as isonicotinic acid hydrazide [5], is one of the leading standard antibiotic treatments for people at low risk for drug-resistance, leading to a significant reduction of mycobacterial load [6]. INH inhibits the synthesis of mycolic acids, an essential component of the bacterial cell wall, and is used in conjunction with other effective anti-tuberculosis agents in a multi-drug therapy protocol [7]. INH has a short half-life ranging from 1 to 4 h [8] and a double-activity: for the first 24 h from the administration, INH shows a bacteriostatic mechanism, then its activity becomes bactericidal [9,10,11]. This pro-drug requires a preliminary activation, which is carried out by the heme enzyme catalase/peroxidase (KatG) of MTB [12]. The interactions between the host immune system and INH allow to decrease the growth of intracellular and extracellular MTB bacilli. It is worth mentioning that the active form of tuberculosis should be treated with different combinations of anti-tuberculosis drugs to prevent the emergence of drug resistance phenomena. This is due to the fact that the single use of isoniazid for active tuberculosis is not always effective. The high bactericidal activity, the elevated intracellular penetration, and the low costs make INH one of the most commonly used antimicrobial agents to fight tuberculosis.
Second-line drugs are sub-divided into two categories: fluoroquinolones (ofloxacin (OFX), levofloxacin (LEV), moxifloxacin (MOX) and ciprofloxacin (CIP) and injectable antituberculosis drugs (kanamycin (KAN), amikacin (AMK) and capreomycin (CAP). Other second-line antituberculosis (ethionamide (ETH)/prothionamide (PTH), cycloserine (CS)/terizidone, p-aminosalicylic acid (PAS) [4]) are used for the treatment of drug-resistant and multi-drug-resistant TB patients. However, second-line treatment options own some disadvantages because they require very long treatment regimens, along with a toxic exposure and high costs for the patients.
To overcome these issues, many EU-funded projects are trying to fight TB with specific trials concerning new therapeutic strategies. Among these, the HORIZON 2020 In Silico Trial for Tuberculosis Vaccine Development (STriTuVaD) project aims to evaluate a specific therapeutic vaccine against tuberculosis through an innovative computational modelling infrastructure named Universal Immune System Simulator (UISS). In this context, UISS for Tuberculosis (UISS-TB) is capable to reproduce the dynamics of the immune system affected by TB and predict the outcome of a real clinical trial under the administration of specific interventions such as the RUTI vaccine [13].
RUTI vaccine is a polyantigenic liposomal vaccine previously used as an immunotherapeutic intervention during antibiotic treatment for Multi-Drug-Resistant Tuberculosis (MDR-TB). This vaccine showed an excellent safety profile in a phase 2 trial [14], and has the potential to reduce the time required for the current antibiotic treatments significantly.
To investigate the effects of the combination of a conventional anti-TB chemotherapy strategy with a potential therapeutic vaccine such as RUTI, we present here an extension of our pre-existing version of UISS-TB able to predict their combined efficacy.
Methods
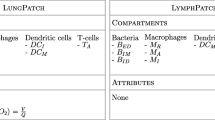
UISS computational framework, widely discussed in [13], was successfully applied to a large number of disease modelling scenarios [15,16,17], including COVID-19 [18]. UISS is based on Agent-Based Model (ABM) methodology [19, 20] that predicts the efficacy of vaccines and/or antibiotics treatments targeting MTB in a specific digital patients cohort.
To simulate the effects of isoniazid, we implemented in UISS its mechanism of action and modeled the effects on MTB using the administration protocol described in [14] for one month.
To this end, we added INH as a new entity (also called “agent” in ABM terminology) into the simulation framework. INH agents are described through their concentration in each position of simulation space and their half-life, used by the simulation framework to calculate the degradation of INH and to manage the bacteriostatic and bactericidal activities. INH injection time and quantities are defined according to the administration protocol described in [14]. The interaction that describes the effects of INH against MTB can be briefly reassumed as follows. The bacteriostatic effect was implemented considering infected AM cells that encounter INH formulation within the lung compartment. With a probability dependent on INH concentration, the intracellular and extracellular replication rates of MTB are reduced. The mathematical law that describes the intracellular and extracellular proliferation of MTB has been implemented with a method similar to the one described in [21, 22]. The bactericidal activity of INH affects the circulating TB bacilli. With a probability depending on INH concentration, circulating TB bacilli are cleared from the bloodstream.
Moreover, we also revised the RUTI implementation in UISS, to better model the mechanism of action (MoA) and the vaccine interaction with the host immune system. According to RUTI formulation, we added the liposome entity and its related dynamics. At the beginning of each simulation, the user provides UISS with two parameters: i) RUTI dosage and ii) the time of the administration. The aim was to allow UISS to simulate the interaction between the liposome and dendritic cell (DC). In particular, when in the lymph node compartment, a naïve DC encounters a liposome, DC scans the surface of the liposome to recognize the MHC-1/peptide complex. Through the calculation of a proportional probability function that depends on the affinity level between DC pattern recognition receptor (DC-PRR) and MHC-1/peptide complex expressed on the surface of the liposome. This immunological process led by DC is known as nibbling. Finally, the liposome—CD8 T cells (TC) interaction has been added. If the interaction succeeds, i.e., TC recognizes the MHC-I/liposome peptide on the liposome surface (by affinity score calculation), the TC releases a predefined quantity of interferon gamma (IFN-γ) in situ. The release of free antigens through the liposomes (due to physiological degradation) over time has also been considered.
To better represent the biological diversity of TB patients, we enriched the composition of the vector of features used for the generation of digital patients libraries. In particular, the "vector of features" that defines a specific TB patient is composed by the following parameters: (1) MTB virulence; (2) MTB Sputum; (3) CD4-Th1; (4) CD4-Th2; (5) IgG; (6) TC; (7) IL-23; (8) IL-12; (9) IL17-A; (10) IL-2; (11) IL-1; (12) IL-10; (13) IFN1A; (14) IFN1B; (15) IFNG; (16) TNF; (17) Treg; (18) LXA4; (19) PGE2; (20) Vitamin D; (21) Age; (22) BMI. The digital patients were generated according to the steps explained in [23]. Table 1 summarizes the biological description of each entity that composes the vector of features, specifying the unit of measurements and the values used to run the simulations.
As UISS is written in C language, a Graphic User Interface (GUI) and a web server is needed to provide a user-friendly interface. In a previous work, we presented a web-interface developed in Flask micro-server [24]. Here, we improved the performance of the web platform. These enhancements allow the launch of the simulations separately from the main thread and in a more efficient way. To this aim, we used Django, the high-level Python Web framework. Figure 1 shows the last version of the UISS web-GUI. On the right side, one can see a box called "Your simulation" containing a list of the simulations, sorted by their creation date and classified in "running" or in "completed" status. On the left side, one can see a box named "Simulation Parameters" that contains a set of the biological and physiopathological parameters that compose the vector of features, created for the customization of TB patients.
Web Graphic User Interface of UISS-TB. This figure depicts the GUI of UISS that allows the run of the simulations. The "Simulation's Parameters" zone, on the left side of the figure represents the vector of features for the personalization of digital patients. The "Your Simulations" box, on the right side of the figure, depicts the list of all the simulations launched by the user. The simulations are classified in "running" or in "completed" status
In details, after the user connects to the UISS-TB web interface, she/he selects the Tuberculosis disease model. After that, the general GUI panel appears. The user finds already filled in default values in the vector of features parameters. She/he can vary these values according to the ranges that are shown within brackets, near the selected parameter. After that, one can press the Submit button and a unique identification simulation number is assigned. The user can check the simulation status simply clicking on the check status button, after selecting the simulation id. When the simulation is completed, the user can visualise results of immune system dynamics, simply choosing the one she/he would like to analyze.
Results and discussion
A first step in moving UISS towards clinical validation was to evaluate its prediction capabilities. In this context, we designed different simulations over cohorts of digital patients to obtain accurate in silico predictions about the efficacy of therapeutic interventions directed against TB. We run a total of 400 simulations, within four different scenarios: (1) 100 digital patients treated with INH only; (2) 100 digital patients treated with the combination of INH and RUTI vaccine; (3) 100 digital patients treated with the combination of INH and two RUTI vaccine administrations; (4) 100 digital patients treated with the combination of INH and two RUTI vaccine administrations, at different timing. We took into account only drug-sensitive digital patients (i.e., not affected by MDR-TB). MTB infection peaks after two weeks from the starting of the simulation.
In order to show the effects of RUTI vaccination protocol complemented with the administration of INH on the host immune system, we tracked the dynamics of Alveolar Macrophages (AM), CD4 Th1, Interferon-gamma (IFN-γ), Cytotoxic T cells (TC), CD4 Th17. In Figs. 2 and 3, the mean behavior (green line) and standard deviation (orange shaded region) of the biological entities taken into consideration are depicted. Untreated TB digital patients have been widely discussed in [13, 24]. Figure 2 shows the cellular dynamics where an initial challenge with a virulent strain of MTB is supposed to happen on day 15. Soon after, we simulated the injection of INH once a day for one month. Figure 2, panel A shows the dynamics of AM; here, we can observe a not negligible reduction of the average population of necrotic AM. In other words, the injection of INH allows a tissue recovery of the lung's patient. Regarding cytotoxic CD8 T cells, Fig. 2, panel B shows no significant differences from the untreated cases. This is in good agreement with clinical observations as INH antibiotic therapy does not affect immune system behavior. Accordingly, panel C and panel E of Fig. 2 shows no Th1 cell activation and no IFN-γ presence [25].
Outcome of digital patients treated with INH. Green line shows the average trend of the considered cellular entities. The orange shaded area represents their standard deviation (SD + /−). a Depicts the dynamics of AM before and after the administration of INH; the antibiotic, administered accordingly to the clinical trial protocol, reveals a not negligible biological restore of the damaged AM. b The dynamics of CD8 T cells. d The dynamics of TH17 cells responding to bacterial infection. c and e show flat curves because INH is not supposed to stimulate immune response. Simulation time has been set to 365 days (1 years) and digital patients have been challenged with MTB at day 15
Outcome of digital patients treated with INH and RUTI vaccine. Green line shows the average trend of cell populations, while the orange shaded area represents the standard deviation. One month after the end of antibiotic treatment, RUTI vaccine was administered accordingly to the clinical trial design. a Depicts the dynamics of AM before and after the administration of INH and after the administration of RUTI. The combination of INH with RUTI allows a better recovery of infected AM population when compared to the one without RUTI injection. Substantial increase in levels of TC, Th1, Th17 and IFNG is observed (b–e). For all the biological scenarios, simulation time has been set to 365 days (1 years) and digital patient have been challenged with MTB at day 15
Th17 cells are a subpopulation of helper T cells. Their production is stimulated by cytokines such as IL-6, IL-1, and IL-23, produced in response to extracellular bacteria, such as in tuberculosis [25]. They are involved in the recruitment of leukocytes to the infection site and have an essential role in the elimination of bacteria. Figure 2 panel D, depicts the increase of Th17 cells in response to MTB infection. After an initial burst, Th17 number gradually reduces as patients convert into latent tuberculosis [26].
Figure 3 shows the second scenario in which the administration of RUTI vaccine is coupled with INH. As above, we kept the MTB challenge on day 15, followed by INH administration (once a day per one month). This time, one month after the end of the antibiotic treatment, an injection of 25 μg of RUTI vaccine was simulated.
Panel A, Fig. 3 depicts the dynamics of AM. In this case, one can see as RUTI significantly reduces the AM necrotic population. According to literature, panel B of Fig. 3 highlights an increased activation of CD8+ T cells. The diminution of CD8+ T cells in the latent stage of the infection led to an increase in the bacterial load, which indicates that these cells are necessary for the long-term control of the disease [27]. This could suggest that a second RUTI administration could be beneficial to the MTB eradication. Figure 3 panel C shows a considerable Th1 response that is also supported by a not negligible release of IFN-γ (panel E). There is also an increased activation of Th17 (panel D). Reassuming, the RUTI orchestrated immune response is in very good agreement with specialized literature [14].
Figure 4 shows the results of the second RUTI injection as reported in the clinical protocol design [28]. In comparison to the immune response obtained with one RUTI administration as previously shown in Fig. 3, here one notices a stronger CD4+ Th1 response (panel C) followed by an increased IFN- γ levels (panel E). Moreover, also CD8+ T cell response (panel B) is positively triggered by the second administration of RUTI.
Outcome of digital patients treated with the second RUTI vaccine administration. Green line shows the average trend of cell populations, while the orange shaded area represents the standard deviation. One month after the end of antibiotic treatment, RUTI vaccine was administered accordingly to the clinical trial design followed by a second injection of RUTI (28 days after the first one). a The dynamics of AM that is comparable to the scenario observed after only one vaccine administration. Substantial increase in levels of TC, Th1, Th17 and IFNG is observed (b–e) compared to dynamics obtained with only one vaccine administration. For all the biological scenarios, simulation time has been set to 365 days (1 years) and digital patient have been challenged with MTB at day 15
To assess if a different timing of a second RUTI injection could improve the overall immune response of the host against MTB, we simulated a later second injection time compared to the clinical trial protocol design (i.e., at day 200, about three months after the one set in the clinical trial). In Fig. 5, we report the in silico predictions of such a different timing of second RUTI administration. A negligible difference in the overall immune response driven by CD4+ Th1 cells and CD8+ T cells is observed. This suggests that the timing agreed in the clinical trial dossier corresponds to the optimal one.
UISS in silico predictions with different timing of a second RUTI vaccine administration. Green line shows the average trend of cell populations, while the orange shaded area represents the standard deviation. In comparison to the scenarios observed in Fig. 4, a negligible difference in the overall immune response driven by CD4+ Th1 cells and CD8+ T cells is observed
Conclusions
In silico trials are increasingly used to predict the effects of several types of interventional strategies and related clinical outcomes. In this context, the EC and Indian DBT funded project STriTuVaD aims to create a computational infrastructure that predicts the efficacy of antibiotic strategies when coupled with RUTI vaccine against M. tuberculosis. Here, we present a further step in UISS framework implementation toward the clinical validation of the platform. We found that the simulated MoA of RUTI and INH is in proper alignment with the double-blind, randomized, placebo-controlled phase II clinical trial. To explore potential possibilities to increase the overall immune response against MTB, we simulated 100 digital patients treated with INH and two RUTI vaccine administrations varying the timing of the second one. In silico results confirm that the overall immune response driven by CD4+ Th1 cells and CD8+ T cells is not influenced, suggesting that the timing agreed in the clinical trial protocol is optimal.
Availability and requirements
Project name UISS-TB.
Project home page https://www.combine-group.org/software.
Operating system(s) Platform independent.
Programming language C and Python.
Other requirements none.
Any restrictions to use by non-academics not applicable.
Availability of data and materials
The main computational framework is fully described in the paper. The UISS-TB framework used for this research is available at: https://combine.dmi.unict.it/UISS-TB/.
Abbreviations
- TB:
-
Tuberculosis
- MTB:
-
Mycobacterium tuberculosis
- STriTuVaD:
-
In Silico Trial for Tuberculosis Vaccine Development
- UISS:
-
Universal Immune System Simulator
- INH:
-
Isoniazid
- MDR-TB:
-
Multidrug-resistant tuberculosis
- WHO:
-
World Health Organization
- ABM:
-
Agent-based modeling
- KatG:
-
Heme enzyme catalase/peroxidase
- MHC-I:
-
Major histocompatibility complex class I
- MHC-II:
-
Major histocompatibility complex class II
- APC:
-
Antigen processing cell
- MoA:
-
Mechanism of action
- IgG:
-
Immunoglobulin class G
- AM:
-
Alveolar macrophage
- N:
-
Neutrophils
- LXA4:
-
Lipoxin A4
- PGE2:
-
Prostaglandin E2
- IFN-γ:
-
Interferon-gamma
- TReg:
-
Regulatory T cells
- TC:
-
Cytotoxic T cells
- TNF:
-
Tumor necrosis factor
- GUI:
-
Graphic user interface
References
WHO. Global tuberculosis report 2019. 2019.
Glaziou P, Floyd K, Raviglione MC. Global epidemiology of tuberculosis. Semin Respir Crit Care Med. 2018;39:271–85.
Bahuguna A, Rawat DS. An overview of new antitubercular drugs, drug candidates, and their targets. Med Res Rev. 2020;40:263–92.
Nath H, Ryoo S. First- and second-line drugs and drug resistance. In: Tuberculosis—current issues in diagnosis and management. InTech; 2013. p. 13. https://doi.org/10.5772/54960.
Timmins GS, Deretic V. Mechanisms of action of isoniazid. Mol Microbiol. 2006;62:1220–7.
Meller HJM. Hydrazine derivatives of pyridinecarboxylic acids. Monatsschr Psychiatr. 1912;33:400.
Favrot L, Ronning DR. Targeting the mycobacterial envelope for tuberculosis drug development. Expert Rev Anti Infect Ther. 2012;10:1023–36.
Tiwari S, Chaturvedi AP, Tripathi YB, Mishra B. Macrophage-specific targeting of isoniazid through mannosylated gelatin microspheres. AAPS PharmSciTech. 2011;12:900–8.
Middlebrook G. Sterilization of tubercle bacilli by isonicotinic acid hydrazide and the incidence of variants resistant to the drug in vitro. Am Rev Tuberc. 1952;65:765–7.
Mitchison DA, Selkon JB. The bactericidal activities of antituberculous drugs. Am Rev Tuberc. 1956;74(2 Part 2):109–16 (discussion 116–23).
Schaefer WB. The effect of isoniazid on growing and resting tubercle bacilli. Am Rev Tuberc. 1954;69:125–7.
Unissa AN, Subbian S, Hanna LE, Selvakumar N. Overview on mechanisms of isoniazid action and resistance in Mycobacterium tuberculosis. Infect Genet Evol. 2016;45:474–92.
Pennisi M, Russo G, Sgroi G, Bonaccorso A, Parasiliti Palumbo GA, Fichera E, et al. Predicting the artificial immunity induced by RUTI® vaccine against tuberculosis using universal immune system simulator (UISS). BMC Bioinformatics. 2019;20:504. https://doi.org/10.1186/s12859-019-3045-5.
Nell AS, D’Lom E, Bouic P, Sabaté M, Bosser R, Picas J, et al. Safety, tolerability, and immunogenicity of the novel antituberculous vaccine RUTI: randomized, placebo-controlled phase II clinical trial in patients with latent tuberculosis infection. PLoS ONE. 2014a;9:e89612.
Pappalardo F, Russo G, Pennisi M, Parasiliti Palumbo GA, Sgroi G, Motta S, et al. The potential of computational modeling to predict disease course and treatment response in patients with relapsing multiple sclerosis. Cells. 2020;9:586. https://doi.org/10.3390/cells9030586.
Pappalardo F, Fichera E, Paparone N, Lombardo A, Pennisi M, Russo G, et al. A computational model to predict the immune system activation by citrus-derived vaccine adjuvants. Bioinformatics. 2016;32:2672–80. https://doi.org/10.1093/bioinformatics/btw293.
Pappalardo F, Lollini PL, Castiglione F, Motta S. Modeling and simulation of cancer immunoprevention vaccine. Bioinformatics. 2005;21:2891–7.
Russo G, Pennisi M, Viceconti M, Pappalardo F. In silico trial to test COVID-19 candidate vaccines: a case study with UISS platform. 2020.
Pennisi M, Rajput A-M, Toldo L, Pappalardo F. Agent based modeling of Treg-Teff cross regulation in relapsing-remitting multiple sclerosis. BMC Bioinformatics. 2013;14(Suppl 1):S9. https://doi.org/10.1186/1471-2105-14-S16-S9.
Pennisi M, Russo G, Ravalli S, Pappalardo F. Combining agent based-models and virtual screening techniques to predict the best citrus-derived vaccine adjuvants against human papilloma virus. BMC Bioinformatics. 2017;18:544. https://doi.org/10.1186/s12859-017-1961-9.
Bianca C, Riposo J. Mimic therapeutic actions against keloid by thermostatted kinetic theory methods. Eur Phys J Plus. 2015;130:159.
Bianca C, Fermo L. Bifurcation diagrams for the moments of a kinetic type model of keloid–immune system competition. Comput Math with Appl. 2011;61:277–88.
Pennisi M, Juarez MA, Russo G, Viceconti M, Pappalardo F. Generation of digital patients for the simulation of tuberculosis with UISS-TB. In: 2019 IEEE international conference on bioinformatics and biomedicine (BIBM). San Diego, CA, USA, USA: IEEE; 2019. pp. 2163–7. doi:https://doi.org/10.1109/BIBM47256.2019.8983100.
Russo G, Pappalardo F, Juarez MA, Pennisi M, Cardona PJ, Coler R, et al. Evaluation of the efficacy of RUTI and ID93/GLA-SE vaccines in tuberculosis treatment: in silico trial through UISS-TB simulator. Antimicrob Agents Chemother. 2019;58:7250–7. https://doi.org/10.1128/AAC.03728-14.
Abbas Abul K., Lichtman; AH, Pillai S. Cellular and molecular immunology. 2014.
Shen H, Chen ZW. The crucial roles of Th17-related cytokines/signal pathways in M. tuberculosis infection. Cell Mol Immunol. 2018;15:216–25.
van Pinxteren LA, Cassidy JP, Smedegaard BH, Agger EM, Andersen P. Control of latent Mycobacterium tuberculosis infection is dependent on CD8 T cells. Eur J Immunol. 2000;30:3689–98.
Nell AS, D’Lom E, Bouic P, Sabaté M, Bosser R, Picas J, et al. Safety, tolerability, and immunogenicity of the novel antituberculous vaccine RUTI: randomized, placebo-controlled phase II clinical trial in patients with latent tuberculosis infection. PLoS ONE. 2014b;9:1–10.
Acknowledgements
Not applicable.
About this supplement
This article has been published as part of BMC Bioinformatics Volume 21 Supplement 17 2020: Selected papers from the 3rd International Workshop on Computational Methods for the Immune System Function (CMISF 2019). The full contents of the supplement are available at https://bmcbioinformatics.biomedcentral.com/articles/supplements/volume21-supplement-17.
Funding
Authors of this paper acknowledge support from the STriTuVaD project. The STriTuVaD project has been funded by the European Commission and Indian Department of Biotechnology, under the contract H2020-SC1-2017- CNECT-2, No. 777123. The information and views set out in this article are those of the authors and do not necessarily reflect the official opinion of the European Commission. Neither the European Commission institutions and bodies nor any person acting on their behalf may be held responsible for the use which may be made of the information contained therein. Publication costs are funded by the STriTuVaD project.
Author information
Authors and Affiliations
Contributions
GR: developed the conceptual model, checked the biological adherence and meaning, analyzed data, wrote the manuscript. GS: implemented the extension of UISS, performed numerical simulations, analyzed data, wrote the manuscript. GAPP: performed numerical simulations, developed the python scripts for results generations, wrote the manuscript. MP: performed numerical simulations, analyzed data and wrote the manuscript. MAJ; performed statistical simulation and developed the procedure for digital patient cohort generation. PJC: gave biomedical knowledge and useful data about RUTI® vaccine, wrote the manuscript. SM: gave useful insights about numerical simulation, wrote the manuscript. KBW: provided valuable insights about TB disease, wrote the. manuscript. EF: checked the biological adherence and meaning, harmonized the clinical data. MV: gave useful insights about in silico clinical trial development, curated the validation of the simulator. FP: supervised, conceived and developed the model, gave computational immunological knowledge, drafted the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Russo, G., Sgroi, G., Parasiliti Palumbo, G.A. et al. Moving forward through the in silico modeling of tuberculosis: a further step with UISS-TB. BMC Bioinformatics 21 (Suppl 17), 458 (2020). https://doi.org/10.1186/s12859-020-03762-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12859-020-03762-5