Abstract
Introduction
The National Eye Institute Visual Function Questionnaire (NEI VFQ) is a common patient-reported outcome measure (PROM) in uveitis trials. Its psychometric properties using state-of-the-art scoring based on Rasch models, a latent trait model that improves accuracy of PROMs assessment, has not yet been investigated.
Methods
The study participants were recruited online from uveitis patient organizations, where individuals self-reported their uveitis diagnosis and visual acuity level. These participants then completed the NEI VFQ-25. The visual function (VF) and socioemotional (SE) subscales were psychometrically analysed in terms of item fit, targeting, internal consistency, dimensionality, and differential item functioning (DIF), using Rasch models. Criterion validity was examined based on associations between NEI VFQ person measures and recent visual acuity (VA) levels.
Results
Ninety-nine participants recruited online from uveitis patient organizations (68 women, 31 men; mean age 50 ± 15 years; 46.5% self-reported receiving systematic therapy for uveitis, 0.6% NEI VFQ-25 missing data) were included. The mean difficulty of items was lower than the average person ability. None of the items demonstrated misfit to an extent that would induce noise into the measurement. The consistency metrics person reliability and person separation index of the subscales were 0.85 and 2.34 (NEI VFQ-VF), 0.86 and 2.52 (NEI VFQ-SE), respectively. There was no evidence of multidimensionality and none of the items showed DIF by gender. The differences between item and person measures were 1.44 (NEI VFQ-VF) and 1.03 (NEI VFQ-SE). NEI VFQ-25 person measures were significantly lower in participants with visual impairment (all p values ≤ 0.007).
Conclusion
Rasch model-based scoring of the re-engineered NEI VFQ-25 demonstrates acceptable internal consistency, item fit and construct validity for assessing two key domains of quality of life in individuals self-reporting uveitis. The PROM was targeted at a higher level of difficulty than present in our heterogeneous sample.
Similar content being viewed by others
Introduction
Uveitis can have detrimental effects on visual function and quality of life (QoL) in affected people and can have serious complications leading to blindness and long-term disability [1,2,3]. Patient-reported outcome measures (PROMs) are commonly used to assess QoL, and they become increasingly integrated into regulatory drug approval processes and routine clinical practice in the context of uveitis [4].
The National Eye Institute Visual Function Questionnaire (NEI VFQ) is among the most frequently used PROMs in ophthalmology [1, 5, 6] and assesses vision-related QoL (VR-QoL). It was developed based on a literature review, focus group discussion with patients and expert panel input, covering five eye conditions (cataracts, glaucoma, age-related macular degeneration, diabetic retinopathy, cytomegalovirus (CMV) retinitis) [7]. The most common version of the NEI VFQ includes 25 items spanning eleven vision-related domains, while other versions with e.g. 51 and 39 items are available [8,9,10].
The NEI VFQ is also a commonly used PROM in uveitis trials [1, 2, 4,5,6, 11, 12]. Its internal consistency, test–retest reliability, reproducibility, and convergent validity in uveitis has been supported by previous psychometric analysis but this was based on conventional sum scoring [13]. However, this scoring of the NEI VFQ comes with problems in the stability of the measured construct [6], and use of a scoring system based on latent trait models has been recommended more recently [14, 15]. The lack of use of these modern scoring methods in uveitis have been recently criticized [4].
In this study, we have addressed this by evaluating the psychometric properties of the NEI VFQ-25 in uveitis patients. We have performed a psychometric analysis of the NEI VFQ-25 [6] using the primary items and the subscale structure of the NEI VFQ-25C [13] based on the Rasch model, a latent trait model, and investigated additional psychometric dimensions of the questionnaire in uveitis patients that cannot be investigated based on the conventional sum scoring system.
Materials and methods
Participants
Members of the German uveitis patient organizations Uveitis e.V. and the German Uveitis work group (Deutsche Uveitis Arbeitsgemeinschaft e.V.; DUAG) were recruited for remote participation in this study. The selection of participants was included based on self-reports and included the administration of other sociodemographic and patient-reported outcome questionnaires as well as self-reports of recent best corrected visual acuity (BCVA) data in the better eye, via an online form. The main outcome of the study was outside the work presented here (unpublished data). Inclusion criteria were a reported history of uveitis and available data on the NEI VFQ-25, participants with a high proportion of missing data (more than 50% of items per subscale) were excluded.
The study adhered to the tenets of the Declaration of Helsinki. Since the survey was performed anonymously, the ethics committee at the University Hospital Bonn, Germany waived the requirement of specific ethics committee approval.
National Eye Institute Visual Function Questionnaire
The 25-item version of the NEI VFQ covers eleven vision-related subscales as per conventional sum scoring, as well as one general health item. It has been used among various ophthalmic conditions [1, 9, 15, 16] but has severe psychometric use limitations when the conventional scoring algorithm is applied, including item fit and dimensionality of the subscales, which leads to imprecise measurements [6]. The application of latent trait models, of which the Rasch model is an example implemented commonly, is state of the art today, which has been used to psychometrically reconstruct the NEI VFQ as a two-dimensional scale (NEI VFQ-25C), including a visual function (NEI VFQ-VF) and socioemotional (NEI VFQ-SE) subscale [14, 15]. Latent trait models assume that the single items of a scale form a common construct and thus increase the precision of measurements and decrease the impact of missing data on the outcome [6, 17]. In Rasch analysis, the probability of a person given a certain response to an item is determined by both the person’s ability (e.g. in visual tasks) and the item’s difficulty. The Rasch model assumes that these are measured on the same underlying scale and that the probability of a particular response can be modelled using a logistic function. By transforming ordinal data into pseudo interval-level scales (expressed in logits), it is possible to accurately compare individuals’ abilities and item difficulties [18,19,20].
Psychometric and statistical analysis
We investigated the psychometric properties of the NEI VFQ-25 in a uveitis cohort based on Rasch models, using the primary items of the NEI VFQ-25C [15]. We generated a person-item map to visualize the difficulty of test items in relation to the abilities of individuals and further evaluated the targeting of the scale based on the difference between mean item and person measures [21]. We assessed item fit, using infit mean-square (MNSQ) and outfit MNSQ values. Values within the range of 0.5 to 1.5 were considered indicative of effective measurement [22]. Internal consistency was analysed based on the metrics person reliability (PR) and person separation index (PSI), where values above 0.8 and 2.0 were considered acceptable, respectively [22]. The dimensionality of the pre-established subscales was investigated based on a principal component analysis (PCA) of the model residuals. Lastly, we examined DIF for the participants’ sex. A significant standard threshold of > 1 logit units was used as an indicator of DIF.
Person measures were compared between groups with binocular visual impairment (VI), monocular VI, and no VI [23], using the Kruskal–Wallis test and a post-hoc Mann–Whitney-U-test. Rasch analysis was conducted with Winsteps software (version 3.92.1, Chicago, IL). Statistical analysis was performed using IBM SPSS, versions 25 (IBM, Armonk, NY) and p values < 0.05 were considered statistically significant.
Results
A total of 107 responses were available. After excluding participants with > 50% missing responses in either of the subscales, ninety-nine participants (68 females, 69%; 31 males, 31%) were included in our analysis. In the final dataset, 13 item responses to the NEI VFQ were missing (0.6% of all responses). The mean age at participation was 49.6 ± 14.6 years. Sixty-one (61.6%) participants indicated having an occupation whereas thirty-eight (38.4%) indicated being unemployed. Forty-six participants (46.5%) received systemic immunomodulatory therapy. The mean BCVA of the better eye was 0.17 ± 0.28 logMAR units and 0.51 ± 0.62 logMAR units in the worse eye (data available in 79 participants, 80%). Seven participants (9%) had binocular VI, 24 participants (30%) had monocular VI, and 48 participants (61%) had no VI [23].
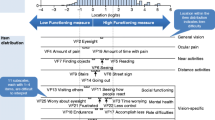
The person-item map of both NEI VFQ subscales, NEI VFQ-VF and NEI VFQ-SE, revealed a lower average item difficulty than the average person ability, meaning that the items of the instrument were, in general, too easy for the ability level of the participant (Fig. 1).
Person-item map of the National Eye Institute Visual Function Questionnaire in the uveitis sample. Items marked with an A belong to the visual function subscale, and items marked with a B are part of the socioemotional subscale. Individual respondents are shown on the left and items are displayed on the right. Items are plotted according to their order of difficulty with the easiest at the bottom and the most difficult at the top of the Figure
Initially, three items of the visual functioning subscale (item 4 [pain], infit mean square 1.81 and outfit mean square 2.03; item 6 [work up close], infit mean square 0.46; item 7 [finding objects on crowded shelf], infit mean square 0.48) and one item of the socioemotional subscale (item 3 [worry about eyesight], outfit mean square 1.78) misfit the Rasch model, suggesting that these items did not effectively measure the underlying construct and introduced noise into the measurement. To address this, we removed 15 misfitting responses from the visual functioning subscale and excluded 23 misfitting responses from the socioemotional subscale for the psychometric investigation. This adjustment improved the fit statistic but did not resolve the misfit of item 6 (infit mean square 0.46) of the visual functioning subscale (Supplementary Figure). Person measures before and after removal of misfitting responses were positively correlated (r = 0.99 [0.99–1.00]).
The PR and the PSI fell within the recommended range (Table 1). The NEI VFQ-VF subscale was targeted at a lower functioning level than that of the participants. PCA indicated potential multidimensionality of the NEI VFQ-SE subscale within the cohort, but an exploration of the contrasting clusters indicated a high correlation between the respective person measures (r = 0.95 [0.92, 0.96]), supporting unidimensionality of the socioemotional subscale of the NEI VFQ. No significant DIF by sex was observed in any of the NEI VFQ items.
VR-QoL was significantly different across VA levels (all p values ≤ 0.003, Kruskal–Wallis-test). Post-hoc testing revealed lower VRQoL in individuals with binocular or monocular VI, compared to participants with no VI (all p values ≤ 0.007, U-test; Fig. 2).
Discussion
Our data support the item fit, internal consistency, unidimensionality and construct validity of the NEI VFQ in a heterogeneous cohort of uveitis patients. This supports that Rasch scoring of the NEI VFQ-25 should be implemented in future uveitis trials, given validity in the investigated sub-populations (e.g. by anatomic location, inflammatory activity, complications).
This study confirms the psychometric findings obtained by methods from classical test theory [13]. Traditional sum scoring indicated a Cronbach’s alpha between 0.87 to 0.94 [13], while alpha was > 0.9 in our study. While previous assessments of psychometric properties (test–retest reliability, reproducibility, convergent validity) of the NEI VFQ in uveitis relied on conventional sum scoring [13], our current study delves further into psychometric dimensions such as item fit, targeting, and DIF, aspects that are not ascertainable through classical test theory methods. Additionally, the analyses reveal adjustments that may further optimize the assessment of VR-QoL in uveitis cohorts, which pends further evaluation.
Our study findings reveal relative mistargeting of the NEI VFQ-VF subscale in a heterogeneous population of uveitis patients, suggesting that the instrument may not effectively capture the full spectrum of VR-QoL issues experienced by uveitis patients. This may relate to the high levels of visual acuity observed in our cohort (mean visual acuity was 0.17 ± 0.28 logMAR units in the better eye). Clinical trials in uveitis often include participants with lower visual acuity levels than those in our study, while visual acuity levels in our cohort were at the upper end of the spectrum expected in uveitis trial populations [2, 11, 12]. Thus, we expect the NEI VFQ-25 to be better targeted at lower visual acuity populations. However, this needs to be further validated in an independent cohort.
Since the analyses were focused on the psychometric properties of scoring method based on Rasch models, our results do not allow commenting on the content validity of the NEI VFQ-25 in uveitis. The development of content domains and validation included 17/246 (7%) individuals with CMV retinitis, an infectious posterior uveitis [7]. The initial validation study of the NEI VFQ (51-item version) also included a proportion of individuals with CMV retinitis (37/598, 6%) [8]. This supports the content validity of the NEI VFQ in a specific uveitis entity but does not allow making assumptions about its validity in other types of uveitis (e.g. non-infectious forms, anterior uveitis), where more research is needed. However, the recent development of the Rasch model-scored version of the NEI VFQ (NEI VFQ-25C [15]), did not report inclusion of any uveitis patients and therefore, our results strengthen the use of an model-based scoring system of the NEI VFQ in instances where the use context justifies including NEI VFQ items to assess of VR-QoL in uveitis.
We have conducted an analysis of psychometric properties of a commonly used PROM in uveitis trials. While our findings suggest overall sound psychometric properties, it is important to acknowledge several limitations. Our sample was recruited via an online survey from patient organizations where only self-reported acuity data and no further clinical data were available, and a reporting bias cannot be fully excluded. As no information on the anatomic classification uveitis or level of inflammation were available, the external validity of our findings may be limited and further research is needed to validate the model-based scoring approach in clinical sub-populations. The performance on the NEI VFQ-25 may vary across different uveitis subtypes as uveitis is a largely heterogeneous condition with diverse clinical presentations and treatment responses. One of the NEI VFQ-25C sub-items (item 16a) could not be included in the analysis but has high content similarity with one item included (item 16), thus we do not expect this to impact the validity of the results. Moreover, the focus group discussions conducted during the development of the NEI VFQ involved only a limited number of uveitis patients. Despite the NEI VFQ-25 being commonly used in uveitis trials, further research is needed to investigate the content validity and patient-reported dimensions that are additionally relevant. Our study sample was recruited form uveitis patient organizations in Germany, possibly limiting its representativeness of uveitis patients internationally.
To address these limitations, future research should incorporate larger, more diverse uveitis populations with verified diagnoses and detailed subtype information, while also considering comprehensive validity assessments (concurrent, convergent, discriminant and known group) to confirm and extend our findings. A broader range of items with varying levels of difficulty and covering different aspects relevant to uveitis patients may be required to fully capture VR-QoL in uveitis.
Overall, the data from our exploratory study support the use of a Rasch model-based scoring algorithm in uveitis patients in the future, which can make PROM assessments more precise. Our study endorses the further use of patient-relevant endpoints in clinical studies in uveitis. Nevertheless, addressing the constraints identified in our research warrants further inquiry in future studies.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author on reasonable request.
Abbreviations
- BCVA:
-
Best corrected visual acuity
- DIF:
-
Differential item functioning
- MNSQ:
-
Mean square
- NEI VFQ:
-
National Eye Institute Visual Function Questionnaire
- PCA:
-
Principal component analysis
- PR:
-
Person reliability
- PROMs:
-
Patient-reported outcome measures
- PSI:
-
Person separation index
- QoL:
-
Quality of life
- SE:
-
Socioemotional
- VA:
-
Visual acuity
- VF:
-
Visual function
- VI:
-
Visual impairment
- VR-QOL:
-
Vision-related quality of life
References
Senthil MP, Simon S, Constable PA (2023) A review of patient-reported outcome measures used in uveitis. Surv Ophthalmol 68:225–240. https://doi.org/10.1016/j.survophthal.2022.11.004
Naik RK, Rentz AM, Foster CS et al (2013) Normative comparison of patient-reported outcomes in patients with noninfectious uveitis. JAMA Ophthalmol 131:219–225. https://doi.org/10.1001/2013.jamaophthalmol.102
Shamdas M, Bassilious K, Murray PI (2019) Health-related quality of life in patients with uveitis. Br J Ophthalmol 103:1284–1288. https://doi.org/10.1136/bjophthalmol-2018-312882
O’Donovan C, Panthagani J, Aiyegbusi OL et al (2022) Evaluating patient-reported outcome measures (PROMs) for clinical trials and clinical practice in adult patients with uveitis or scleritis: a systematic review. J Ophthalmic Inflamm Infect 12:29. https://doi.org/10.1186/s12348-022-00304-3
Finger RP, Fleckenstein M, Holz FG et al (2008) Quality of life in age-related macular degeneration: a review of available vision-specific psychometric tools. Qual Life Res 17:559–574. https://doi.org/10.1007/s11136-008-9327-4
Pesudovs K, Gothwal VK, Wright T et al (2010) Remediating serious flaws in the National Eye Institute Visual Function Questionnaire. J Cataract Refract Surg 36:718–732. https://doi.org/10.1016/j.jcrs.2009.11.019
Mangione CM, Berry S, Spritzer K et al (1998) Identifying the content area for the 51-item National Eye Institute Visual Function Questionnaire: results from focus groups with visually impaired persons. Arch Ophthalmol 116:227–233. https://doi.org/10.1001/archopht.116.2.227
Mangione CM, Lee PP, Pitts J et al (1998) Psychometric properties of the National Eye Institute Visual Function Questionnaire (NEI-VFQ). NEI-VFQ Field Test Investigators Arch Ophthalmol 116:1496–1504. https://doi.org/10.1001/archopht.116.11.1496
Szegedi S, Boltz A, Scharinger E-M et al (2022) Quality of life in patients with glaucoma assessed by 39-item National Eye Institute Visual Functioning Questionnaire (NEI VFQ-39). Graefes Arch Clin Exp Ophthalmol 260:1623–1631. https://doi.org/10.1007/s00417-021-05434-3
Mangione CM, Lee PP, Gutierrez PR et al (2001) Development of the 25-item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol 119:1050–1058. https://doi.org/10.1001/archopht.119.7.1050
Jaffe GJ, Dick AD, Brézin AP et al (2016) Adalimumab in Patients with Active Noninfectious Uveitis. N Engl J Med 375:932–943. https://doi.org/10.1056/NEJMoa1509852
Kempen JH, Altaweel MM, Holbrook JT et al (2011) Randomized comparison of systemic anti-inflammatory therapy versus fluocinolone acetonide implant for intermediate, posterior, and panuveitis: the multicenter uveitis steroid treatment trial. Ophthalmology 118:1916–1926. https://doi.org/10.1016/j.ophtha.2011.07.027
Naik RK, Gries KS, Rentz AM et al (2013) Psychometric evaluation of the National Eye Institute Visual Function Questionnaire and Visual Function Questionnaire Utility Index in patients with non-infectious intermediate and posterior uveitis. Qual Life Res 22:2801–2808. https://doi.org/10.1007/s11136-013-0412-y
Marella M, Pesudovs K, Keeffe JE et al (2010) The psychometric validity of the NEI VFQ-25 for use in a low-vision population. Invest Ophthalmol Vis Sci 51:2878–2884. https://doi.org/10.1167/iovs.09-4494
Goldstein JE, Bradley C, Gross AL et al (2022) The NEI VFQ-25C: Calibrating Items in the National Eye Institute Visual Function Questionnaire-25 to Enable Comparison of Outcome Measures. Transl Vis Sci Technol 11:10. https://doi.org/10.1167/tvst.11.5.10
Künzel SH, Möller PT, Lindner M et al (2020) Determinants of Quality of Life in Geographic Atrophy Secondary to Age-Related Macular Degeneration. Invest Ophthalmol Vis Sci 61:63. https://doi.org/10.1167/iovs.61.5.63
Norquist JM, Fitzpatrick R, Dawson J et al (2004) Comparing alternative Rasch-based methods vs raw scores in measuring change in health. Med Care 42:I25-36. https://doi.org/10.1097/01.mlr.0000103530.13056.88
Lamoureux EL, Pallant JF, Pesudovs K et al (2007) The impact of vision impairment questionnaire: an assessment of its domain structure using confirmatory factor analysis and rasch analysis. Invest Ophthalmol Vis Sci 48:1001–1006. https://doi.org/10.1167/iovs.06-0361
Boone WJ, Staver JR, Yale MS What Is Rasch Measurement and How Can Rasch Measurement Help Me? 1–19. https://doi.org/10.1007/978-94-007-6857-4_1
Wright BD, Linacre JM (1989) Observations are always ordinal; measurements, however, must be interval. Arch Phys Med Rehabil 70:857–860
Khadka J, McAlinden C, Pesudovs K (2013) Quality assessment of ophthalmic questionnaires: review and recommendations. Optom Vis Sci 90:720–744. https://doi.org/10.1097/OPX.0000000000000001
Linacre JM (2023) A Users's Guide to WINSTEPS® MINISTEP Rasch-Model computer programs.: Program Manual 5.6.0. Available at: https://www.winsteps.com/winman/copyright.htm (Accessed 5 Oct 2023).
World Health Organization (2019) World report on vision. Licence: CC BY-NC-SA 3.0 IGO.
Acknowledgements
We acknowledge the continuous support of our scientific work by the patient organizations Uveitis e.V. and German Uveitis work group (DUAG) without which our work would not have been possible.
Funding
Open Access funding enabled and organized by Projekt DEAL. Open Access funding enabled and organized by Projekt DEAL. This research was funded by the German Ophthalmologic Society (Deutsche Ophthalmologische Gesellschaft, DOG), grant number FF 2019, project number FF 2020.
Author information
Authors and Affiliations
Contributions
JHT, RPF and JQL designed the study. JD, JQL and RPF collected the data. LG, JHT, RPF, JQL, MWMW and CH analysed and interpreted the data. LG and JHT prepared the manuscript, which was then critically revised by JQL, JD, MWMW, CH and RPF. All authors agreed to the final version of the manuscript being published and to be responsible for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All data gathered as part of this research project was collected anonymously, obviating the need for approval from the institution’s Ethics Committee. Consequently, written informed consent from participants was not required.
Consent for publication
Not applicable.
Competing interests
LG: None. JQL: None. JD: None. MWMW: Bayer AG, Berlin-Chemie AG, CenterVue SpA, Carl Zeiss Meditec, Eyenuk, Inc., Eyepress Fachmedien GmbH, glaucare GmbH, Heine Optotechnik GmbH, Heidelberg Engineering, Novartis Pharma GmbH, Optos, Pro Generika e.V., Science Consulting in Diabetes GmbH. CH: Alimera, Bayer, Biogen, Novartis. RPF: Alimera, Apellis, Bayer, Boehringer-Ingelheim, Novartis, ODOS, Oxford Innovation, ProGenerika, Roche/Genentech, Biogen, Icare, Heidelberg Engineering, Zeiss Meditec. JHT: Heidelberg Engineering, Optos, Zeiss, CenterVue, Novartis, Okko.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gittel, L., Li, J.Q., Dell, J. et al. Piloting Rasch model scoring of the National Eye Institute Visual Function Questionnaire in uveitis. J Ophthal Inflamm Infect 14, 16 (2024). https://doi.org/10.1186/s12348-024-00398-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12348-024-00398-x