Abstract
Purpose
To report a surgical-induced necrotizing scleritis, as well as its medical and surgical management.
Methods
Case-report.
Results
An 88 year-old patient with a three-day severe single-left-eye ocular pain. One-time surgery involving PPV with removal of dislocated intraocular lens and secondary implantation of iris-claw Artisan® lens was performed 6 months earlier. Visual acuity of 20/100. Slit-lamp examination revealed a 5 × 2 mm non-suppurative superior scleral defect. Empirical topical antibiotic treatment with dexamethasone, as well as oral doxycycline was started. Infectious and autoimmune diseases were ruled out. Non-infectious scleritis treatment was conducted with intravenous Methylprednisolone 3 day pulses, followed by weekly tapered Prednisone and intramuscular Methotrexate. However, 1 month after the diagnosis, the defect was worsened; hence, a heterologous scleral patch graft was performed and, days after the intervention, Adalimumab was initiated. To date, 6 months later, remains with proper scleral patch, a diary low-dose Prednisone, and spacing Adalimumab treatment.
Conclusion
Surgery-induced necrotizing scleritis is a severe condition that compromise the ocular and visual integrity. Proper diagnosis, as well as early treatment is required to achieve remission, prevent relapses, and avoid structural complications. In refractory cases, anti-TNF-α immunotherapy associated with surgical tectonic graft interventions can achieve promising results.
Similar content being viewed by others
Introduction
Surgery-induced necrotizing scleritis (SINS) is a rare local autoimmune reaction of the sclera adjacent to previous surgical incisions, which has been reported following cataract surgery, trabeculectomy, scleral buckling, as well as pterygium and strabismus surgery [1,2,3,4]. Ocular trauma serves as more than just a pathogenic mechanism; it acts as a triggering factor that can initiate scleral necrosis through various pathogenic pathways. Patients who develop SINS exhibit an atypical response to surgical trauma, which can be attributed to the presence of unusual local and systemic immunological factors [1].
We present the case of a patient with SINS following vitrectomy after explantation of a luxated intraocular lens (IOL) and secondary implantation of an anterior iris-fixated Worst claw Artisan® IOL. A systemic workup was conducted to rule out underlying pathologies. We describe the multidisciplinary medical management as well as the surgical approach. Slit lamp and intraoperative images are provided to illustrate the clinical case.
Case description
An 88-year-old woman with a history of insulin-dependent diabetes mellitus, stage 3a chronic kidney disease (CKD), bilateral atrophic age-related macular degeneration (ARMD) and advanced glaucoma in her right eye, along with four months of nonspecific joint pain without clear signs of inflammation, sought medical attention.
She exhibited a spontaneous posterior dislocation of her left eye intraocular lens (IOL) and subsequently underwent a pars plana vitrectomy. During the procedure, the dislocated IOL was removed, and a secondary implantation of a prepupillary iris-claw Artisan® IOL was performed through a 5.5 mm superior sclerocorneal incision. The surgery was successfully completed, and the immediate postoperative recovery period was free from any complications. Several weeks later, the four Nylon 10/0 sutures used during the surgery were removed.
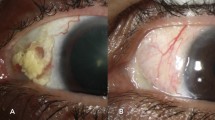
Nonetheless, six months following the medical intervention, she presented at the emergency room with acute ocular pain in her left eye that had persisted for three days. Her visual acuity had deteriorated to 20/100 (previous 20/40). A slit-lamp examination revealed a non-suppurative defect in the superior sclera measuring 5 × 2 mm (see Fig. 1A). Her intraocular pressure was within the normal range, and the fundus examination showed no other abnormalities. Based on the clinical findings, a diagnosis of anterior necrotizing scleritis was made, with uncertainty about whether it was due to infection or related to the prior surgery. Empirical treatment was initiated, including Tobramycin-Dexamethasone eye drops every 8 hours, Moxifloxacin 0.5% eye drops every 4 hours, Atropine 1% eye drops twice a day, and oral Doxycycline 100 mg every 12 hours.
The patient was then referred to the multidisciplinary ocular inflammation clinic at the University Hospital of Navarra, where a comprehensive systemic evaluation was performed. This evaluation included a complete blood count with biochemical analysis, C-reactive protein, rheumatoid factor, complement fractions, and serological tests, as well as testing for specific antigens (HLA-B27, HLA-B51, HLA-A29) and autoantibodies (such as antinuclear, antineutrophil cytoplasmic, or anti-citrullinated antibodies, among others). A tuberculin test and chest X-ray were also conducted. However, these tests did not reveal any underlying infectious or autoimmune systemic disorders. Additional tests, such as PCR analysis of the aqueous humor sample and conjunctival scrape for microbiological culture, were negative for bacteria, fungi, and atypical mycobacteria.
Consequently, a definitive diagnosis of surgery-induced anterior necrotizing scleritis was established, leading to the discontinuation of the empirical treatment, except for oral Doxycycline. The patient was then started on intravenous systemic treatment with Methylprednisolone succinate at a daily dose of 60 mg for three days (1 mg/kg/day), followed by a weekly tapering dose of oral Prednisone at 30 mg/day. Methotrexate subcutaneous injection at a dose of 7.5 mg per week was also initiated.
Unfortunately, the patient experienced a significant increase in blood sugar levels, prompting a reduction of Prednisone to 10 mg per day and an increase in Methotrexate to 12.5 mg per week. This exacerbated the ongoing scleritis, necessitating the resumption of Methylprednisolone in three-day boluses, this time at a dose of 90 mg (1.5 mg/kg/day), with strict monitoring and control of blood sugar levels.
Despite these interventions, one month after the initial diagnosis, and due to the progressive nature of the scleral defect (see Fig. 1B), a heterologous scleral patch graft surgery was performed following meticulous debridement of the adjacent necrotic tissue (see Fig. 2A & Video). Additionally, a second esclerocorneal scrape was performed, but the microbiological results remained inconclusive.
To manage postoperative inflammation, subcutaneous Adalimumab was introduced after the surgery, starting with an 80 mg dose, and gradually reducing it to 40 mg in subsequent weeks. Methotrexate was discontinued from the second week post-surgery, and a new tapering regimen of Prednisone at 30 mg per day was initiated, this time with careful spacing. Six months after the surgery, the scleral patch remained stable (see Fig. 2B), and the patient continued with Prednisone at 7.5 mg/day and Adalimumab at a dosage of 40 mg every six weeks.
Discussion
Surgery-induced necrotizing scleritis (SINS) can be triggered by any type of ocular surgical intervention, and the latency period is highly variable, ranging from first postoperative day to years after surgery [1]. Women are more affected, and the average age is fifth decade of life [1]. Pterygium excision is the most associated ocular surgery and autoimmune diseases are specially related in the cataract extraction cases [1, 2].
Predicting SINS poses a considerable challenge, as postoperative scleral thinning can go unnoticed, leading to a delayed diagnosis. In the early stages of the condition, patients may encounter symptoms like conjunctival redness and mild discomfort, which are frequently misinterpreted as dry eye disease or conjunctivitis, prolonging the diagnosis and treatment process [1]. In advanced cases, patients typically manifest significant pain, visual impairment, peripheral corneal ulcers, scleral necrosis, and the development of anterior staphylomas [1].
This entity involves a common induction mechanism (ocular surgery) and a characteristic pathological finding (scleral necrosis) [1]. Physical trauma caused by excessive cauterization or cryotherapy, chemically induced damage with antimetabolites, compression-related ischemia, like tighten sutures, as well as autoimmune local activation, represent a wide range of pathogenic mechanisms that can induce scleral necrosis [1, 2, 5]. Diabetes is also related due to the pro-ischemic inflammatory environment that exerts [6]. All these induce a slowdown in surgical wound healing, that can lead to a secondary infection [7]. The overlap between these mechanisms complicates the diagnosis and its corresponding treatment.
Considering the multiple aetiologies related to necrotizing scleritis, a comprehensive study should be conducted to discard primary infectious scleritis or underlying autoimmune involvement [5]. The research should include complete blood count, erythrocyte sedimentation rate, C-reactive protein, liver and kidney function tests, serum complement levels, antinuclear antibody, rheumatoid factor, antineutrophil cytoplasmic antibody, anti-citrullinated protein antibody, and serum angiotensin-converting enzyme levels [5]. To rule out infectious involvement, wound scrape for microbiological culture, or for scleral biopsy, and intraocular samples for PCR are necessary [2, 5, 7]. In addition, testing for tuberculosis, syphilis, HIV infection, hepatitis B and C, herpes simplex and varicella-zoster viruses should be performed [2, 7].
Due to the devastating consequences for the eye, early detection and treatment are fundamental. Topical antibiotics and/or antifungals are often empirically administered [1, 2]. The presence of mucopurulent discharge or hypopyon increases suspicion of an infectious aetiology, thus initiating topical and systemic antibiotic treatment is recommended [7]. Topical corticosteroids are associated with poor wound healing [1, 8]. Therefore, they have the potential to perpetuate the scleral thinning process, as it happens in the early stages of our case. As adjunctive treatment, oral doxycycline (100 mg/day) can also be added for its anticolagenolytic effect [8].
Systemic nonsteroidal anti-inflammatory drugs are useful at diagnosis [1, 5]. However, long-term use is not recommended due to their side effects [8]. Oral prednisone is considered first-line therapy in non-infectious necrotizing scleritis, with an initial immunosuppressive dose of 1 mg/kg/day gradually tapered based on clinical recovery [1, 5, 8]. Due to the stage 3a CKD of our patient, the corticosteroid doses were inferior to usual. Intravenous methylprednisolone for 3 days has shown efficacy in patients with severe inflammation, as it happens in our case [1, 8]. A patient with SINS will require a combination with nonsteroidal immunomodulatory therapy to enhance efficacy and avoid the long-term adverse effects of corticosteroids [1, 5, 8]. Some medications used include methotrexate, azathioprine, mycophenolate mofetil, cyclophosphamide cyclosporine and tacrolimus [5, 8, 9]. We choose the first one due to his safety profile in elderly and comorbidly patients [8].
A better understanding of the immunopathogenesis of ocular inflammatory diseases, as well as the development of new molecules, has enriched our therapeutic arsenal and created more effective treatment approaches [10, 11]. Monoclonal antibodies against TNF-α (all except Etanercept), IL-1 inhibitors (Anakinra), IL-6 inhibitors (Tocilizumab), and anti-CD20 (Rituximab) targeted-drugs have been shown to control inflammation and reduce scleritis flares, allowing for a corticosteroid-sparing effect [5, 8, 10, 11]. TNF-α inhibitors like Adalimumab or Infliximab are used as first-line biological agents [12, 13]. Adalimumab is the only biologic treatment approved for non-infectious uveitis and it has been used in other case reports with excellent clinical outcomes [13].
However, patients with active and progressive scleral necrosis will require immediate conjunctival debridement [14]. Apart from obtaining a scrape when infection is suspected, conjunctival resection results in a decrease of protease concentration, including collagenase, and a temporary interruption of the local inflammatory process [1, 14]. The use of cyanoacrylate glue after surgical debridement can help prevent neutrophil migration [1]. Conjunctival and Tenon’s flap grafts, as well as amniotic membrane transplantation, can also be used [1]. However, when uveal tissue is exposed, a tectonic procedure with scleral patch graft is preferred [1, 5, 15].
Conclusion
Surgery-induced necrotizing scleritis is a severe ophthalmological condition that can compromise the ocular and visual integrity. It is associated with autoimmune diseases in around 50% of cases and can be their initial manifestation, which is why a comprehensive analytical screening is necessary to rule out this possibility. Concurrent infectious involvement should also be ruled out as it influences the therapeutic management of the condition. Aggressive and early treatment is required to achieve rapid remission, prevent relapses, and ultimately avoid irreversible structural complications. Systemic corticosteroids combined with alkylating immunomodulators are positioned as first-line therapy, with anti-TNF biological drugs as the alternative option. The management of scleritis should be carried out in a multidisciplinary setting to maximize treatment benefits and minimize safety concerns. Surgical intervention is reserved for extensive defects with significant uveal exposure, despite adequate medical treatment. Amniotic membrane transplantation and heterologous scleral patch graft are the main options to consider, amongst others.
Availability of data and materials
The data used in this case report is available from the corresponding author on reasonable request.
Abbreviations
- PPV:
-
Pars plana vitrectomy
- IOL:
-
Intraocular lens
- SINS:
-
Surgical-induced necrotizing scleritis
- CKD:
-
Chronic kidney disease
- ARMD:
-
Age-related macular disease
- HLA:
-
Human leukocyte antigens
- HIV:
-
Human immunodeficiency virus
- PCR:
-
Polimerase chain reaction
- IL:
-
interleukin
- TNF:
-
Tumour necrosis factor
- PGDLM:
-
Pablo González de los Mártires
- GGP:
-
Gonzalo Guerrero Pérez
- ILB:
-
Iñigo Les Bujanda
- IEG:
-
Iñaki Elejalde Guerra
- HEM:
-
Henar Heras Mulero
- ECS:
-
Esther Compains Silva
References
Ruiz-lozano RE, Garza-garza LA, Davila-cavazos O, Foster CS, Rodriguez-garcia A (2021) The clinical and pathogenic spectrum of surgically-induced scleral necrosis : A review. Surv Ophthalmol 66:594–611
Doshi RR, Harocopos GJ, Schwab IR, Cunningham ET (2013) The spectrum of postoperative scleral necrosis. Surv Ophthalmol 58:620–633
Khurram Butt D, Khan MI, Fathalla BM, Ali SA, Kozak I (2022) Atypical noninfectious surgically induced necrotizing Scleritis in a child. Ocul Immunol Inflamm 30:998–1000
Shalaby U, Heikal MA (2016) Unilateral surgically induced necrotizing Scleritis after trabeculectomy with Ologen in a patient with pigmentary glaucoma. Am J Ophthalmol Case Rep 3:47–49
Nevares A, Raut R, Libman B, Hajj-Ali R (2020) Noninfectious autoimmune Scleritis: recognition, systemic associations, and therapy. Curr Rheumatol Rep 22
O’Donoghue E, Lightman S, Tuft S, Watson P (1992) Surgically induced necrotising sclerokeratitis (SINS)- precipitating factors and response to treatment. Br J Ophthalmol 76:17–21
Balasopoulou A et al (2017) Scleritis: differentiating infectious from non-infectious entities. BMC Ophthalmol 17:1
Stem MS, Todorich B, Faia LJ (2017) Ocular pharmacology for Scleritis: review of treatment and a practical perspective. J Ocul Pharmacol Ther 33:240–246
Promelle V, Goeb V, Gueudry J (2021) Rheumatoid arthritis associated episcleritis and scleritis: an update on treatment perspectives. J Clin Med 10
Sota J et al (2021) Biologic therapies and small molecules for the Management of non-Infectious Scleritis: A narrative review. Ophthalmol Ther 10:777–813
de Fidelix TSDA, Vieira LA, de Freitas D, Trevisani VFM (2015) Biologic therapy for refractory scleritis: a new treatment perspective. Int Ophthalmol 35:903–912
Sen HN, Sangave A, Hammel K, Levy-Clarke G, Nussenblatt RB (2009) Infliximab for the treatment of active scleritis. Can J Ophthalmol 44:e9
Durrani K et al (2017) Adalimumab for ocular inflammation. Ocul Immunol Inflamm 25:405–412
Cordero-Coma M, Franco-Benito M, García-Ruiz-de-Morales JM, Alonso-Orcajo N, Del Barrio-Manso I (2009) Successful treatment of surgically induced necrotizing sclerokeratitis (SINS) with systemic immunosuppresive agents and amniotic membrane grafting. Arch Soc Esp Oftalmol 84:577–580
de la Maza MS, Tauber J, Foster CS (1989) Scleral grafting for necrotizing Scleritis. Ophthalmology 96:306–310
Acknowledgements
Not applicable.
Funding
No funding or grant support was received.
Author information
Authors and Affiliations
Contributions
PGDLM and GGP is responsible for the design, manuscript preparation, literature search, data acquisition, and data analysis. ILB, IEG, HEM and ECS are responsible for the concept, definition of intellectual content, manuscript editing, and manuscript review. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This article does not contain any studies with human participants or animals.
Consent for publication
A consent to publish was obtained from the patient.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
de los Mártires, P.G., Pérez, G.G., Bujanda, I.L. et al. Surgical induced necrotizing scleritis following intraocular lens replacement. J Ophthal Inflamm Infect 13, 53 (2023). https://doi.org/10.1186/s12348-023-00373-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12348-023-00373-y