Abstract
Endophthalmitis is among the most sight-threatening infections in ophthalmology practice. Many microorganisms causing endophthalmitis have been reported. Stenotrophomonas maltophilia is among the rare causes of endophthalmitis and has been reported after cataract surgery, intravitreal injections and ocular trauma. We report a case of S. maltophilia endophthalmitis after keratoplasty, which is a rare entity, in a 63-year-old female patient.
Similar content being viewed by others
Introduction
Stenotrophomonas maltophilia is a gram-negative bacillus which is opportunistic, nonfermenting, obligate aerobic and motile [1]. The microorganism is usually isolated from water, soil and plants [2, 3]. S. maltophilia infections are known as nosocomial infections due to their ability to live on plastic and glass surfaces [4]. Pneumonia, acute exacerbations of chronic obstructive pulmonary diseases, bacteremia, septicemia, cellulitis, myositis, osteomyelitis, meningitidis, endocarditis, urinary tract infections and biliary sepsis are S. maltophilia associated infections [5]. The most important ophthalmological diseases caused by S. maltophilia are keratitis, scleritis, conjunctivitis, preseptal cellulitis, dacryocystitis and endophthalmitis [6,7,8,9,10]. S. maltophilia is a rare cause of endophthalmitis and cases of endophthalmitis associated with S. maltophilia have generally been reported after cataract surgery, trauma or intravitreal injections [11,12,13].
When we searched the literature, we found very few cases of S. maltophilia endophthalmitis after keratoplasty. In this case, we present a patient who developed S. maltophilia endophthalmitis after a keratoplasty procedure.
Case report
A 63-year-old female patient was referred to our clinic due to corneal thinning and melting in the left eye. Her best corrected visual acuity (BCVA) was finger counting from 20 cm in the right eye and finger counting from 10 cm in the left eye. Slit-lamp biomicroscopic examination revealed an opacity of 8 mm in the left cornea, thinning, and a central descemetocele (Fig. 1-A); while the right eye was pseudophakic, and penetrating keratoplasty (PKP) was previously performed on the right eye. She had optic atrophy on the right, and her history could only reveal that she had been treated for glaucoma for a long time. At the same time, the left eye was phakic, fundus examination could not be performed in detail due to corneal opacity, but no vitreous problems were observed while the retina was attached in the B-scan ultrasonography.
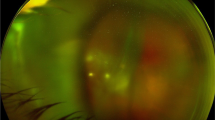
A Corneal central thinning and descemetocele at the time of first admission, B Anterior segment photograph after deep lamellar keratoplasty, C Graft failure due to endotheliitis, D Anterior segment photograph after penetrating keratoplasty, E–F-G Hypopyon in the anterior chamber, fibrinous reaction, mature cataract and ciliary injection, H Anterior segment photograph after phaco-vitrectomy
After deep anterior lamellar keratoplasty (DALK) was performed in the left eye, endotheliitis and endothelial insufficiency developed in the follow-ups, and PKP was applied to the left eye 2 weeks later (Fig. 1-B,C,D). Fibrin reaction started in the anterior chamber on the second postoperative day of the patient and it was observed that this reaction gradually increased. Subconjunctival dexamethasone was added twice a day to the patient who received topical dexamethasone 8 times a day, topical moxifloxacin 4 times a day, valacyclovir 1000 mg orally 3 times a day and acetazolamide 250 mg orally 3 times a day. The gradually increasing reaction was replaced by a 1.5 mm hypopyon in the first week, and additionally, posterior synechiae and vitreous condensation were found on B-scan ultrasonography (Fig. 1-E,F,G). With the preliminary diagnosis of endophthalmitis, samples were taken from the anterior chamber and vitreous, then intravitreal injections vancomycin (1 mg / 0.1 mL) and ceftazidime (2.25 mg / 0.1 mL) were given; and cefuroxime (1 mg / 0.1 mL) was administered to the anterior chamber. Topical fortified vancomycin and ceftazidime drops hourly and cyclopentolate 3 times daily were started. It was reported that S. maltophilia isolated in vitreous and anterior chamber samples (Fig. 2-A,B,C). According to the patient's antibiogram sensitivity result, intravenous levofloxacin 750 mg once a day was added to the treatment. Instead of topical fortified vancomycin, levofloxacin drops were started hourly. In the follow-ups, the hypopyon regressed and completely disappeared after 11 days. However, due to the development of phacomorphic glaucoma, narrowing of the anterior chamber in the left eye, and non-resolving vitreous haze on ultrasonography, combined phacoemulsification and pars plana vitrectomy were performed (Fig. 1-H). In her follow-ups, her cornea was clear, there was no reaction in the anterior chamber, no hypopyon was observed, and there was no vitritis.
Discussion
S. maltophilia is an opportunistic infection that is a rare cause of endophthalmitis and cases of S. maltophilia-related endophthalmitis have often been reported following cataract surgery, trauma or intravitreal injections [11,12,13]. We present a case of S. maltophilia endophthalmitis after keratoplasty, which is a rare entity in the literature.
There are some cases in the literature who underwent intravitreal injection for various reasons and subsequently developed S. maltophilia endophthalmitis. Boeke et al. reported S. maltophilia endophthalmitis developing 1 month later in a 70-year-old female patient who underwent intravitreal aflibercept for diabetic macular edema. Due to the suspicion of endophthalmitis a tap procedure was performed and then intravitreal vancomycin, ceftazidime and dexamethasone were injected. Topical prednisolone acetate 1% every hour, topical moxifloxacin 4 times daily and cyclopentolate 3 times daily were started. Then S. maltophilia growth was observed in the patient's aqueous humor, and his clinical improvement was observed with the continuation of the topical treatment and the need for vitrectomy did not arise [13]. Our patient did not have severe pain as stated in this case. Although hypopyon was also observed in our patient, a fibrinous reaction occurred in the anterior chamber first, and then it was gradually replaced by hypopyon. Since condensation in the vitreous and phacomorphic glaucoma developed in the follow-up of our patient, combined phaco-vitrectomy surgery was performed.
Karakurt et al. reported 6 cases who developed S. maltophilia endophthalmitis between 1 and 19 days after cataract surgery [14]. In addition, Chang et al. reported 8 cases of S. maltophilia endophthalmitis that occurred following cataract surgery [11]. Vitrectomy was required in 3 of these 8 patients. Similarly, Ji et al. published 14 cases of S. maltophilia endophthalmitis that occurred between 1 and 56 days postoperatively after cataract surgery [15]. As can be seen, S. maltophilia endophthalmitis cases in the literature were generally seen after cataract surgery. In our patient, we encountered an endophthalmitis that gradually appeared after keratoplasty.
In addition to all these, there are also cases of S. maltophilia endophthalmitis reported after ocular traumas. Lai et al. reported a case of S. maltophilia endophthalmitis after penetrating injury by a wooden splinter [12]. Patton et al. brought to the literature a case of S. maltophilia endophthalmitis in a patient with intraocular metallic foreign body after trauma [16]. Also, Kherani et al. published a S. maltophilia endophthalmitis case following penetrating corneal injury [17]. As it is known, due to impaired sterility in intraocular penetrating injuries, we frequently encounter endophthalmitis as in these cases. However, we usually see rapidly progressive endophthalmitis in these patients. In our patient, the fibrin reaction that occurred after keratoplasty was followed for a while, then it was replaced by a hypopyon, but the size of this hypopyon remained more stable than in classical endophthalmitis.
In a case published by Díez-Álvarez et al., a case of S. maltophilia-associated keratitis-endophthalmitis has been reported. In this case, an 84-year-old female patient developed a persistent epithelial defect and a dense stromal infiltrate after descemet stripping automated endothelial keratoplasty (DSAEK) surgery and S. maltophilia growth has been reported in the corneal scraping sample taken. Complete recovery was achieved in 3 weeks after oral and topical trimethoprim-sulfamethoxazole (TMP/SMX) treatment. This case emphasized the importance of keeping in mind that S. maltophilia may also be a factor in keratitis after corneal transplantation [18]. In our case, there was a patient who developed S. maltophilia-related endophthalmitis after penetrating keratoplasty, presented with progressively increasing inflammation, fibrin reaction and vitreous condensation, and was more resistant to heal.
There is one case report describing S. maltophilia keratitis that developed after penetrating keratoplasty surgery [19]. In this case, a 70-year-old patient complained of decreased vision 5.5 months after the surgery and S. maltophilia was isolated in corneal scraping samples. In this patient, as in our patient, the treatment plan was shaped according to the antibiotic susceptibility test and it was observed that the keratitis was completely resolved in 2.5 months with topical 0.3% ciprofloxacin hydrochloride treatment. In our patient, unlike this patient, S. maltophilia-related endophthalmitis was observed after keratoplasty, and the time of occurrence in our case was seen earlier after keratoplasty.
Conclusion
Although S. maltophilia is a rare cause of endophthalmitis, microbiological samples should be taken from the vitreous and anterior chamber when there are findings in favor of endophthalmitis on examination. We should start the appropriate endophthalmitis treatment without waiting for the culture result and adjust the treatment by switching to appropriate sensitive antibiotics when S. maltophilia grows. It can be confused with inflammatory conditions, such as anterior chamber fibrinous reaction. S. maltophilia should be kept in mind in endophthalmitis that develops after any interventional procedure to the eye.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
References
Denton M, Kerr KG (1998) Microbiological and clinical aspects of infection associated with Stenotrophomonas maltophilia. Clin Microbiol Rev 11:57–80
Berg G (2009) Plant-microbe interactions promoting plant growth and health: perspectives for controlled use of microorganisms in agriculture. Appl Microbiol Biotechnol 84(1):11–18
Hoefel D, Monis PT, Grooby WL, Andrews S, Saint CP (2005) Profiling bacterial survival through a water treatment process and subsequent distribution system. J Appl Microbiol 99(1):175–186
Jucker BA, Harms H, Zehnder AJ (1996) Adhesion of the positively charged bacterium Stenotrophomonas (Xanthomonas) maltophilia 70401 to glass and Teflon. J Bacteriol 178(18):5472–5479
Brooke JS (2012) Stenotrophomonas maltophilia: an emerging global opportunistic pathogen. Clin Microbiol Rev 25(1):2–41
Mauger TF, Kuennen RA, Smith RH, Sawyer W (2010) Acanthamoeba and Stenotrophomonas maltophilia keratitis with fungal keratitis in the contralateral eye. Clin Ophthalmol 21(4):1207–1209
Lin HC, Ma DH, Chen YF, Yeh LK, Hsiao CH (2011) Late-onset intrascleral dissemination of Stenotrophomonas maltophilia scleritis after pterygium excision. Cornea 30(6):712–715
Penland RL, Wilhelmus KR (1996) Stenotrophomonas maltophilia ocular infections. Arch Ophthalmol 114(4):433–436
Wladis EJ (2011) Dacryocystitis secondary to Stenotrophomonas maltophilia infection. Ophthalmic Plast Reconstr Surg 27(5):e116-7
Akçakaya AA, Sargin F, Erbil HH, Yazici S, Yaylali SA, Mesçi C, Ergin S, Midilli K (2011) A cluster of acute-onset postoperative endophthalmitis over a 1-month period: investigation of an outbreak caused by uncommon species. Br J Ophthalmol 95(4):481–484
Chang JS, Flynn HW Jr, Miller D, Smiddy WE (2013) Stenotrophomonas maltophilia endophthalmitis following cataract surgery: clinical and microbiological results. Clin Ophthalmol 7:771–777
Lai TY, Kwok AK, Fung KS, Chan WM, Fan DS, Lam DS (2001) Stenotrophomonas maltophilia endophthalmitis after penetrating injury by a wooden splinter. Eye (Lond) 15(Pt 3):353–354
Boeke PS, Gottlieb JL (2019) Stenotrophomonas maltophilia endophthalmitis 1 month after intravitreal aflibercept. Retin Cases Brief Rep 13(4):327–328
Karakurt A, Abdik O, Sengün A, Karadağ R, Saricaoğlu S, Sarikatipoğlu HY, Hasiripi H (2006) Stenotrophomonas maltophilia Endophthalmitis after cataract extraction. Ocul Immunol Inflamm 14(1):41–46
Ji Y, Jiang C, Ji J, Luo Y, Jiang Y, Lu Y (2015) Post-cataract endophthalmitis caused by multidrug-resistant Stenotrophomonas maltophilia: clinical features and risk factors. BMC Ophthalmol 24(15):14
Patton N (2001) Post-traumatic endophthalmitis caused by Xanthomonas maltophilia. Eye (Lond) 15(Pt 6):801–802
Kherani F, Kherani A, Gehrs KM, Heilskov TW, Sutphin JE, Wagoner MD (2002) Xanthomonas maltophilia endophthalmitis following penetrating corneal injury. Can J Ophthalmol 37(5):301–303
Díez-Álvarez L, Lumbreras-Fernández B, García-Pérez JL (2015) Stenotrophomonas maltophilia keratitis treated with trimethoprim-sulfamethoxazole. Arch Soc Esp Oftalmol 90(11):539–41 (English, Spanish)
Fernandes M, Gangopadhyay N, Sharma S (2005) Stenotrophomonas maltophilia keratitis after penetrating keratoplasty. Eye (Lond) 19(8):921–923
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Patient diagnosis and follow-up were made by EKA and MAY, keratoplasty by EKA, phaco-vitrectomy by MAY, microbiological tests by BÖ, data collection by BT. The first draft of the manuscript was written by BT and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study complies with the principles of the Declaration of Helsinki. The study was approved by the review board of the Ankara Bilkent City Hospital. Written informed consent was obtained from the patient.
Consent for publication
Written informed consent to publication (including images, personal and clinical details of the participant) was obtained from the patient.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Tarım, B., Yorgun, M.A., Özdem, B. et al. Stenotrophomonas maltophilia endophthalmitis following keratoplasty. J Ophthal Inflamm Infect 13, 46 (2023). https://doi.org/10.1186/s12348-023-00368-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12348-023-00368-9