Abstract
Dust events are concerning due to their potential to cause environmental pollution and health issues by carrying numerous particles from various regions. However, the risks of airborne bacteria from dust have not yet been thoroughly investigated. This study aimed to reveal the particle size distribution, antibiotic resistance, microbial community structure, and diversity of airborne bacteria by using culture methods, and assess the potential health risks by calculating the dose expectation \((\overline{d })\), daily short-term intake (STI), and Hazard Index (HI) during an extreme dust event in urban Beijing (China). Airborne bacteria were sampled before, during, and the day after a severe dust event in March 2021 in Beijing using the six-stage impactor. The major findings were as follows: (1) airborne bacterial concentration increased during the dust event, and inhalable bacteria account for 67.93%. The Hazard Index (HI) of cultivable and inhalable airborne bacteria in men, women, and children exposed to dust events was up to 1.42 and 1.54 times higher than that in individuals who were not exposed, respectively. HI was 1.52 times higher in children than in men when exposed to the dust event. (2) The percentage of Gram-positive bacteria (GPB) resistant to different antibiotics was altered. The abundance of ciprofloxacin-resistant bacteria increased by 24.51%, while that of clindamycin-resistant bacteria decreased by 34.64%. The \(\overline{d }\), STI, and HI of antibiotic-resistant bacteria per breath for men, women, and children after the dust event were 14 times greater than those before the dust event. (3) The diversity of airborne bacteria increased throughout the dust event. Opportunistic bacteria were found after the dust event. From a health perspective, airborne bacteria during extreme dust events should be further studied for their sources, changes, human exposure, and so forth. Government-scale measures are necessary to control dust dissemination.
Graphical Abstract

Highlights
-
Airborne bacterial concentration reached 27,611.31 CFU/m3 during dust event
-
Health risk of inhalable bacteria exposed to dust increased to 1.54 times
-
Risk of antibiotic-resistant bacterial exposure increased to 14 times after dust
-
Staphylococcus hominis and Kocuria rosea were discovered
Similar content being viewed by others
Introduction
Dust events are defined as strong winds that roll up large amounts of dust from the ground, making horizontal visibility less than 1 km, and are characterized by suddenness, short duration, small probability, and high hazard [1]. In Asia, they mostly occur in early spring and affect the atmosphere and, consequently, human health. High-speed winds can aerosolize dry soil into dust in the atmosphere, and the deserts of Mongolia and northwestern China alone release an average of 800 trillion grams of dust each year [2]. Chemicals (organic substances and heavy metals) and biological components (bacteria, fungus, and allergies) bonded to dust particles can travel vast distances from a source [3].
Dust particles are present in the atmosphere at several hundred times the normal level during a dust event. Dusts containing various toxic chemicals, germs, etc., can pass through layers of defense to enter the mouth, nose, eyes, and ears, causing adverse human health outcomes [4, 5]. There was a 39% increase in emergency admissions in Brisbane and a 20% increase in respiratory emergency department attendances in Sydney during the first extreme dust event across Australia in 2009 [6, 7]. There was an increase of 7.66% and 4.92% in the number of deaths due to respiratory diseases on the first and second days after a dust storm in Taipei, respectively [8]. All-cause mortality increased by 7.4% and cardiopulmonary mortality increased by 7% on the day of the dust event, and its effect on mortality lasted until the next day [9].
The content and concentration of bioaerosols also altered dramatically during dust episodes [5, 10]. Bacterial concentration could reach 495.95 CFU/m3 during the dust events in Iran, which is four times higher than it is on non-dust days [11]. The majority of cultivable airborne bacteria were brightly colored GPB during a dust event in Beijing, with strains belonging to the Actinobacteria and Firmicutes phyla dominating [12]. The relative abundance of desert soil-associated bacteria increases during dust events, which carry virulence factors and antibiotic resistance genes that can be horizontally transferred to local microbes, while that of anthropogenic-influenced taxa decreases [13]. But the relative abundance of the intI1, qnrS, and sul1 genes decreased by two orders of magnitude during the Eastern Mediterranean dust event [14]. The surge in bioaerosols carried by dust events increases the allergen burden, the incidence of asthma, and the spread of diseases such as Kawasaki disease [15, 16].
Inhalation and cutaneous exposure are the main ways that humans are exposed to bioaerosols. They may have negative health effects depending on the microorganism's host, pathogenicity, antibiotic resistance, and exposure level [17,18,19,20,21,22]. Previous research on bioaerosol health risk assessment has primarily focused on environments like wastewater treatment plants, landfills, hospitals, and farms [18, 20, 23, 24]. Zhang et al. conducted a quantitative microbial risk assessment (QMRA) and found that airborne pathogens from wastewater treatment plants pose exponentially decreasing health risks to workers and nearby residents with increasing distance [18]. Yang et al. used a U.S. Environmental Protection Agency (EPA)-recommended model to calculate the average daily dose (ADD) and assessed the health risks of exposure to airborne bacteria in various treatment facilities within wastewater treatment plants [20]. Wendy et al. used the BIOGAVAL method to assess the occupational exposure of landfill workers to antibiotic-resistant bacteria bioaerosols, finding notably high average concentrations [23]. Zhou et al. suggested using STI exposure doses for antibiotic resistance risk assessment. They observed that the occupational intake of antibiotic resistance genes (ARGs) in pig farms and hospitals was 110 and 29 times higher in suburban areas, respectively [24]. Yet, acceptable bioaerosol threshold limits remain undefined, and suitable dose–response relationships are lacking.
The risks of inhalation or antibiotic-resistance of airborne bacteria caused by the sharp rise in microbial concentrations during dust events are currently not sufficiently understood by the public. This study investigated a mega dust event in Beijing, China, based on the culture method. Potential risks were quantitatively evaluated based on bacterial concentration and exposure dose. Particle size distribution, antibiotic resistance, and bacterial community structure were also analyzed to further highlight possible risks. The purpose is to look into the distribution of cultivable bacteria and their antibiotic resistance during dust events, to quantify the health risks associated with regional bioaerosols, to understand the potential health issues, and to provide useful references for the development of preventive and control measures during dust events.
Materials and methods
Site description and air sampling
Air samples were collected before, during, and after the dust event, i.e., at 9 a.m. on March 11, 15, and 16, 2021, respectively (Fig. 1D). During this event, the sand swirled through the air and the skies were a hazy orange, with the PM10 concentration reaching 6450 µg/m3 and rising fourfold within an hour on March 15 in Beijing [25]. The sampling point was the sixth floor (approximately 15 m above the ground) of the Experiment Building at the National Institute of Environmental Health (NIEH, 39°52′48″N, 116°27′26″E) of the Chinese Center for Disease Control and Prevention in the Chaoyang district of Beijing [26]. Air samples were collected using the six-stage impactor (Liaoyang Kangjie Instrument Research Institute, China) with cut-off diameters > 7.0, 4.7–7.0, 3.3–4.7, 2.1–3.3, 1.1–2.1, and 0.65–1.1 μm at a flow rate of 28.3 L/min for 5 min. Each successive stage represents the nose and mouth, pharynx, trachea and primary bronchi, secondary bronchi, terminal bronchi, and alveoli of the human respiratory system. The third to sixth stages of the sampler correspond to the inhalable particulate matter mentioned in this study [27]. Inhalable particles were defined as particles with an aerodynamic diameter less than 4.7 μm that can enter the lower respiratory tract (the bronchi, fine bronchi, and alveoli) [28]. Nutrient agar (NA; Guangzhou Detgerm Microbiological Science Ltd., China) culture plates with a diameter of 90 mm were directly placed on all six stages of the sampler to collect airborne bacteria.
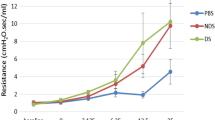
Airborne bacterial composition during a dust event. A Distribution of cultivable airborne bacterial concentration at different particle sizes before, during, and the day after the extreme dust event. B Proportions of cultivable airborne bacterial concentration at different particle sizes before, during, and the day after the extreme dust event. C Proportions of cultivable airborne antibiotic-resistant bacteria at different particle sizes before and the day after the extreme dust event. (The Roman numerals I to VI represent the different stages of the six-stage sampler.) D Representative photographs before, during, and the day after an extreme dust event of Beijing’s urban area (taken at the same spot). E Composition of cultivable airborne bacteria at genus level. The inner and outer rings represent before and the day after the extreme dust event, respectively
Sample culture and counting
After collection, the culture medium was placed in a constant temperature incubator at 37 ℃. The number of colony-forming units (CFUs) was counted manually after 48 h. Concentrations are expressed as colony-forming units per cubic meter of air (CFU/m3). During sampling, superposition occurred when microbial particles touched the same spot through the same pore of the sampler. The counting results of each sample were therefore statistically corrected according to Andersen [26].
Bacterial isolation and identification
Each colony from the samples taken on March 11 and March 16, 2021—representing the day before and after the dust event, respectively—was picked up separately onto the blood agar media (Columbia) (Thermo Fisher Scientific, USA) using an inoculation loop and incubated at 37 °C for 24 h. To make sure that the colonies developing on each final culture plate were of a single bacterial species, the aforementioned stages were done twice.
Each isolated purified cultivable bacterial total genomic DNA was extracted using a prepGEM® Bacteria DNA Extraction Kit (ZyGEM, New Zealand). Following polymerase chain reaction (PCR) amplification of the 16S ribosomal RNA (rRNA) gene using the universal primer pair 27F/1492R, the amplified gene was cloned and sequenced (ABI3730XL, Majorbio, China). Nucleotide Basic Local Alignment Search Tool (BLAST) searches against the National Center for Biotechnology Information (NCBI)'s 16S rRNA gene sequence reference database (https://blast.ncbi.nlm.nih.gov/Blast.cgi) were used to identify each purified cultivable bacterial isolate, and taxonomic data, including information on Gram positivity, were obtained for each identified cultivable bacterium from the NCBI Taxonomy database (https://www.ncbi.nlm.nih.gov/Taxonomy/Browser/wwwtax.cgi).
Antimicrobial susceptibility testing (AST)
The AST was carried out using the minimal inhibitory concentration (MIC) agar dilution method with AST plates (Biofosun, China). Specific antibiotics from more than 10 popular classes that are used to treat both GPB and Gram-negative bacteria (GNB) were applied to the wells of each AST plate in gradient concentrations [29] (Additional file 1: Tables S1 and S2). Antibiotic classes included penicillins, β-lactam/-lactamase inhibitor combinations, cephems, lipopeptides, glycopeptides, penems, macrolides, lincosamides, macrolide–lincosamide combinations, pseudomonic acid, fluoroquinolones, folate pathway inhibitors, tetracyclines, phenicol, and aminoglycosides. Antibiotics were not used to treat the negative and positive control wells. Single bacterial isolate colonies were suspended in nutrient broth (NB) and diluted to 1.5 × 108 CFU/mL according to the McFarland standard. Each bacterial suspension was applied to all wells of one AST plate except the negative control well, which contained just NB. The AST plates were then incubated for 18–20 h at 37 °C. Following incubation, the plates were manually read according to the manufacturer's instructions and assessed using the MIC values given in the Clinical and Laboratory Standards Institute's standards [30].
Health risk assessment
Dose expectation
The average dosage of exposure is the \(\overline{d }\). The number of microorganisms in the media and the volume of media consumed are also issued in calculating exposure. Quantity refers to the concentration of cultivable airborne bacteria in this study, while medium consumption refers to the volume of air inhaled. The following formula can be used to calculate the dose expectation [31]:
where μ is the concentration and m is the consumption per exposure (Additional file 1: Table S3). If μ and m are statistically independent, the \(\overline{d }\) can be estimated using the formula below:
Daily short-term intake
The following equations were used to assess airborne bacterial exposure [24]:
where Ci is the bacterial concentration, \({IR}_{i}\) is the inhalation rate, and \({t}_{i}\) is the exposure time. If \({\sum }_{{\text{i}}=1}^{{\text{n}}}{t}_{i}(hr)=24(hr)\), then STI represents the population’s daily inhalation of bacteria.
Non-carcinogenic risk
The exposure rates and risk assessment of airborne bacteria were estimated using the models recommended by the U.S. EPA, which have been verified in previous studies [20, 32, 33]. The ADD through the inhalation and skin exposure pathways and the risk quotient characterized by the hazard quotient (HQ) and HI were calculated using the following equations:
where \({ADD}_{inhalation}\) and \({ADD}_{skin}\) represent the average daily doses of exposure by inhalation and skin contact [CFU/(kg \(\cdot\) d)], respectively; C is the airborne bacterial concentration (CFU/m3); IR is the inhalation rate (m3/d); EF is the exposure frequency (d/yr), assuming most individuals spend about 20% of their time outdoors [34]; \({ED}_{inhalation}\) and \({ED}_{skin}\) are the durations of exposure by inhalation and skin contact (yr), respectively; SA is the surface area of skin contact (m2); ABS is the dermal absorption factor (m/h); AF is the skin adherence factor; BW is the body weight (kg); and AT is the average lifetime (d). RfD is the reference dose [CFU/(kg \(\cdot\) d)], representing the maximum acceptable daily dose of a substance. The RfD of airborne bacteria has not been determined until now. Concentrations of the cultivable bacterial exposure should not exceed 500 CFU/m3 on a working day, as recommended by the Bioaerosols Committee of the American Conference of Governmental Industrial Hygienists (ACGIH). Therefore, the limit of 500 CFU/m3 was applied in this study. All the parameters are summarized in Additional file 1: Table S3. Health risks could be ignored when HQ and HI are lower than 1; however, the risks should be examined further when the HQ and HI are higher than 1 [35].
The urban area of Beijing was assumed to experience 3 days of dust events annually based on the number of dust events that have occurred over previous years. HQ for individuals exposed to dust events was estimated using the following formulas:
Select the cultivable bacteria concentration from 10 air samples of dust-free weather between January and March 2021 as the non-dust concentration (cultivable bacteria: 550.53 CFU/m3; inhalable bacteria: 289.04 CFU/m3, Additional file 1: Table S4).
Data analysis
Statistical analyses were conducted using Microsoft Excel 2010. A database was established first, and the data were then analyzed and visualized.
Results and discussion
Health risks of airborne bacteria concentration through the dust event
Airborne bacterial concentrations increased during the dust event. The concentration was as high as 27,611.31 CFU/m3 during the dust event (DD), which was 260 and 16 times higher than that before the dust event (BD) and after the dust event (AD), respectively, and the airborne bacterial concentration in AD was 16.5 times higher than in BD (Fig. 1A and Additional file 1: Table S5). This is in line with previous studies that have shown that severe dust events can elevate airborne bacterial concentrations [36]. For example, the respective airborne bacterial concentration increased by 4.3- and 7-times during dust events in Daejeon and Seoul, Korea [37, 38]. There is a 1000-fold increase in bacterial abundance during a severe Asian dust event in Beijing, relative to non-Asian dust days [8]. According to the Bioaerosols Committee of ACGIH, the concentration of cultivable bacteria surpassed the limit of 500 CFU/m3 by nearly 55 and 5 times for DD and AD, respectively. Airborne microorganisms mostly adhere to particulate matter [39, 40]. We observed that the AQI, PM2.5, and PM10 concentrations were quite high, which was compatible with the elevated levels of bacterial concentrations observed during the dust events (Additional file 1: Tables S5 and S6). The PM10 concentration in DD reached 9753 µg/m3, which is 58 and 137 times higher than that in BD and AD, respectively. Meanwhile, the PM2.5 concentration reached 705 µg/m3, which is 3 and 47 times higher than that in BD and AD, respectively (Additional file 1: Table S6). The majority of airborne bacteria are found in bacterial aggregates or in combination with other particles. Particles can give nutrients and a bigger surface area for bacteria to survive in the air, as well as protection from UV radiation and desiccation [39, 40]. The significant increase in airborne bacterial concentration is primarily attributed to the elevated particulate matter levels during dust events [41]. Consider that many airborne bacteria cannot grow on culture media. The rise in the number of cultivated bacteria during DD and AD suggests that the actual health risks may be higher because of the more viable bacteria that are able to proliferate in the environment [42].
The proportion of inhalable airborne bacteria increased during the dust event. 67.93% of airborne bacteria were inhalable in the DD group, which means they settled on stages 3 to 6 (0.65–4.7 μm) of the sampler, while 53.33% and 52.63% were inhalable in the BD and AD groups, respectively (Fig. 1B and Additional file 1: Table S5). The proportion of inhalable airborne bacteria carried on such smaller particles increased by more than 10% in the DD group. Bacterial particle sizes differed among groups. The AD group had the highest concentration on stage 5 (1.1–2.1 μm), DD on stage 1 (> 7.0 μm), and BD on stage 3 (3.3–4.7 μm). The cut-off diameter from the 3rd to the 6th stage of the sampler corresponds to the regions of the human respiratory system, including the trachea and primary bronchi, secondary bronchi, terminal bronchi, and alveoli, respectively. As wind blows dust from the ground, airborne bacteria mainly inhabit large-sized particles. These larger particles gradually settle after the dust event, while the smaller, inhalable particles remain suspended in the air. A study conducted in Italy has shown that during dust storms, there is a significant increase in the concentration of small-sized bacteria. However, research on airborne microorganisms transported by Saharan dust in the Mediterranean region indicated a faster increase in the concentration of larger-sized bacteria. This suggests that there may be differences in the particle size distribution of airborne bacteria during different dust events [43,44,45]. An increase in the proportion of inhalable airborne bacteria during the dust event also indicates an elevated health risk in the lower respiratory tract.
Exposure risks to airborne bacteria were dramatically increased by the dust event. The \(\overline{d }\) and STI of cultivable bacteria per breath for men, women, and children in the DD group were 260 times greater than those in the BD group (Table 1). The \(\overline{d }\) and STI of cultivable bacteria per breath for men, women, and children in the AD group were 16 times greater than those in the BD group. The HI of individuals exposed to dust events was 1.42 times higher than that of individuals who were not exposed. Inhalable bacteria exhibit a more noticeable disparity before, during, and after the dust event. The \(\overline{d }\) and STI of inhalable bacteria per breath for men, women, and children in the DD group were 332 times greater than those in the BD group (Table 1). The \(\overline{d }\) and STI of inhalable bacteria per breath for men, women, and children in the AD group were 16 times greater than those in the BD group. HI of individuals exposed to dust events was 1.54 times higher than that of individuals who were not exposed. HI was 1.52 times greater in children than in men when exposed to the dust event (Additional file 1: Table S7). Inhalation exposure poses far greater health risks to both adults and children than does skin exposure. Although inhaled dose of airborne bacteria was high, the total HI in the DD group was less than 1. The \(\overline{d }\) value represents the average of a single exposure, while STI is the daily intake for the population. Both are quantitative indicators, but corresponding limits have not been established yet. HI is a qualitative assessment that can be used to determine the presence of health risks based on their magnitude, but it cannot quantify the extent of the risk. Therefore, combining multiple assessment methods can yield a more comprehensive conclusion.
Health risks before and after the dust event
Antibiotic resistance of cultivable airborne bacteria
Antibiotic resistance of cultivable airborne bacteria altered after the dust event. Resistance to penicillin, ampicillin, ciprofloxacin, and sulfamethoxazole increased, while resistance to clindamycin decreased in the AD group compared to the BD group (Table 2). Some of the airborne bacterial genera that are resistant to these antibiotics have properties such as resistance to desiccation or ultraviolet light, which allow them to survive during atmospheric transport [46]. Antibiotic-resistant bacteria in soil may also be transported through the atmosphere on dust particles [47]. The proportion of bacteria resistant to these antibiotics was greater in soil in areas where dust originated and passed than in Beijing. Given the increase in concentrations of airborne bacteria carried by dust, a high number of bacteria resistant to these above antibiotics may enter the atmosphere during the dust event. But several previous studies conducted using high-throughput sequencing have shown that during dust events, there was a decrease in the abundance of ARGs in the air compared to clear days [13]. Most notably, the majority of cultivable bacteria (BD: 77.78%, AD: 89.22%) displayed β-lactam resistance (including penicillin and ampicillin). Approximately 52% of the cultivable airborne GPB were found to be β-lactam resistant during another dust event in Beijing [48]. Horizontal gene transfer of β-lactam resistance can spread antibiotic resistance in the environment [49]. β-Lactam resistance genes threaten the last frontier for antibiotics and therefore pose a serious threat to human health. The sources of airborne ARGs are likely local, and dust events do not seem to be an important vector for the transport of ARGs. A higher percentage of cultivable airborne bacteria in the 1 to 2 stages were resistant to ampicillin, vancomycin, amikacin, and ciprofloxacin in the first and second stages in the AD group (Fig. 1C). The concentrations of PM10 and PM2.5 sharply increase as strong winds transport particulate matter laden with microorganisms to Beijing during a sandstorm. High quantities of bacteria that are resistant to the aforementioned kinds of antibiotics may be present in soil or air in dust source and dust pathway areas. Considerably more bacteria in the 3–6 stages (inhalable particle size) were resistant to penicillin and trimethoprim/sulfamethoxazole in the AD group. A greater quantity of microscopic particles lingered in the air for a considerable amount of time after dust events. They act as vehicles which transport tiny antibiotic-resistant bacteria into the lower respiratory systems of people and even enter the alveoli. Once colonized, they can spread horizontally and vertically, passing on resistance genes to other bacteria in the body and increasing the risk to human health [50].
The distribution of multidrug-resistant (MDR) bacteria was not much different before and the day after the dust event. MDR accounted for 9.01% (10/111) of all cultivable bacteria (BD: 1/9, 11.11%; AD: 9/102, 8.82%, Table 2). MDR bacteria in the BD group were resistant to penicillin (1/1), sulfamethoxazole (1/1), and tetracycline (1/1), and those in the AD group were resistant to penicillin (9/9), ampicillin (8/9), sulfamethoxazole (7/9), and Ciprofloxacin (6/9). Most of the aforementioned antibiotics are broad-spectrum antibiotics. MDR bacteria are an acute risk factor for respiratory illness, and thus, the management and regulated use of broad-spectrum antibiotics should be strengthened in the future [51].
Exposure to airborne antibiotic-resistant bacteria increased after the dust event. The concentrations of cultivable airborne antibiotic-resistant bacteria (bacteria resistant to at least one antibiotic) were 49.47 CFU/m3 and 592.58 CFU/m3 in the BD and AD groups, respectively. The \(\overline{d }\), daily STI values and HI of airborne antibiotic-resistant bacteria per breath for men, women, and children in the AD group were 14 times greater than those in the BD group (Table 3). HI of airborne antibiotic-resistant bacteria was 1.52 times greater in children than in men (Additional file 1: Table S8). Previous studies have indicated that the inhalation risk values for adults, regardless of heavily or lightly polluted days, are less than 1 in Qingdao [12]. Similarly, the maximum HQ values for airborne bacteria and fungi were also lower than 1 in the Pearl River Estuaries [52]. Additionally, the average inhalation risks for both adult males and females in wastewater treatment plants were less than 1 [20]. All above suggests that the inhalation risks can be neglected. However, it is important to note that more attention should be paid to the health hazards posed by bioaerosols when special weather occurs. Further research on antibiotic-resistant bacteria introduced in the atmosphere during dust events is warranted to assess the health risks posed by these bacteria.
Diversity of cultivable airborne bacteria
The diversity of airborne bacteria increased after the dust event. At the phylum level, Firmicutes and Actinobacteria were dominant among cultivable airborne bacteria in the BD and AD groups, respectively (Additional file 1: Fig. S1B). Proteobacteria, Firmicutes, Actinobacteria, and Bacteroidetes were the main phyla in the atmospheric dust of the Red Sea dust event [53]. Similar bacterial classification distributions were found in previous Beijing dust events, albeit with differences in their relative abundances [5]. Another research in Beijing found dominant bacterial phyla and classes were Actinobacteria, Bacilli, and Acidobacteria during Asian dust [54]. At the genus level, Bacillus was dominant among 7 genera in the BD group (40.00%, Fig. 1E). 16 genera were found in AD group, with Arthrobacter being the dominant genus (45.83%) and Bacillus falling to 13.33%. Previous studies found the absolute dominance of Bacillus in non-dust conditions using culture methods [55, 56]. Arthrobacter is widely present in various environments, especially soil, where its abundance is related to its ability to degrade a variety of contaminants, such as dibutyl phthalate [57]. Moreover, Arthrobacter is strongly resistant to dry conditions and is easily transported by air. Its capability to preserve DNA integrity while traversing the atmosphere may have played a role in its prevalence. Coarse particulate matter can protect microbial cells against damage in harsh environmental conditions and can provide them with energy and a carbon source [58]. Dust particles tend to introduce soil microorganisms into the atmosphere, resulting in changes in composition of the airborne bacterial community. During the Asian dust event, air samples from the East China Sea yielded a significant amount of bacteria that could be effectively isolated and cultivated, proving that the dust contained live bacteria [59]. Air samples taken 15 days after the dust event were more similar in microbial composition to those taken during the dust event than to those taken before the dust event in the Iberian Peninsula [60]. Thus, dust events can cause significant perturbations in the composition of airborne bacterial communities.
Opportunistic pathogenic bacteria were discovered in AD group, e.g., Staphylococcus hominis (2 strains) and Kocuria rosea (1 strain). S. hominis is a common commensal bacterium found on human skin and has been found to possess extracellular toxins that can cause cytopathic effects [61]. Both strains of S. hominis were resistant to penicillin, ampicillin, and erythromycin. K. rosea can cause opportunistic infections in species with impaired immune systems [62]. K. rosea strain found in this study was not resistant to any of the antibiotics tested. The bacterial diversity associated with dust events may have an important influence on human, plant, and animal health.
Limitations
First, only air samples before and the day after the dust event were tested for isolation culture and antimicrobial susceptibility testing. The bacterial count in air samples was exceptionally high during the dust event (~1805 colonies). While the appropriate experimental equipment, lab and incubator spaces, financial and labor sources were in shortage. Moreover, we focused on the changes in air bacteria brought by dust events rather than on brief exposure to dust. Second, culture-based methods may have underestimated the concentration of airborne bacteria, as only approximately 0.1% to 75% of the sampled bacteria can be cultured [63]. Some bacterial aerosol particles cannot adhere to the surface of culture medium or are failed to survive during sampling process [64, 65]. In addition, 16S rRNA sequencing is considered the gold standard for bacterial species identification, as it can accurately identify species up to the genus level, surpassing other methods such as biochemical identification [66]. However, it relies on the data available in databases, and the discriminatory power at the inter- and intraspecies level may be insufficient for certain bacterial genera [67]. Third, only one site in a single dust event was examined due to the brief sampling period, limited study area, short sampling durations, high bacterial counts, and heavy workloads.
Conclusion
To the best of our knowledge, this is the first attempt to assess the health risks of cultivable and antibiotic-resistant bacteria before, during, and after an extreme dust event in Beijing, using culture methods. First, the airborne bacterial concentration increased during the dust event, and inhalable bacteria account for 67.93%, indicating a potential health risk to the respiratory tract. The HI of cultivable and inhalable airborne bacteria in men, women, and children exposed to dust events was up to 1.42 and 1.54 times higher than that in individuals who were not exposed, respectively. HI was 1.52 times greater in children than in men when exposed to the dust event. Second, the percentage of GPB resistant to different antibiotics was altered simultaneously. The abundance of ciprofloxacin-resistant bacteria increased by 24.51%, while that of clindamycin-resistant bacteria decreased by 34.64%. The \(\overline{d }\), daily STI values and HI of airborne antibiotic-resistant bacteria per breath for men, women, and children after the dust event were 14 times greater than those before the dust event. Third, the diversity of airborne bacteria at the genus level increased throughout the dust event, and the predominant genus changed from Bacillus to Arthrobacter. Opportunistic pathogenic bacteria Staphylococcus hominis and Kocuria rosea were cultivated after the dust event.
These findings clarify potential health risks by revealing the particle size distribution, antibiotic resistance, and community structure of bioaerosols during dust episodes. These discoveries indicate the need for appropriate preventive and control measures when sandstorms occur. From the perspective of the government, it is important to intensify public awareness campaigns prior to extreme sandstorm events, reminding citizens to take protective measures and, if necessary, implement work-from-home arrangements. From the perspective of the healthcare system, establishing emergency plans for respiratory outpatient services and enhancing relevant healthcare support may have a crucial effect. From the perspective of an individual, it is advisable to stay informed and follow guidelines provided by authorities, e.g., keep windows closed during dust events and for a period afterwards. Usage of an air conditioner or a HEPA filter air purifier is highly recommended. Outdoor activities should be reduced as much as possible. Outdoor workers should halt work, or wear a mask that provides a high level of protection and properly wash their nasal passages and gargle with water after arriving home. Children are more susceptible than adults to respiratory issues during dust events. Hence, it is advisable to keep a close eye on children’s movements and prevent them from engaging in outdoor sports during dust events. Additionally, maintaining good personal hygiene practices and seeking medical attention if necessary are important steps to mitigate potential health impacts.
Future research may (1) observe a longer period after the dust event to collect more data and thus make a more solid conclusion, considering few evidences were found on how long dust events can affect the airborne bacterial community; (2) bring into more representative sites in Beijing or other cities to obtain more general results and scientific insights; (3) combine culture methods, culturomics, and high-throughput sequencing to analyze the diversity and antibiotic resistance of airborne bacteria on dust days to completely assess the relevance of environmental factors and biological risks of the entire dust event.
Availability of data and materials
No datasets were generated or analyzed during the current study.
References
United Nations Environment Programme (2016) Global Assessment of Sand and Dust Storms.
Zhang XY, Arimoto R, An ZS (1997) Dust emission from Chinese desert sources linked to variations in atmospheric circulation. J Geophys Res Atmos 102:28041–28047. https://doi.org/10.1029/97JD02300
Dasari KB, Cho H, Jacimovic R et al (2020) Chemical composition of Asian dust in Daejeon, Korea, during the spring season. ACS Earth Space Chem 4:1227–1236. https://doi.org/10.1021/acsearthspacechem.9b00327
Li J, Wang G, Ren Y et al (2016) Identification of chemical compositions and sources of atmospheric aerosols in Xi’an, inland China during two types of haze events. Sci Total Environ 566–567:230–237. https://doi.org/10.1016/j.scitotenv.2016.05.057
Yamaguchi N, Baba T, Ichijo T et al (2016) Abundance and community structure of bacteria on Asian dust particles collected in Beijing, China, during the Asian dust season. Biol Pharm Bull 39:68–77. https://doi.org/10.1248/bpb.b15-00573
Barnett AG, Fraser JF, Munck L (2012) The effects of the 2009 dust storm on emergency admissions to a hospital in Brisbane, Australia. Int J Biometeorol 56:719–726. https://doi.org/10.1007/s00484-011-0473-y
Merrifield A, Schindeler S, Jalaludin B et al (2013) Health effects of the September 2009 dust storm in Sydney, Australia: did emergency department visits and hospital admissions increase? Environ Health 12:1–7. https://doi.org/10.1186/1476-069X-12-32
Chen Y-S, Sheen P-C, Chen E-R et al (2004) Effects of Asian dust storm events on daily mortality in Taipei. Taiwan Environ Res 95:151–155. https://doi.org/10.1016/j.envres.2003.08.008
Ho HC, Wong MS, Yang L et al (2018) Influences of socioeconomic vulnerability and intra-urban air pollution exposure on short-term mortality during extreme dust events. Environ Pollut 235:155–162. https://doi.org/10.1016/j.envpol.2017.12.047
Maki T, Puspitasari F, Hara K et al (2014) Variations in the structure of airborne bacterial communities in a downwind area during an Asian dust (Kosa) event. Sci Total Environ 488:75–84. https://doi.org/10.1016/j.scitotenv.2014.04.044
Amarloei A, Fazlzadeh M, Jafari AJ et al (2020) Particulate matters and bioaerosols during Middle East dust storms events in Ilam. Iran Microchem J 152:104280. https://doi.org/10.1016/j.microc.2019.104280
Yuan H, Zhang D, Shi Y et al (2017) Cell concentration, viability and culture composition of airborne bacteria during a dust event in Beijing. J Environ Sci (China) 55:33–40. https://doi.org/10.1016/j.jes.2016.03.033
Mazar Y, Cytryn E, Erel Y et al (2016) Effect of dust storms on the atmospheric microbiome in the Eastern Mediterranean. Environ Sci Technol 50:4194–4202. https://doi.org/10.1021/acs.est.5b06348
Gat D, Mazar Y, Cytryn E et al (2017) Origin-dependent variations in the atmospheric microbiome community in Eastern Mediterranean dust storms. Environ Sci Technol 51:6709–6718. https://doi.org/10.1021/acs.est.7b00362
Jorquera H, Borzutzky A, Hoyos-Bachiloglu R et al (2015) Association of Kawasaki disease with tropospheric winds in Central Chile: is wind-borne desert dust a risk factor? Environ Int 78:32–38. https://doi.org/10.1016/j.envint.2015.02.007
Bédard A, Sofiev M, Arnavielhe S et al (2020) Interactions between air pollution and pollen season for rhinitis using mobile technology: a MASK-POLLAR study. J Allergy Clin Immunol Pract 8:1063-1073.e1064. https://doi.org/10.1016/j.jaip.2019.11.022
Kummer V, Thiel WR (2008) Bioaerosols–sources and control measures. Int J Hyg Environ Health 211:299–307. https://doi.org/10.1016/j.ijheh.2007.06.006
Zhang X, Lu B, Chen G et al (2023) Culturable and inhalable airborne bacteria in a semiunderground municipal wastewater treatment plant: distribution, transmission, and health risk assessment. J Hazard Mater 459:132234. https://doi.org/10.1016/j.jhazmat.2023.132234
Chen YH, Yan C, Yang YF et al (2021) Quantitative microbial risk assessment and sensitivity analysis for workers exposed to pathogenic bacterial bioaerosols under various aeration modes in two wastewater treatment plants. Sci Total Environ 755:142615. https://doi.org/10.1016/j.scitotenv.2020.142615
Yang K, Li L, Wang Y et al (2019) Airborne bacteria in a wastewater treatment plant: emission characterization, source analysis and health risk assessment. Water Res 149:596–606. https://doi.org/10.1016/j.watres.2018.11.027
Li Y, Zhang H, Qiu X et al (2013) Dispersion and risk assessment of bacterial aerosols emitted from rotating-brush aerator during summer in a wastewater treatment plant of Xi’an, China. Aerosol Air Qual Res 13:1807–1814. https://doi.org/10.4209/aaqr.2012.09.0245
Rocha-Melogno L, Crank KC, Ginn O et al (2022) Quantitative microbial risk assessment of outdoor aerosolized pathogens in cities with poor sanitation. Sci Total Environ 827:154233. https://doi.org/10.1016/j.scitotenv.2022.154233
Morgado-Gamero WB, Parody A, Medina J et al (2021) Multi-antibiotic resistant bacteria in landfill bioaerosols: environmental conditions and biological risk assessment. Environ Pollut 290:118037. https://doi.org/10.1016/j.envpol.2021.118037
Zhou Z, Shuai X, Lin Z et al (2022) Short-term inhalation exposure evaluations of airborne antibiotic resistance genes in environments. J Environ Sci (China) 122:62–71. https://doi.org/10.1016/j.jes.2021.10.002
Liang P, Chen B, Yang X et al (2021) Revealing the dust transport processes of the 2021 mega dust storm event in northern China. Sci Bull 67:21–24. https://doi.org/10.1016/j.scib.2021.08.014
Mao Y, Ding P, Wang Y et al (2019) Comparison of culturable antibiotic-resistant bacteria in polluted and non-polluted air in Beijing. China Environ Int 131:104936. https://doi.org/10.1016/j.envint.2019.104936
Andersen AA (1958) New sampler for the collection, sizing, and enumeration of viable airborne particles. J Bacteriol 76:471–484. https://doi.org/10.1128/jb.76.5.471-484.1958
Pastuszka JS, Paw UKT, Lis DO et al (2000) Bacterial and fungal aerosol in indoor environment in Upper Silesia, Poland. Atmospheric Environ 34:3833–3842. https://doi.org/10.1016/S1352-2310(99)00527-0
Magiorakos AP, Srinivasan A, Carey RB et al (2012) Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect 18:268–281. https://doi.org/10.1111/j.1469-0691.2011.03570.x
CLSI (2021) Performance standards for antimicrobial susceptibility testing, M100, 31st edn. Clinical and Laboratory Standards Institute, Wayne
Haas CN, Rose JB, Gerba CP (2014) Quantitative microbial risk assessment. John Wiley & Sons, Hoboken
Agency U S E P. Human health risk assessment. Vol. 2022-07-26.
Liu H, Zhang Z, Wen N et al (2018) Determination and risk assessment of airborne endotoxin concentrations in a university campus. J Aerosol Sci 115:146–157. https://doi.org/10.1016/j.jaerosci.2017.09.002
Eguiluz-Gracia I, Mathioudakis AG, Bartel S et al (2020) The need for clean air: the way air pollution and climate change affect allergic rhinitis and asthma. Allergy 75:2170–2184. https://doi.org/10.1111/all.14177
Chen H, Carter KE (2017) Modeling potential occupational inhalation exposures and associated risks of toxic organics from chemical storage tanks used in hydraulic fracturing using AERMOD. Environ Pollut 224:300–309. https://doi.org/10.1016/j.envpol.2017.02.008
Maki T, Noda J, Morimoto K et al (2022) Long-range transport of airborne bacteria over East Asia: Asian dust events carry potentially nontuberculous mycobacterium populations. Environ Int 168:107471. https://doi.org/10.1016/j.envint.2022.107471
Yamaguchi N, Park J, Kodama M et al (2014) Changes in the airborne bacterial community in outdoor environments following Asian dust events. Microbes Environ. https://doi.org/10.1264/jsme2.me13080
Jeon EM, Kim HJ, Jung K et al (2011) Impact of Asian dust events on airborne bacterial community assessed by molecular analyses. Atmospheric Environ 45:4313–4321. https://doi.org/10.1016/j.atmosenv.2010.11.054
Aller JY, Kuznetsova MR, Jahns CJ et al (2005) The sea surface microlayer as a source of viral and bacterial enrichment in marine aerosols. J Aerosol Sci 36:801–812. https://doi.org/10.1016/j.jaerosci.2004.10.012
Wang JD, Levin PA (2009) Metabolism, cell growth and the bacterial cell cycle. Nat Rev Microbiol 7:822–827. https://doi.org/10.1038/nrmicro2202
Liu T, Duan F, Ma Y et al (2023) Classification and sources of extremely severe sandstorms mixed with haze pollution in Beijing. Environ Pollut 322:121154. https://doi.org/10.1016/j.envpol.2023.121154
Su C, Lei L, Duan Y et al (2012) Culture-independent methods for studying environmental microorganisms: methods, application, and perspective. Appl Microbiol Biotechnol 93:993–1003. https://doi.org/10.1007/s00253-011-3800-7
Conte M, Merico E, Cesari D et al (2020) Long-term characterisation of African dust advection in south-eastern Italy: influence on fine and coarse particle concentrations, size distributions, and carbon content. Atmos Res 233:104690. https://doi.org/10.1016/j.atmosres.2019.104690
Federici E, Petroselli C, Montalbani E et al (2018) Airborne bacteria and persistent organic pollutants associated with an intense Saharan dust event in the Central Mediterranean. Sci Total Environ 645:401–410. https://doi.org/10.1016/j.scitotenv.2018.07.128
Lee S, Choi B, Yi SM et al (2009) Characterization of microbial community during Asian dust events in Korea. Sci Total Environ 407:5308–5314. https://doi.org/10.1016/j.scitotenv.2009.06.052
Griffin DW, Gonzalez-Martin C, Hoose C et al (2017) Global-scale atmospheric dispersion of microorganisms. Microbiol Aerosol. https://doi.org/10.1002/9781119132318.ch2c
Chen C, Li J, Chen P et al (2014) Occurrence of antibiotics and antibiotic resistances in soils from wastewater irrigation areas in Beijing and Tianjin, China. Environ Pollut 193:94–101. https://doi.org/10.1016/j.envpol.2014.06.005
Wang M, Yao M, Zhu Y-g (2022) Antibiotic resistance genes and antibiotic sensitivity in bacterial aerosols and their comparisons with known respiratory pathogens. J Aerosol Sci 161:105931. https://doi.org/10.1016/j.jaerosci.2021.105931
Ochman H, Lawrence JG, Groisman EA (2000) Lateral gene transfer and the nature of bacterial innovation. Nature 405:299–304. https://doi.org/10.1038/35012500
Zhou Z-C, Shuai X-Y, Lin Z-J et al (2021) Prevalence of multi-resistant plasmids in hospital inhalable particulate matter (PM) and its impact on horizontal gene transfer. Environ Pollut 270:116296. https://doi.org/10.1016/j.envpol.2020.116296
Guitor AK, Wright GD (2018) Antimicrobial resistance and respiratory infections. Chest 154:1202–1212. https://doi.org/10.1016/j.chest.2018.06.019
Liang Z, Yu Y, Ye Z et al (2020) Pollution profiles of antibiotic resistance genes associated with airborne opportunistic pathogens from typical area, Pearl River Estuary and their exposure risk to human. Environ Int 143:105934. https://doi.org/10.1016/j.envint.2020.105934
Aalismail NA, Díaz-Rúa R, Ngugi DK et al (2020) Aeolian prokaryotic communities of the global dust belt over the Red Sea. Front Microbiol 11:538476. https://doi.org/10.3389/fmicb.2020.538476
Park J, Li PF, Ichijo T et al (2018) Effects of Asian dust events on atmospheric bacterial communities at different distances downwind of the source region. J Environ Sci (China) 72:133–139. https://doi.org/10.1016/j.jes.2017.12.019
Fang Z, Ouyang Z, Zheng H et al (2007) Culturable airborne bacteria in outdoor environments in Beijing, China. Microb Ecol 54:487–496. https://doi.org/10.1007/s00248-007-9216-3
Shaffer B, Lighthart B (1997) Survey of culturable airborne bacteria at four diverse locations in Oregon: urban, rural, forest, and coastal. Microb Ecol 34:167–177. https://doi.org/10.1007/s002489900046
Kong X, Bai Z, Jin T et al (2022) Arthrobacter is a universal responder to di-n-butyl phthalate (DBP) contamination in soils from various geographical locations. J Hazard Mater 422:126914. https://doi.org/10.1016/j.jhazmat.2021.126914
Kim KY, Kim CN (2007) Airborne microbiological characteristics in public buildings of Korea. Build Environ 42:2188–2196. https://doi.org/10.1016/j.buildenv.2006.04.013
Hara K, Zhang D, Matsusaki H et al (2015) UV-tolerant culturable bacteria in an Asian dust plume transported over the East China Sea. Aerosol Air Qual Res 15:591–599. https://doi.org/10.4209/aaqr.2014.03.0067
González-Toril E, Osuna S, Viúdez-Moreiras D et al (2020) Impacts of Saharan dust intrusions on bacterial communities of the low troposphere. Sci Rep 10:6837. https://doi.org/10.1038/s41598-020-63797-9
Szczuka E, Krzymińska S, Bogucka N et al (2018) Multifactorial mechanisms of the pathogenesis of methicillin-resistant Staphylococcus hominis isolated from bloodstream infections. Antonie Van Leeuwenhoek 111:1259–1265. https://doi.org/10.1007/s10482-017-1007-3
Purty S, Saranathan R, Prashanth K et al (2013) The expanding spectrum of human infections caused by Kocuria species: a case report and literature review. Emerg Microbes Infect 2:1–8. https://doi.org/10.1038/emi.2013.71
Lighthart B (2000) Mini-review of the concentration variations found in the alfresco atmospheric bacterial populations. Aerobiologia 16:7–16. https://doi.org/10.1023/A:1007694618888
Fahlgren C, Bratbak G, Sandaa R-A et al (2011) Diversity of airborne bacteria in samples collected using different devices for aerosol collection. Aerobiologia 27:107–120. https://doi.org/10.1007/s10453-010-9181-z
Yoo K, Lee TK, Choi EJ et al (2017) Molecular approaches for the detection and monitoring of microbial communities in bioaerosols: a review. J Environ Sci (China) 51:234–247. https://doi.org/10.1016/j.jes.2016.07.002
Church DL, Cerutti L, Gürtler A et al (2020) Performance and application of 16S rRNA gene cycle sequencing for routine identification of bacteria in the clinical microbiology laboratory. Clin Microbiol Rev. https://doi.org/10.1128/cmr.00053-19
Bosshard PP, Zbinden R, Abels S et al (2006) 16S rRNA gene sequencing versus the API 20 NE system and the VITEK 2 ID-GNB card for identification of nonfermenting Gram-negative bacteria in the clinical laboratory. J Clin Microbiol 44:1359–1366. https://doi.org/10.1128/jcm.44.4.1359-1366.2006
Acknowledgements
We are grateful to all participants. Special thanks to Dr. Y Hu and Dr. JC Han for their helpful recommendations during the manuscript-drafting process. We gratefully acknowledge the editors and reviewers for their careful review, which has substantially improved the quality of our work.
Funding
This work was jointly supported by Population Antibiotic Resistant Bacteria and Antibiotic Resistance Gene Project in Typical Areas (21zxdc05, 22zxdc05 and 23zxdc05), Young Scholar Scientific Research Foundation of National Institute of Environmental Health, China CDC (No.2020YSRF_03), National Science and Technology Basic Resources Survey Project, China (No.2017FY101201), and consultancy project (2023-JB-12-04) by the Chinese Academy of Engineering (CAE).
Author information
Authors and Affiliations
Contributions
YL: investigation, methodology, validation, formal analysis, data curation, writing–original draft. QY: validation, data curation, writing–original draft. PD.: investigation. MH: investigation. FD: data curation. YW: investigation. CD: investigation. XL: investigation. DW: writing–review & editing. ZS: investigation. ST: writing–review & editing, supervision, project administration. YM: conceptualization, writing–review & editing, supervision, project administration. XY: conceptualization, writing–review & editing, supervision, project administration. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
(A) Gram staining results of cultivable airborne bacteria before and the day after the extreme dust event. (B) Composition proportion of the cultivable airborne bacteria at phylum level before and the day after the extreme dust event. Table S1. Antibiotic concentrations of AST plate for gram-positive bacteria (µg/mL). Table S2. Antibiotic concentrations of AST plate for gram-negative bacteria (µg/mL). Table S3. Parameters used in risk assessment. Table S4. Cultivable bacteria concentration from 10 dust-free weather samples between January and March 2021. Table S5. Distribution of airborne bacteria before, during, and the day after the extreme dust event in Beijing’s urban area. Table S6. Environmental parameters of air sample collection. Table S7. HQ and HI of cultivable airborne bacteria and inhalable bacteria with and without dust events. Table S8. HQ and HI of airborne antibiotic-resistant bacteria with and without dust events. Table S9. Abbreviations and full names.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Luo, Y., Yao, Q., Ding, P. et al. Health impacts of an extreme dust event: a case and risk assessment study on airborne bacteria in Beijing, China. Environ Sci Eur 36, 41 (2024). https://doi.org/10.1186/s12302-024-00858-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12302-024-00858-0