Abstract
Background
Xanthogranulomatous pyelonephritis (XGP) is common in middle-age female, involved kidney usually is hydronephrotic, non-functioning and associated with stones but giant hydronephrotic presentation is a very rare.
Case presentation
We report a case of 25-year-old female presented as huge cystic abdominal lump involving left hemi-abdomen and crossing midline associated with pain. On radiological evaluation, she had giant left non-functioning hydronephrotic kidney pushing small and large bowel on right side for which she underwent open simple nephrectomy. To our surprise, her histopathology report was Xanthogranulomatous pyelonephritis. Only one case reported till date of Xanthogranulomatous pyelonephritis presented as giant hydronephrosis in adult.
Conclusion
Xanthogranulomatous pyelonephritis is very rare cause of giant hydronephrosis with a varying clinical and radiological presentation and difficult to diagnose preoperatively.
Diagnosis of XGP should be entertained in case long-standing gross hydronephrotic obstructed, infected kidney with stone disease.
Similar content being viewed by others
1 Introduction
Xanthogranulomatous pyelonephritis (XGP) is a variant of chronic pyelonephritis in which there is massive unilateral destruction of the kidney with the presence of granulomatous tissue. This disease could occur due to defective phagocytosis of bacteria by macrophages during an infection [1]. Xanthogranulomatous pyelonephritis is common in middle-age female, involved kidney usually is hydronephrotic, non-functioning and associated with stones but giant hydronephrotic presentation is very rare. XGP usually confused with renal tumours, and in majority cases, histopathology gives definitive diagnosis [2].
2 Case presentation
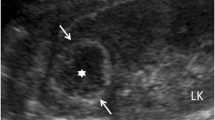
A 25-year-old female patient presented with huge abdominal lump and mild intermittent pain since 2 to 3 years. Patient had no history of other urological symptoms. On examination, she had left-sided abdominal lump of size approximately 20 × 20 x 10cm, which is non-tender, smooth surface, cystic in consistency, crossing midline, and not moving with respiration (Fig. 1b). Her complete blood count, renal function test, and urine culture were normal. On ultrasound evaluation, she had left gross hydronephrosis with papery thin cortex secondary to pelvi-ureteric junction obstruction. Contrast-enhanced computer tomography (CECT) scan of the abdomen was done that showed grossly enlarged hydronephrotic left kidney of size 21.43 × 21.43x13.58 cm with CT-based volume of content 6.2 L, involved abdominal cavity of five vertebral length, paper thinning of cortex, pushing entire small and large bowel on right side, 1.4cm calculi in lower pole and non-excreting kidney on 2 h delayed scan secondary to pelvi-ureteric junction obstruction (PUJO) (Fig. 1a, c, d). Her DTPA scan shows left non-functioning with right normal functioning kidney. Considering huge hydronephrotic non-functioning kidney for which she underwent simple nephrectomy Fig. 2a and intraoperatively more than 6 L of infected fluid [pyonephrosis] was sucked out. Her postoperative course was uneventful and discharged on 10th day. To our surprise, histopathological examination revealed Xanthogranulomatous pyelonephritis with dilated pelvicalyceal system (Fig. 2b).
a, b, c, d CT-based volumetric assessment of giant hydronephrosis (Length X Breadth X Width) 6.2 Litre. Clinical photograph showing huge lump in left hemi-abdomen crossing midline. Axial image of CT scan showing giant hydronephrosis crossing midline and shifting bowel in rt hypochondriac region. Giant hydronephrosis occupying five vertebral levels of abdomen
3 Discussion
Stirling in 1939 defined giant hydronephrosis as the presence of more than one-litre urine or 1.6% of the bodyweight of urine in the collecting system. Radiologically, it is defined as the kidney occupying hemi-abdomen with midline crossing and/or that equals the height of five vertebral bodies (Fig. 1e). It is not common in adults, and diagnosis is often not clear [3].
The differential diagnoses for cystic intra-abdominal mass which resemble giant hydronephrosis includes PUJO, renal cell carcinoma, retroperitoneal tumour, pseudomyxoma, ovarian cyst, and rarely Xanthogranulomatous pyelonephritis [2, 4].
XGP is a chronic suppurative infection involving mostly unilaterally but some bilateral cases have been reported. In this condition, the renal parenchyma replaced by lipid-laden macrophages [1, 5]. Urinary tract obstructions with or without stones, urosepsis, disorders of lipid metabolism, impaired immunity, chronic renal ischaemia, and lymphatic obstructions are the etiological factor. Our case was non-diabetic and non-immune deficient. Kidney involvement in XGP can be focal, segmental or diffuse [1]. In diffuse type, there is tendency to involve the entire kidney and the perirenal tissue, and it mimics renal tumours making differential diagnosis difficult preoperatively. In our case, it was diffuse type of XGP [2, 5].
XGP mostly presents with intermittent flank pain, fever or chills, weight loss, abdominal mass, high blood pressure and urinary tract infection. It is difficult to make diagnosis preoperatively on the basis of radiological imaging like CT or magnetic resonance imaging but there still were certain radiological signs which help in diagnosis. Radiological and clinical findings which help in diagnosing XGP were unilateral or bilateral enlargement of kidneys, kidney or ureteral stones, pyonephrosis, multiple subcortical anechoic lesions and multiple sites with abscess density at the parenchyma. Leucocytosis and anaemia with positive urine culture which usually grows bacteria like Proteus mirabilis and Escherichia coli are usual laboratory findings in XGP [1, 2, 5].
The most important aspect of management of XGP is early diagnosis, aggressive antimicrobial treatment but most of the time treatment is surgical. Open nephrectomy is treatment of choice most of the times, as there is often poorly functioning renal parenchyma with or without pyonephrosis. Laparoscopic approach can be used in selected cases but conversion rate to open is higher. Diagnosis is usually made in histopathological examination [1,5].
4 Conclusion
Xanthogranulomatous pyelonephritis is very rare cause of giant hydronephrosis with a varying clinical and radiological presentation and difficult to diagnose preoperatively.
Diagnosis of XGP should be entertained in case long-standing gross hydronephrotic obstructed, infected kidney with stone disease.
Availability of data and materials
Data sharing is not available to this article as no dataset were generated during the study.
Abbreviations
- XGP:
-
Xanthogranulomatous pyelonephritis
- CECT:
-
Contrast-enhanced computerized tomography
- PUJO:
-
Pelvi-ureteric junction obstruction
References
Herrera-Bedoya M, Avendaño-Capriles CA, Zakzuk-Martinez E, Barrera J (2021) Xanthogranulomatous pyelonephritis and its differential diagnoses: an in-depth case review. Cureus 13:e19133
Yazırlıoğlu R (2017) Giant size xanthogranulomatous pyelonephritis: a case report. J Urol Surg 4:215–217
Hassen SM, Issack FH, Mummed FO, Hassen IK (2021) Giant hydronephrosis secondary to ureteropelvic junction obstruction, a rare occurrence, case report. Urol Case Rep 10(39):101803
Dino, Masresha & Hassen, Seid & Tufa, Tesfaye. Unilateral Giant Hydronephrosis Secondary to Ureteropelvic Junction Obstruction in a Middle-Aged Woman. Case Rep Urol. 2021; 9900560.
Artiles-Medina A, Laso-García I, Lorca-Álvaro J et al (2021) Xanthogranulomatous pyelonephritis: a focus on microbiological and antibiotic resistance profiles. BMC Urol 21:1–7
Acknowledgements
We acknowledge the pathology department, GMC, Aurangabad, Maharashtra, India.
Funding
Nil.
Author information
Authors and Affiliations
Contributions
Both authors have made substantial contributions to the conception, design of the work, the acquisition, analysis, interpretation of data, drafted and substantively revised the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Patient consent taken.
Competing interests
No.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Dhakne, B., Gite, V.A. Xanthogranulomatous pyelonephritis presenting as giant hydronephrosis in young women: a very rare case report. Afr J Urol 30, 8 (2024). https://doi.org/10.1186/s12301-023-00406-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12301-023-00406-x