Abstract
Background
Vesicoureteral reflux (VUR) is a common condition associated with childhood urinary tract infection (UTI) that can lead to chronic renal failure and hypertension. Various anti-reflux treatments were advocated, with various degrees of morbidity and success. The purpose of this study is to analyze and compare the results of modified Gil-Vernet anti-reflux surgery and bulking agent injection in children with unilateral high-grade reflux.
Methods
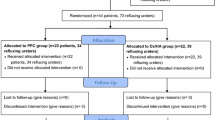
The study involved 179 patients who underwent surgical interventions for primary VUR from February 2013 to September 2019. Data on baseline demographics, preoperative symptoms, radiological imaging studies, and postoperative outcomes were analyzed. Treatment goal was defined as when no VUR or downgrading was detected 6 months or later after the intervention.
Results
A total of 128 patients underwent modified Gil-Vernet anti-reflux surgery and 51 patients underwent dextranomer/hyaluronic acid (Dx/HA) injection with mean VUR grading of 4.3 in both groups (P = 0.687). The overall VUR resolution rates were significantly higher in modified anti-reflux surgery rather than Dx/HA injection (86% vs. 68%, P = 0.021). Dx/HA injection was associated with shorter operation time (21 ± 8 min vs. 57 ± 11 min, P = 0.01), and shorter hospital stay (0.34 ± 0.22 days vs. 3.50 ± 0.50 days, P < 0.001). No major complications were identified in both groups.
Conclusions
Dx/HA injection has a significantly shorter operation time, lower postoperative analgesic usage, and shorter hospital stay, modified Gil-Vernet anti-reflux surgery is associated with significantly higher VUR downgrading and resolution rates than Dx/HA injection, particularly in the higher grade VUR.
Similar content being viewed by others
1 Background
Vesicoureteral reflux (VUR) is the most common congenital urologic disorder, characterized by abnormal flow of urine from the bladder to the ureter and renal pelvis through a malfunctioning vesicoureteral junction. According to studies, VUR ranges between 0.4 and 1.8% of the general pediatric population, and approximately 30% of children with urinary tract infections have VUR in further evaluations [1, 2]. In most cases, VUR does not cause any symptoms and is detected prenatally in children with hydronephrosis or postnatally following the development of symptomatic urinary tract infection (UTI) [3]. Furthermore, precise VUR prevalence is unavailable because cystography is not performed in healthy children due to ethical concerns [4].
In general, VUR can be either primary or secondary to defective vesicoureteral junction development, neurogenic bladder dysfunction, and high intravesical pressure and posterior urethral valves [5]. One or more episodes of urinary reflux can cause renal scarring, resulting in pyelonephritis and an increased risk of hypertension, decreased renal function, and impaired somatic growth [6]. Observation, antibiotic prophylaxis, endoscopic injection, and ureteral reimplantation are the four primary treatment choices for patients with VUR [7].
It has been known that VUR spontaneously resolves over time. However, observation and medical treatment, including behavioral modification and urotherapy with or without antibiotic therapy only deemed appropriate for patients with a low risk of renal injury (i.e., males with low-grade VUR) [8].
Endoscopic and surgical intervention may be beneficial in cases of medical treatment failure, recurrent UTI, persistent VUR, and the formation of new renal parenchymal scars, as well as in patients who do not comply with treatment and whose VUR is clinically less likely to resolve (as in patients with high-grade reflux, older age, and female gender) [9, 10].
Consequently, despite the high prevalence of VUR in children, there is no consensus on the optimal therapeutic approach. Better identification of children at risk of renal scarring, robust data regarding potential therapies, and an improved VUR grading system is required for continued treatment advancement.
In the present study, the success rate of both modified Gil-Vernet anti-reflux surgery and bulking agent injection groups are evaluated in a non-randomized group of unilateral high-grade VUR at two-year follow-up.
2 Methods
The document of all patients with unilateral high-grade VUR (grade four/ and five) from February 2013 to September 2019 who were referred to the Labbafinejad hospital, Tehran-Iran, and had been indicated for surgical intervention were included.
2.1 Inclusion and exclusion criteria
The criteria for surgical or endoscopic intervention were as follows: Impaired renal function, development of new parenchymal scars, breakthrough UTI despite antibiotic prophylaxis and poor compliance with conservative medical treatment by patients and/or parents, lack of sufficient cooperation.
Diagnosis of VUR was established by voiding cystourethrography, and severity of VUR was determined using the International Reflux Study classification [11]. This classification system is based on the appearance of the ureteral orifice during cystoscopy and classifies VUR into five grades ranging from grade one (mildest) to grade five (most severe). Grade one reflux involves reflux only into the distal ureter, while grade five reflux involves reflux with ureteral dilatation and tortuosity. Downgrading was defined as a reduction in the reflux grade, while achieving a state of complete absence of reflux was considered a cure.
The exclusion criteria were: history of previous failed open or endoscopic anti-reflux surgery at the affected side, secondary VUR, duplex system, single kidney, overt spinal dysraphism, evidence for a pop-off mechanism of a high-grade VUR, untreated overt bladder or bowel dysfunction (diagnosed based on the urodynamic study test), and bilateral VUR.
2.2 Procedures
The preoperative evaluation included urine analysis and culture, sonography of the kidneys, and urinary tract. Finally, the decision on the surgical approach or bulking agent injection was made by the parents.
In the modified Gil-Vernet group, a short Pfannenstiel skin incision was made. The bladder was opened in the midline, and 3 French (Fr) ureteral catheters were passed through both ureters; a horizontal mucosal incision was made in the trigone (between ureteral orifices), and medial sides of both ureters were dissected gently to mobilize enough both ureters. The medial wall of both ureters were sutured by two 5–0 Vicryl sutures and approximated to each other in the midline. The ureteral orifices were checked for proper efflux of urine; the incised trigonal mucosa was sutured longitudinally by separate 5–0 vicryl sutures. The bladder and wound were closed, suction drainage, and a Foley catheter was inserted (Fig. 1).
In the injection group, we have used dextranomer/hyaluronic acid (Dx/HA), (Deflux, Q-Med Scandinavia, Uppsala, Sweden) bulking agent, all injections were administered with an 8–10 Fr pediatric rigid cystourethroscope under general anesthesia. The bulking agent was injected through a 3.7-Fr flexible catheter inserted into the ureteral lumen with the intraureteral hydrodistention technique at 6 o’clock (The injection was carried out until the shape of the ureteral orifice changed to a slit-like mound.). Then, the efflux of urine through the ureter was checked [12]. Both procedures were performed by the same surgeon (F.S).
Patients were evaluated after treatment for early and delayed (more than one month) complications such as lower urinary tract symptoms (LUTS), unexplained fever, UTI, and hydronephrosis, which were considered indications for patient reevaluation.
The response to both procedures was monitored and recorded 18 months following surgery by direct radionuclide cystography (DRNC). Ultrasound scan was repeated at one day, first week, one month, 6- and 12-month postoperation and repeated each year as routine.
Parents were fully informed about both approaches, advantages, and disadvantages, and written informed consent was signed by the parents.
The ethical committee of the Urology and Nephrology Research Center of Shahid Beheshti University of Medical Sciences approved the protocol of study with an ethical code as IR.SBMU.UNRC.REC.1397.15.
2.3 Statistical analysis
The statistical analysis was performed with SPSS statistics version 26.0 (SPSS Inc., IBM Company, Chicago, IL, USA). Ordinal variables were compared using independent t-test and Mann–Whitney U-test. Categorical nominal variables were compared with Fisher’s exact test and Chi-square test as appropriate. A P-value of less than 0.05 was considered statistically significant.
3 Results
In this study, the outcomes of 179 eligible children (179 renal refluxing units) with mean age 3.69 ± 1.0 years old (ranged from 1 to 7 years) after modified Gil-Vernet anti-reflux surgery and Dx/HA injection were evaluated and compared. Among the patients, 120 (67.5%) had reflux grade 4, while 59 patients had reflux grade 5. Table 1 shows the demographics and pre- and postoperative findings of the patients.
In the Gil-Vernet group and the Dx/HA injection group, the VUR resolution rate was 86% and 68%, respectively (P = 0.021). The duration of surgery was (57 ± 11 vs. 21 ± 8 min, P ≤ 0.001) for the modified Gil-Vernet and endoscopic injection, respectively, and the duration of hospitalization in patients with modified Gil-Vernet and the Dx/HA injection group was (3.50 ± 0.50 vs. 0.34 ± 0.22 days, P = 0.01) (Table 2).
Dysuria was reported by 73 (57%) patients in the modified Gil-Vernet group and 16 (31%) patients in the Dx/HA injection group, and hematuria was founded in 57 (47%) patients in the modified Gil-Vernet group and 11 (22%) patients in the Dx/HA injection group, both of which were statistically significant (P = 0.011 & P = 0.014, respectively) (Table 1). However, all bothersome symptoms resolved gradually with or without medication three weeks after the operation.
Within 18 months of treatment, all patients underwent DRNC to assess the success rate. In the modified Gil-Vernet group, 112/128 (86%) patients were completely cured, while in the Dx/HA injection group, 35/51 (68%) patients were completely cured. VUR had been downgraded in other patients in these groups. A subgroup analysis was carried out according to the grade of VUR (Table 2).
Among patients with grade 4 VUR, there was a complete response to modified Gil-Vernet in 76 out of 87 (87.3%), while the rate was 70% in the Dx/HA group (shown in Figs. 2 and 3). In addition, there was a downgrading of VUR (partial response) in 12.7% (11/87) and 30% (10/33) of the modified Gil-Vernet and injection groups, respectively (Table 2).
Among the patients with reflux grade 5, 88% (36/41) in the modified Gil-Vernet group and 67% (12/18) in the Dx/HA injection group showed complete resolution, while the rest had reduced grade findings (Table 2, shown in Figs. 4 and 5).
3.1 Follow-up
After two-year follow-up, five patients in Dx/HA group required re-treatment by reinjection, with four of them fully treated and one with downgrading severity. None of the patients required open surgical treatment such as ureteral reimplantation. In modified Gil-Vernet group, three patients who required re-treatment received a bulking agent injection, with two patients being completely cured and one with downgrading severity.
4 Discussion
VUR is a common urological problem in children. As the child grows and the submucosal ureter lengthens, most cases resolve spontaneously, so conservative treatment is recommended in the lower grades of VUR, with surgical treatment reserved for failure of conservative treatments [8]. Higher grades of reflux, on the contrary, have a lower chance of spontaneous healing, and patients are likely to develop more complications at an early age [9, 13]. For higher grades of VUR, most physicians prefer surgical intervention, which includes open or laparoscopic surgery, as well as endoscopic treatment.
It is important to note that there are no universally agreed upon gold standards for the treatment of VUR. Various surgical approaches, such as ureteral reimplantation and the endoscopic method, are recommended as surgical treatments of choice, with varying degrees of success and morbidity. However, because of the disparity in research findings in different grades, there is a general agreement for higher grades of VUR to be treated invasively by surgical approaches or endoscopic injection of bulking agents.
According to the safety and effectiveness of O’Donnel’s biocompatible injection methods, endoscopic treatment of VUR has gained popularity since its first report in 1981 by Matouschek, and a large number of interventions related to VUR are now performed through endoscopic injection each year [14, 15].
Following modified Gil-Vernet surgery, common complications include dysuria, pyuria, hematuria, flank pain, and a febrile UTI [16]. However, only dysuria and hematuria were found to be significantly higher in the modified Gil-Vernet group than in the Dx/HA injection group in our study. There was no major complication according to Clavien-Dindo classification of surgical complications in either group, implying that both procedures are safe to perform. Although Dx/HA treatment was linked to less postoperative pain and a shorter hospital stay, success rates were lower, particularly in higher-grade VUR.
Chertin et al. [17] reported 68–92% success for endoscopic bulking agents depending on VUR grade. Furthermore, according to a recent meta-analysis, the resolution rate of mild-to-severe VUR following treatment with Dx/HA was 76% [18]. Harper et al. [19] recently reported an 85% success rate in children with mild-to-moderate VUR who underwent endoscopic injection of Dx/HA with a follow-up period of more than 10 years. In a study by Friedmacher et al. in 2018, 851 children with grades 4 and 5 VUR, including 415 children with unilateral VUR underwent endoscopic injection of Dx/HA. After the first injection, 70.4% of patients with VUR grade 4 and 61.9% of patients with VUR grade 5 were treated and reported an overall success rate of 69.5% [20]. Leung et al. recently differentiated the resolution rate of VUR following Dx/HA injection according to the grade of the affected ureter at 60-month follow-up, which was 63% grade 3, 40% grade 4, and 70% grade 5 [21]. In a study conducted by Qahtani on children with high-grade VUR, the endoscopy group had a success rate of 58%, and 17% of the cases were downgraded to low-grade VUR [22].
Moradi et al. conducted a study in 2018, in which 183 patients with 290 renal refluxing units of high-grade VUR underwent Gil-Vernet anti-reflux surgery, which reported a 95% cure rate and 5% downgrade of reflux in a long time follow-up [23]. In a study conducted by Mirshmirani et al. In 2010, 72 patients with 104 renal refluxing units underwent Gil-Vernet anti-reflux surgery, with results showing a 96% complete cure and 4% downgrading of reflux [24]. Also, in a study by Irani et al., 30 patients with 46 renal refluxing units with mild-to-severe VUR underwent Gil-Vernet surgery and were followed up for an average of 18 months, with 95.6% complete recovery and 4.4% reduction in grade [25].
If treatment success is measured by downgrading VUR, the success rate is significantly higher in the modified Gil-Vernet group than in Dx/HA injection (86% vs. 68%, P = 0.021). Subgroup analyses across the different VUR grades also revealed that in grade 4 and grade 5 VUR, the modified Gil-Vernet group had significantly higher downgrading and resolution rates than the Dx/HA injection group.
There are limitations to the current study that should be addressed: First, it has the usual limitations of a retrospective study compared to a prospective study design. Second, the biodegradable nature of bulking agents may result in recurrences after longer follow-up periods, therefore studies with longer follow-up times and larger sample size are recommended. Third, in the current study, the incidence of reflux in the counterside ureter has not been evaluated. The last one is the cultural and economic bias in favor of surgery among parents in our country.
Both surgical approaches of modified Gil-Vernet anti-reflux surgery and endoscopic injection of Dx/HA both of which are safe and effective in the treatment of unilateral high-grade VUR. While Dx/HA injection has a significantly shorter operation time, lower postoperative analgesic usage, and shorter hospital stay, Gil-Vernet anti-reflux surgery is associated with significantly higher VUR downgrading and resolution rates than Dx/HA injection at two-year follow-up.
Availability of data and materials
All data generated or analyzed during this study are included in this article. Further enquiries can be directed to the corresponding author.
Abbreviations
- DRNC:
-
Direct radionuclide cystography
- Dx/HA:
-
Dextranomer/hyaluronic acid
- UTI:
-
Urinary tract infection
- VUR:
-
Vesicoureteral reflux
References
Hoberman A, Charron M, Hickey RW, Baskin M, Kearney DH, Wald ER (2003) Imaging studies after a first febrile urinary tract infection in young children. N Engl J Med 348(3):195–202. https://doi.org/10.1056/NEJMoa021698
Capozza N, Gulìa C, Heidari Bateni Z, Zangari A, Gigli S, Briganti V et al (2017) Vesicoureteral reflux in infants: what do we know about the gender prevalence by age? Eur Rev Med Pharmacol Sci 21(23):5321–5329
Blais AS, Bolduc S, Moore K (2017) Vesicoureteral reflux: from prophylaxis to surgery. Can Urol Assoc J 11(1-2Suppl):S13-s8. https://doi.org/10.5489/cuaj.4342
Lee LC, Lorenzo AJ, Koyle MA (2016) The role of voiding cystourethrography in the investigation of children with urinary tract infections. Can Urol Assoc J 10(5–6):210–214. https://doi.org/10.5489/cuaj.3610
Sillén U (2008) Bladder dysfunction and vesicoureteral reflux. Adv Urol 2008:815472. https://doi.org/10.1155/2008/815472
Hoberman A, Greenfield SP, Mattoo TK, Keren R, Mathews R, Pohl HG et al (2014) Antimicrobial prophylaxis for children with vesicoureteral reflux. N Engl J Med 370(25):2367–2376. https://doi.org/10.1056/NEJMoa1401811
Kirsch AJ, Arlen AM (2020) Evolving surgical management of pediatric vesicoureteral reflux: is open ureteral reimplantation still the ‘Gold Standard’? Int Braz J Urol 46(3):314–321. https://doi.org/10.1590/s1677-5538.Ibju.2020.99.05
Park Y (2012) Renal scar formation after urinary tract infection in children. Korean J Pediatr 55:367–370. https://doi.org/10.3345/kjp.2012.55.10.367
Estrada CR Jr, Passerotti CC, Graham DA, Peters CA, Bauer SB, Diamond DA et al (2009) Nomograms for predicting annual resolution rate of primary vesicoureteral reflux: results from 2462 children. J Urol 182(4):1535–1541. https://doi.org/10.1016/j.juro.2009.06.053
Dothan D, Kocherov S, Jaber J, Chertin B (2021) Endoscopic correction of reflux utilizing polyacrylate polyalcohol bulking copolymer (vantris) as a tissue augmenting substance: lessons learned over the 10 years of experience. J Laparoendosc Adv Surg Tech A 31(9):1073–1078. https://doi.org/10.1089/lap.2021.0089
Lebowitz RL, Olbing H, Parkkulainen KV, Smellie JM, Tamminen-Möbius TE (1985) International system of radiographic grading of vesicoureteric reflux. International reflux study in children. Pediatr Radiol 15(2):105–109. https://doi.org/10.1007/bf02388714
Cerwinka WH, Scherz HC, Kirsch AJ (2008) Endoscopic treatment of vesicoureteral reflux with dextranomer/hyaluronic acid in children. Adv Urol 2008:513854. https://doi.org/10.1155/2008/513854
Mattoo TK, Chesney RW, Greenfield SP, Hoberman A, Keren R, Mathews R et al (2016) Renal scarring in the randomized intervention for children with vesicoureteral reflux (RIVUR) trial. Clin J Am Soc Nephrol 11(1):54–61. https://doi.org/10.2215/cjn.05210515
Schwab CW Jr, Wu HY, Selman H, Smith GH, Snyder HM 3rd, Canning DA (2002) Spontaneous resolution of vesicoureteral reflux: a 15-year perspective. J Urol 168(6):2594–2599. https://doi.org/10.1097/01.ju.0000037530.11361.8b
O’Donnell B, Puri P (1984) Treatment of vesicoureteric reflux by endoscopic injection of Teflon. Br Med J (Clin Res Ed) 289(6436):7–9. https://doi.org/10.1136/bmj.289.6436.7
Wein JA, KLR, Patrin AW, Peters CA (2016) Campbell-Walsh Urology. Chapter 137. 11 ed
Chertin B, Kocherov S, Chertin L, Natsheh A, Farkas A, Shenfeld OZ et al (2011) Endoscopic bulking materials for the treatment of vesicoureteral reflux: a review of our 20 years of experience and review of the literature. Adv Urol 2011:309626. https://doi.org/10.1155/2011/309626
Gholami B, Gholami S, Khodaei B, Sharifiaghdas F (2022) Comparison of polyacrylate polyalcohol copolymer (PPC) and dextranomer/hyaluronic acid (Dx/HA) for treatment of vesicoureteral reflux. A systematic review and meta-analysis. J Pediatr Urol 18(5):664–673. https://doi.org/10.1016/j.jpurol.2022.08.012
Harper L, Paillet P, Minvielle T, Dobremez E, Lefevre Y, Bouali O et al (2018) Long-term (>10 years) results after endoscopic injection therapy for vesicoureteral reflux. J Laparoendosc Adv Surg Tech A 28(11):1408–1411. https://doi.org/10.1089/lap.2018.0035
Friedmacher F, Puri P (2019) Ureteral obstruction after endoscopic treatment of vesicoureteral reflux: does the type of injected bulking agent matter? Curr Urol Rep 20(9):49. https://doi.org/10.1007/s11934-019-0913-5
Leung L, Chan IHY, Chung PHY, Lan LCL, Tam PKH, Wong KKY (2017) Endoscopic injection for primary vesicoureteric reflux: predictors of resolution and long term efficacy. J Pediatr Surg 52(12):2066–2069
Al Qahtani W, Sarhan O, Al Otay A, El Helaly A, Al KF (2020) Primary bilateral high-grade vesicoureteral reflux in children: management perspective. Cureus 12(12):e12266. https://doi.org/10.7759/cureus.12266
Moradi M, Seyedzadeh A, Gharakhloo S, Teymourinezhad A, Kaseb K, Rezaee H (2018) The modified Gil-Vernet antireflux surgery: a successful technique for high-grade vesicoureteral reflux correction in children-long-term follow-up. Adv Urol 2018:4948165. https://doi.org/10.1155/2018/4948165
Mirshemirani A, Khaleghnejad Tabari A, Roshanzamir F, Shayeghi S (2010) Gil-Vernet antireflux surgery in children’s primary vesicoureteral reflux. Pediatr Surg Int 26(10):981–984. https://doi.org/10.1007/s00383-010-2651-0
Irani D, Heidari M (2004) Results of modified Gil-Vernet antireflux surgery in the treatment of vesicoureteral reflux. Urol J 1(2):107–10
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
FS and BN helped in project development, supervision, and review and editing manuscript. BN, MHS, and MBH helped in supervision, review and editing manuscript, and data collection and management. AJ and MAE contributed to writing and editing original draft and data collection and management. HR, MAE, AJ and MA contribute to writing and editing original draft, analysis and interpretation of data, and data collection and management. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All procedures involving human participants in the study were approved by the ethical committee of the Urology and Nephrology Research Center of Shahid Beheshti University of Medical Sciences with an ethical code as IR.SBMU.UNRC.REC.1397.15.
Consent for publication
Written informed consent was signed by all children’s parents or legal guardians.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Sharifiaghdas, F., Narouie, B., Soltani, M.H. et al. Investigating the clinical outcomes of bulking agent injection in comparison with modified Gil-Vernet anti-vesicoureteral reflux surgery in children with high-grade reflux (4 or 5). Afr J Urol 29, 67 (2023). https://doi.org/10.1186/s12301-023-00403-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12301-023-00403-0