Abstract
Mesothelioma is a rare cancer that generally affects the lining of the lungs. However, in more rare cases, there are extra-pleural involvement of organs that are lined with mesothelial cells, including the testicle. Mesothelioma of the tunica vaginalis of the testicle typically presents with a painless scrotal mass with accompanying hydrocele of the affected side. The most common predisposition to mesothelioma of the tunica vaginalis is previous asbestos exposure, long-standing hydrocele, and previous scrotal surgeries. In this case we present a patient with isolated left tunica vaginalis mesothelioma of the testicle, yet without classic risk factors or other sites of disease. Left radical orchiectomy was performed and subsequent follow-up imaging did not reveal any sites of recurrence or metastasis. Although, mesothelioma of the tunica vaginalis is a rare cancer, it should be seen as a possible differential when evaluating new testicular masses.
Similar content being viewed by others
1 Background
Mesotheliomas are rare tumors that generally arise after exposure to asbestos and often present in the pleura or peritoneum. However, more rarely, mesotheliomas can occur in extra-pleural tissue that is lined by mesothelial cells, such as the peritoneum and the tunica vaginalis. Mesotheliomas arising from the tunica vaginalis are rare with less than 300 documented cases and comprising less than 5% of all mesothelioma tumors [1]. Asbestos exposure is a primary risk factor for the development of mesothelioma of the tunica vaginalis, though inflammatory causes such as trauma and long-standing hydrocele are also risk factors [1, 2]. These tumors most commonly arise in middle-aged men with a mean age of 53.5 years. The clinical presentation is typically of insidious onset with unilateral painless enlargement of the scrotum with accompanying hydrocele. An important ultrasonic finding is thickening of the tunica vaginalis [3]. The overall survival in patients with mesothelioma of the tunica vaginalis is 1.5 years with a 5 year overall survival of 49% [4]. In this case report we describe a case of malignant mesothelioma without the common presentation or associated risk factors.
2 Case report
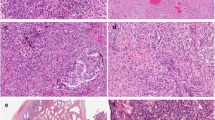
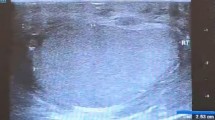
A 60-year-old male presented to a urology clinic with a left scrotal lump that had been present for “several years” but was painless and stable in size. A scrotal ultrasound was ordered and displayed a 1.5 × 1.0 cm solid mass arising from the left epididymis (Fig. 1). Serum tumor markers, alpha fetoprotein (AFP), lactate dehydrogenase (LDH), and beta human chorionic gonadotropin (β-HCG), were ordered, and all of which were negative. A left radical orchiectomy was then performed. The patient’s pathology from the radical left orchiectomy revealed malignant mesothelioma of the tunica vaginalis (Fig. 2). The tumor was measured at 3.0cm in size and all margins were negative. The patient was then sent for a computed tomography (CT) of the chest, abdomen and pelvis. The CT scan did not reveal any local adenopathy or evidence of metastatic disease. He had a repeat CT scan at 1 and 2 years postoperatively, and is currently on a surveillance protocol without any recurrence of disease after 2 years.
Histological evaluation of the patient’s scrotal mass. A Hematoxylin–eosin-stained revealing tumor infiltrating soft tissue, 50x. B Hematoxylin–eosin-stained showing fibrosis and tubular proliferation with normal spermatogenesis occurring, 100x. C Hematoxylin–eosin-stained demonstrating tubular and papillary mesothelial proliferation, 50x. D Immunohistochemical staining for Calretinin positive, 200x. E Immunohistochemical staining for D2-40 positive, 200x. F Immunohistochemical staining for CK5/6 positive, 200x
3 Discussion
Mesotheliomas stem from mesothelial cells which make up the lining of the pericardium, pleura, lungs, and testicles. Mostly commonly, mesotheliomas arise from exposure to asbestos. Asbestos induces DNA damage via creation of radical oxygen and nitrogen species, and iron free radicals. These in turn can cause DNA substitutions, deletions, and insertions. In addition to the creation of DNA damage, asbestos exposed mesothelial cells continually proliferate via the NF-kB pathway [5].
In addition to asbestos exposure, chronic inflammation can induce mesothelial cells to undergo oncogenic transformation. Cases of pleural mesothelioma have been documented without asbestos exposure but were subject to recurrent lung infections, pulmonary tuberculosis, and recurrent pleural effusions. For testicular mesotheliomas, it is posited that long-standing hydroceles and persistent inflammation in the tunica vaginalis predispose individuals to mesothelioma [6].
When approaching a scrotal mass, a thorough history and physical exam is required. It is important to inquire about a family history of testicular cancer, previous inguinal hernia repair, cryptorchidism, and previous orchiopexy. When physical exam confirms a solid mass, trans-scrotal ultrasound is the primary imaging technique to further investigate the solid mass. Seminomas are the most common testicular carcinoma in men older than 35 and it is imperative to retrieve serum tumor markers, including αFP, LDH, and β-HCG [6,7,8]. In contrast to testicular masses, solid epididymal masses, however, are typically benign. The incidence of malignancy is correlated with epididymal mass size greater than 1.5 cm and is generally regarded as the cutoff for intervention [9].
Mesothelioma of the tunica vaginalis is a rare form of an already uncommon cancer. The majority of reported cases have been found incidentally during hydrocelectomies [10]. The presentation in this case report was atypical. Commonly patients present with risk factors for mesothelioma of the tunica vaginalis. Our patient presented with a long-standing painless testicular mass, lack of primary asbestos exposure and lack of a concomitant long-standing hydrocele. Moreover, he had no other sites of mesothelioma, indicating a primary mesothelioma of the tunica vaginalis of the testicle.
In conclusion, mesothelioma of the tunica vaginalis is a rare form of an already rare cancer. Despite having notable risk factors and found in conjunction with long-standing hydrocele it should be kept on the differential diagnosis when evaluating a middle-aged male presenting with a testicular mass.
Availability of data and materials
Not applicable.
Abbreviations
- β-HCG:
-
Beta human chorionic gonadotropin
- LDH:
-
Lactate dehydrogenase
- AFP:
-
Alpha fetoprotein
- PSA:
-
Prostate specific antigen
References
Goel A, Agrawal A, Gupta R, Hari S, Dey AB (2008) Malignant mesothelioma of the tunica vaginalis of the testis without exposure to asbestos. Cases J 1(1):310. https://doi.org/10.1186/1757-1626-1-310.PMID:19014568;PMCID:PMC2596792
Akin Y, Bassorgun I, Basara I, Yucel S (2015) Malignant mesothelioma of tunica vaginalis: an extremely rare case presenting without risk factors. Singapore Med J 56(3):e53–e55. https://doi.org/10.11622/smedj.2015053.PMID:25820862;PMCID:PMC4371211
Chekol SS, Sun C-C (2012) Malignant mesothelioma of the tunica vaginalis testis: diagnostic studies and differential diagnosis. Arch Pathol Lab Med 136(1):113–117
Nazemi A, Nassiri N, Pearce S, Daneshmand S (2019) Testicular mesothelioma: an analysis of epidemiology, patient outcomes, and prognostic factors. Urology 126:140–144. https://doi.org/10.1016/j.urology.2019.01.009. (Epub 2019 Jan 19 PMID: 30668959)
Yang H, Testa JR, Carbone M (2008) Mesothelioma epidemiology, carcinogenesis, and pathogenesis. Curr Treat Options Oncol 9(2–3):147–157. https://doi.org/10.1007/s11864-008-0067-z
Yen CH, Lee CT, Su CJ et al (2012) Malignant mesothelioma of the tunica vaginalis testis: a malignancy associated with recurrent epididymitis? World J Surg Onc 10:238. https://doi.org/10.1186/1477-7819-10-238
Ghazarian AA, Rusner C, Trabert B, Braunlin M, McGlynn KA, Stang A (2018) Testicular cancer among US men aged 50 years and older. Cancer Epidemiol 55:68–72. https://doi.org/10.1016/j.canep.2018.05.007.PMID:29807233;PMCID:PMC6668029
Gaddam SJ. Testicle cancer [Internet]. StatPearls [Internet]. U.S. National Library of Medicine; 2021 [cited 2021Oct19]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK563159/
Alleman WG, Gorman B, King BF, Larson DR, Cheville JC, Nehra A (2008) Benign and malignant epididymal masses evaluated with scrotal sonography: clinical and pathologic review of 85 patients. J Ultrasound Med 27(8):1195–1202. https://doi.org/10.7863/jum.2008.27.8.1195. (PMID: 18645078)
Drevinskaite M, Patasius A, Kevlicius L, Mickys U, Smailyte G (2020) Malignant mesothelioma of the tunica vaginalis testis: a rare case and review of literature. BMC Cancer 20(1):1–6
Acknowledgements
Not applicable.
Funding
All the authors have no funding sources to declare relevant to this report.
Author information
Authors and Affiliations
Contributions
SR made significant contributions researching and writing this report. SN made significant contributions performing research for this article. NF was responsible for treatment plan and performance. NF also made a significant critical assessment of this article and edits for this report. All authors agree on the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent for publication of case report was obtained from the participant patient.
Competing interests
There was no funding for the study and no conflicts of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Reed, S.J., Nasui, S. & Farber, N. Atypical presentation of testicular mesothelioma. Afr J Urol 29, 70 (2023). https://doi.org/10.1186/s12301-023-00402-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12301-023-00402-1