Abstract
Background
Emphysematous pyelonephritis is a necrotizing infection of the renal parenchyma by gas-forming organisms. The diagnosis of emphysematous pyelonephritis is made by clinical features and the detection of air in the renal parenchyma. In the past, nephrectomy was considered the only treatment option with a high mortality rate, but with advances in minimally invasive conservative techniques and better antibiotic treatment, the rate of kidney salvage has increased.
Case presentation
From January 2019 to December 2022, eight cases of emphysematous pyelonephritis were diagnosed based on clinical features and documentation of gas in the renal parenchyma by a Computed tomography scan. The mean age was 61.75 ± 4.3 years. 62.5% were female and 75% were diabetics. E. coli was the most common pathogen (87.5%). All 8 patients underwent early interventions in the form of DJ stenting or percutaneous nephrostomy tube insertion with only one patient requiring nephrectomy without any immediate mortality.
Conclusion
Emphysematous pyelonephritis is more common in women and the elderly. Diabetes mellitus and nephrolithiasis are major risk factors. E. coli was the most frequently isolated pathogen. Early diagnosis and early minimally invasive intervention in the form of a DJ stenting or percutaneous nephrostomy reduced the rate of nephrectomy and mortality.
Similar content being viewed by others
1 Background
Emphysematous pyelonephritis (EPN) is an acute necrotizing infection of the renal parenchyma and peri-renal tissue resulting in the formation of gas within the renal parenchyma, collecting system, or perinephric tissue [1,2,3]. More than 90% of all cases of EPN occur in patients with diabetes mellitus (DM). Moreover, it is commonly seen in patients with obstructive uropathy, polycystic kidney disease, and end-stage renal disease. EPN is a life‐threatening infection with a mortality rate as high as 80% in earlier studies [4, 5]. Earlier the treatment of choice was nephrectomy to prevent life-threatening complications but in recent times with the development of advanced imaging techniques and minimally invasive interventions nephrectomy and mortality can be avoided. In this study, we have analyzed the characteristics of 8 patients with EPN concerning patient demographics, clinical presentation, investigations, diagnosis, microbiological findings, treatment modality, and outcome.
2 Case presentation
The study was carried out at Dhiraj Hospital, SBKS medical institute and research center, Vadodara. The study included 8 diagnosed cases of EPN admitted during the period from Janurary 2019 to December 2022. The diagnosis of EPN was done based on clinical features and documentation of gas within the renal parenchyma, collecting system, or perinephric tissue on computed tomography (CT) scan. The clinical, laboratory, radiological, and microbiological findings, treatment modality, and outcome of these patients were reviewed retrospectively.
A Total of 8 cases were diagnosed to have Emphysematous pyelonephritis. The mean age was 61.75 ± 4.3 years. 5 (62.5%) out of 8 were female, 6 (75%) were diabetic and 3 (37.5%) were having nephrolithiasis. Urine culture was positive in 7 (87.5%) patients. E. coli was the most common isolate seen in 6 (85.7%) patients out of 7 culture-positive samples. 4 (50%) patients had bilateral EPN, 3 (37.5%) had left EPN and 1 (12.5%) had right EPN. All patients were treated with intravenous antibiotics according to the culture sensitivities or with empirical antibiotics in culture negative cases. All patients were given appropriate supportive care. All patients underwent DJ stenting. 5 (62.5%) patients required only DJ stenting, 1 (12.5%) patient required DJ stenting with perinephric drainage of infected urinoma, 1 (12.5%) patient required DJ stenting plus percutaneous nephrostomy tube insertion and 1 (12.5%) patient required DJ stenting followed by nephrectomy. All patients improved at discharge and had improved renal function after 1 month of follow-up. DJ stent was removed after 1 month in all cases. There was no immediate mortality.
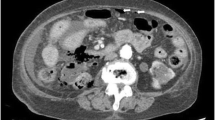
The CT images of a patient with Emphysematous pyelonephritis. A & B: Transverse section showing multiple air pockets within Right renal parenchyma with peri-nephric fat stranding. C & D: Coronal section showing multiple air pockets within Right renal parenchyma and a well-defined collection with air pockets extending from the right renal pelvis to the right iliac fossa suggestive of urinoma formation
The clinical details of each case are presented in Table 1. Table 2 contains information about the hematological & metabolic panel, urine analysis, culture report, interventions, and outcome of each of the patients in the study.
3 Discussion
EPN is a severe, necrotizing infection with gas in renal parenchyma and can be fatal if not diagnosed early and treated promptly. The conditions required for the development of EPN are based on three pillars: (1) the presence of pathogenic bacteria with the ability to do mixed acid fermentation, (2) hyperglycemia in tissue, and (3) impaired perfusion to the tissue [6]. These factors can work together, resulting in a rapid disease progression. It predominantly affects the female gender. Diabetics are more prone to emphysematous pyelonephritis. Patients with ureteric obstruction who are non-diabetic can also develop EPN but the severity of the disease is less as compared to diabetic patients.
The pathogenesis of EPN includes gas‐producing bacteria, high glucose concentration in the tissue, impaired tissue perfusion, and defective immune response which occurs in DM [7]. The high tissue glucose level acts as a substrate for the microorganisms such as E-coli and other Enterobacteriaceae. They produce hydrogen (H2) and carbon dioxide (CO2) by glucose fermentation. In a study by Huang et al., five of the six gas samples contained H2 and all the gas samples contained CO2 [8].
In our study, 5 out of 8 patients were female, and 75% of the patients were diabetic. 37.5% had nephrolithiasis as a risk factor.
The most common causative organism of EPN is E-coli. It is isolated in 47–90% of patients of EPN. The other commonly involved organisms include Proteus mirabilis, Klebsiella pneumoniae, Enterococcus species, and Pseudomonas aeruginosa [9, 10]. Supporting the literature, we also found that E. coli was isolated in 75% of our cases. Klebsiella pneumonia was also isolated in one of the patients. In our study, one patient was culture negative.
In EPN, the left kidney is more frequently involved than the right. A recent meta‐analysis has reported that 52% of patients had left‐sided, 37.7% right‐sided, and 10.2% bilateral EPN [9]. In our series, the left kidney was involved in 37.5% of patients. In our series, a much larger proportion of patients (50%) had bilateral EPN as compared to previous studies.
Traditionally, early nephrectomy was considered the treatment of choice in EPN with few reports suggesting increased mortality with medical therapy as compared to surgery, but surgery is often poorly tolerated in EPN due to the poor hemodynamic status of the patient. In 1996, Chen et al. reported that antibiotic therapy along with CT‐guided percutaneous drainage was an acceptable alternative to nephrectomy. In that study, most patients received medical therapy with percutaneous therapy and only two patients required nephrectomy. The treatment of EPN has evolved over the years from invasive surgery to more conservative approaches due to the availability of better imaging modalities, potent antibiotics, and image‐guided drainage.
A similar study done by Gite et al. showed that early intervention can help in salvaging the kidney and preventing mortality [11]. Also, another study by Jain et al. concluded that conservative management with an appropriate algorithm leads to reduced mortality and avoids unnecessary emergency nephrectomies [12].
Patients with EPN present with vague symptoms initially, but frequently undergo a sudden deterioration in their condition, requiring urgent medical intervention. Treatment of patients with EPN comprises resuscitation, correction of any electrolyte imbalance and hyperglycemia, and administration of antibiotics targeting Gram-negative bacteria. Ureteric obstruction is relieved by a percutaneous nephrostomy or stent. Definitive management is by percutaneous drainage or DJ stenting. Nephrectomy is advised when there is extensive diffuse gas with renal destruction not responding to conservative management.
4 Conclusions
According to our study, EPN is more common in women and the elderly. Diabetes mellitus and nephrolithiasis are major risk factors. E. coli was the most frequently isolated pathogen. A higher percentage of EPNs were bilateral in our study. All patients underwent interventions which included DJ stenting with or without peri-nephric drain insertion or percutaneous nephrostomy tube placement. Only one patient required a nephrectomy. All patients recovered without any mortality. Early diagnosis and minimally invasive intervention reduced the rates of nephrectomy and mortality.
Availability of data and materials
All the data regarding patients are available with us and can be provided with due request.
Abbreviations
- EPN:
-
Emphysematous pyelonephritis
- DM:
-
Diabetes mellitus
- CT:
-
Computed tomography
- DJ:
-
Double J
References
Shokeir AA, El-Azab M, Mohsen T, El-Diasty T (1997) Emphysematous pyelonephritis: a 15-year experience with 20 cases. Urology 49:343–346
Tang HJ, Li CM, Yen MY, Chen YS, Wann SR, Lin HH et al (2001) Clinical characteristics of emphysematous pyelonephritis. J Microbiol Immunol Infect 34:125–130
Misgar RA, Mubarik I, Wani AI, Bashir MI, Ramzan M, Laway BA (2016) Emphysematous pyelonephritis: A 10-year experience with 26 cases. Indian J Endocrinol Metab 20(4):475–480. https://doi.org/10.4103/2230-8210.183475. PMID: 27366713; PMCID: PMC4911836.
Smitherman KO, Peacock JE Jr (1995) Infectious emergencies in patients with diabetes mellitus. Med Clin North Am 79(1):53–77. https://doi.org/10.1016/s0025-7125(16)30084-0. PMID: 7808095.
Schaeffer AJ (2002) Infections of the urinary tract. In: Walsh PC, Retik AB, Vaughan ED, Wein AJ, Campbell M (eds) Campbell’s Urology, 8th ed. Saunders, Philadelphia, PA, p 556–58
Vivek V, Panda A, Devasia A (2012) Emphysematous pyelonephritis in a renal transplant recipient—Is it possible to salvage the graft? Ann Transpl 17(3):138–141
Huang JJ, Chen KW, Ruaan MK (1991) Mixed acid fermentation of glucose as a mechanism of emphysematous urinary tract infection. J Urol 146:148–151
Huang JJ, Tseng CC (2000) Emphysematous pyelonephritis: clinicoradiological classification, management, prognosis, and pathogenesis. Arch Intern Med 160:797–805
Aboumarzouk OM, Hughes O, Narahari K, Coulthard R, Kynaston H, Chlosta P et al (2014) Emphysematous pyelonephritis: time for a management plan with an evidence-based approach. Arab J Urol 12:106–115
Lu YC, Chiang BJ, Pong YH, Huang KH, Hsueh PR, Huang CY et al (2014) Predictors of failure of conservative treatment among patients with emphysematous pyelonephritis. BMC Infect Dis 14:418
Gite VA, Shaw V, Agrawal M, Sankapal P, Maheshwari M (2021) Minimally invasive techniques as a first line approach in the management of emphysematous pyelonephritis—a single centre experience. J Postgrad Med 67(3):146–153. https://doi.org/10.4103/jpgm.JPGM_1315_20
Jain A, Manikandan R, Dorairajan LN, Sreenivasan SK, Bokka S (2019) Emphysematous pyelonephritis: Does a standard management algorithm and a prognostic scoring model optimize patient outcomes? Urol Ann 11(4):414–420. https://doi.org/10.4103/UA.UA_17_19
Acknowledgements
We acknowledge the support provided by our Department of Urology and Anesthesiology at SBKS Medical institute & Research centre, Pipariya, Vadodara.
Funding
Not applicaple.
Author information
Authors and Affiliations
Contributions
The authors confirm their contribution to the paper as follows: study conception and design: HJ: Conception, data collection, design of the work, analysis, interpretation of data, drafting and revising manuscript. VS: data collection, drafting and revising manuscript. MP: design of the work, analysis, interpretation of data. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
As this is a retrospective observational study Ethics committee approval was not taken. Consent of all the participants were taken.
Consent for publication
Consent was taken from all the participants.
Competing interests
The authors have no competing interests to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Joshi, H.K., Shah, V.R. & Parikh, M.D. Clinical profile and outcome of emphysematous pyelonephritis presenting to a tertiary care hospital. Afr J Urol 29, 51 (2023). https://doi.org/10.1186/s12301-023-00380-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12301-023-00380-4