Abstract
Objective
We aimed to determine factors responsible for chronic kidney disease (CKD) following nephrectomy for renal tumours.
Methods
A retrospective study was undertaken in patients underwent partial or radical nephrectomy due to kidney tumour between January 2015 and June 2020. Patients with eGFR above 60 ml/min/1.73m2 were included in the study. Demographic information, surgical features, eGFR values and some comorbidities of patients were recorded. The patients were evaluated for the development of CKD according to the CKD-EPI equation postoperatively.
Results
One hundred and sixty-six patients who underwent radical (n = 125) or partial (n = 41) nephrectomy were included to study. According to the logistic regression analysis, radical nephrectomy (adjusted OR 0.139 (95% CI 0.038–0.507), p = 0.003), age (adjusted OR 1.037 (95% CI 1.001–1.074), p = 0.045), preoperative proteinuria (adjusted OR 0.251 (95% CI 0.084–0.750) p = 0.013) and preoperative lower eGFR (adjusted OR 0.943 (95% CI 0.917–0.969) p < 0.001) were determined as independent predictor for development of CKD.
Conclusions
CKD is an important disease that causes morbidity and mortality. Age, type of surgery and preoperative eGFR and preoperative proteinuria are an independent risk factor for CKD development. Patients should be informed about this problem before surgery.
Similar content being viewed by others
1 Background
Renal cell carcinoma (RCC) is one of the most fatal diseases in urology. It constitutes 3% of adult cancers and is the third most common urological malignancy [1]. The incidence of RCC has increased in last 3 decades with the widespread availability of imaging modalities such as ultrasound and computerised tomography [2]. Approximately 150.000 new cases are diagnosed each year, and patients are predominantly over the age of 60 [3].
Stage of the disease, tumour size and comorbidities are the most important factors affecting the choice of treatment. The definitive treatment of non-metastatic RCC is radical nephrectomy (RN) or partial nephrectomy (PN). Functional results such as residual renal functions are also very important after treatment, apart from oncological outcomes.
Chronic kidney disease (CKD) is defined as abnormalities of kidney structure or function, present for > 3 months, with implications for health according to current guidelines, and it was classified based on GFR category. CKD situation is accepted as normal when eGFR value ≥ 90 ml/min/1.73 m2. Stage 2 means eGFR value between 60 and 89, Stage 3 is 30 and 59 and Stage 4 indicates 15 and 29. Patients with < 15 ml/min/1.73 m2 eGFR are accepted end-stage kidney disease [4]. CKD has a high global prevalence about 11–13%, and stage 3 is seen predominantly. The first impaired stage of the estimated glomerular filtration rate (eGFR) is defined as less than 90 ml/min/1.73 m2 [5].
Kidney cancers patients generally have elderly profile and comorbidities. In addition to these, if the other kidney is not well preserved till that moment, extra morbidity and mortality may occur with development of postoperative CKD [6]. Nephrons decrease with nephrectomy procedure, and it leads a decline at eGFR values. eGFR < 60 is associated with increased cardiovascular events, death and hospitalisation [5, 7]. Furthermore, CKD has major complications such as anaemia, hypertension, malnutrition and neuropathy [8]. Therefore, residual kidney functions after RCC treatment are considerable problem. We aimed to evaluate predictive factors of CKD in patients who underwent surgery for RCC.
2 Methods
We retrospectively examined the patients who underwent RN and PN between January 2015 and June 2020. This study protocol was approved by local ethics committee and carried out in accordance with the Declaration of Helsinki. The centre is one of the well-known high-volume hospitals for oncological surgeries. All operations performed only one expert surgeon (AO from authors).
Demographic data, type of surgery, eGFR values and comorbidities such as hypertension and diabetes mellitus were recorded. Patients with preoperative eGFR value of above 60 ml/min/1.73m2 were included in the study. Patients with unknown eGFR value preoperatively or postoperatively and patients with a history of dialysis were excluded to prevent confounding eGFR data.
Preoperative proteinuria was assessed according to urinalysis. At least two urinalyses of the patients from the preoperative period were evaluated. Negative and trace values were accepted as no proteinuria. Cases with 2+ ,3+ and 4+ recorded as there is proteinuria.
Some equations based on serum creatinine were developed to calculate eGFR value. Other methods have been abandoned recently, and the CKD-EPI equation is frequently used in current guidelines. Therefore, we used Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation. Patients were evaluated at postoperative end of first year, and CKD patients were determined according to abnormal GFR values. CKD was defined as eGFR of less than 60 ml/min/1.73 m2 (Stage 3) in the present study. The Kidney Disease Improving Global Outcomes (KDIGO) classification was used for CKD staging [4]. The patients were divided into two groups according to postoperative eGFR as eGFR ≥ 60 and eGFR < 60.
The data were analysed with the Statistical Package for Social Sciences (SPSS) version 22.0™ (IBM Corporation, Los Angeles, CA, USA). The Chi-square and Student t tests were used for comparative analyses between groups. Multivariate logistic regression analysis was performed to explore parameters associated with postoperative CKD. All p values were two-tailed, and a p value of < 0.05 was noted statistically significant.
3 Results
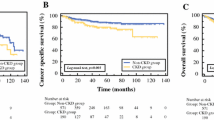
A total of 166 RCC patients underwent surgery were included in the study. Patient characteristics according to the CKD development are presented in Table 1. CKD developed in 68 patients (eGFR < 60) and eGFR was above 60 in 98 patients. Among these, 41 patients underwent PN, and 125 patients underwent RN. Our CKD rates were 4/41 (9.7%) in PN and 64/125 (51.2%) in RN according to the type of surgery. CKD rate was statistically significantly lower in patients with PN (p = 0.001). The mean age of CKD group was 65.4 ± 12.3, and non-CKD was 55.2 ± 11.7 (p < 0.001). Male/female rates were 48/20 in the CKD group and 59/39 in non-CKD group. There is no statistically significant difference between the groups according to gender (p = 0.169).
The mean preoperative eGFR value was 71.3 ± 14.9 ml/min/1.73m2 in CKD group and 91 ± 17.9 ml/min/1.73m2 in non-CKD group. Preoperative eGFR value was statistically significantly lower in CKD group (p < 0.001). The mean tumour size was 6.9 ± 3 cm and 5.2 ± 3.1, respectively, in CKD and non-CKD group and statistically significantly lower in non-CKD group (p = 0.001). There was no significant difference with respect to diabetes mellitus and hypertension between groups (p = 0.558, p = 0.133, respectively).
Multivariate logistic regression analysis for predicting CKD is presented in Table 2. In the logistic regression analysis, type of surgery (RN), age, preoperative proteinuria and preoperative lower eGFR were found independent predictor for development of CKD. On the other hand, according to regression analysis, gender, diabetes, hypertension, BMI were not found a predictor for CKD development. In particular, although tumour size differed statistically between groups in Table 1, regression analysis showed that it was not an independent predictor of CKD development.
4 Discussion
According to current urological guidelines, the surgical treatment of non-metastatic resectable renal tumour is either radical or partial nephrectomy. Cardiovascular problems, hospitalization and death have been related to the development of CKD [8]. Therefore, it is important to analyse risk factors responsible for CKD following nephrectomy.
Surgical treatment is the most effective curative option in suitable patients with RCC. Some adaptation mechanisms occur such as hyperfiltration and hypertrophy after unilateral radical nephrectomy. Nevertheless, renal failure may develop in some patients. Partial nephrectomy has replaced radical nephrectomy in the treatment of small renal masses due to similar oncological results [9, 10]. The main superiority of partial nephrectomy over radical nephrectomy is preservation of the renal function [11]. In our study, it was found that patients who underwent partial nephrectomy had lower CKD rates consistent with the literature [12]. And also, radical nephrectomy was found an independent risk factor for CKD development. Many studies demonstrate that partial nephrectomy reduces CKD rates, postoperative complications in comparison with radical nephrectomy [8, 12]. It should be considered that the type of surgery affects the probability of CKD independently of other factors and the preservation of a maximum renal reserve should be pursued. In addition, recent studies show that partial nephrectomy is superior to radical nephrectomy in terms of kidney function [13].
Proteinuria may be also one of the indicators of renal dysfunction. A recent study showed that proteinuria is a risk factor for acute kidney injury even after non-urological surgical [14]. Takagi et al. found there is no relationship proteinuria with postoperative poor renal function [15]. However, their study relatively had small number of patients. A larger recent study showed that worse preoperative proteinuria is related poor postoperative renal function [16]. They evaluated proteinuria in daily urine, unlike our spot urine evaluation. Similarly, our study showed that preoperative proteinuria is an independent risk factor for CKD development. Preoperative proteinuria may be related with lower eGFR although we did not evaluate, because both of them may be considered reflecting the poor renal function.
Tumour size is one of the important factors when deciding on the type of surgery. Current guidelines say that partial nephrectomy is a standard treatment in selected patients with 4 cm or less mass [17, 18]. There are conflicting studies in the literature that associate CKD development with tumour size. Lane et al. showed that tumour size predicts lower eGFR after surgery [19]. Conversely, Kong et al. demonstrated tumour size is not a clinical factor for CKD development [20]. We found statistically significant difference in tumour size between groups in the present study. However, tumour size was not an independent risk factor for CKD development. In fact, the main problem is not only tumour size, but also location. Resection of same size exophytic tumour and intraparenchymal tumour does not have the same degree of nephron damage when considering residual renal reserve. The heterogeneity in the data may be related to this.
Serum creatinine levels are used in many centres to determine kidney function. However, approximately 25% of patients with normal serum creatinine levels have at least moderate level CKD (eGFR < 60). Therefore, eGFR values reflect kidney function better [21, 22]. On the other hand, in a recent study, it was shown that renal functions are not stable for a while after kidney surgery and poor eGFR values in early time were recovered later on [23]. Therefore, we evaluated the eGFR values of the patients at the end of first year to stabilize acute changes on kidney function after surgery [24]. Kidney tissue does not have a regeneration property. Therefore, every negative effect on kidney shows a cumulation and adaptation mechanisms may not improve it all time. Although patients with preoperative eGFR > 60 included in the study, we showed that lower preoperative eGFR is a predictor for CKD in the present study. Similarly, other studies including partial and/or radical nephrectomy have also shown that lower preoperative eGFR is a predictor for CKD [19, 25]. According to recent interesting study, surgically induced kidney deficiency has lower progression and mortality rates than medical chronic kidney disease [26]. This may suggest that preoperative GFR, reflecting non-surgical kidney function, is important for postoperative kidney function. In order to reduce the effects other than surgery, we may recommend patients to consume adequate fluids and avoid nephrotoxic agents in the preoperative period.
The world is aging and expecting age is being over 60 years old by time [27]. Comorbidities are common with increasing age, and they are close relation. Most elderly oncological patients have at least one comorbidity requiring treatment [28]. Kidney cancer is seen in elderly patients and commonly associated with diabetes mellitus, hypertension and obesity [9]. According to transplantation data, CKD development is not common in donor patients with bilateral normal functioning kidneys after nephrectomy [29, 30]. It may be related to the fact that donor patients are generally younger and do not have comorbidities. We found older age to be an independent prognostic factor for CKD development in the present study. In parallel, there are studies in the literature showing that age is an important determinant for the development of CKD [20, 31]. We think that major reason is as age increases, nephron atrophy occurs and eGFR decreases.
There are conflicting studies regarding relationship between CKD development and diabetes mellitus, hypertension and BMI in the literature. Kong et al. reported that diabetes mellitus, BMI and hypertension are not important clinical factor in CKD patients [20]. On the other hand, Jeon et al. showed that diabetes mellitus is an independent prognostic factor for CKD development [25]. Reinstatler et al. found that BMI was related postoperative decline in kidney function unlike Wang et al.’s study [23, 32]. According to our study, BMI, diabetes mellitus and hypertension are not prognostic factors for CKD. Diabetes mellitus and hypertension effect on all body and have a scale in themselves. Uncontrolled or mild diseases may have different effects on the body. Data may show variability due to stage of comorbidities of included patients in the studies.
Repetitive surgical intervention may be needed due to recurrence of disease in herediter kidney tumours [33, 34]. Residual kidney function is very important problem in patients with solitary kidney, hereditary kidney tumour, bilateral or multifocal tumours. Therefore, partial nephrectomy should be forced in particularly these patients.
There are some limitations in our study. Firstly, we did not evaluate warm ischaemia time in partial nephrectomy cases. It may affect postoperative eGFR values. Secondarily, one of the factors of blocking homogenization in the study is excluding patients below eGFR 60 ml/min/1.73m2. Grouping the patients according to the type of surgery rather than the development of CKD would also give us valuable data. Retrospective design of study and relatively small number of patients are other limitations of the current study.
5 Conclusions
Preoperative renal functions, advanced age and type of surgery are most important factors affecting CKD development after surgery. Renoprotective preventions should be considered, and patients who have irreversible risk factors should be informed for possible CKD development-related surgery.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CKD:
-
Chronic kidney disease
- RCC:
-
Renal cell carcinoma
- RN:
-
Radical nephrectomy
- PN:
-
Partial nephrectomy
- eGFR:
-
Estimated glomerular filtration rate
- CKD-EPI:
-
Chronic Kidney Disease Epidemiology Collaboration
- KDIGO:
-
Kidney Disease Improving Global Outcomes
References
Siegel RL, Miller KD, Jemal A (2019) Cancer statistics, 2019. CA Cancer J Clin 69:7–34. https://doi.org/10.3322/caac.21551
Tyson MD, Humphreys MR, Parker AS, Thiel DD, Joseph RW, Andrews PE et al (2013) Age-period-cohort analysis of renal cell carcinoma in United States adults. Urology 82:43–47. https://doi.org/10.1016/j.urology.2013.02.065
Godley P, Kim SW (2002) Renal cell carcinoma. Curr Opin Oncol 14:280–285. https://doi.org/10.1097/00001622-200205000-00005
Levin A, Stevens PE, Bilous RW, Coresh J, De Francisco ALM, De Jong PE, Kidney disease: Improving global outcomes (KDIGO) CKD work group. KDIGO et al (2012) clinical practice guideline for the evaluation and management of chronic kidney disease. Kidney Int Suppl 2013:3. https://doi.org/10.1038/kisup.2012.73
Hill NR, Fatoba ST, Oke JL, Hirst JA, O’Callaghan CA, Lasserson DS et al (2016) Global prevalence of chronic kidney disease—a systematic review and meta-analysis. PLoS ONE 11:7e0158765. https://doi.org/10.1371/journal.pone.0158765
Leppert JT, Lamberts RW, Thomas IC, Chung BI, Sonn GA, Skinner EC et al (2018) Incident CKD after radical or partial nephrectomy. J Am Soc Nephrol 29:207–216. https://doi.org/10.1681/ASN.2017020136
Wang S, Liu Z, Zhang D, Xiang F, Zheng W (2022) The incidence and risk factors of chronic kidney disease after radical nephrectomy in patients with renal cell carcinoma. BMC Cancer. https://doi.org/10.1186/s12885-022-10245-8
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu C (2004) Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med. https://doi.org/10.1056/nejmoa041031
Sorbellini M, Kattan MW, Snyder ME, Hakimi AA, Sarasohn DM, Russo P (2006) Prognostic nomogram for renal ınsufficiency after radical or partial nephrectomy. J Urol. https://doi.org/10.1016/j.juro.2006.03.090
Lerner SE, Hawkins CA, Blute ML, Grabner A, Wollan PC, Eickholt JT et al (1996) Disease outcome in patients with low stage renal cell carcinoma treated with nephron sparing or radical surgery. J Urol. https://doi.org/10.1016/S0022-5347(01)66032-4
Ljungberg B, Bensalah K, Canfield S, Dabestani S, Hofmann F, Hora M et al (2015) EAU guidelines on renal cell carcinoma: 2014 update. Eur Urol 67:913–924. https://doi.org/10.1016/j.eururo.2015.01.005
Huang WC, Elkin EB, Levey AS, Jang TL, Russo P (2009) Partial nephrectomy versus radical nephrectomy in patients with small renal tumors—is there a difference in mortality and cardiovascular outcomes? J Urol. https://doi.org/10.1016/j.juro.2008.09.017
Scosyrev E, Messing EM, Sylvester R, Campbell S, Van Poppel H (2014) Renal function after nephron-sparing surgery versus radical nephrectomy: Results from EORTC randomized trial 30904. Eur Urol. https://doi.org/10.1016/j.eururo.2013.06.044
Wahl TS, Graham LA, Morris MS, Richman JS, Hollis RH, Jones CE et al (2018) Association between preoperative proteinuria and postoperative acute kidney injury and readmission. JAMA Surg. https://doi.org/10.1001/jamasurg.2018.2009
Takagi T, Kondo T, Iizuka J, Kobayashi H, Hashimoto Y, Nakazawa H et al (2011) Postoperative renal function after partial nephrectomy for renal cell carcinoma in patients with pre-existing chronic kidney disease: a comparison with radical nephrectomy. Int J Urol. https://doi.org/10.1111/j.1442-2042.2011.02765.x
Bhindi B, Lohse CM, Schulte PJ, Mason RJ, Cheville JC, Boorjian SA et al (2019) Predicting renal function outcomes after partial and radical nephrectomy (figure presented). Eur Urol. https://doi.org/10.1016/j.eururo.2018.11.021
McKiernan J, Simmons R, Katz J, Russo P (2002) Natural history of chronic renal insufficiency after partial and radical nephrectomy. Urology. https://doi.org/10.1016/S0090-4295(02)01501-7
Thompson RH, Boorjian SA, Lohse CM, Leibovich BC, Kwon ED, Cheville JC et al (2008) Radical nephrectomy for pT1a renal masses may be associated with decreased overall survival compared with partial nephrectomy. J Urol. https://doi.org/10.1016/j.juro.2007.09.077
Lane BR, Babineau DC, Poggio ED, Weight CJ, Larson BT, Gill IS et al (2008) Factors predicting renal functional outcome after partial nephrectomy. J Urol. https://doi.org/10.1016/j.juro.2008.08.036
Kong HJ, Park JS, Kim DY, Shin HS, Jung HJ (2013) Renal function following curative surgery for renal cell carcinoma: who is at risk for renal insufficiency? Korean J Urol. https://doi.org/10.4111/kju.2013.54.12.830
Huang WC, Levey AS, Serio AM, Snyder M, Vickers AJ, Raj GV et al (2006) Chronic kidney disease after nephrectomy in patients with renal cortical tumours: a retrospective cohort study. Lancet Oncol. https://doi.org/10.1016/S1470-2045(06)70803-8
Lucas SM, Stern JM, Adibi M, Zeltser IS, Cadeddu JA, Raj GV (2008) Renal function outcomes in patients treated for renal masses smaller than 4 cm by ablative and extirpative techniques. J Urol. https://doi.org/10.1016/j.juro.2007.08.156
Wang Z, Liu C, Chen R, Liu S, Feng C, Yu K et al (2018) Will the kidney function be reduced in patients with renal cell carcinoma following laparoscopic partial nephrectomy? Baseline eGFR, warm ischemia time, and RENAL nephrometry score could tell. Urol Oncol Semin Orig Investig. https://doi.org/10.1016/j.urolonc.2018.08.007
Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW et al (2003) National kidney foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med 139:137–147. https://doi.org/10.7326/0003-4819-139-2-200307150-00013
Jeon HG, Jeong IG, Lee JW, Lee SE, Lee E (2009) Prognostic factors for chronic kidney disease after curative surgery in patients with small renal tumors. Urology. https://doi.org/10.1016/j.urology.2009.05.090
Lane BR, Campbell SC, Demirjian S, Fergany AF (2013) Surgically induced chronic kidney disease may be associated with a lower risk of progression and mortality than medical chronic kidney disease. J Urol. https://doi.org/10.1016/j.juro.2012.11.121
Newgard CB, Sharpless NE (2013) Coming of age: Molecular drivers of aging and therapeutic opportunities. J Clin Invest. https://doi.org/10.1172/JCI68833
Peyton CC, Rothberg MB, Jiang V, Heavner MG, Hemal AK (2017) Comparative analysis of renal functional outcomes and overall survival of elderly vs nonelderly patients undergoing radical nephrectomy. J Endourol. https://doi.org/10.1089/end.2016.0525
Najarian JS, McHugh LE, Matas AJ, Chavers BM (1992) 20 years or more of follow-up of living kidney donors. Lancet. https://doi.org/10.1016/0140-6736(92)92683-7
Fehrman-Ekholm I, Blinder CG, Stenbeck M, Tydén G, Groth CG (1997) Kidney donors live longer. Transplantation. https://doi.org/10.1097/00007890-199710150-00007
Barlow LJ, Korets R, Laudano M, Benson M, McKiernan J (2010) Predicting renal functional outcomes after surgery for renal cortical tumours: a multifactorial analysis. BJU Int 106:489–492. https://doi.org/10.1111/j.1464-410X.2009.09147.x
Reinstatler L, Klaassen Z, Barrett B, Terris MK, Moses KA (2015) Body mass index and comorbidity are associated with postoperative renal function after nephrectomy. Int Braz J Urol. https://doi.org/10.1590/S1677-5538.IBJU.2014.0383
Bratslavsky G, Liu JJ, Johnson AD, Sudarshan S, Choyke PL, Linehan WM et al (2008) Salvage partial nephrectomy for hereditary renal cancer: feasibility and outcomes. J Urol. https://doi.org/10.1016/j.juro.2007.08.150
Shuch B, Singer EA, Bratslavsky G (2012) The surgical approach to multifocal renal cancers: hereditary syndromes, ıpsilateral multifocality, and bilateral tumors. Urol Clin North Am. https://doi.org/10.1016/j.ucl.2012.01.006
Acknowledgements
The authors would like to thank Cansu Olt for the helpful assistance.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
AO defined the concept. AO, OC designed the study. AO, ME defined the intellectual content. OC, RBD, KS helped in literature search. OC, RBD acquired the data. MB, ED, ME analysed the data. OC, AO, ME, ED prepared the manuscript. OC, MB, ED edited the manuscript. AO, ED reviewed the manuscript. All authors reviewed and edited the manuscript and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written consent form is not required due to retrospective nature of manuscript. Istanbul Prof. Dr. Cemil Tascioglu city Hospital Ethics Committee approved the study in 24/05/2021. Approval no is 209.
Consent for publication
Consent for publication was obtained from the patient/next of kin.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Can, O., Sabuncu, K., Erkoç, M. et al. Chronic kidney disease following nephrectomy for renal tumours: retrospective analysis risk factors. Afr J Urol 29, 42 (2023). https://doi.org/10.1186/s12301-023-00373-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12301-023-00373-3