Abstract
Background
Dyslipidemia is directly related to morbidity and mortality in elderly prostate carcinoma patients. The purpose of this study was to evaluate the effects of androgen deprivation therapy (ADT) on the lipid profile among Indian patients with locally advanced and metastatic prostate carcinoma.
Methods
The prospective database of prostate carcinoma patients, who received ADT and whose lipid profile data for the first two years of treatment with ADT was available, were divided into two groups for retrospective analysis: Group A patients are those who had undergone bilateral orchidectomy, while group B patients received luteinizing hormone-releasing hormone agonist (LHRHa). The data analyzed include baseline characteristics, prostate-specific antigen (PSA), and lipid profile.
Results
A total of 69 eligible patients were divided into two groups: group A—29 patients and group B—40 patients. Patients of both the groups reported a significant decrease in the mean serum PSA level from the commencement of ADT and remained close to nadir level till 24 months. In the group A patients, lipid profile parameters except high-density lipoprotein cholesterol showed statistically insignificant deterioration with maximum impact at 6 months. Among the group B patients, the total cholesterol (11.9%), triglycerides (22.2%), and low-density lipoprotein cholesterol (21.1%) increased significantly at 6 months and returned to the near baseline at 12 months and thereafter persisted at the similar level. The mean very low-density lipoprotein level (15.5%) also increased significantly at 6 months and then showed a gradual decline till 24 months of follow-up.
Conclusions
LHRH agonist used as ADT for prostate carcinoma leads to a statistically significant but clinically insignificant temporary worsening in the lipid profile.
Similar content being viewed by others
1 Background
Prostate carcinoma is the second most common cancer among men and the fifth most common cause of cancer-related mortality, with the average age at diagnosis being 66 years [1]. Effective systematic treatment of prostate carcinoma has greatly improved the life expectancy for these patients and, except for patients with metastatic disease, the 5-year relative survival rate today is in excess of 98% [2]. Androgen deprivation therapy (ADT) is one of the main modalities for treating patients with metastatic disease, and is also used as an adjunct to radiation therapy in patients with locally advanced disease as well as in those with unfavorable intermediate-risk or high-risk localized disease. The aim of ADT is hypogonadism, which is either achieved surgically with bilateral orchidectomy or medically using luteinizing hormone-releasing hormone agonists (LHRHa) or LHRH antagonists [3]. However, ADT has its side effects, such as loss of libido, hot flashes, osteoporosis, fatigue, loss of lean body mass, anemia, gynecomastia, and development of the metabolic syndrome [4, 5].
Several studies have reported changes in the lipid profile of men on ADT, but with inconsistent results. Most studies demonstrated a significant increase in triglyceride levels (by about 26%), total cholesterol (by about 10%), and high-density lipoprotein (HDL) levels (by approximately 8–10%), but no change in low-density lipoprotein (LDL) levels, after 3, 6, and 12 months of ADT [6, 7].
A large population-based cohort study including 73,196 patients reported a significantly increased risk of cardiac events among patients on LHRHa; however, in contrast, orchidectomy did not significantly alter the risk of cardiac events [8]. Hence, there is a possibility that orchidectomy could be associated with fewer adverse effects on multiple health domains compared to long-term LHRHa use. Since dyslipidemia is directly related to morbidity and mortality in elderly prostate carcinoma patients, this study aimed to evaluate the effects of two commonly used modalities of ADT on the lipid profile in Indian patients with locally advanced and metastatic prostate carcinoma.
2 Methods
We prospectively maintained a database of patients who attended the prostate carcinoma clinic at our hospital between January 2013 and December 2019 and patients who satisfied the eligibility criteria, were included in this retrospective analysis. Inclusion criteria: patients with prostate carcinoma who received ADT and whose lipid profile data for the first two years of treatment with ADT were available. Exclusion Criteria: (1) Those who required medication other than ADT for prostate carcinoma during the first two years; (2) Those who were on lipid-lowering agents at the time ADT was started.
The eligible patients were divided into two groups. Group A: Those patients who had undergone a bilateral orchidectomy. Group B: Those patients who had received LHRH agonist (Triptorelin is the LHRH agonist prescribed at our center). The choice between bilateral orchidectomy and LHRH agonist was made by the patient after a detailed discussion on the advantages and disadvantages of the two modalities of ADT.
Data recorded for each patient included: Diagnosis, detailed treatment history, age, body mass index (BMI), prostate-specific antigen (PSA), and lipid profile [including total cholesterol, serum triglycerides (TG), HDL, LDL, and very low-density lipoprotein (VLDL)] at the baseline and then at 6, 12 and 24 months follow-up after ADT initiation.
The study parameters were entered into a Microsoft Excel spreadsheet (Microsoft, Seattle, WA USA) and analyzed by SPSS version 21.0 (SPSS Inc., Chicago, IL) software package. Qualitative data were analyzed with Fisher exact test and quantitative data with one-way ANOVA test and t test as applicable with a p value < 0.05 being considered as significant.
3 Results
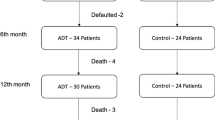
A total of 157 prostate carcinoma patients were started on ADT during the study period, of which 69 patients satisfied the eligibility criteria and were divided into two groups: group A—29 patients and group B—40 patients. Of 88 excluded patients, 54 patients were already on lipid-lowering medication at the time of ADT initiation,15 and 9 received chemotherapy and abiraterone, respectively, within the first two years of starting ADT, and in 10 patients, lipid profile data for the first two years after initiation of treatment was not available. One patient from group A and two from group B were started on lipid-lowering agent 6 months after ADT initiation and data of these patients were excluded from subsequent analysis (Fig. 1).
The baseline characteristics of the two groups are summarized in Table 1. Among group A and B patients, eight and nine patients, respectively, had a history of either radical prostatectomy or radical radiotherapy. Antiandrogen (Bicalutamide 50 mg once daily) was started from the day of bilateral orchidectomy or the start of LHRHa in 23 and 34 patients of groups A and B, respectively. In one patient of group A and 3 patients of group B, bicalutamide was added between 12 and 18 months of follow-up owing to a rise in the serum PSA.
In both groups, serum PSA decreased significantly following commencement of androgen deprivation and remained close to nadir level till 24 months of follow-up. In group A patients, all the lipid profile parameters except HDL cholesterol showed some deterioration with maximum impact at 6 months (percentage deterioration from baseline was 8.3, 7.7, 11.5, and 2.9% for total cholesterol, triglycerides, LDL, and VLDL cholesterol, respectively) of follow-up but none were statistically significant. (Table 2). Among the group B patients (Table 3), the total cholesterol, triglycerides, and LDL cholesterol increased significantly at 6 months (percentage deterioration from baseline was 11.9, 22.2, and 21.1%, respectively) and returned to the near baseline level at 12 months and thereafter persisted at the similar level till 24 months of follow-up. The mean VLDL level also increased significantly at 6 months (percentage deterioration from baseline was 15.5%) and then showed gradual decline till 24 months. HDL cholesterol did not show significant change during the two years of follow-up.
4 Discussion
ADT, targeted at achieving castrate level of serum testosterone, leads to a state of acute andropause with its attendant side effects and alteration in the metabolic profile of the patients. It is important to address these issues as not only the number of people getting ADT is increasing but also the duration of therapy which extends for longer periods, sometimes even over 10 years [9]. Several studies have documented alteration in the lipid profile of men started on ADT, but the results are not consistent and depend on the duration of treatment and the modality of the ADT.
In the present study, we observed statistically insignificant deterioration in the lipid profile parameters in patients who were treated with orchidectomy. Moorjani et al. reported similar changes in TG, LDL, VLDL, and HDL cholesterol levels following orchidectomy [10]. However, Ostergren et al., in a randomized comparative study including 57 patients, observed a significantly higher increase in the fat mass and body weight with orchidectomy compared to that of LHRHa [11]. Saglam et al., in a retrospective study including 44 patients, reported a significant increase in the total cholesterol, LDL, and TG at 12 months along with an increase in the HDL level for the first 3 months followed by a significant decline at 12 months. The difference between LHRHa and orchidectomy concerning the lipid profile was insignificant [12]. The inconsistency in the literature regarding the impact of orchidectomy on lipid profile might be due to different baseline BMI, small sample size, dietary habits, and socioeconomic status.
With LHRHa, we observed a significant increase in the mean total cholesterol, TG, and LDL cholesterol at 6 months followed by a return to the baseline at 12 months, and thereafter persisted at a similar level till 24 months. The mean VLDL level also increased significantly till 6 months and then showed a gradual decline till 24 months follow-up. Only the mean HDL cholesterol did not show a significant change during the study duration. Similar results were reported by Salvador et al. in a prospective study with LHRHa in 33 locally advanced and metastatic prostate cancer patients. They observed a significant increase in the total cholesterol [210–227 mg/dl (p < 0.05)] and LDL [132–148 mg/dl (p < 0.05)] with no significant change in HDL and TG levels at 6 months follow-up with the return of all lipid parameters to baseline at 12 months of follow-up [13]. In another prospective study, including 39 patients receiving LHRHa with or without bicalutamide, a significant increase was reported in the total cholesterol and LDL cholesterol starting at 3 months and the significant rise persisted till 9 months for total cholesterol and 12 months for LDL [14].
The difference in the impact of orchidectomy vs LHRHa on the lipid profile may be due to the different hormonal changes in either group: higher serum FSH, and LH, lower serum testosterone and estrogen with orchidectomy compared to low FSH and LH, and relatively higher estrogen with LHRHa. Also, in the absence of testosterone, serum FSH regulates the level of anti-Mullerian hormone levels [10, 15, 16]. However, the impact of the changes in the hormonal milieu on cardiovascular morbidity is not clearly defined as variable effects have been reported in the literature. Moorjani et al. observed a more favorable impact of LHRHa plus flutamide on lipoprotein profile and consequent cardiovascular disease compared to orchidectomy [10]. Sun et al. in a retrospective cohort study reported significantly higher cardiovascular events (p = 0.01) with gonadotropin-releasing agonist therapy compared to that of orchidectomy [15]. However, Thomsen et al. in an analysis of the prostate cancer population database found a similar 10-year crude probability of cardiovascular disease between medical and surgical castration [16]. In our study, though there was a significant but temporary deterioration in lipid profile with LHRHa and no significant alteration with orchidectomy, we did not observe any new onset clinical cardiovascular event during the 2 years of follow-up.
The results of this study may have an impact on the management of hyperlipidemia secondary to ADT among patients with prostate carcinoma. However, the results of this study are limited by the small sample size. We would like to recommend a prospective randomized study with a larger sample size to assess the impact of different modalities of ADT on lipid profile and consequent cardiovascular health parameters.
5 Conclusions
LHRH agonist used as ADT for locally advanced and metastatic prostate carcinoma was associated with a statistically significant but clinically insignificant temporary worsening in the lipid profile with the return of most of the lipid profile parameters to the baseline by 12 months follow-up. Surgical orchidectomy did not significantly alter the lipid profile.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ADT:
-
Androgen deprivation therapy
- BMI:
-
Body mass index
- LDL:
-
Low-density lipoprotein
- LHRHa:
-
Luteinizing hormone-releasing hormone agonist
- PSA:
-
Prostate-specific antigen
- TG:
-
Triglycerides
- VLDL:
-
Very low-density lipoprotein
References
Rawla P (2019) Epidemiology of prostate cancer. World J Oncol 10(2):63–89
Ryan CJ, Small EJ (2005) Early versus delayed androgen deprivation for prostate cancer: new fuel for an old debate. J ClinOncol 23:8225–8231
Mottet N, Bellmunt J, Bolla M, Joniau S, Mason M, Matveev V et al (2011) EAU guidelines on prostate cancer. Part II: treatment of advanced, relapsing, and castration-resistant prostate cancer. Eur Urol. 59:572–583
Jeong SJ, Kwak C, Lee SE (2001) Therapeutic effect of maximal androgen blockade in metastatic prostate cancer. Korean J Urol 42:642–649
Flaig TW, Glode LM (2008) Management of the side effects of androgen deprivation therapy in men with prostate cancer. Expert OpinPharmacother 9:2829–2841
Smith JC, Bennett S, Evans LM et al (2001) The effects of induced hypogonadism on arterial stiffness, body composition, and metabolic parameters in males with prostate cancer. J Clin Endocrinol Metab 86:4261–4267
Prospective Study Collaboration, Lewington S, Whitlock G, Clarke R et al (2007) Blood cholesterol and vascular mortality by age, sex, and blood pressure: a metaanalysis of individual data from 61 prospective studies with 55,000 vascular deaths. Lancet 370:1829–1839
Keating NL, O’Malley AJ, Smith MR (2006) Diabetes and cardiovascular disease during androgen deprivation therapy for prostate cancer. J ClinOncol 24(27):4448–4456
Pope A, Abel P (2010) Androgen deprivation therapy for prostate cancer and its complications. Trends Urol Gynaecol Sex Health 15(3):32–37
Moorjani S, Dupont A, Labrie F et al (1988) Changes in plasma lipoproteins during various androgen suppression therapies in men with prostatic carcinoma: effects of orchiectomy, estrogen, and combination treatment with luteinizing hormone-releasing hormone agonist and flutamide. J Clin Endocrinol Metab 66(2):314–322
Østergren PB, Kistorp C, Fode M, Bennedbaek FN, Faber J, Sønksen J (2019) Metabolic consequences of gonadotropin-releasing hormone agonists vs orchiectomy: a randomized clinical study. BJU Int 123(4):602–611
Sağlam HS, Köse O, Kumsar S, Budak S, Adsan O (2012) Fasting blood glucose and lipid profile alterations following twelve-month androgen deprivation therapy in men with prostate cancer. Sci World J 2012:696329
Salvador C, Planas J, Agreda F et al (2013) Analysis of the lipid profile and atherogenic risk during androgen deprivation therapy in prostate cancer patients. Urol Int 90(1):41–44
Torimoto K, Samma S, Kagebayashi Y et al (2011) The effects of androgen deprivation therapy on lipid metabolism and body composition in Japanese patients with prostate cancer. Jpn J ClinOncol 41(4):577–581
Sun M, Choueiri TK, Hamnvik OP et al (2016) Comparison of gonadotropin-releasing hormone agonists and orchiectomy: effects of androgen-deprivation therapy. JAMA Oncol 2(4):500–507
Thomsen FB, Sandin F, Garmo H et al (2017) Gonadotropin-releasing hormone agonists, orchiectomy, and risk of cardiovascular disease: semi-ecologic, nationwide, population-based study. Eur Urol 72(6):920–928
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
NK and SY were involved in the conception. NK, VV and VP/SP were involved in the acquisition of data. NK and VV were involved in the interpretation of data. NK and VP/SP were involved in manuscript drafting. VV and SY were involved in manuscript revision. SY was involved in the analysis. VP/SP was involved in data analysis. All the authors have approved the submitted version and agreed both to be personally accountable for the author's own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval and consent to participate
The study is approved by Institute ethics committee, VMMC and Safdarjung Hospital, New Delhi, India Date of approval: 05/08/2020 (IEC/VMMC/Project/2020-07/CC-07).
Consent to participate
Not required as the study was retrospective analysis of long term hospital database. The same was exempted by the Institute Ethics Committee.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Kumar, N., Vasudeva, V., Yadav, S. et al. The impact of androgen deprivation therapy on the lipid profile in patients with prostate carcinoma. Afr J Urol 28, 27 (2022). https://doi.org/10.1186/s12301-022-00295-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12301-022-00295-6