Abstract
Background
Patients with idiopathic calcium oxalate stones are advised to consume a low-oxalate diet to prevent recurrence. In this study, on patients with calcium oxalate stones we have attempted to determine the effect of calcium content of diet on the formation of calcium oxalate crystals in urine by in vitro supersaturation study of fresh postprandial urine samples and observing the morphology of the crystals formed using polarized optical microscopy.
Methods
The trial was conducted as a prospective interventional randomised crossover clinical trial in a repeated measures design. Sixty patients with calcium oxalate stones and no metabolic abnormalities in urine treated by lithotripsy at a tertiary care centre during the period May 2016 to May 2019 were recruited. Following a 14 h overnight fasting, urine samples were collected after providing the patient with either a low- or high-calcium meal for breakfast followed four hours later, by high-oxalate meal for lunch. Urine was tested for multiple parameters including urine pH, specific gravity, calcium/creatinine ratio and supersaturation of urine with sodium oxalate followed by optical density measurement by spectrophotometry and microscopic analysis of crystals formed.
Results
Optical density values and calcium/creatinine ratio of urine samples obtained after high-calcium meal are significantly higher than in corresponding sample obtained after low-calcium meal (p < 0.001). These findings were reflected in the morphology of formed crystals in their size, shape and number. When urinary calcium levels were low, no crystals were formed during supersaturation study of postprandial urine samples following a high-oxalate diet.
Conclusions
High calcium content in diet significantly contributes to kidney stone formation. There is a lower risk of kidney stone formation with a low-calcium meal even on consumption of a high-oxalate diet.
Similar content being viewed by others
1 Background
Calcium oxalate stones are the most common kidney stones followed by calcium phosphate and uric acid. One basic event that is common in all stone patients is supersaturation of urine with crystal components—calcium and oxalate in the case of calcium oxalate stone formers. This is the driving force behind stone formation [1, 2]. As the supersaturation of a substance increases, there is increased chance of particle interaction and crystal formation [3]. Calcium oxalate stone formation is a multi-step process that involves nucleation, crystal growth, crystal aggregation, and crystal retention in a micro-environment of supersaturation and altered urine pH [4, 5].
The current advice generally given to calcium oxalate stone patients is to consume a low-oxalate diet for preventing recurrence [6]. Such diets may be high in calcium content, and there is a strong correlation between intake of calcium and urinary calcium excretion, with one study reporting a mean urinary calcium increase in 55–72 mg associated with every 1000 mg increase in daily calcium [7]. Studies have shown that the urinary levels of calcium peaks at 4 h after calcium test meal in the postprandial period [8]. This study was conceptualized to determine whether the calcium content of diet can independently affect the tendency for stone formation in calcium oxalate stone formers.
2 Methods
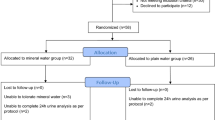
This prospective interventional randomized crossover clinical trial was a repeated measures design study in which each patient was randomly assigned to a sequence of interventions in the form of diet. The sample size was calculated to be sixty, and the sixty patients in the study were randomly allotted into two groups with an allocation ratio of 1:1 following simple randomization procedures (computer-generated list of random numbers), thirty patients in each group. The first group (group A) was provided a high-calcium breakfast followed by a high-oxalate lunch, and the second group (group B) was provided a low-calcium breakfast followed by a high-oxalate lunch. Seven days later the patients were asked to return, and the dietary intervention was reversed (low-calcium breakfast followed by a high-oxalate lunch for group A and high-calcium breakfast followed by a high-oxalate lunch for group B).
Sixty patients in the age group between 19 and 60 years with calcium oxalate stones in the kidney or upper ureter who were evaluated for their stone and treated by extracorporeal shock wave lithotripsy (ESWL) in the urology department of our tertiary care hospital during the period May 2016 to May 2019 were recruited. After ESWL, patients were advised life style correction and citrate therapy for a period of three months prior to enrolment.
Patients were excluded from the study if they had urinary stones which are not calcium based (such as: uric acid, cystine, struvite) or if they suffered from obstructive uropathy, chronic urosepsis, positive urine culture, gross hematuria, renal failure (S. creatinine > 2.0 mg%), renal tubular acidosis, medullary sponge kidney, hyperoxaluria (> 40 mg/day), hypercalciuria (> 300 mg/day), hyperuricosuria (> 700 mg/day), hypomagnesuria (< 40 mg/day), hypocitraturia (< 320 mg/day), anatomical abnormalities of the urinary tracts, active cancer, or were pregnant or unable to give informed consent.
Each patient underwent overnight fasting of 14 h from 6.00 p.m. to 8.00 a.m. (allowed intake of only mineral water 500 ml to avoid dehydration), and an early morning urine sample was collected. The patient was then provided with a high-calcium breakfast consisting of six slices of white bread, three slices of cheese, 200 mL plain milk and one 500 mg tablet of calcium carbonate. This was followed four hours later by a high-oxalate lunch (Calcium content of high calcium breakfast: 1340 ± 20 mg). The patient was adequately hydrated between meals with mineral water of known calcium content. Urine samples were collected two and four hours after each meal. The second batch of tests were conducted after a period of seven days of normal diet. The procedure followed was the same as above except for the nature of the diet given—a low-calcium breakfast consisting of three pieces of plain dosa and 45 mL of coconut chutney. This was followed four hours later by a high-oxalate lunch (calcium content of low-calcium breakfast: 90 ± 10 mg.)
Collected urine samples were assayed for pH, specific gravity and calcium/creatinine ratio. The urine was then subjected to crystal aggregation assay: spectrophotometric estimation of optical density (OD) of urine samples during supersaturation at 620 nm wavelength [1].
2-ml centrifuged urine sample was taken in the cuvette for the study. 10 µl of sodium oxalate was added per minute into the urine sample with continuous stirring to a maximum of 150 µl. OD was measured every minute for 61 min, and subsequently the sample was centrifuged. The sediment was subjected to microscopy under polarizing microscope, and type of crystals, their number, shape and size of formed crystals were studied.
Continuous variables were expressed as mean and standard deviation (SD), and statistical significance for comparisons was determined using unpaired t test analysis. A p value < 0.01 was considered as statistically significant. Data analysis was performed using SPSS ver 16.0. The mean and SD values obtained were first compared between the two groups, to assess whether any significant differences were there depending on which diet was administered first. Then we grouped the values obtained after consumption of high-calcium diet together and compared them with the values obtained after consumption of low-calcium diet to assess whether any significant difference was there depending on the nature of the diet that was administered.
3 Results
The two groups of 30 patients each showed no statistically significant differences between the mean values for age, sex distribution, pH, specific gravity and urinary calcium/creatinine ratio as shown in Table 1.
On comparing between the values of the 60 patients obtained after consumption of low-calcium diet and high-calcium diet, it was found that the mean urinary calcium/creatinine ratio after low calcium diet was 0.07 (SD = 0.03), while after high-calcium diet was 0.128 (SD = 0.069). This was found to be statistically significant (p < 0.001). Data are provided in Additional file 2.
The mean OD value (maximum optical density value obtained for the urine sample) on crystal aggregation study of post-breakfast urine samples after low-calcium diet was 0.056 (SD = 0.078), whereas after high-calcium diet was 0.124 (SD = 0.095). This was found to be statistically significant (p < 0.001). Data are provided in Additional file 2. In the post-lunch (high oxalate) samples, the mean OD time after low-calcium diet was 0.027 (SD = 0.059) and after high-calcium diet was 0.107 (SD = 0.082). This was also found to be statistically significant (p < 0.001).
The number and size of crystals induced by supersaturation studies were significantly higher and larger in the four hour and post-lunch samples of high-calcium diet compared to low-calcium diet (p < 0.001) (Figs. 1, 2).
4 Discussion
The urinary calcium/creatinine ratio after consumption of a high-calcium diet was significantly higher than after consumption of a low-calcium diet. This clearly indicates that on consuming a diet rich in calcium the amount of calcium excreted in urine increases significantly, and there is a corresponding decrease in the amount of calcium excreted in urine when a low-calcium-containing diet is consumed. The same has been stated by Grieff and Bushinsky in 2013 [7].
The crystal aggregation assay by supersaturation showed that optical density time after consumption of a high-calcium diet is significantly higher than after consumption of a low-calcium diet. These findings imply that the tendency for crystal formation in patients treated for calcium oxalate stones can be significantly decreased if the amount of calcium in the diet is reduced. This decreased tendency for crystal formation persisted even after consumption of a high-oxalate meal for lunch. Therefore, if the patient takes a low-calcium diet, the tendency for nucleation and crystal aggregation becomes negligible even if the patient takes a high-oxalate diet afterwards. This is in contrast to the statement by Holmes, Knight and Assimos that a deviation from low-oxalate diet in even a single meal could potentially result in significant stone growth [6].
Crystal morphology study by polarizing microscope was performed on the urine samples. Figures 1 and 2 show the changes in the number and size of crystals formed after urine supersaturation when viewed under the microscope. There was a significant decrease in the number and size of the crystals formed in samples obtained after a low-calcium meal when compared to the samples obtained after a high-calcium meal. This provided visual confirmation of decreased tendency of stone formation on reduction of the calcium content of the diet.
It is interesting to note that in some patients after a low-calcium breakfast optical density could not be recorded in the postprandial urine sample. In these patients, the level of calcium in the sample was < 4 mg% and crystals do not form during supersaturation study of the post-breakfast urine sample. When the patient consumes an oxalate loaded lunch after four hours, there is still no crystal formation. A limitation of the study was that though the patients were randomly allotted to the two groups, blinding was not possible.
The current dietary recommendation to consume a low-oxalate diet is very rarely followed by many patients because a low-oxalate diet reduces the taste and palatability of the diet. Table 3 shows the calcium content of food items commonly included in breakfast that were used in this study. Our results show that it may be possible to modify the dietary recommendations for calcium oxalate stone formers such that when an occasional high-oxalate meal is consumed, significantly decreasing the calcium content of the diet for that day may help to ensure that the risk of stone formation remains low. Further studies are required before the dietary recommendations can be modified in this manner.
5 Conclusions
Calcium content of diet is reflected in the urinary excretion of calcium. There is a strong positive correlation between the calcium levels of urine and the chance for crystal formation in stone patients. Consumption of a diet rich in calcium may increase the chance of stone formation in calcium oxalate stone formers, and there is a lower risk of kidney stone formation with a low-calcium diet even on consumption of a high-oxalate meal.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CaOx:
-
Calcium oxalate
- ESWL:
-
Extracorporeal shock wave lithotripsy
- OD:
-
Optical density
- SD:
-
Standard deviation
References
Borghi L, Guerra A, Meschi T, Briganti A, Schianchi T, Allegri F, Novarini A (1999) Relationship between supersaturation and calcium oxalate crystallization in normals and idiopathic calcium oxalate stone formers. Kidney Int 55:1041–1050
Coe FL, Worcester EM, Evan AP (2016 Sep) Idiopathic hypercalciuria and formation of calcium renal stones. Nat Rev Nephrol 12(9):519–533
Carvalho M, Vieira MA (2004) Changes in calcium oxalate crystal morphology as a function of supersaturation. Int Braz J Urol 30(3):205–209
Chaiyarit S, Thongboonkerd V (2017) Defining and systematic analyses of aggregation indices to evaluate degree of calcium oxalate crystal aggregation. Front Chem 5:113
Ratkalkar VN, Kleinman JG (2011) Mechanisms of stone formation. Clin Rev Bone Miner Metab. 9(3–4):187–197
Holmes RP, Knight J, Assimos DG (2016) Lowering urinary oxalate excretion to decrease calcium oxalate stone disease. Urolithiasis 44(1):27–32
Grieff M, Bushinsky DA (2013) Nutritional prevention and treatment of kidney stones. In: Kalantar-Zadeh K (ed) Joel D Kopple, Shaul G Massry. Academic Press, Nutritional management of renal disease, pp 699–709
Kolbach-Mandel AM, Kleinman JG (2015 Oct) JA Wesson (2015) Exploring calcium oxalate crystallization: a constant composition approach. Urolithiasis. 43(5):397–409
Acknowledgements
The authors wish to acknowledge the contribution of Mr. Jayakumar, statistician for providing advice regarding proper statistical methods and of Mrs. Rejitha, laboratory technician for her help in the analysis of the urine samples.
Funding
This project has been funded under the Science Research Scheme by the Kerala State Council for Science, Technology and Environment (KSCSTE), an autonomous body under the ministry of science and technology, Kerala, India. Award Number: 018/SRSHS/2013/CSTE. Recipient: Sathish Kumar Gopala, M.S., M.Ch (Urology). They provided the financial aid for conduct of the study.
Author information
Authors and Affiliations
Contributions
SKG conceived the study, significantly contributed to the acquisition, analysis and interpretation of data and drafted the manuscript. JJ significantly contributed to the design of the work and interpretation of data and was a major contributor in writing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Human Ethics Committee, Medical College Thiruvananthapuram, IEC.No.07/04/2017/MCT. Registered 07 July 2017. Clinical Trials Registry-India (CTRI), CTRI/2017/07/009143. Registered 27 July 2017-Retrospectively registered, http://ctri.nic.in/Clinicaltrials/pmaindet2.php?trialid=18408.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
. Trial reporting: The authors declare that they have adhered to CONSORT guidelines for reporting clinical trials while preparing the manuscript and the CONSORT checklist is included as a supplementary file.
Additional file 2
. Urine calcium-creatinine ratio and O.D values of the sixty patients.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Gopala, S.K., Joe, J. Effect of calcium content of diet on crystal formation in urine of patients with calcium oxalate stones: a randomized crossover clinical trial. Afr J Urol 27, 124 (2021). https://doi.org/10.1186/s12301-021-00222-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12301-021-00222-1