Abstract
Background
Varicocele presents as the most frequent cause of infertility in men. Most reports showed that varicocelectomy has a significant impact on male fertility and reproductive outcome. This study aims to evaluate the safety and effectiveness of scrotal–inguinal microsurgical varicocelectomy in treating male infertility.
Methods
We prospectively studied preoperatively and postoperatively (at 3 and 6 months) 86 consecutive patients diagnosed with varicocele, abnormal semen parameters, and infertility, undergoing scrotal–inguinal microsurgical varicocelectomy. Semen test was performed before surgery and at 3 months and 6 months after surgery. The reproductive events were short-term followed up.
Results
The median age of the patient was 32.9 ± 5.1 (20–43). Two cases (2.7%) had a minor infection of the scrotum incision, who were well treated by appropriate antibiotics. After operation, total sperm count and the percentage of motile sperms at 3 months and 6 months were significantly higher than those pre-varicocelectomy, respectively. In total, 26.7% (23/86) of all couples achieved a spontaneous pregnancy. Late complications such as testicular atrophy, hydroceles, and recurrent varicocele have not occurred.
Conclusions
Scrotal–inguinal microsurgical varicocelectomy is an acceptable method in treating male infertility due to high rate of reproductive outcomes and very low rate of complications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.1 Background
A varicocele is determined as abnormal tortuous and dilated veins in the pampiniform venous plexus of the scrotal sac. The prevalence of varicocele is between 15 and 20% of the men, up to 35% of male patients with infertility, and 75–81% of secondary male infertility [1]. It is proven that the presence of varicocele is correlated with a risen risk of abnormal sperm parameters [2,3,4]. Despite the mechanisms that have not yet been thoroughly described, it is possible to be multifactorial. Therefore, the management of varicoceles has been one of the resolutions of male reproductive medicine in the modern era.
Varicoceles are now known as the most cause of male infertility that could be surgically repaired [5]. Several surgical techniques have been applied for varicocele treatment, such as open surgical ligation of the spermatic vein, microsurgical varicocelectomy, and laparoscopic varicocelectomy. Each method has its advantages and disadvantages, and different results have been reported in many previous studies [6,7,8].
Among varied surgical techniques, microsurgical varicocelectomy has been known as the golden standard for varicocele treatment recently because of its high rate of success and very low rate of complications [6, 9]. The most common approaches are retroperitoneal abdominal laparoscopic, infra-inguinal, and sub-inguinal below the groin or intrascrotal [10, 11]. According to Fretz, the scrotal approach is no longer considered due to the higher risk of damage to the spermatic arteries and resultant testicular atrophy [12]. But from our experience, the scrotal–inguinal approach is easier, straightforward, and faster as compared to inguinal approach. Therefore, we carried out this study to evaluate the safety and effectiveness of scrotal–inguinal microsurgical varicocelectomy in treating male infertility.
2 Methods
2.1 Study population
Between January 2018 and February 2020, we prospectively studied preoperatively and postoperatively (at 3 and 6 months) 86 consecutive male patients with varicocele, abnormal semen parameters, and infertility, undergoing scrotal–inguinal microsurgical varicocelectomy. All operations were performed by only one urologist who had more than ten years of experience in microsurgical technique.
We included varicoceles according to the American Society for Reproductive Medicine and Society for Male Reproduction and Urology’s Practice Committee report [4] when each of the following criteria are met: (1) The varicocele is palpable on physical examination of the scrotum; (2) the couple infertility for at least 12 months; (3) the male partner had at least one alteration semen parameter; (4) none of the other contributing male risk factors; and (5) his wife confirmed fertile at the date of evaluation. We excluded from this study the patients with azoospermia or with others like multiple risk factors, abnormality in his wife.
2.2 Surgical technique
The decision to treat was taken by an andrology team including andrologists, urologists, gynecologists, and biologists. The couple was provided with comprehensive information on the advantages and complications of the surgical technique. All patients underwent a unilateral microsurgical varicocelectomy.
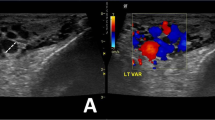
Using either spinal or general anesthesia, two 2‐cm incisions were made (scrotal and inguinal incision, as shown in Fig. 1). The spermatic cord was identified, and its fascia was opened. Under 10× microscopic magnification, the external and internal spermatic veins were identified (Fig. 2) and ligated using either sutures or surgical clips, while preserving the internal spermatic arteries, deferential artery, vasal vein, and lymphatic vessels (Fig. 3). Testicular biopsy was also performed in most cases to determine whether patients may benefit from varicocele repair [13, 14].
2.3 Semen analysis
A semen analysis was performed once before the surgery and at least two times after the surgery at the third and sixth month. Sperm count and total motile sperm count (TMSC) were calculated. The TMSC was calculated using the following formula: TMSC = ejaculate volume × concentration × motile fraction.
Semen samples were examined within 60 min after ejaculation in order to maintain the quality of the specimen.
2.4 Statistical analysis
Outcome variables included: sperm concentration, percentage of motile sperms, spontaneous pregnancy, early and late complications. Postoperative complications were recorded and graded as per Clavien–Dindo classification. Subsequently, all patients were contacted by telephone in February 2020 to determine the reproductive events.
SPSS version 20 was used for statistical analysis. Descriptive statistics were used for semen health parameters at the 3- and 6-month stages. A paired T-test (or Wilcoxon test in case of not normally contributed data) was used to compare the evolution of sperm quality between the pre-operational level and the 3- and 6-month review.
3 Results
A total of 86 consecutive men with palpable varicocele and infertility participated in our study. The median of age was 32.9 ± 5.1 years (range 20–43). The pre- and postoperative semen parameters are shown in Table 1. After operation, the mean (± SE) of total sperm count and the percentage of motile sperms at 3 months and 6 months were significantly higher than those pre-varicocelectomy.
The median follow‐up period for reproductive outcome was 12.9 months (range 2–19 months).
The first spontaneous pregnancy in a couple was informed at 2 months after surgery. Cumulatively, 26.7% (23/86) of all couples achieved a pregnancy at the end of follow-up.
Out of the 63 patients that did not have pregnancy outcome data, 12 patients were histopathologically confirmed with testicular hyalinization. The remaining 51 patients were not significantly different from the 23 men with available pregnancy data with respect to initial sperm concentration, sperm motility, or age (male patients and spouse) (data not shown).
Postoperative events: Two cases (2.7%) get a minor infection of the scrotum incision within one week after surgery, who were well treated with appropriate antibiotics. Late complications such as testicular atrophy, hydroceles, and recurrent varicocele have not occurred within a 6-month postoperative follow-up.
4 Discussion
The target of varicocele treatment is to obstruct the refluxing venous drainage to the testis while maintaining arterial inflow and lymphatic drainage as much as possible [15, 16]. Many surgical techniques have been suggested. A number of studies have been reported, and they showed somewhat different outcomes, such as for pregnancy rates and potential complications [17]. According to Fretz, the scrotal approach is no longer considered to perform due to the higher risk of damage to the spermatic arteries and resultant testicular atrophy [12]. But in our experience, the scrotal–inguinal microsurgical varicocelectomy had many advantages that were proven in our series with a high success rate and very low potential complication. Furthermore, via the scrotal incision, the testicle was also examined in order to perform biopsy in most cases. This is the reason we prefer unilateral scrotal–inguinal microsurgical varicocelectomy in treating male infertility at our hospital recently to other surgical technique, such as inguinal microsurgical varicocelectomy. To our knowledge, this is the first paper using the scrotal–inguinal microsurgical technique for varicocelectomy.
The microsurgical varicocelectomy is an innovative technique that allows the ligation of all of the veins except the vasal vein while protecting the testicular artery and lymphatics, leading to a minimal rate of varicocele recurrence and postoperative complications [18]. During microsurgical operation, delivery of the testicle provides direct visual access to all avenues of testicular venous effluent, which leads to a significantly decreased rate of varicocele recurrence [19].
Our data were consistent with most previous studies that varicocele repair had a positive impact on semen parameters. Agarwal et al. [20] conducted a meta-analysis from 17 studies to evaluate the efficacy of surgical varicocelectomy (inguinal microsurgery or high ligation) in developing semen parameters, including both observational studies and randomized clinical trials. The target population was men diagnosed infertile with clinically examined unilateral or bilateral varicocele and at least one alteration semen parameter. The results presented that the total sperm count increased by 9.71 × 106/mL (p < 0.00001), and sperm motility increased by 9.92% (p < 0.0001) after performing a microsurgical varicocelectomy. Similarly, the sperm count increased by 12.03 × 106/mL (p = 0.0002), and sperm motility increased by 11.72% (p = 0.002) after doing a high ligation varicocelectomy.
Baazeem et al. [21] carried out a similar meta-analysis study that consisted of only randomized clinical trials, but several studies for interventional radiology (embolization) as well as operation were included in their study. Sperm concentration, total sperm motility, and progressive motility before and after operation of clinical varicocele were investigated. The results suggested that varicocelectomy is correlated with a significant increase in sperm count, and total as well as progressive motility. In a meta-analysis conducted by Schauer et al. [22], they investigated the influence of 3 operative methods (sub-inguinal varicocelectomy, the inguinal approach, and high ligation) for varicocelectomy on sperm parameters (concentration and motility) and indicated that varicocelectomy could significantly improve the sperm concentration and motility regardless of operative methods. Besides, varicocele was correlated with sperm DNA damage, and this sperm pathology might be a secondary to varicocele-mediated oxidative stress. Some studies presented that varicocelectomy could reverse this sperm DNA damage [23].
Regarding the influence of varicocele treatment on the reproductive outcomes, our study showed 26.7% (23/86) of all couples achieved a spontaneous pregnancy within a short-term follow-up. The pregnancy rate in our study was lower than in other reports because out of the 63 patients that did not have pregnancy outcome data, 12 patients were histopathologically confirmed with testicular hyalinization. Therefore, diagnostic testicular biopsy during varicocele repair contributes a realistic and important role [13, 14].
In 2009, Cayan et al. [24] evaluated the pregnancy rate after varicocelectomy from 36 studies to find out the best surgical method based on the reproductive outcomes. They defined that the microsurgical varicocelectomy has a higher rate of spontaneous pregnancy and lower postoperative varicocele recurrence than conventional surgical methods and radiological intervention in treating male infertility.
In 2011, Diegidio et al. [25] analyzing from 33 studies with 5000 male patients with infertility showed similar results. The overall rate of pregnancy was reported to be 38.37%, which was highest for the group performing microsurgical sub-inguinal and the microsurgical inguinal operation (44.75% and 41.78%, respectively). Other surgical methods seem to obtain a lower rate of pregnancy outcomes compared with the microsurgical varicocelectomy. For example, the pregnancy rate with the laparoscopic technique was 27.5%, 30.1% for the conventional inguinal surgery, and 34.2% for the Palomo surgical technique.
Our study has some limitations. The small sample size, short-term follow-up, and lack of assisted reproductive techniques were known as the reasons for the spontaneous pregnancy rate in our study being lower than that in other reports. Furthermore, the absence of a control group made it less significant to prove efficacy of this surgical technique.
5 Conclusion
Our study highlights that scroto-inguinal microsurgical varicocelectomy is an excellent option for the treatment of male infertility because it has acceptable rates of reproductive outcomes and very low risk of complication. Further studies are strongly recommended in the field with a larger sample size and long-term follow-up to ascertain conclusions drawn from this study.
Availability of data and materials
The corresponding author has full access to all of the data and takes full responsibility for the veracity of the data.
References
Gorelick JI, Goldstein M (1993) Loss of fertility in men with varicocele. Fertil Steril 59(3):613–616
Kantartzi PD, Goulis ChD, Goulis GD, Papadimas I (2007) Male infertility and varicocele: myths and reality. Hippokratia 11(3):99–104
Niederberger C (2005) Increased seminal reactive oxygen species levels in patients with varicoceles correlate with varicocele grade but not with testis size. J Urol 174(2):660
Practice Committee of the American Society for Reproductive M, Society for Male R, Urology (2014) Report on varicocele and infertility: a committee opinion. Fertil Steril 102(6):1556–1560
Schlesinger MH, Wilets IF, Nagler HM (1994) Treatment outcome after varicocelectomy. A critical analysis. Urol Clin North Am 21(3):517–529
Al-Kandari AM, Shabaan H, Ibrahim HM, Elshebiny YH, Shokeir AA (2007) Comparison of outcomes of different varicocelectomy techniques: open inguinal, laparoscopic, and subinguinal microscopic varicocelectomy: a randomized clinical trial. Urology 69(3):417–420
Cayan S, Kadioglu TC, Tefekli A, Kadioglu A, Tellaloglu S (2000) Comparison of results and complications of high ligation surgery and microsurgical high inguinal varicocelectomy in the treatment of varicocele. Urology 55(5):750–754
Unal D, Yeni E, Verit A, Karatas OF (2001) Clomiphene citrate versus varicocelectomy in treatment of subclinical varicocele: a prospective randomized study. Int J Urol 8(5):227–230
Wang J, Xia SJ, Liu ZH, Tao L, Ge JF, Xu CM, Qiu JX (2015) Inguinal and subinguinal micro-varicocelectomy, the optimal surgical management of varicocele: a meta-analysis. Asian J Androl 17(1):74–80
Velasquez M, Tanrikut C (2014) Surgical management of male infertility: an update. Transl Androl Urol 3(1):64–76
Leslie SW, Sajjad H, Siref LE (2020) Varicocele. In: StatPearls. Treasure Island.
Fretz PC, Sandlow JI (2002) Varicocele: current concepts in pathophysiology, diagnosis, and treatment. Urol Clin North Am 29(4):921–937
Hwang K, Lamb DJ (2011) Diagnostic testicular biopsy before varicocele repair plays a realistic and important role. Fertil Steril 95(2):488
Inci K, Gunay LM (2013) The role of varicocele treatment in the management of non-obstructive azoospermia. Clinics (Sao Paulo) 68(Suppl 1):89–98
Masson P, Brannigan RE (2014) The varicocele. Urol Clin North Am 41(1):129–144
Evers JL, Collins JA (2003) Assessment of efficacy of varicocele repair for male subfertility: a systematic review. Lancet 361(9372):1849–1852
Cho KS, Seo JT (2014) Effect of varicocelectomy on male infertility. Korean J Urol 55(11):703–709
Choi WS, Kim SW (2013) Current issues in varicocele management: a review. World J Mens Health 31(1):12–20
Beck EM, Schlegel PN, Goldstein M (1992) Intraoperative varicocele anatomy: a macroscopic and microscopic study. J Urol 148(4):1190–1194
Agarwal A, Deepinder F, Cocuzza M, Agarwal R, Short RA, Sabanegh E, Marmar JL (2007) Efficacy of varicocelectomy in improving semen parameters: new meta-analytical approach. Urology 70(3):532–538
Baazeem A, Belzile E, Ciampi A, Dohle G, Jarvi K, Salonia A, Weidner W, Zini A (2011) Varicocele and male factor infertility treatment: a new meta-analysis and review of the role of varicocele repair. Eur Urol 60(4):796–808
Schauer I, Madersbacher S, Jost R, Hubner WA, Imhof M (2012) The impact of varicocelectomy on sperm parameters: a meta-analysis. J Urol 187(5):1540–1547
Zini A, Dohle G (2011) Are varicoceles associated with increased deoxyribonucleic acid fragmentation? Fertil Steril 96(6):1283–1287
Cayan S, Shavakhabov S, Kadioglu A (2009) Treatment of palpable varicocele in infertile men: a meta-analysis to define the best technique. J Androl 30(1):33–40
Diegidio P, Jhaveri JK, Ghannam S, Pinkhasov R, Shabsigh R, Fisch H (2011) Review of current varicocelectomy techniques and their outcomes. BJU Int 108(7):1157–1172
Acknowledgements
The authors thank Dr. Nguyen Huu Son for his valuable assistance.
Funding
No funding resources.
Author information
Authors and Affiliations
Contributions
HTP and TXN have contributed to format the design of the study and revised the collected data. DVN, HAV, DAL, and NHP have done the main work of the statistical data analysis. HTP, TXN, and NDV have shared the operational work of the study and writing works. HTP, TXN, and DVN have recruited the participants, contributed to the operational works, interpretation, and analysis of the results. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee Review Board of Hue Central Hospital under the reference number of 01012018-HCH. Written consents were obtained from all patients. All couples were provided in detail the surgical procedure, success rate, costs, and likely complications.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Phan, H.T., Nguyen, T.X., Nguyen, D.V. et al. Efficacy of scroto-inguinal microsurgical varicocelectomy in treating male infertility. Afr J Urol 27, 38 (2021). https://doi.org/10.1186/s12301-021-00141-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12301-021-00141-1