Abstract
Background
Antiphospholipid syndrome causes systemic arterial and venous thromboses due to the presence of antiphospholipid antibodies. Adrenal insufficiency is a rare complication of antiphospholipid syndrome that may result in fatal outcomes if left untreated. Therefore, we report adrenal insufficiency as a rare complication of bilateral adrenal infarction associated with antiphospholipid syndrome and trauma surgery.
Case presentation
A 64-year-old male patient underwent surgery for a left traumatic hemothorax. He concurrently had antiphospholipid syndrome and was receiving warfarin. Postoperatively, the patient complained of severe lumbar back pain despite resuming anticoagulation therapy, and he experienced paralytic ileus and shock. Abdominal contrast-enhanced computed tomography revealed adrenal swelling and increased surrounding retroperitoneal adipose tissue density. Diffusion-weighted abdominal magnetic resonance imaging showed high-intensity areas in the bilateral adrenal glands. Cortisol and adrenocorticotropic hormone levels were 3.30 μg/dL and 185.1 pg/dL, respectively. Subsequently, the patient was diagnosed with bilateral adrenal infarction and acute adrenal insufficiency, and hydrocortisone was immediately administered. Adrenal insufficiency improved gradually, and the patient was discharged after initiating steroid replacement therapy.
Conclusions
The timing of postoperative anticoagulant therapy initiation remains controversial. Therefore, adrenal insufficiency due to adrenal infarction should be monitored while anticoagulant therapy is discontinued in patients with antiphospholipid syndrome.
Similar content being viewed by others
Background
Antiphospholipid syndrome (APS) is an autoimmune disease that causes systemic arterial and venous thromboses due to antiphospholipid antibodies (aPL). Adrenal insufficiency (AI) is a rare complication of APS that occurs in only 0.4% of patients [1] and can lead to fatal outcomes if left untreated. The mortality rate of APS complicated with AI is 3.81% [1]. Here, we report AI as a rare complication of bilateral adrenal infarction associated with APS and trauma surgery.
Case presentation
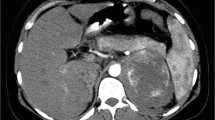
Ethics approval was not needed for this case report. Written informed consent was obtained from the patient for the publication of this report and its accompanying images. A 64-year-old male patient underwent surgery for a left traumatic hemothorax (Fig. 1A). He concurrently had atrial fibrillation and APS with an inferior vena cava filter placement and was receiving warfarin. The preoperative prothrombin international normalized ratio and hemoglobin level were 3.18 and 5.9 g/dL, respectively, and the blood volume in the thoracic cavity at thoracotomy was 1800 g. Bleeding from a right internal thoracic vein branch was suspected, although the bleeding point was unclear (Fig. 1B). Bleeding could not be controlled with cauterization but was managed using multiple hemostatic agents. The intraoperative blood loss was 200 g; hence, 560 and 480 mL of red blood cells and fresh frozen plasma, respectively, were transfused. Autologous blood (1021 mL) was transfused intraoperatively using a cell saver system. A hematoma extending from the right inguinal to the femoral lesions was observed, and it expanded postoperatively; therefore, the initiation of oral warfarin at 1 mg as an anticoagulation therapy was delayed and resumed on postoperative day (POD) 4. Additional continuous intravenous heparin was administered at 100 IU/kg, and oral warfarin was increased to 2 mg on POD 5. However, the patient complained of severe lumbar back pain on POD 6. Abdominal contrast-enhanced computed tomography (CECT) showed no aortic dissection, intra-abdominal hemorrhage, organ infarction, or adrenal swelling. On POD 8, the patient developed paralytic ileus (Fig. 2A) and shock, and his blood pressure decreased to 70/40 mmHg. Septic shock was ruled out based on blood and urine cultures, and disseminated intravascular coagulation was excluded based on the results of the coagulation fibrinolysis tests. Repeated abdominal CECT revealed adrenal swelling and increased surrounding retroperitoneal adipose tissue density (Fig. 2B). The white blood cell count, C-reactive protein level, sodium level, potassium level, serum creatinine level, glucose level, cortisol level, and adrenocorticotropic hormone level were 8340/mm3, 27.54 mg/dL, 130 mmol/L, 4.4 mmol/L, 1.08 mg/dL, 69 mg/dL, 3.30 μg/dL, and 185.1 pg/dL, respectively. Acute AI was suspected, and hydrocortisone (HC) was intravenously administered immediately. Abdominal magnetic resonance imaging revealed high-intensity areas in both adrenal glands on diffusion-weighted images (Fig. 2C), and a diagnosis of AI caused by bilateral adrenal infarctions was made. HC was intravenously administered for 5 days, followed by oral administration at a dosage of 50 mg/day, and AI improved gradually. The patient was discharged on POD 20 after steroid replacement therapy was initiated. HC was tapered and switched to prednisolone (PSL; 5 mg/day) on POD 111. One year has passed since the surgery, and the patient continues to receive PSL (5 mg/day) as an outpatient.
Postoperative findings. A Abdominal radiography shows intestinal gas. B Contrast-enhanced computed tomography reveals adrenal swelling and increased surrounding retroperitoneal adipose tissue density. C Abdominal magnetic resonance imaging reveals high-intensity areas in both adrenal glands on diffusion-weighted images
Discussion and conclusions
APS can cause hemorrhagic adrenal gland infarction and is typically associated with stress factors, including surgery [2]. Bleeding is the leading cause of AI in APS, followed by infarction [1]. Adrenal involvement is usually bilateral [3], and the vascular system of the adrenal gland is unique and complex [3]. Capillary branches from three main arteries form a vascular plexus around the zona reticularis. Furthermore, the transition from the artery to the capillary plexus is known as the “vascular dam,” which is drained by the medullary sinusoids and eventually forms a single central adrenal vein. Venous stasis and hypercoagulability in this region can promote thrombosis, infarction, and subsequent bleeding [3]. Berneis et al. reported a novel mechanism involving the zona fasciculata’s cellular characteristics [4]. In this zone, cells have a high density of late endosomes, which are organelles involved in cholesterol exchange and protein sorting. The membranes of these organelles contain lysobisphosphatidic acid, which is the target of aPLs. These aPLs react locally and promote cholesterol accumulation in cells, leading to cell death and release of lysosomal proteinases, consequently activating endothelial cells, which favors coagulation and causes micro-thromboses [4].
The timing of postoperative anticoagulant therapy initiation is controversial. APS increases the risk of developing venous thromboembolism according to the American College of Chest Physicians guidelines for the perioperative management of antithrombotic therapy [5]. Therefore, heparin bridging is recommended when warfarin is discontinued. However, caution is required when using high-intensity therapeutic dose heparin bridging postoperatively, paticularly in patients undergoing high bleeding-risk surgeries and procedures. If therapeutic dose bridging is used in patients at a high risk of postoperative bleeding, its initiation should be delayed for 48–72 h postoperatively when adequate surgical hemostasis is achieved [5]. However, the intraoperative bleeding point was unclear in our case, and various hematomas were observed from the right inguinal to the femoral lesions. Therefore, heparin and warfarin were resumed 72 h postoperatively. AI caused by adrenal infarction should be monitored while anticoagulant therapy is discontinued in patients with APS.
Availability of data and materials
All data generated or analyzed during this study are included in this published article.
Abbreviations
- AI:
-
Adrenal insufficiency
- aPL:
-
Antiphospholipid antibodies
- APS:
-
Antiphospholipid syndrome
- CECT:
-
Contrast-enhanced computed tomography
- POD:
-
Postoperative day
References
Lee KH, Lee H, Lee CH, Kim JY, Kim JM, Kim SS, et al. Adrenal insufficiency in systematic lupus erythematosus (SLE) and antiphospholipid syndrome (APS): a systematic review. Autoimmun Rev. 2019;18:1–8.
Caron P, Chabannier MH, Cambus JP, Fortenfant F, Otal P, Suc JM. Definitive adrenal insufficiency due to bilateral adrenal hemorrhage and primary antiphospholipid syndrome. J Clin Endocrinol Metab. 1998;83:1437–9.
Tan JW, Shukla A, Hu JR, Majumdar SK. Spontaneous adrenal hemorrhage with mild hypoadrenalism in a patient anticoagulated with apixaban for antiphospholipid syndrome: a case report and literature review. Case Rep Endocrinol. 2022;2022:6538800.
Berneis K, Buitrago-Téllez C, Müller B, Keller U, Tsakiris DA. Antiphospholipid syndrome and endocrine damage: why bilateral adrenal thrombosis? Eur J Haematol. 2003;71:299–302.
Douketis JD, Spyropoulos AC, Spencer FA, Mayr M, Jaffer AK, Eckman MH, et al. Perioperative management of antithrombotic therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141:e326S – e350.
Acknowledgements
We would like to thank Editage (www.editage.jp) for the English language editing.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
YI participated in the surgery, conceived and conducted the study, and performed a literature search. YI, MI, and HU participated in the surgery. NM and HU supervised the manuscript preparation and critically revised the manuscript. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for the publication of this report and its accompanying images.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Iijima, Y., Ishikawa, M., Motono, N. et al. Bilateral adrenal infarction and insufficiency associated with antiphospholipid syndrome and surgery: a case report. Int J Emerg Med 16, 93 (2023). https://doi.org/10.1186/s12245-023-00575-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12245-023-00575-0