Abstract
Background
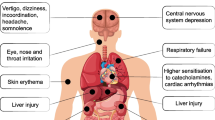
Benzyl alcohol is used as stripping agent in paints and other applications, and benzyl alcohol poisoning is indicated by symptoms, such as impaired consciousness, respiratory depression, hypotension, metabolic acidosis, and renal dysfunction.
Case presentation
A 27-year-old Asian man was transported to a hospital for severe disturbance of consciousness following exposure to a paint stripper containing benzyl alcohol, ethylene glycol, and hydrogen peroxide, which he was using to repaint a bridge. The patient was treated under sedation for benzyl alcohol poisoning. On day 3 of hospitalization, his abdominal computed tomography scan revealed a paralytic ileus, so he was transferred to our hospital. The combined toxicity from multiple substances, mainly benzyl alcohol, was thought to be a contributing factor for the paralytic ileus. Upon arrival, the patient also had chemical burns, hypernatremia, and elevated myogenic enzyme levels. His urinary hippuric acid level was high (14.9 g/L) upon admission to the previous hospital. We treated the patient with artificial respiration management, while avoiding high-density oxygen, and with gastrointestinal decompression by gastric tube implantation; laxatives were also administered. The paralytic ileus improved on the 4th day, the tube was removed on the 6th day, and the patient was discharged on the 11th day of hospitalization. No apparent complications were observed at discharge.
Conclusions
To the best of our knowledge, this is the first case report of paralytic ileus caused by benzyl alcohol, although multiple factors may have influenced the symptoms. After exposure to benzyl alcohol by inhalation and dermal absorption, the patient developed impaired consciousness, metabolic acidosis, and paralytic ileus, and the presence of elevated urinary hippuric acid led to a definitive diagnosis.
Similar content being viewed by others
Background
Benzyl alcohol is used as a stripping agent in paints and other industrial applications and even found in cosmetic products and food additives. Benzyl alcohol is a clear, colorless liquid that is readily available commercially. Although it was previously used as an additive in injectable drugs, its use has been discontinued because of problems, such as “gasping syndrome” in infants [1,2,3].
There are very few reports on benzyl alcohol poisoning in adults, and to our knowledge, there are no reports of poisoning complicated with paralytic ileus. Here, we report the case of a patient with impaired consciousness and paralytic ileus due to complex poisoning mainly from benzyl alcohol.
Case presentation
A 27-year-old Asian man was transported to a nearby general hospital because he experienced severe disturbance of consciousness while using painting material stripper containing benzyl alcohol, ethylene glycol, and hydrogen peroxide to repaint a bridge in the summer. There was no relevant medical history of laparotomy and no noteworthy family history or psychosocial history of addiction.
On arrival at the nearby general hospital, his Glasgow Coma Scale score was 3 (eye, 1; verbal, 1; motor, 1), with no fever and elevated white blood cell count of 25.7 × 103/μL. Computed tomography (CT) and magnetic resonance imaging (MRI) scans of the head showed no abnormal findings. Based on field conditions and interviews with the workplace supervisor, benzyl alcohol poisoning was suspected. The patient was restless and managed with midazolam under sedation, supplemental fluids, and oxygen administration. On the second day of admission, the results of his blood tests revealed worsening of liver and kidney function and metabolic acidosis (Table 1). Since paralytic ileus was suspected on the third day of admission, the patient was transferred to our hospital for further investigation and treatment. No specific treatment for poisoning or ileus paralysis was administered by the previous physician.
On arrival at our hospital, the patient’s Glasgow Coma Scale score was 9 (eye, 2; verbal, 3; motor, 4); he was administered midazolam under sedation (intravenous drip infusion; 5 mg/h). On physical examination, body temperature of 37.7 °C, respiratory rate of 20 breaths/min with a normal respiratory pattern, heart rate of 84 beats/min, and blood pressure of 151/90 mmHg were observed. Auscultation revealed no abnormalities in the heart and lung sounds. Saturation of percutaneous oxygen was measured at 98% in room air, and arterial blood gas analysis showed a partial pressure of arterial oxygen (PaO2) of 87.3 mmHg and alveolar-arterial oxygen difference of 23.2 mmHg; his quick sequential organ failure assessment score was 1. His abdomen was distended, and bowel sounds were attenuated. Blister caps and epidermolysis were found on the abdomen, axillae, elbows, buttocks, and right knee (Fig. 1). The total body surface area, burn index, and prognostic burn index were 14%, 7%, and 34%, respectively.
His laboratory test results showed hypercoagulability (levels of fibrinogen, 733 mg/dL; fibrin/fibrinogen degradation product, 8.4 μg/mL; and D-dimer, 40 μg/mL), elevated levels of myogenic deviation enzymes (creatinine kinase, 1803 IU/L; aspartate transaminase, 64 IU/L; and lactate dehydrogenase, 392 IU/L), and hypernatremia (Na; 148 mmol/L) (Table 2). Urinary screening was performed using a simple drug screening kit, Trigae®DOA (Sysmex Corporation, Kobe, Japan), which showed positive results for benzodiazepines under continuous intravenous midazolam administration and negative results for other drugs, including opioids.
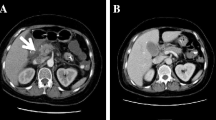
His abdominal radiographic scan showed dilatation of the intestine (Fig. 2A), and abdominal CT scan showed no obvious obstruction, although small bowel dilatation and fluid retention were observed (Fig. 2B). No other organs showed abnormal findings.
As the patient was in the acute stage when he was transferred to our hospital, symptomatic treatment was considered the only feasible treatment option for the poisoning; hence, the patient was intubated and managed with an inhaled oxygen concentration of 30% (Fig. 3). Next, a gastric tube was placed, and laxatives were administered for the paralytic ileus; furthermore, he was started on tazobactam/piperacillin considering the risk of bacterial translocation or generalized peritonitis. Additionally, we treated his metabolic acidosis with infusion crystalloids and skin injury with daily washing and ointment application. On the second day after the patient was transferred to our hospital, a high level of urinary hippuric acid (14.9 g/dL; reference range, < 1.0 g/L) was observed, consistent with the finding of benzyl alcohol poisoning.
After transfer to our hospital, the patient’s progress was good, his laboratory data gradually improved, and his PaO2/fraction of inspired oxygen (FIO2) did not worsen. On the fourth day at our hospital, contrast medium was administered through the gastric tube, and on the fifth day, it had reached the rectum; hence, tube feeding was initiated (Fig. 4). On the sixth day, bowel movement was confirmed, so the patient was extubated, and oral feeding was started. No complications were observed, and the patient was discharged on the tenth day.
Discussion
We encountered a patient with impaired consciousness and a paralytic ileus due to complex benzyl alcohol poisoning. To the best of our knowledge, this is the first case report of paralytic ileus after exposure to benzyl alcohol. The patient developed impaired consciousness, metabolic acidosis, and paralytic ileus, and the presence of elevated urinary hippuric acid led to a definitive diagnosis. It is important to be aware of the possibility of exposure to multiple poisonous substances via multiple routes, especially in enclosed spaces during the summer.
Benzyl alcohol is a key ingredient in many paint removers and can be absorbed orally, by inhalation, or transdermally. It is oxidized by alcohol-depleting enzymes in the liver to produce benzoic acid, which is then combined with glycine and excreted in urine as hippuric acid [4]. Benzyl alcohol poisoning in humans causes impaired consciousness, respiratory depression, hypotension, metabolic acidosis, renal dysfunction, and hypothermia. Laboratory findings of benzyl alcohol poisoning include anion gap-opening metabolic acidosis, high creatinine kinase level, and hypernatremia [4]. It is thought that benzyl alcohol causes direct injury to the central nervous system, but the evidence is lacking [1].
There are several reports of “gasping syndrome” in premature infants in the past, where the symptoms appeared when the blood concentration of benzyl alcohol increased after continuous administration of antimicrobials or after umbilical catheter cleaning [1,2,3, 5]. Reports of acidosis in children and adults are quite rare; Lopez-Herce et al. reported a case of hypotension and high anion gap-opening metabolic acidosis caused by benzyl alcohol added to continuous intravenous diazepam infusion in a 5-year-old girl with seizure aggravation [6]. Smith et al. reported a case of convulsions and respiratory arrest in an adult after intravenous administration of 9000 mg benzyl alcohol, which was added as a preservative to etoposide, during chemotherapy for malignant lymphoma [7]. Another report highlighted a case of an adult intoxicated patient with symptoms of sudden altered mental status, headache, anorexia, metabolic acidosis, hypokalemia, hypophosphatemia, and hyperammonemia associated with renal tubular dysfunction due to inhalation exposure to benzyl alcohol. As mentioned above, the condition is currently characterized by a wide variety of symptoms [8]. In the present case, we postulated that the consciousness disorder and metabolic acidosis were induced by benzyl alcohol because the patient did not have a high body temperature when he was admitted to the previous hospital, so heatstroke could be ruled out, and there was no notable history of illness. However, since hippuric acid is a metabolite of toluene, an organic solvent, inhaled toluene is also excreted in the urine as hippuric acid. Therefore, in this case, the patient was diagnosed with benzyl alcohol poisoning from the components of the exfoliant he used, although toluene poisoning is a differential diagnosis of benzyl alcohol poisoning [4].
However, there is no specific treatment, so systemic management must be performed symptomatically [4]. In the present case, the patient also had a paralytic ileus. This patient had no notable medical history or history of opioid use before onset, there was no active suspicion of infection based on clinical data and findings, and there was no other known cause of paralytic ileus. Therefore, the possibility of poisoning with other ingredients must be considered. The main ingredients of the paint removal agent that the patient had used were benzyl alcohol, hydrogen peroxide, and ethylene glycol. It has been suggested that hydrogen peroxide can cause oxygen gas embolism in the blood vessels due to the decomposition of hydrogen peroxide into oxygen in the bloodstream [9, 10]. However, hydrogen peroxide breaks down quickly in the blood and is a very small molecule, so confirming the diagnosis of hydrogen peroxide poisoning is difficult [11]. In addition, there was no perioral or oral damage in this case, and ethylene glycol is considered to have poor percutaneous absorption. However, we speculated that hydrogen peroxide, ethylene glycol, and other substances, including unknown substances not detected in routine medical practice, combined with benzyl alcohol may have produced a complex toxic effect leading to the development of paralytic ileus and other symptoms. Therefore, since the involvement of hydrogen peroxide could not be ruled out, we maintained FIO2 levels of around 0.3 and avoided high concentrations of oxygen to suppress the formation of free radicals and promote oxygen dissolution.
In cases of industrial product poisoning, there is a possibility of exposure to multiple toxic substances in addition to the main substance, and unexpected symptoms may occur. The present case highlights that benzyl alcohol poisoning should be suspected in patients with paralytic ileus, sudden altered mental status, and metabolic acidosis.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging
- FIO2 :
-
Fraction of inspired oxygen
- PaO2 :
-
Partial pressure of arterial oxygen
References
Gershanik J, Boecler B, Ensley H, McCloskey S, George W. The gasping syndrome and benzyl alcohol poisoning. N Engl J Med. 1982;307:1384–8. https://doi.org/10.1056/NEJM198211253072206.
Brown WJ, Buist NR, Gipson HT, Huston RK, Kennaway NG. Fatal benzyl alcohol poisoning in a neonatal intensive care unit. Lancet. 1982;1:1250. https://doi.org/10.1016/s0140-6736(82)92377-7.
Anderson CW, Ng KJ, Andresen B, Cordero L. Benzyl alcohol poisoning in a premature newborn infant. Am J Obstet Gynecol. 1984;148:344–6. https://doi.org/10.1016/s0002-9378(84)80086-1.
Luke Y. Other alcohols, glycols, and glycol ethers. In: Dart RC, et al., editors. Medical Toxicology. 3rd ed. USA: Lippincott Williams & Wilkins; 2003. p. 1230–2.
Menon PA, Thach BT, Smith CH, Landt M, Roberts JL, Hillman RE, et al. Benzyl alcohol toxicity in a neonatal intensive care unit. Incidence, symptomatology, and mortality. Am J Perinatol. 1984;1:288–92. https://doi.org/10.1055/s-2007-1000023.
López-Herce J, Bonet C, Meana A, Albajara L. Benzyl alcohol poisoning following diazepam intravenous infusion. Ann Pharmacother. 1995;29:632. https://doi.org/10.1177/106002809502900616.
Smith AL, Haider K, Schachtner JM, Mathur S, Vanorden R, Gentile TC. Fatal hemolysis after high-dose etoposide: is benzyl alcohol to blame? Pharmacotherapy. 2001;21:764–6. https://doi.org/10.1592/phco.21.7.764.34567.
Inada M, Kato H, Maruyama H, Okada E, Imai F, Inada S. Toxic benzyl alcohol inhalation: altered mental status with metabolic acidosis and hyperammonemia. Am J Emerg Med. 2022;57(234):e3–5. https://doi.org/10.1016/j.ajem.2022.04.005.
Baharnoori M, Lazarou J. A case of acute cerebral gas embolism due to ingestion of hydrogen peroxide. J Neurol. 2012;259:381–3. https://doi.org/10.1007/s00415-011-6180-0.
Moon JM, Chun BJ, Min YI. Hemorrhagic gastritis and gas emboli after ingesting 3% hydrogen peroxide. J Emerg Med. 2006;30:403–6. https://doi.org/10.1016/j.jemermed.2005.05.036.
Watt BE, Proudfoot AT, Vale JA. Hydrogen peroxide poisoning. Toxicol Rev. 2004;23:51–7. https://doi.org/10.2165/00139709-200423010-00006.
Acknowledgements
The authors would like to thank the paramedical crew who shared the data obtained by them with us and allowed us to use the data in this report. We would like to thank Editage (www.editage.com) for English language editing.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
HF, RK, HO, YK, TY, SY, and SO participated in patient treatment. HF and HO drafted the manuscript. RY revised and edited the manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
In Japan, approval from an ethics committee is not required to report the cases. This case was reported in accordance with ethical guidelines for medical and health research involving human subjects established by the Japanese government.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fukuda, H., Kamidani, R., Okada, H. et al. Complex poisoning mainly with benzyl alcohol complicated by paralytic ileus: a case report. Int J Emerg Med 15, 31 (2022). https://doi.org/10.1186/s12245-022-00434-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12245-022-00434-4