Abstract
Background
Gliomas are aggressive malignant tumors, with poor prognosis. There is an unmet need for the discovery of new, non-invasive biomarkers for differential diagnosis, prognosis, and management of brain tumors. Our objective is to validate four plasma biomarkers – glial fibrillary acidic protein (GFAP), neurofilament light (NEFL), matrix metalloprotease 3 (MMP3) and fatty acid binding protein 4 (FABP4) – and compare them with established brain tumor molecular markers and survival.
Methods
Our cohort consisted of patients with benign and malignant brain tumors (GBM = 77, Astrocytomas = 26, Oligodendrogliomas = 23, Secondary tumors = 35, Meningiomas = 70, Schwannomas = 15, Pituitary adenomas = 15, Normal individuals = 30). For measurements, we used ultrasensitive electrochemiluminescence multiplexed immunoassays.
Results
High plasma GFAP concentration was associated with GBM, low GFAP and high FABP4 were associated with meningiomas, and low GFAP and low FABP4 were associated with astrocytomas and oligodendrogliomas. NEFL was associated with progression of disease. Several prognostic genetic alterations were significantly associated with all plasma biomarker levels. We found no independent associations between plasma GFAP, NEFL, FABP4 and MMP3, and overall survival. The candidate biomarkers could not reliably discriminate GBM from primary or secondary CNS lymphomas.
Conclusions
GFAP, NEFL, FABP4 and MMP3 are useful for differential diagnosis and prognosis, and are associated with molecular changes in gliomas.
Similar content being viewed by others
Introduction
Glioblastoma (GBM, WHO Grade 4) [1] is the most common primary adult brain cancer. Despite the current standard of care, comprised of maximal safe surgical resection, chemotherapy, and radiation, nearly all GBM inevitably recur, with ultimately fatal outcome. At presentation, clinical and imaging indices alone are insufficient for definitively distinguishing GBM from other malignant intra-axial brain tumors, such as astrocytomas, oligodendrogliomas, brain metastases and primary central nervous system lymphomas (PCNSL) [2]. This is an important unmet clinical need since the optimal management of each disease is different. Differential diagnosis necessitates direct tissue acquisition through a neurosurgical procedure. Unfortunately, surgery poses significant risks. Even minimally invasive stereotactic brain tumor sampling has 4–7% risk of major morbidity and 3% mortality. Such complications can increase hospitalization costs by as much as 10% in a disease that is already known to have a significant financial impact on healthcare, the patients, and their families. Given that non-invasive stereotactic radiosurgery has emerged as a viable option for most brain metastases, and that the management of PCNSL is strictly based on chemotherapy and radiation, the added risk of potentially unnecessary surgery should be avoided. In addition, only a small proportion of resected tumors are used for histological testing, which is complicated with inter-observer variability, with as many as 12% of tumors being misdiagnosed [2]. Due to significant intra-tumor heterogeneity [3], these surgical samples also reflect poorly the entire molecular landscape of the tumor, potentially missing detection of currently established prognostic markers (e.g., IDH mutation and MGMT promoter hypermethylation) [4,5,6] and limiting our ability to identify other viable targetable mutations.
In the nearly five decades since randomized, controlled trials first established the benefit of cranial irradiation and carmustine in patients with GBM, the overall survival for afflicted patients has improved by no more than four months [1]. Only two new therapeutic agents have received FDA approval for patients with GBM: one (temozolomide) [4, 5] because it is a less toxic and easier-to-use alkylating agent, and one (bevacizumab) [7] because it improves quality of life but not survival. Although the Tumor Cancer Genome Atlas (TCGA) established three major GBM subtypes, based on transcriptional analysis, this has had limited clinical applicability. Thus far, only IDH mutation and MGMT promoter methylation have established prognostic value [6]. Establishing additional predictive biomarkers for patient stratification strategies for use in developing targeted therapies and identifying determinants of long-term survival of IDH wild-type GBM remain significant challenges.
Tumor heterogeneity [3] influences initial diagnosis and management and remains relevant even during adjuvant therapy, when serial imaging is used to monitor for true tumor recurrence (TTR) versus pseudo-progression (PP; ~15% of cases) or radiation necrosis (RN; ~10% of cases) [8]. Despite advances in imaging modalities, pathological tissue assessment remains the gold standard for distinguishing among these entities, implying that a notable proportion of patients may undergo unnecessary surgery for RN or PP. Short interval follow-up MRI is recommended to distinguish between TTR and PP [9, 10]. Unfortunately, it is not uncommon to observe rapid progression of disease in cases of TTR, at which point enrolment into clinical trials is not feasible due to advanced disease. Thus, it behooves us to develop approaches that help avoid unnecessary surgery and tailor the specific approach based on tumor prognosis when surgery is necessary. Commonly referred to as liquid biopsy, sampling of proximal fluids has offered valuable insight into various systemic cancers as an alternative to tissue biopsy [11, 12].
Considerable efforts have already been undertaken to discover non-invasive, blood-based biomarkers for brain tumor diagnosis, subclassification, prognosis, and treatment response. This need arises, since the standard of care (imaging) is expensive, restricting frequent appointments, and in a proportion of patients, the interpretation of findings is unclear [8]. A plethora of “liquid biopsy” glioma biomarkers have been proposed in the literature [11]. None of them has yet been thoroughly validated or routinely implemented clinically.
Some reported non-invasive glioma biomarkers include extracellular vesicles (EV) [13]. Plasma EV concentration is higher in GBM compared with healthy controls, brain metastases and extra-axial brain tumors. Circulating tumor DNA (ctDNA) is a pan-cancer, non-specific biomarker for many tumors, including gliomas [11, 14, 15]. ctDNA can be isolated from plasma, urine or CSF and subjected to molecular and other analyses, including DNA amount, methylation status and mutational status. This information is valuable for patient diagnosis, prognostication, and management [11, 15]. The method is promising and is used in clinical trials but is expensive (~$1,500 per sample), slow and technically demanding. The value of ctDNA for early diagnosis is currently debated, especially for brain tumors, which release less ctDNA in the circulation than other tumors [16].
Many other individual serum/plasma or CSF protein or nucleic acid biomarkers have been tried for glioma differential diagnosis, prognosis, and therapy response. Prominent among them are glial fibrillary acidic protein (GFAP) [17,18,19], neurofilament light (NEFL) [20], laminin-5, fibronectin, Type IV collagen, circulating microRNAs; secreted markers of inflammatory response, namely interleukin-6, tumor necrosis factor-α, interferon-γ and kynurenine; and the proliferation markers human telomerase, reverse transcriptase, and microtubule-associated-protein-Tau [19]. Such studies promise to develop and evaluate a non-invasive panel of secreted biomarkers using liquid biopsy [15, 18, 21, 22] for evaluating disease progression, to accomplish a clinical translation.
Despite the current plethora of candidate glioma non-invasive biomarkers, very few, if any, are used routinely, because of their low clinical sensitivity and specificity, high cost and the lack of evidence that they can contribute to improved patient survival or quality of life. In our previous work, we have undertaken the task of using new technology, the proximity extension assay (PEA) [23], to quantitatively profile for the first time ~ 3,000 proteins in plasma of glioma and other brain malignancies to confirm (GFAP, NEFL) and discover additional glioma biomarkers, which, individually or as a small panel, could assist in glioma patient management [24]. We hypothesized that a small panel of non-invasive serum/plasma biomarkers can aid in the optimal management of patients with brain tumors, in combination with current imaging modalities (CT, MRI).
In this paper, we used a different analytical technology (ultrasensitive electroluminescent immunoassay instead of PEA) and an independent, more diverse, and larger cohort of patients, to validate GFAP, NEFL, matrix metalloprotease 3 (MMP3) and fatty acid-binding protein 4 (FABP4), as non-invasive biomarkers of benign and malignant primary and secondary brain tumors. More specifically, we sought to validate our original findings [24], identify additional associations between plasma biomarker levels and molecular characteristics, explore the possibility of differential diagnosis based on the four biomarkers of interest, establish an association between clinical outcomes and biomarker levels (including overall survival), and explore the possibility of differential diagnosis between GBM and primary and secondary CNS lymphomas.
Materials and methods
Experimental design and inclusion criteria
Plasma samples from benign and malignant brain tumors were provided by the Northwestern University Brain Tumor Biobank. Plasma samples from apparently healthy individuals were obtained from volunteers working at the University Health Network (UHN), Toronto, Ontario, Canada. These samples included both sexes. The inclusion criteria incorporated plasma samples that were collected from patients that were histologically- and imaging-confirmed for various malignant and benign tumors before surgical intervention, as well as healthy control individuals. Our protocols were approved by the Institutional Review Boards of Northwestern University and UHN. Since our series of patients represent a retrospective cohort, glioma patients were categorized by using the old and the new WHO classification system, as appropriate [25]. We used these classification systems to compare the current data with our previous discovery data, and in particular, we focused on the new classification system [24]. According to the old WHO classification system, the following categories were included: (N = number of samples in brackets): Glioblastoma multiforme (astrocytoma grade 4; N = 71), astrocytoma grade 2 (N = 13), astrocytoma grade 3 (N = 19), oligodendroglioma, grade 2 (N = 10), oligodendroglioma, grade 3 (N = 13), pituitary adenoma (N = 15), Schwannoma, grade 1 (N = 15) meningioma, grade 1 (N = 45), meningioma, grade 2 (N = 25), metastatic adenocarcinoma to CNS (with primary sites in brackets) (colorectal; N = 5) (breast; N = 10), (lung; N = 10), (melanoma; N = 10), primary brain lymphoma (N = 9), secondary brain lymphoma (N = 7) and normal individuals (N = 30). The new classification system [25] is mainly based on molecular indices. The following categories were included (N = number of samples in brackets): GBM, gliomas with wild-type IDH (N = 77), gliomas with IDH mutant and no 1p19q co-deletion (astrocytomas; N = 26), gliomas with mutant IDH and 1p19q co-deletion (oligodendrogliomas; N = 23). For each analysis in the Results section, we indicate which categories of patients and classification systems were used. The samples were analyzed in a randomized fashion and the code was broken after the analysis was completed.
Although power calculations were not performed, we decided to increase the power of the statistical analyses, in some cases by combining patients with astrocytoma grades 2 and 3 (N = 32) and oligodendrogliomas grades 2 and 3 (N = 23). In other analyses, we combined all benign tumors together (pituitary adenomas, Schwannomas grade 1, meningiomas grade 1, and meningiomas grade 2) (N = 100).
Statistical analysis
Patient characteristics were summarized using descriptive statistics: tallies are presented with number (%) for categorical variables. Means (with standard deviations, sd) and medians (with intra-quartile ranges, IQR) are reported for continuous attributes.
Logarithmic transformations: Histograms of the four immunoassay-derived plasma protein levels revealed skewed distributions. Consequently, log transformations have been applied to the biomarker values to obtain near-normal distributions.
Comparison of Olink and immunoassay data: The original Olink assay data for the four candidate biomarkers of interest, presented in our previous manuscript [24], were compared with the Meso Scale Discovery® (MSD) immunoassay data for 50 samples with both data available (Supplementary Fig. 2). Scatterplots were drawn, comparing the protein concentrations between the two methods. Spearman’s rank correlation was calculated as an indicator of the strength of the agreement, with a high correlation coefficient for each marker (Supplementary Fig. 2). The immunoassay from MSD had a lower range for GFAP and NEFL, and thus, saturation was observed, which lowered the r value to a still acceptable value (r = 0.91, r = 0.90 for GFAP and NEFL respectively).
Validation of data of previous findings: We replicated our original findings [24] (Olink data) with the present data (immunoassay) to identify gliomas and meningiomas using FABP4 and GFAP levels utilizing (1) thresholds that achieve 100% specificity, (2) using logistic regression. Because the immunoassay and Olink values do not use the same analytical units, we identified method-specific thresholds. We then evaluated the performance (sensitivity, specificity, area under the curve (AUC)) of the models based on these thresholds.
Assay reproducibility: Since we had only four patients with repeat analyses (due to plasma volume depletion), no statistical analysis was performed for assay reproducibility, but the repeat observations were plotted onto the protein concentration distributions, to provide a visual semi-quantitative assessment of the assay precision.
Biomarkers and patient characteristics
Exploratory analyses were conducted to determine if biomarker levels were associated with age, sex, or ethnicity for the entire sample (n = 291) as well as the subset of patients with glioma (n = 126). Scatterplots and Spearman correlation coefficients were calculated for each biomarker according to age. For sex and ethnicity, \({\chi }^{2}\) tests were performed.
Genetic variables and biomarker concentrations
Genetic mutation status was available from the Northwestern University Biobank for the subset of patients with glioma (n = 126). There was a single patient with EGFR VIII status who was not included in the analysis. In our study, t tests were used to determine if there were differences in biomarker concentrations between the following genetic variants: IDH1(wild-type vs. mutant), ATRX expression (retained or lost), P53 NGS (wild-type or mutant), EGFR (wild-type vs. mutant), MGMT promoter methylation (positive or negative), TERT promoter (wild-type or mutant), CDKN2A (wild-type or lost), 1p19q co-deletion (negative or positive) and NF1 (wild-type or mutant). Boxplots were created to display the differences in numerical or categorical variables.
Diagnosis and grade and biomarker concentrations
Plots of the biomarker concentrations as a function of diagnostic category and WHO grade were created. For a subset of glioma patients, multivariable linear regression models were used to explore the effect of diagnostic category and WHO grade on biomarker concentrations.
Association between biomarker concentration and survival
Since the four biomarker concentrations vary by diagnostic category, and diagnosis is predictive of overall survival, an exploration of the association between biomarker concentration and survival was conducted within diagnostic groups for three diagnostic categories: GBM (wild-type IDH), meningioma and secondary tumors (tumors that metastasized to the brain); these categories were chosen because each subgroup had at least five recorded deaths. Initially, Cox proportional hazards models were fit, but the proportional hazards assumption was not met for several biomarker/diagnostic combinations; consequently, simple Kaplan-Meier survival curves were drawn, using the median as cut-off.
All analyses were conducted using the R statistical programming language version 4.2.2 [26].
Meso Scale Discovery (MSD) assays
MSD’s combination of electroluminescence and multianalyte immunoassay technology provides exceptional sensitivity and multiplex functionality, making it a highly useful analytical immunoassay system. For more descriptions of the MSD assays and their applications, please refer to our previous publications [23, 27,28,29] and the manufacturer’s website (www.mesoscale.com). The MSD assay characteristics that apply to the four assays used are as follows: The analytical sensitivity (limit of detection, LOD) is 2–4 pg/mL. Precision is generally < 15% and all plasma samples were measured in duplicate. Concentrations above the upper end of the assay range (upper limit of quantification, ULOQ) were assigned the ULOQ concentration. The assays are devoid of any known interferences.
Demographic variables
Supplementary Table 2 summarizes the patient demographic characteristics. The subject information was blinded prior to analysis. The age, sex, and ethnicity of the 291 patients was recorded.
Results
Biomarker distributions
The distributions of plasma concentrations of the four candidate biomarkers GFAP, NEFL, MMP3 and FABP4 among all patients are shown in Supplementary. All proteins have skewed distributions (not shown) but after logarithmic transformation, the distributions become near normal.
Separation of various brain tumors by using a combination of plasma GFAP and FABP4. Our preliminary findings [22] have been replicated using MSD immunoassay, instead of Olink PEA technology. (A): 100% specificity threshold. All patients with GFAP < 226 pg/mL (vertical dotted line) and FABP4 > 7,736 pg/mL (horizontal dotted line) had meningioma (blue dots), with 53% sensitivity to detect glioma. (B): Logistic regression model with 64% specificity and 84% sensitivity for meningiomas and gliomas, respectively (shown is the separating dotted line). Cases for whom the diagnosis has changed under the new WHO classification are highlighted with circles, indicating a GBM with wild-type IDH, previously categorized as astrocytoma. Squares indicate astrocytomas with IDH mutation, previously [22] classified as GBM. For more discussion see text
Comparison of Olink PEA assays and MSD immunoassays
In our previous biomarker discovery investigation, we used Olink analytical technology (PEA) to quantify plasma GFAP, NEFL, MMP3 and FABP4, in addition to another 3,000 proteins. The concentrations of all proteins are expressed in relative quantification (NPX) values [23]. In the present validation study, we quantified the 4 proteins in plasma with specific, sensitive, precise, and quantitative MSD® multiplexed immunoassays. For 50 plasma samples, we paired Olink and immunoassay results for comparison (Supplementary Fig. 2).
The Spearman rank-order correlation coefficients are shown in the bottom-right corner of each plot. The agreement is generally good, except when GFAP and NEFL values exceed the ULOQ and were assigned the ULOQ concentration.
Validation of our previous findings
We previously found [24] that high plasma GFAP was associated with GBM, low GFAP and high FABP4 were associated with meningiomas and low GFAP and low FABP4 were associated with astrocytomas. For this independent validation study, the samples considered were from patients with similar final diagnoses in the new set of patients (N = 196) as shown in Supplementary Table 1 (we used pre 2021 and post 2021 WHO glioma classification).
Analysis of the data was accomplished with two different methods as follows:
Method 1
Analytical parameter cutoffs were set at 100% specificity for separating meningiomas from gliomas. As shown in Fig. 1 panel A, all patients with meningiomas had GFAP < 226 pg/mL and FABP4 > 7,736 pg/mL. The two-marker (GFAP/FABP4) combination model performance was as follows: at 100% specificity (where all 70 meningiomas were correctly predicted to be meningiomas), the sensitivity for glioma detection was 53%, the positive predictive value (PPV) for meningioma detection was 1.00, the negative predictive value (NPV) was 0.54, and the accuracy was 70%. Oligodendrogliomas grade 2 and 3 and astrocytomas grade 2 and 3, in general, exhibited low FABP4 and low GFAP values. These data are in accordance with those of our previous, smaller study [24].
Method 2
Logistic Regression. A logistic regression model was fitted combining GFAP and FABP4 (Fig. 1 panel B). With this model, at 64% specificity (among 70 meningiomas 25 were misclassified as gliomas), the sensitivity for glioma detection is 84% (20 gliomas were misclassified as meningiomas). The PPV was 0.81, the NPV was 0.69, and the overall accuracy was 77%.
These data are in accordance with our previous findings [24], summarized as follows: High GFAP was associated with GBM, low GFAP and high FABP4 were associated with meningiomas grade 1 and 2 and low GFAP and low FABP4 were associated with astrocytomas grade 2 and 3 (mutant IDH, no 1p19q co-deletion) and oligodendrogliomas grade 2 and 3 (mutant IDH with 1p19q co-deletion).
Assay reproducibility
The manufacturer-stated analytical reproducibility of the four utilized MSD assays is < 15%. We have limited data (only two replicates for plasma samples from 4 patients) to systematically examine reproducibility, due to patient sample depletion. Consequently, no extensive reproducibility statistics have been calculated. Instead, for the four biomarkers of interest, the available replicates are shown by super-imposing them on the full cross-sectional data (all values are log-transformed). The color of the dots and the y-axis positioning are the same for each patient with multiple assay values (see Supplementary Fig. 3). In most cases with available duplicates, the assay values are similar, and the y-axis positioning are the same for each of the four patients with duplicate assay values. Where only a single dot is visible, the values of both replicates are identical. For most samples with duplicate values, the concentrations are similar. Due to the small number of replicates (the reason being plasma sample depletion) statistical analyses were not done. For more comments see text.
Age and protein concentrations
All 291 patients with age information were included. The data are presented in Supplementary Fig. 4. Age is positively, but weakly, correlated with all four protein concentrations. The Spearman correlation coefficient ranged from 0.26 to 0.47 and it is shown on top of each graph.
Effect of patient sex
The effect of patient sex on plasma protein concentrations are presented in Supplementary Tables 3 and graphically in Supplementary Fig. 5. Three proteins (GFAP, MMP3, NEFL) are higher in males and one protein (FABP4) is higher in females. All patients with sex information were included.
Effect of ethnicity
The effect of ethnicity on plasma biomarker concentrations is shown in Supplementary Tables 4 and graphically in Supplementary Fig. 6. In general, Blacks have the highest plasma biomarker values and White Hispanics the lowest, but the differences are small.
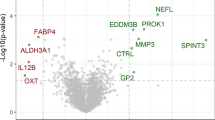
Genetic variables and biomarker concentrations
We used a retrospective cohort of samples from a biobank, collected over many years, and not all genetic changes are reported for all patients. Values not reported were re-coded as missing. For EGFR status there was a single patient with EGFR VIII; this patient was not included in the comparisons. Despite several tests indicating statistical significance between protein concentrations and genetic changes, the magnitude of the differences is relatively small. (See Supplementary Tables 5 and graphically in Fig. 2, below). Note that these data have not been adjusted for multiple comparisons, because our main purpose was to determine if these factors should be incorporated into a diagnostic model.
Comparison of genetic and proteomic markers. Genetic markers of gliomas and their relationship to plasma concentrations of the four biomarkers shown (FABP4, GFAP, MMP3, NEFL). The figure shows the median (horizontal lines), and interquartile range. Means are indicated with an ‘x’. Significance levels for independent t tests are shown at the top of each plot and have not been adjusted for multiple comparisons. Despite several differences indicating statistical significance, these differences are generally small. For more details of patient genetic status see also Supplementary Table 5. For GFAP, the most important differences (P = < 0.01) were between GFAP and IDH1 status, ATRX expression, MGMT promoter methylation, TERT promoter mutation, and CDKN2A/B p16 and 1p/19q co-deletion
Descriptive plots
In Fig. 3, we present scattergrams showing the four biomarker concentrations for each patient group, and according to tumor grade. There is significant overlap between biomarker values for all shown patient groups. In general, the highest levels of the biomarkers are seen in GBM, except FABP4 which is higher in meningiomas vs. gliomas.
Scattergrams of the four protein plasma concentrations (FABP4, GFAP, MMP3, NEFL) by diagnostic groups. Oligo = Oligodendroglioma IDH mut/1p19q co-deletion, Astro = Astrocytoma IDH mut, no 1p19q co-deletion, GBM = GBM wild-type IDH, Secondary = secondary tumors, Adenoma = pituitary adenoma, Schwannoma = Schwannoma, grade 1. For each diagnostic group the patients are stratified by WHO grade along the x-axis with different symbols. For more comments see text. Number of samples per category can be found in Supplementary Tables 1 and 2
WHO grade and glioma subclass
In our sample set, WHO grade is associated with the diagnostic category, with most grade 4 patients diagnosed with GBM wild-type IDH (Supplemental Table 6). We do not have sufficient sample sizes to perform sub-group analyses within grade or diagnostic category, to properly investigate whether biomarker levels are associated primarily with disease type or with disease severity. Instead, we have attempted to estimate the relative importance of diagnosis and grade on biomarker levels by undertaking multiple linear regression to estimate protein levels from diagnostic category and WHO grade. For each of the four biomarkers of interest, we fit a multivariable model with both diagnosis and grade, and separate models for each predictor. The unique contribution to R2 was then equal to total R2 less R2, without the predictor of interest. Supplemental Table 7 summarizes the findings and indicates that WHO grade is the most important predictor of protein levels in this sample. This has important implications for future work; longitudinal studies of early-stage patients will be necessary to determine if protein levels are diagnostic, prognostic or both.
The effect of WHO grade on the values of the four biomarkers is further shown graphically in Fig. 3.
We investigated the correlations of each biomarker with the other three biomarkers in the various diagnostic groups. An example is shown in Fig. 4, which includes all diagnostic groups. For all comparisons (not all data are shown) the strongest correlations were between NEFL and GFAP, with Spearman correlation coefficients (r) in the range of 0.7. For the other comparisons between the biomarkers the Spearman correlation coefficient was lower (Fig. 4).
Correlation between the four markers for various patient groups. Correlation between the four biomarkers for GBM (n = 77), astrocytoma with mutant IDH no 1p19q co-deletion (n = 26), oligodendroglioma mutant IDH with 1p19q co-deletion (n = 23), secondary tumors (n = 35), meningioma (n = 70), Schwannoma (n = 15), pituitary adenoma (n = 15) and normal controls (n = 30). Spearman correlation is shown on the right bottom corner of each plot. NEFL shows the strongest correlation with GFAP (r = 0.74). The reported Spearman correlations were calculated by including all patient groups
Survival and biomarker concentrations
To explore associations between plasma protein levels and overall survival we examined survival status within each diagnostic category. While this limited the sample size, it also removed confounding due to the diagnostic category (the latter is independently associated with survival). Initially, Cox proportional hazards models were fit to investigate the effect of protein levels on survival, but the proportional hazards assumptions were often violated. So, for this exploratory work, which should be considered hypothesis-generating, we chose to examine Kaplan-Meier curves, splitting the sample at the median protein level. Analysis was limited to the three patient groups with a minimum of five observed deaths: GBM wild-type IDH, meningioma and secondary tumors. Data for GBM are shown in Fig. 5 and for the other two groups in Supplementary Figs. 7 and 8.
Survival analysis. Survival analysis (Kaplan-Meier plots) of patients with GBM, divided into high (blue crosses) or low (red crosses) plasma GFAP, NEFL, MMP3 and FABP4 level. The median of each protein concentration was used as a cut-off. Cut-offs are shown after log transformation, along with the p value, calculated by the log-rank test. Only patients with high FABP4 have significantly lower survival (p = 0.025)
Longitudinal plots
For 24 patients we had plasma collected at both diagnosis and recurrence. We compared these two values to obtain a preliminary estimate of their changes during progression. We found that on average, values tend to be higher at recurrence, but not for all patients. For FABP4 and MMP3 no changes > 50% in either direction were seen. For GFAP one patient had a > 50% decrease at recurrence and 3 patients had > 50% increase at recurrence. For NEFL, four patients had > 50% increase at recurrence (Supplementary Fig. 9). All other patients had changes of < 50% in magnitude.
Discussion
One of the unmet clinical needs in the area of brain tumors is the discovery and validation of non-invasive biomarkers and other technologies which can assist in optimal patient management. These tools could help in disease differential diagnosis, prognosis, monitoring the success of treatments, and facilitate early inclusion of patients in clinical trials, as new therapies become available. In addition to the valuable, but expensive and slow, imaging technologies, methods based on liquid biopsy, utilizing serum or plasma, could have important complementary clinical utility. Recently, we used a new, powerful proteomic technology, PEA (Olink Proteomics), to simultaneously quantify about 3,000 plasma proteins in patients with gliomas and meningiomas (as controls) [24]. Among all proteins, a few had discriminatory potential between gliomas and meningiomas. In this paper, we validated our previous findings for the 4 most promising candidate biomarker proteins (GFAP, NEFL, MMP3 and FABP4) and extended our previous observations by using a larger and more diverse set of well-characterized samples from benign and malignant primary and secondary brain tumors.
In our previous work we analyzed plasma samples by the PEA technology [23] collected from glioma patients of various WHO grades before therapy initiation and compared the results with age- and sex-matched patients with meningiomas. In the current work, we used an orthogonal quantification technology (MSD electroluminescence immunoassays), to simultaneously quantify the four proteins in plasma, (GFAP, NEFL, MMP3 and FABP4), and examined their value as diagnostic and prognostic markers. The MSD assays used are more economical than PEA, sensitive, specific, quantitative, and more precise, requiring small plasma volumes, and they are ideal for a large-scale validation of biomarkers. The four selected biomarkers for validation were chosen for their performance in the discovery phase and their link to brain tumors.
The four candidates, GFAP [30,31,32,33,34], NEFL [35, 36], MMP3 [37,38,39] and FABP4 [40,41,42,43] have previously been associated with brain tumors in small studies and have also been shown to be elevated in plasma and cerebrospinal fluid (CSF) of patients with other brain disorders, including traumatic brain injury, neurodegeneration, multiple sclerosis, etc [44,45,46,47,48]. The non-specificity of our markers for brain tumors is a clear disadvantage, but the clinical presentation of these brain disorders is sufficiently different from brain tumors. Additionally, our biomarkers will likely find more clinical applicability during management of already diagnosed brain tumors.
In this study, we found several new associations between patient clinicopathological features and the four candidate plasma biomarkers. As in the previous study, we found that GFAP, as compared to the other three proteins, had the highest discriminatory potential between gliomas and meningiomas. The combination of two markers (GFAP and FABP4) further enhances the discrimination between gliomas and meningiomas (Fig. 1).
The putative functional role of GFAP in astrocytes (the main type of glial cells in the central nervous system (CNS)) was previously reported [46]. GFAP is involved in numerous astrocyte functions. In the early stages of recovery following brain surgery, GFAP increases in response to astrocytic reaction to brain injury [49].
Convincing evidence supports the involvement of GFAP in GBM. Serum GFAP was significantly increased in WHO grade 4 glioma (GBM) and was detected in 63% of all grade 4 patients compared to 13% of healthy controls [31, 50], , suggesting that glioma patients have elevated plasma GFAP, in accordance with our findings. (Fig. 3). Serum GFAP correlates with invasiveness in astrocytomas and high-grade gliomas, compared to lower grade gliomas. Thus, GFAP represents a potential prognostic biomarker and a candidate therapeutic target for gliomas [51].
Another well-known glioma biomarker is NEFL (neurofilament light polypeptide) also known as neurofilament light chain, a potential tumor suppressor [20]. NEFL is involved in a variety of common human cancers such as breast, prostate, and head and neck cancers. Plasma NEFL concentration was higher in patients with CNS tumors with disease in progression versus CNS tumors with stable disease. In addition, plasma NEFL was higher in patients with metastatic solid tumors with known brain metastases than in those with metastatic tumors with no brain metastases [52]. As such, NEFL is also a prognostic marker of brain tumors.
FABP4 is one of ten intracellular small molecular weight proteins that belong to the FABP family and is found in adipose tissue, peripheral macrophages, and microglia but not in normal brain blood vessels, although it has been found in certain endothelial cells or tumor cells in benign and malignant meningiomas. FABP4 could have a role in carcinogenesis in meningiomas by stimulating cell proliferation in a cell type-independent way [41, 42]. In this connection, rapamycin, a well-known inhibitor of the mTOR pathway, which is a master regulator of cell growth and metabolism, inhibits FABP4 production by endothelial cells. FABP4 is expressed in a significantly higher percentage of GBMs in comparison to both normal brain tissues and lower-grade glial tumors. Other data suggest that FABP4 may play a role in angiogenesis associated with GBMs. Another study analyzed FABP4 expression in a cohort of paraffin-embedded meningioma specimens by immunohistochemistry and double immunofluorescence analyses. These results demonstrate that FABP4 is commonly expressed in meningioma vascular endothelial cells while tumor cell expression of FABP4 is primarily observed in anaplastic meningiomas. A combination of FABP4 immunostaining with histopathologic grading might provide a more accurate prediction of the biological behavior of meningiomas than histopathologic grading alone.
MMP3 plays a role in cell migration. Platelet-derived growth factor receptor-alpha (PDGFR-alpha) induces MMP3 gene expression and increased cell proliferation and cell migration upon stimulation by PDGF. The induction of expression of MMP3 in glioblastoma cells triggers a cascade of gene expression events, resulting in decreased cell adhesion and migration [37].
Among our new findings, we report for the first time the dependence of the plasma concentration of these candidate biomarkers on genetic changes frequently seen in gliomas (Fig. 2). In general, mutations that are associated with better patient prognosis are associated with lower levels of the four biomarkers in plasma. This observation may be clinically useful. Tumors with late-stage disease (grade 4) are usually associated with higher levels of these proteins in plasma (Fig. 3). However, protein levels were not significantly associated with overall patient survival (Fig. 5 and Supplementary Figs. 7 and 8), presumably due to the small number of patients and to the rather short follow-up time. Pairwise plots have shown that among the four proteins, the strongest correlation was seen between GFAP and NEFL. (Fig. 5).
Primary and secondary CNS lymphomas are relatively rare brain tumors, and our lymphoma cohort is rather small and does not allow for definitive conclusions (data not shown). However, we found qualitative evidence that lymphomas demonstrate variable levels of the four proteins, with high overlap between the patient groups (gliomas and lymphomas). From these data (which were not included in this paper) we conclude that these four biomarkers cannot discriminate primary or secondary lymphomas from GBM, even if the levels of GFAP are, in general, higher in GBM in some cases.
Patients from whom we had two samples, at diagnosis and at relapse (Supplementary Fig. 9), showed a trend for increase of the four biomarkers with time. Although we could not confidently conclude from these limited data, we speculate that changes in these biomarkers with time, and their possible correlation with tumor progression, may qualify these proteins as non-invasive, cheap, and fast tools for monitoring patients with brain tumors, including assessment of the effectiveness of new therapeutic agents. To this end, we are currently prospectively recruiting patients to establish the monitoring value of these four biomarkers in brain tumors.
Limitations
Our study is retrospective and the provision of the samples by a Biobank may be associated with sample collection and storage bias. Our primary and secondary brain lymphoma cases are few due to the relative rarity of these conditions. Our biomarkers may perform well for the intended application (aid in diagnosis and management) but they may not contribute towards better patient survival, quality of life or selection of treatments.
Data availability
The excel file with the concentrations of the four biomarkers, as well as the anonymized clinical information are available by request from the corresponding author (EPD).
Abbreviations
- GBM:
-
Glioblastoma
- PCNSL:
-
Primary Central Nervous System Lymphomas
- IDH:
-
Isocitrate Dehydrogenase
- MGMT:
-
O(6)-Methylguanine-DNA Methyltransferase
- TCGA:
-
Tumor Cancer Genome Atlas
- TTR:
-
True Tumor Reoccurrence
- PP:
-
Pseudo-Progression
- RN:
-
Radiation Necrosis
- EV:
-
Extracellular Vesicles
- ctDNA:
-
circulating tumor DNA
- GFAP:
-
Glila Fibrillary Acidic Protein
- NEFL:
-
Neurofilament Light
- PEA:
-
Proximity Extension Assay
- MMP3:
-
Matrix Metalloprotease 3
- FABP4:
-
Fatty Acid-Binding Protein 4
- UHN:
-
University Health Network
- IQR:
-
Intra-Quartile Range
- MSD:
-
Meso Scale Discovery®
- AUC:
-
Area Under The Curve
- EGFR:
-
Epidermal Growth Factor Receptor
- ATRX:
-
Alpha-Thalassemia mental Retardation X-linked
- NGS:
-
Next Generation Sequencing
- TERT:
-
Telomerase Reverse Transcriptase
- CDKN2A:
-
Cyclin-Dependent Kinase Inhibitor 2 A
- NF1:
-
Neurofibromatosis type 1
- LOD:
-
Limit Of Detection
- ULOQ:
-
Upper Limit Of Quantification
- NPX:
-
Normalized Protein Expression
- PPV:
-
Positive Predictive Value
- NPV:
-
Negative Predictive Value
- CSF:
-
Cerebrospinal Fluid
- mTOR, PDGFR-alpha:
-
Platelet-Derived Growth Factor Receptor- alpha
References
Weller M, Wick W, Aldape K, Brada M, Berger M, Pfister SM, et al. Glioma Nat Rev Dis Primer. 2015;1(1):1–18.
Zuccato JA, Patil V, Mansouri S, Voisin M, Chakravarthy A, Shen SY, et al. Cerebrospinal fluid methylome-based liquid biopsies for accurate malignant brain neoplasm classification. Neuro-Oncol. 2023;25(8):1452–60.
Petrilli LL, Fuoco C, Palma A, Pasquini L, Pericoli G, Grabovska Y, et al. Inter and intra-tumor heterogeneity of paediatric type diffuse high-grade gliomas revealed by single-cell mass cytometry. Front Oncol. 2022;12:1016343.
Omuro A, Brandes AA, Carpentier AF, Idbaih A, Reardon DA, Cloughesy T, et al. Radiotherapy combined with nivolumab or temozolomide for newly diagnosed glioblastoma with unmethylated MGMT promoter: an international randomized phase III trial. Neuro-Oncol. 2023;25(1):123–34.
Rong L, Li N, Zhang Z. Emerging therapies for glioblastoma: current state and future directions. J Exp Clin Cancer Res. 2022;41(1):142.
Richardson LG, Miller JJ, Kitagawa Y, Wakimoto H, Choi BD, Curry WT. Implications of IDH mutations on immunotherapeutic strategies for malignant glioma. Neurosurg Focus. 2022;52(2):E6.
Park JH, Lee HS, Choi JW, Lim SD, Koh HK, Cho KR, et al. Clinical Benefit of Bevacizumab and Irinotecan (BEV + IRI) in patients with Relapsed/Refractory glioblastoma (r/rGBM) and its potential predictors. Anticancer Res. 2022;42(12):6091–8.
Stock A, Hancken CV, Kandels D, Kortmann RD, Dietzsch S, Timmermann B, et al. Pseudoprogression is frequent after Front-Line Radiation Therapy in Pediatric Low-Grade Glioma: results from the German low-Grade Glioma Cohort. Int J Radiat Oncol Biol Phys. 2022;112(5):1190–202.
Liao D, Liu YC, Liu JY, Wang D, Liu XF. Differentiating tumour progression from pseudoprogression in glioblastoma patients: a monoexponential, biexponential, and stretched-exponential model-based DWI study. BMC Med Imaging. 2023;23(1):119.
Weller M, van den Bent M, Tonn JC, Stupp R, Preusser M, Cohen-Jonathan-Moyal E, et al. European Association for Neuro-Oncology (EANO) guideline on the diagnosis and treatment of adult astrocytic and oligodendroglial gliomas. Lancet Oncol. 2017;18(6):e315–29.
Alix-Panabières C, Pantel K. Liquid Biopsy: from Discovery to Clinical Application. Cancer Discov. 2021;11(4):858–73.
Bauman MMJ, Bouchal SM, Monie DD, Aibaidula A, Singh R, Parney IF. Strategies, considerations, and recent advancements in the development of liquid biopsy for glioblastoma: a step towards individualized medicine in glioblastoma. Neurosurg Focus. 2022;53(6):E14.
Osti D, Del Bene M, Rappa G, Santos M, Matafora V, Richichi C, et al. Clinical significance of Extracellular vesicles in plasma from Glioblastoma patients. Clin Cancer Res. 2019;25(1):266–76.
Fiala C, Kulasingam V, Diamandis EP. Circulating Tumor DNA for early Cancer detection. J Appl Lab Med. 2018;3(2):300–13.
Corcoran RB, Chabner BA. Application of cell-free DNA analysis to Cancer Treatment. N Engl J Med. 2018;379(18):1754–65.
Fiala C, Diamandis EP. Utility of circulating tumor DNA in cancer diagnostics with emphasis on early detection. BMC Med. 2018;16(1):166.
Radu R, Petrescu GED, Gorgan RM, Brehar FM, GFAPδ:. A Promising Biomarker and Therapeutic Target in Glioblastoma. Front Oncol [Internet]. 2022 [cited 2022 Nov 9];12. https://www.frontiersin.org/articles/https://doi.org/10.3389/fonc.2022.859247.
van Asperen JV, Fedorushkova DM, Robe PAJT, Hol EM. Investigation of glial fibrillary acidic protein (GFAP) in body fluids as a potential biomarker for glioma: a systematic review and meta-analysis. Biomark Biochem Indic Expo Response Susceptibility Chem. 2022;27(1):1–12.
Ali H, Harting R, de Vries R, Ali M, Wurdinger T, Best MG. Blood-based biomarkers for glioma in the context of gliomagenesis: a systematic review. Front Oncol. 2021;11:665235.
Hepner A, Porter J, Hare F, Nasir SS, Zetterberg H, Blennow K, et al. Serum neurofilament light, glial fibrillary acidic protein and tau are possible serum biomarkers for activity of Brain metastases and Gliomas. World J Oncol. 2019;10(4–5):169.
Shrivastava R, Gandhi P, Gothalwal R. The road-map for establishment of a prognostic molecular marker panel in glioma using liquid biopsy: current status and future directions. Clin Transl Oncol off Publ Fed Span Oncol Soc Natl Cancer Inst Mex. 2022;24(9):1702–14.
Yadav N, Mishra K, B C AK, Singh D, Subberwal M. Clinical utility of serum glial fibrillary acidic protein in glial neoplasm. Surg Neurol Int. 2022;13:601.
Ren AH, Diamandis EP, Kulasingam V. Uncovering the depths of the human proteome: antibody-based technologies for Ultrasensitive Multiplexed protein detection and quantification. Mol Cell Proteom MCP. 2021;20:100155.
Ghorbani A, Avery LM, Sohaei D, Soosaipillai A, Richer M, Horbinski C, et al. Discovery of novel glioma serum biomarkers by proximity extension assay. Clin Proteom. 2023;20(1):12.
Berger TR, Wen PY, Lang-Orsini M, Chukwueke UN. World Health Organization 2021 Classification of Central Nervous System Tumors and implications for Therapy for adult-type gliomas: a review. JAMA Oncol. 2022;8(10):1493–501.
R Core Team. R: A Language and Environment for Statistical Computing [Internet]. Vienna, Austria: R Foundation for Statistical Computing: R Core Team. 2022. https://www.R-project.org/.
Ren AH, Soosaipillai A, Mathew A, Nikolenko G, Sardesai L, Stengelin M, et al. Utility of a fifth-generation ultrasensitive prostate-specific Antigen assay for monitoring prostate Cancer patients after Radical Prostatectomy with 3 years of Follow-Up. Clin Chem. 2020;66(10):1329–38.
Eklund E, Diamandis EP, Muytjens C, Wheeler S, Mathew A, Stengelin M, et al. Serum complexed and free prostate specific antigen levels are lower in female elite athletes in comparison to control women. F1000Research. 2017;6:1131.
Diamandis EP, Stanczyk FZ, Wheeler S, Mathew A, Stengelin M, Nikolenko G, et al. Serum complexed and free prostate-specific antigen (PSA) for the diagnosis of the polycystic ovarian syndrome (PCOS). Clin Chem Lab Med. 2017;55(11):1789–97.
Gandhoke C, Shah A, Singh D, Subberwal M, Gupta R, Gupta V, et al. Whether serum glial fibrillary acidic protein (GFAP) can be used as a diagnostic biomarker in patients with Glioblastoma? MAMC J Med Sci. 2020;6(1):27–27.
Baumgarten P, Quick-Weller J, Gessler F, Wagner M, Tichy J, Forster MT, et al. Pre- and early postoperative GFAP serum levels in glioma and brain metastases. J Neurooncol. 2018;139(3):541–6.
Tichy J, Spechtmeyer S, Mittelbronn M, Hattingen E, Rieger J, Senft C, et al. Prospective evaluation of serum glial fibrillary acidic protein (GFAP) as a diagnostic marker for glioblastoma. J Neurooncol. 2016;126(2):361–9.
Vietheer JM, Rieger J, Wagner M, Senft C, Tichy J, Foerch C. Serum concentrations of glial fibrillary acidic protein (GFAP) do not indicate tumor recurrence in patients with glioblastoma. J Neurooncol. 2017;135(1):193–9.
Zottel A, Jovčevska I, Šamec N, Komel R. Cytoskeletal proteins as glioblastoma biomarkers and targets for therapy: a systematic review. Crit Rev Oncol Hematol. 2021;160:103283.
Lin X, Lu T, Deng H, Liu C, Yang Y, Chen T, et al. Serum neurofilament light chain or glial fibrillary acidic protein in the diagnosis and prognosis of brain metastases. J Neurol. 2022;269(2):815–23.
Wang ZY, Xiong J, Zhang SS, Wang JJ, Gong ZJ, Dai MH. Up-Regulation of microRNA-183 promotes Cell Proliferation and Invasion in Glioma by directly targeting NEFL. Cell Mol Neurobiol. 2016;36(8):1303–10.
Li L, Du Y, Xiang D, Chen L, Shi Z, Tian J, et al. Prediction of the anti-glioma therapeutic effects of temozolomide through in vivo molecular imaging of MMP expression. Biomed Opt Express. 2018;9(7):3193–207.
Yu X, Jin J, Zheng Y, Zhu H, Xu H, Ma J, et al. GBP5 drives malignancy of glioblastoma via the Src/ERK1/2/MMP3 pathway. Cell Death Dis. 2021;12(2):1–11.
Laurent M, Martinerie C, Thibout H, Hoffman MP, Verrecchia F, Le Bouc Y, et al. NOVH increases MMP3 expression and cell migration in glioblastoma cells via a PDGFR-alpha-dependent mechanism. FASEB J off Publ Fed Am Soc Exp Biol. 2003;17(13):1919–21.
Sun N, Zhao X. Therapeutic implications of FABP4 in Cancer: an emerging target to Tackle Cancer. Front Pharmacol. 2022;13:948610.
Lee V, Smith TW, Arikan MÇ, Zhang L, Çataltepe O, Çataltepe S. Fatty acid-binding protein 4 expression in Tumor cells as a potential marker for anaplastic meningiomas. Appl Immunohistochem Mol Morphol AIMM. 2021;29(2):e10–6.
Vogel Hertzel A, Bernlohr DA. The mammalian fatty acid-binding protein Multigene Family: Molecular and genetic insights into function. Trends Endocrinol Metab. 2000;11(5):175–80.
Duffy CM, Xu H, Nixon JP, Bernlohr DA, Butterick TA. Identification of a fatty acid binding protein4-UCP2 axis regulating microglial mediated neuroinflammation. Mol Cell Neurosci. 2017;80:52–7.
Thelin EP, Zeiler FA, Ercole A, Mondello S, Büki A, Bellander BM et al. Serial Sampling of Serum Protein Biomarkers for Monitoring Human Traumatic Brain Injury Dynamics: A Systematic Review. Front Neurol [Internet]. 2017 [cited 2023 Oct 19];8. https://www.frontiersin.org/articles/https://doi.org/10.3389/fneur.2017.00300.
Shen XN, Huang SY, Cui M, Zhao QH, Guo Y, Huang YY, et al. Plasma glial fibrillary acidic protein in the Alzheimer Disease Continuum: relationship to other biomarkers, Differential diagnosis, and prediction of clinical progression. Clin Chem. 2023;69(4):411–21.
Hol EM, Pekny M. Glial fibrillary acidic protein (GFAP) and the astrocyte intermediate filament system in diseases of the central nervous system. Curr Opin Cell Biol. 2015;32:121–30.
Bazarian JJ, Biberthaler P, Welch RD, Lewis LM, Barzo P, Bogner-Flatz V, et al. Serum GFAP and UCH-L1 for prediction of absence of intracranial injuries on head CT (ALERT-TBI): a multicentre observational study. Lancet Neurol. 2018;17(9):782–9.
Foerch C, Niessner M, Back T, Bauerle M, De Marchis GM, Ferbert A, et al. Diagnostic accuracy of plasma glial fibrillary acidic protein for differentiating intracerebral hemorrhage and cerebral ischemia in patients with symptoms of acute stroke. Clin Chem. 2012;58(1):237–45.
Wagner DC, Scheibe J, Glocke I, Weise G, Deten A, Boltze J, et al. Object-based analysis of astroglial reaction and astrocyte subtype morphology after ischemic brain injury. Acta Neurobiol Exp (Warsz). 2013;73(1):79–87.
Jung CS, Foerch C, Schänzer A, Heck A, Plate KH, Seifert V, et al. Serum GFAP is a diagnostic marker for glioblastoma multiforme. Brain. 2007;130(12):3336–41.
Gállego Pérez-Larraya J, Paris S, Idbaih A, Dehais C, Laigle-Donadey F, Navarro S, et al. Diagnostic and prognostic value of preoperative combined GFAP, IGFBP-2, and YKL-40 plasma levels in patients with glioblastoma. Cancer. 2014;120(24):3972–80.
Chen B, Chen J, House MG, Cullen KJ, Nephew KP, Guo Z. Role of neurofilament light polypeptide in head and neck cancer chemoresistance. Mol Cancer Res MCR. 2012;10(3):305–15.
Acknowledgements
Not applicable.
Funding
This work was supported by a grant to Dr. Eleftherios P. Diamandis from the Canadian Institutes for Health Research, The Canadian Brain Foundation, and the Canadian Cancer Society Research Institute under a SPARK Grant (grant number: CCS707057). The Northwestern Nervous System Tumor Bank is supported by the P50CA221747 SPORE for Translational Approaches to Brain Cancer.
Author information
Authors and Affiliations
Contributions
AG performed data collection and shipping and drafted the manuscript. MKC drafted and edited the manuscript. LMA and WX performed data analysis and contributed to drafting the manuscript. EPD, IP, CH, KM, GZ, AM and GMY conceptualized and designed the study. In addition, EPD and AM drafted the manuscript, and IP edited the manuscript. MW, JB, RC, TG, SM, NP, DR, MS, AM, GS and JW performed the sample analysis. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved under the Research Ethics Board (REB) of Sinai Health System in Toronto, Canada, under the REB number 21–0114-E.
Consent for publication
Not applicable.
Competing interests
MW, JB, RC, TG, SM, NP, DR, MS, AM and GS are employees and JW is an officer of Meso Scale Diagnostics, LLC. Otherwise, the authors did not identify any potential, perceived or real conflicts of interest to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ghorbani, A., Chatanaka, M.K., Avery, L.M. et al. Glial fibrillary acidic protein, neurofilament light, matrix metalloprotease 3 and fatty acid binding protein 4 as non-invasive brain tumor biomarkers. Clin Proteom 21, 41 (2024). https://doi.org/10.1186/s12014-024-09492-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12014-024-09492-7