Abstract
Background
Tuberous sclerosis complex (TSC) is associated with a wide range of physical manifestations for which international clinical recommendations for diagnosis and management have been established. TSC is, however, also associated with a wide range of TSC-Associated Neuropsychiatric Disorders (TAND) that are typically under-identified and under-treated yet associated with a profound burden of disease. The contemporary evidence base for the identification and treatment of TAND is much more limited and, to date, consensus recommendations for the diagnosis and management of TAND have also been limited and non-specific.
Methods
The TANDem project was launched with an international, interdisciplinary, and participatory consortium of 24 individuals, including TSC family representatives, from all World Health Organization (WHO) regions but one. One of the aims of the TANDem project was to generate consensus recommendations for the identification and treatment of TAND. At the time of this project, no internationally adopted standard methodology and methodological checklists existed for the generation of clinical practice recommendations. We therefore developed our own systematic procedure for evidence review and consensus-building to generate evidence-informed consensus recommendations of relevance to the global TSC community.
Results
At the heart of the consensus recommendations are ten core principles surrounded by cluster-specific recommendations for each of the seven natural TAND clusters identified in the literature (autism-like, dysregulated behavior, eat/sleep, mood/anxiety, neuropsychological, overactive/impulsive, and scholastic) and a set of wraparound psychosocial cluster recommendations. The overarching recommendation is to “screen” for TAND at least annually, to “act” using appropriate next steps for evaluation and treatment, and to “repeat” the process to ensure early identification and early intervention with the most appropriate biological, psychological, and social evidence-informed approaches to support individuals with TSC and their families.
Conclusions
The consensus recommendations should provide a systematic framework to approach the identification and treatment of TAND for health, educational, social care teams and families who live with TSC. To ensure global dissemination and implementation of these recommendations, partnerships with the international TSC community will be important. One of these steps will include the generation of a “TAND toolkit” of “what to seek” and “what to do” when difficulties are identified in TAND clusters.
Similar content being viewed by others
Background
Tuberous sclerosis complex (TSC) is a rare genetic disorder associated with mutations in the TSC1 or TSC2 genes, a wide range of physical manifestations, and a highly heterogeneous clinical presentation [1, 2]. TSC is also associated with a broad range of behavioral, psychiatric, intellectual, academic, neuropsychological, scholastic, and psychosocial difficulties [3,4,5]. Until the 1990s, diagnosis, monitoring, and treatment of TSC tended to be inconsistent and highly variable across the globe. In an attempt to standardize the diagnosis of TSC, a consensus conference was convened in 1998. The meeting led to a simplified and revised set of diagnostic criteria for TSC [6] and was accompanied by recommendations for diagnostic evaluation [7]. The 1998 and 1999 consensus publications provided a structured approach to the physical manifestations of TSC. Given the emerging awareness of the neuropsychiatric manifestations of TSC at the time, the consensus panel also aimed to include information about neuropsychiatric manifestations of TSC, albeit in a limited manner. The recommendations made in relation to “neurodevelopmental testing” suggested “thorough age-appropriate screening for behavioral and neurodevelopmental dysfunction” at the time of diagnosis, and reassessment at school entry. “Periodic” retesting was recommended for older children with “previous test abnormalities,” for those with “abnormal cognitive function or behavior,” and when there was a significant change in behavior. No evaluations were recommended for newly diagnosed adults who appeared not to have any difficulties, and no further evaluations were recommended of those who appeared “normal” or had “stable disabilities” [7].
To provide a more systematic and proactive set of recommendations for the assessment of “cognitive and behavioral problems” in TSC, a meeting was convened in Cambridge, UK, in 2003. The consensus panel, consisting of 20 clinicians, researchers, and family representatives from the USA, UK, and the Netherlands, made two main recommendations [5]. First, to perform a comprehensive evaluation at diagnosis and at key developmental timepoints (infancy, toddler years, pre-school, early school years, middle school years, adolescence, and in young adults). Importantly, this recommendation was aimed at the evaluation of all individuals with TSC and not only those with apparent concerns. The panel provided detailed guidelines for developmentally based, comprehensive assessment [8]. The second recommendation was to perform a comprehensive evaluation when sudden or unexpected change or deterioration was observed, mainly to ensure the identification of biological causes of behavioral difficulties, for example growing Subependymal Giant Cell Astrocytoma (SEGA) or poorly controlled seizures. Other than generic comments, no guidelines were provided for intervention. Even though the recommendations were well received in the TSC community, a decade after the publication, fewer than 20% of individuals in the UK with TSC had actually received a comprehensive neuropsychiatric assessment as proposed by the consensus panel, and only about 40% of individuals in a large-scale natural history study of TSC had ever had an evaluation of their intellectual ability [5, 9,10,11]. These findings suggested a significant “assessment and treatment gap” for these manifestations of TSC [11].
In 2012, an International Consensus Conference was convened which included 79 experts from 14 countries. Expert panels, including a neuropsychiatry panel, made recommendations for diagnosis, monitoring, and treatment of the range of organ systems involved in TSC [12]. At this meeting, the neuropsychiatry panel coined the term “TAND” (TSC-associated neuropsychiatric disorders) as an “umbrella” term for the range of bio-psycho-social difficulties associated with TSC, and to create a “shared language” by describing TAND across 6 “levels” (behavioral, psychiatric, intellectual, academic, neuropsychological, and psychosocial) [5, 12]. In addition to comprehensive assessment at key developmental timepoints and in response to sudden or unexpected change or deterioration in TAND, the panel introduced a new recommendation for annual screening of all people with TSC. Some guidance for the intervention of TAND was provided in the consensus guidelines, but in a non-specific manner (e.g., recommending the use of general population evidence-based guidelines for individual manifestations). The 2012 recommendations were updated in 2021, mainly to include consensus recommendations for the use of mTOR inhibitors for physical manifestations of TSC [1]. The TAND-specific recommendations added included the use of screening tools (such as the TAND Checklist), early identification and treatment of TAND manifestations, and psychosocial support to families [1].
Since the 2012 consensus conference and coining of the term “TAND,” a number of new research developments have emerged. These included development and pilot validation of the TAND Checklist (Lifetime version, TAND-L) [5, 13], natural history, and longitudinal studies on the emergence and development of various TAND manifestations [4, 14,15,16,17], the identification of “natural TAND clusters” (natural groupings of TAND manifestations) [18,19,20,21], and studies on the impact of molecularly targeted treatments using mammalian/mechanistic target of rapamycin (mTOR) inhibitors on TAND, albeit with mixed and unclear results [22,23,24]. The TAND Checklist was recommended as a tool for screening in the 2021 revised recommendations [1], but no specific recommendations were made for the identification of natural TAND clusters. More importantly, to date, no specific consensus recommendations have been made for the treatment of any aspect of TAND.
In 2019, the TANDem project was launched as an international, interdisciplinary, and participatory project with three main aims [9] (www.tandconsortium.org). The first aim was to develop and validate a self-report and quantified version of the TAND Checklist (referred to as the TAND-SQ Checklist) and to build it into a mobile application (“app”). The second aim of the project was to generate consensus clinical recommendations for the identification and treatment of TAND as the foundation for a “TAND toolkit” of evidence-informed consensus information and self-help tips to be built into the app. The third aim was to establish a global TAND network through research capacity-building and a range of impact activities [9]. The focus of this paper is on one of the specific objectives of the TANDem project—the generation of consensus recommendations for the identification and treatment of TAND.
There is an ongoing discourse in the literature about the need to balance “evidence” and “expert consensus” in the generation of clinical practice recommendations [25]. Historically, many authors described their recommendations either as “evidence-based” or as “consensus-based.” In the TANDem project, we acknowledged at the outset that the evidence base for the identification and treatment of TAND may be very limited and/or of poor quality and that we may need to include the opinions of TSC experts as well as evidence from outside TSC-specific literature. However, we wanted to examine all existing evidence from the TSC literature to ensure an unbiased evidence-informed approach to our consensus-building, thus balancing “evidence” and “expert consensus.” We also recognized that access to identification and treatment of TAND and resources to support these actions may be highly variable across the globe. This led us to prioritize higher-level conceptual rather than very detailed recommendations in our consensus-building process.
Here we describe the process of evidence-informed consensus generation and present a set of core principles and cluster-based recommendations for the identification and treatment of TSC-associated neuropsychiatric disorders (TAND).
Methods
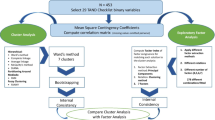
There are at present no formal guidelines for the reporting of consensus-based methods in biomedical research or clinical practice, but encouragingly, a team of researchers has initiated a process to generate what will be known as the ACCORD guidelines [26]. In the absence of a standard methodology and methodological checklist, we created a systematic procedure for evidence generation, review, and consensus-building as outlined in Fig. 1. The majority of activities took place online given the travel restrictions due to the COVID-19 period in the 2020–2022 timeframe of the study.
Step 1. Include all members of the TAND consortium in the consensus panel
The TAND consortium included a group of 24 individuals from all World Health Organization (WHO) regions but one (Eastern Mediterranean), across multiple professional groups including psychiatry, psychology, pediatric neurology, nephrology, speech and language therapy, education, special education, intellectual disability medicine, engineering, and neuroscience [9] (www.tandconsortium.org). The consortium also included “family representatives” of individuals with TSC or family members of people with TSC. Many of the family representatives had “lived expertise” as well as other professional expertise, such as in education or health services. All consortium members participated in the process. Here, we will refer to this group as the “consensus panel.”
Step 2. Creation of cluster groups
Previous research identified seven natural TAND clusters [20]. We therefore divided consortium members into cluster groups for each natural cluster based on areas of expertise and interest. In addition, we created a cluster group for the psychosocial level, given that psychosocial difficulties (the psychological impact of living with TSC and TAND) were not included in the generation of TAND clusters [18,19,20,21]. Each of the eight cluster groups had a lead and a co-lead, plus one or more additional members (for details see [9]). Every cluster, with the exception of the eat/sleep cluster, included at least one family representative. Table 1 shows the eight clusters, the consortium members in each cluster group, and the items from the TAND-L Checklist included in the cluster.
Step 3. Review of the literature
The TAND literature was reviewed in two ways. First, a comprehensive scoping review of all TAND research ever published in the peer-reviewed literature was conducted by the consortium [27]. The purpose of the scoping review was to provide an unbiased review of the TSC-specific evidence (or lack thereof). Secondly, cluster teams each performed a targeted review that focused on literature within and outside TSC that was felt to be relevant and important by the cluster team. These reviews were therefore not highly systematic, but focused on systematic reviews, meta-analyses, and widely accepted clinical guidelines (e.g., NICE guidelines, APA practice parameters). Publications were not only focused on English-speaking healthcare settings, given the international nature of the consortium.
Step 4. Generation of cluster chapters, summary statements, and recommendations
Cluster groups used all available TSC literature and relevant non-TSC literature to draft a “cluster chapter,” as well as summary statements and cluster-based recommendations based on the literature review and their expert opinion. Each cluster chapter was reviewed by two reviewers from other clusters, and improvements were incorporated into cluster chapters, summary statements, and draft recommendations.
Step 5. Presentation and review of summary statements and recommendations per cluster
All cluster chapters, summary statements, and recommendations were made available to the consensus panel. Over a period of 3 months, each cluster group presented their summary statements and recommendations in a series of online meetings. Consensus panel members questioned cluster teams to seek clarification, items were discussed, and text was revised based on discussions. Overall, this process allowed for an iterative and international review of relevant literature given the global goal of our recommendations.
Step 6. Electronic voting and prioritization of summary statements and recommendations
All members of the consensus panel were provided with an online survey which included all summary statements and recommendations—members were asked to vote “strongly agree,” “agree,” “disagree,” or “strongly disagree” on each. They were also asked to provide suggestions if they felt modifications to a statement or recommendation were required and to prioritize their top three statements and recommendations per cluster. Data were collated by the TANDem Action Group in preparation for a 3-day online consensus conference.
Step 7. Consensus conference
At the online consensus conference with the consensus panel, data from votes (as outlined in step 6) were presented, and items where consensus could not be reached even after modification and discussion were excluded.
Step 8. Identification of core principles
It became clear during the evidence review and consensus-building process that a number of core principles were emerging across all clusters. The consortium conference therefore also included the generation of potential core principles from all cluster-specific recommendations.
Step 9. Electronic voting and prioritization of core principles
All potential core principles were collated and consortium members were asked to vote in an online survey whether they “strongly agree,” “agree,” “disagree,” or “strongly disagree” with the proposed principles. From 18 potential principles, a final list of ten core principles was generated with 100% consensus.
Step 10. Generation of the final set of evidence-informed consensus recommendations for the identification and treatment of TAND
The process outlined above led to a final set of recommendations including 10 core principles and eight sets of cluster-specific recommendations. The psychosocial cluster was conceptualized as a “wraparound” cluster (encompassing and relevant to all natural clusters). All consensus panel members reviewed and approved all recommendations.
Results
Figure 2 shows a conceptual representation of the evidence-informed consensus clinical recommendations. At the heart of the recommendations are ten core principles to be used by clinicians and families as an overall guide to the identification and treatment of TAND. This is surrounded by cluster-specific recommendations for each of the seven natural TAND clusters. Around all these recommendations, the wraparound psychosocial cluster recommendations were placed to show how these “wrap around” all the core principles and cluster recommendations.
Core principles for the identification and treatment of TAND
The ten core principles for identification and treatment of TAND are shown in Table 2 and are proposed as a framework to approach any individual with TSC, regardless of their age, sex, genotype (e.g., TSC1 or TSC2), or TAND profile. It recognizes that everyone with TSC is at risk of TAND manifestations (#1) and that it is therefore important to perform lifelong monitoring for the emergence of TAND difficulties (#2) with a minimum of annual screening (#3). The core principles recommend early identification and early intervention (#4) rather than to use a “watch-and-wait” strategy. The consensus panel proposes a cluster-based profiling and identification of needs, but acknowledges that clusters cluster together and that identification of needs in one cluster should also alert caregivers and clinical teams to explore other clusters (#5). In the context of a multi-system condition, core principle #6 points to the importance of the relationship between physical health manifestations and TAND manifestations. Core principle #7 underlines the importance of working with caregivers as lived experts in TSC. Recognizing the very limited traditional “evidence base” in TAND, caregivers, and family communities have valuable contributions to make both in identification and in intervention for TAND. Principle #8 serves as a reminder that TAND difficulties require a “whole-system” understanding to guide an intervention plan. This means that biological, psychological, and social (“bio-psycho-social”) aspects should be considered to understand the needs and to provide interventions and support. By implication, this process requires contributions from many professional groups and disciplines and is not just about finding a “medication” to solve a problem. In spite of the limited evidence base from the scientific literature specifically on TAND, principle #9 recommends the need to be informed by whatever relevant evidence may exist and to guard against approaches known to have evidence of harm. The final principle (#10) is a reminder that the goal of “intervention” and support to individuals with TSC and their caregivers is not merely to reduce symptoms or difficulties, but to help everyone living with TSC achieve an optimal quality of life as individuals and as families and to facilitate their active participation in all aspects of society throughout their journey with TSC and TAND.
Cluster-specific recommendations
Consensus recommendations for the seven natural TAND clusters and the wraparound psychososocial cluster are presented in the text below and in Tables 3, 4, 5, 6, 7, 8, 9 and 10.
Autism-like cluster
The autism-like cluster recommendations are shown in Table 3. TSC is associated with very high rates of social-communication difficulties and a significant proportion of individuals with TSC meet the criteria for autism as defined in the DSM-5 or ICD-11 [16, 28,29,30,31]. However, these difficulties are often identified or diagnosed late, and many children and families miss out on opportunities to access some of the growing number of evidence-based interventions and support programs developed specifically for autism [4]. Similarly, adults with TSC who have social-communication difficulties or autism rarely receive interventional support.
For these reasons, the consensus panel recommended lifelong monitoring of all individuals for manifestations in the autism-like cluster (AU1), from early in infancy and throughout adulthood (AU2). All individuals who show difficulties with autism-like cluster manifestations should be referred for a formal clinical evaluation for communication disorders and autism/autism spectrum disorder (AU3). In the absence of TSC-specific evidence, the consensus panel recommended that the autism literature on children and adults in the general population (i.e., for those with autism without TSC) may be relevant to the TSC community (AU4). For this reason, young children with autism and TSC may benefit from naturalistic developmental behavioral interventions (NDBI) [32, 33], the group of autism interventions with the strongest evidence base at present (AU5). Similarly, adults with TSC and autism-like cluster manifestations may benefit from autism interventions such as social skills training (AU6) [33]. Recognizing the very high rates of co-occurring physical health, neurodevelopmental, and mental health problems in autism in the general population [33], as well as the common co-occurrence of other TAND clusters with the autism-like cluster [18], the panel recommended lifelong monitoring for the presence of co-occurring conditions, followed by appropriate evidence-informed treatments (AU7). Even though autism and the autism-like cluster have been the most extensively examined in TSC research [27], much further research is recommended, particularly in relation to non-pharmacological interventions for difficulties in this cluster (AU8).
Dysregulated behavior cluster
The dysregulated behavior cluster recommendations are shown in Table 4. Difficulties with aggression, temper tantrums, and/or self-injurious behaviors represent some of the greatest concerns and burdens to families who live with TSC [29]. These behaviors are therefore a common reason for referral to specialist services. However, there may be many different reasons for or “pathways” to dysregulated behaviors in TSC. For example, they may be driven by communication difficulties, impulsivity, anxiety, sensory sensitivities, demand avoidance, cognitive inflexibility, trauma, and/or pain [34,35,36,37]. Dysregulated behaviors may also emerge as a result of the physical manifestations of TSC, such as growing SEGA, seizures, or as an adverse effect of medications. For this reason, there is no single intervention approach to this cluster of difficulties, and, equally, no single or simple medication that should be used to “manage” these behaviors. There are also no behavioral treatment studies for dysregulated behavior specifically in people with TSC. However, there is moderate support for real interventions for individuals with intellectual disabilities without TSC, which should inform practice [38]. Non-pharmacological/behavioral interventions may include speech/language work to support communication difficulties, cognitive-behavioral work to support anxiety behaviors and cognitive inflexibility, a range of sensory strategies to support the sensory sensitivities that may trigger dysregulated behaviors, and a range of environmental strategies such as visual schedules to increase predictability and support transitions during daily activities [34,35,36,37,38].
For these reasons, the consensus panel stated that dysregulated behaviors are common, have a major impact on families, and should be investigated in a systematic way (DB1). Given the many possible underlying meanings or functions of behaviors, a careful and systematic functional analysis of behavior should be conducted to generate an understanding of the problem behavior (DB2) [39]. Another important step towards a good understanding is to conduct an evaluation of the intellectual and neuropsychological profile of the individual with TSC (DB3). To ensure rapid identification of any underlying biological cause of dysregulated behaviors, urgent physical examination is recommended for sudden onset and/or rapidly changing or unexpected dysregulated behaviors (DB4). Once the evaluation has been completed, biological causes identified and treated, and a good understanding of the pathways to the dysregulated behavior has been identified, non-pharmacological strategies are recommended as first-line treatment (DB5). Medications should only be used for dysregulated behaviors after a careful and systematic evaluation and always alongside a non-pharmacological intervention plan (DB6). The consensus panel also recognized the need to generate an evidence base particularly for non-pharmacological interventions for dysregulated behaviors in individuals with TSC (DB7).
Eat/sleep cluster
The eat/sleep cluster recommendations are shown in Table 5 with separate recommendations for eating- and sleep-related difficulties. Eating difficulties in TSC are a highly under-researched domain, but the consensus panel recognized that they do occur and may be associated with a range of TAND and/or physical manifestations (ES1). Where eating difficulties are reported, a comprehensive evaluation should be performed to consider the range of potential contributors (e.g., picky eating, autism-related restricted eating, mouth ulcers or anorexia associated with medications, physical ill-health, or pain) (ES2). Recognizing the wide range of developmental, intellectual, and communication levels in TSC, intervention plans for eating should be adapted to the individual needs and profile of each person with TSC. The consensus panel stated that there are no dietary supplements or restricted/special diets with an evidence base in TSC to improve any TAND manifestations (ES3). The ketogenic diet is a well-known approach used for refractory seizures in TSC, but the evidence that it has a direct impact on TAND is mixed [40].
Sleep difficulties are very common across all ages in TSC [4, 41], but there is a complex “bidirectional” association between sleep and other manifestations. For example, sleep difficulties may contribute to neuropsychological difficulties (e.g., in memory or attention), dysregulated behaviors (e.g., increased aggression or temper tantrums), mood problems, or seizures (acting to reduce seizure thresholds or acting as trigger events). Conversely, sleep difficulties may result from other TAND manifestations (e.g., autism-related rigid sleep routines, mood/anxiety-driven insomnia, or early morning wakening), neurological manifestations (e.g., waking from a nocturnal seizure), or result from adverse effects of medications. Sleep difficulties may also be maintained by a behavioral model of reinforcement, such as access to electronic devices or caregiver contact upon waking, or an inadvertent mutual reinforcement cycle including caregivers (e.g., co-sleeping in the caregivers’ bed to help them settle). Pathways to sleep difficulties are complex, and assessment strategies therefore need to be set up to understand each individual’s pathways to their sleep difficulties, in order to ensure appropriate management.
For these reasons, the consensus panel emphasized that sleep difficulties should be monitored regularly regardless of the age, sex, and genotype (ES4) of individuals and that sleep difficulties may be a “cause” and/or a “consequence” of TAND or other neurological manifestations (ES5). Clinicians and caregivers should therefore perform careful examinations to first identify and treat biological contributors to sleep, such as underlying health conditions and behavioral markers of pain (ES6). Next, psychiatric contributors to sleep should be examined and treated (e.g., early morning wakening as part of a depressive disorder or disturbed sleep in the context of an anxiety disorder). Only once these have been identified and treated (or excluded), should other sleep management strategies be explored. Non-pharmacological strategies should always be used first (e.g., sleep education, sleep hygiene) before pharmacological strategies (e.g., melatonin or similar medications) are considered (ES7). Given the very limited evidence base in this cluster, the consensus panel recommended targeted research on eating and sleeping difficulties in TSC (ES8).
Mood/anxiety cluster
The mood/anxiety cluster consensus recommendations are shown in Table 6. The rates of mood and anxiety symptoms and disorders are very high in TSC, often arising in adolescence or adulthood. Difficulties in this cluster are often identified late or not at all. In those with developmental or intellectual disabilities, the identification of mood and anxiety difficulties may be even more difficult. Even though there is no evidence base within TSC for the treatment of depressive and anxiety disorders, there is an encouraging evidence base in the general population that indicates the use and effectiveness of non-pharmacological and pharmacological strategies.
For these reasons, the consensus panel recommended that all children and adults should be monitored for the emergence of mood and anxiety symptoms to ensure early detection and treatment (MA1). Particular efforts should be made to look for mood and anxiety symptoms in those with intellectual and other neurodevelopmental disabilities where manifestations of depressed mood or anxiety may be different (e.g., withdrawal from social interaction, loss of interest in previously enjoyed activities, anorexia, or increased dysregulated behaviors) (MA2). Mood and anxiety symptoms may be the consequence of underlying physical health problems or their treatments (e.g., seizures and anti-seizure medications, renal failure, or chronic pain), and these may require specific management (MA3). Where mood and anxiety symptoms are identified, an appropriate diagnostic evaluation should be performed, and evidence-based non-pharmacological and pharmacological interventions as recommended in the general population should be used to treat mood and anxiety disorders (MA4). Given the heterogeneity in the individual physical health and TAND profiles of individuals with TSC, a personalized approach to management is recommended (MA5). In spite of the high rates of mood and anxiety disorders in TSC, the research evidence base is very limited, and further research, particularly interventional research, was recommended (MA6).
Neuropsychological cluster
The neuropsychological cluster consensus clinical recommendations are shown in Table 7. About half of the individuals with TSC have normal-range intellectual ability (with IQ > 80) and 40–50% have intellectual disabilities. However, the individual profiles of strengths and weaknesses are highly variable between individuals and are often very uneven within individuals regardless of their “overall” intellectual ability [4, 15, 29, 42]. Intellectual ability is a very strong correlate of many TAND manifestations, and uneven intellectual profiles can be associated with many functional impairments. Even in people with above-average and high intellectual abilities, the rates of specific neuropsychological deficits (e.g., in attentional, memory, or executive skills) are very high and can be associated with significant challenges in daily life (e.g., in school, relationships, or the workplace) [43, 44]. This is even more likely to be the case for those with TSC known to have neurodevelopmental disorders such as autism, attention deficit hyperactivity disorder (ADHD), or learning disorders. Understanding the neuropsychological profile of an individual with TSC can help to understand current difficulties and to predict future ones. Performing these evaluations in preparation for transitions in school, in preparation for post-secondary training or for the workplace, and implementing neuropsychological intervention plans, can be of significant value.
For these reasons, the consensus panel recommended that all individuals with TSC should have a comprehensive assessment of their intellectual abilities (NP1) and should be monitored with annual screening for the emergence of neuropsychological deficits (NP2). The recommendations highlighted the fact that specific neuropsychological deficits may have an impact in many ways, including mood and anxiety difficulties (e.g., feeling anxious or easily overwhelmed), having dysregulated behaviors when task demands become too much (e.g., when expected to switch flexibly between tasks), or on their scholastic skills (e.g., in reading, writing, or mathematics) (NP3). Individuals with known neurodevelopmental disorders should receive a detailed evaluation of their profile of neuropsychological strengths and weaknesses and not only be screened for such deficits (NP4). Importantly, the consensus panel recommended that non-pharmacological coaching and training strategies should be used to strengthen areas of neuropsychological deficits (NP5) and that evidence of neuropsychological deficits is likely to require accommodations and specific support in educational or occupational settings (NP6).
Overactive/impulsive cluster
The overactive/impulsive cluster recommendations are shown in Table 8. Overactive, impulsive, and restless behaviors are very common in TSC. Even though the manifestations are typically lower in adults than children, they are seen across ages, sex, and different genotypes [14, 29]. There are many possible reasons why people with TSC have difficulties in this cluster, including physical health, developmental, or environmental reasons. However, a significant proportion of people with difficulties in this cluster may meet the criteria for ADHD and may therefore benefit from the evidence-based treatment strategies for ADHD as recommended in the general population [45], even when they may have co-occurring seizures [46], autism [33], and/or intellectual disability [47, 48].
For these reasons, the consensus panel recommended ongoing screening for difficulties in this cluster and to proceed to appropriate next-step evaluations when difficulties are identified (OI1). All individuals who have difficulties in this cluster should be considered for a diagnostic assessment for ADHD (OI2) and, if diagnosed, be treated using the evidence-based approaches as recommended in the general population (OI3). When ADHD manifestations are moderate-to-severe, treatment with methylphenidate or other stimulant medications should be considered alongside non-pharmacological strategies to support the individual (OI4). Even when ADHD is accompanied by epilepsy, intellectual disability, autism, or other physical or TAND manifestations, the ADHD symptoms may respond appropriately to pharmacological treatments (OI5). The consensus panel also recommended further research to understanding pathways to overactive and impulsive behaviors and to generate an evidence base for intervention strategies (pharmacological and non-pharmacological) for these manifestations in TSC (OI6).
Scholastic cluster
The scholastic cluster recommendations are shown in Table 9. Scholastic difficulties are very common in TSC regardless of the intellectual abilities of individuals with TSC, with rates around 60% [15]. There are often early risk markers of later scholastic difficulties such as the delayed onset of language development, difficulties in social communication, or other developmental milestones [49,50,51]. The majority of school-aged children with TSC are therefore likely to benefit from additional support and/or a personalized approach to their education.
For these reasons, the consensus panel recommended early and ongoing screening for scholastic cluster difficulties followed by appropriate action when concerns are identified (S1). The panel highlighted that delays in early developmental milestones may be markers of future scholastic difficulties (S2). All children with TSC should be considered for an individual educational plan (IEP/IEDP) to support their individual profile of learning needs (S3). There is no “one-size-fits-all” in education provision for children with TSC, and the goal should therefore be to match the comprehensive needs of each child with the most appropriate educational environment (S4). Acknowledging that educational environments and supports may vary significantly across the globe, the panel recommended that in all educational settings, high-quality teaching strategies, response-to-intervention (RTI) approaches, and appropriate accommodations (e.g., differentiated reading material, seats close to the educator, extra time, quite spaces, chunked assignments) should be provided [52, 53] (S5). Educators should monitor the overall TAND profile of each child with TSC and consider how it may affect the child’s ability to access education (S6). Planning for educational transitions through each stage of schooling and beyond secondary education was also recommended (S7).
Wraparound psychosocial cluster
The wraparound psychosocial cluster recommendations are shown in Table 10. The psychosocial health and wellbeing of individuals and families who live with TSC is a priority area, yet very little research has been conducted in this domain, and very little is typically done to evaluate and support the psychosocial needs of families [54,55,56,57,58].
For this reason, the consensus panel recommended monitoring of the psychosocial health and wellbeing of all individuals with TSC (PS1) and of all their family members (PS2), using screening (e.g., with the TAND-SQ Checklist), observation, family reports, or other standardized instruments. Based on their psychosocial needs, families should be provided with integrated and well-coordinated care (PS3). This should include practical support as well as psychosocial interventions (e.g., psychological therapies) as required (PS4). The overall focus should be on “family quality of life” by helping individuals and families identify their goals towards, for example, social activities and active participation (PS5). TSC often has a major impact on the employment and professional lives of individuals with TSC and their families. This should therefore also be a specific focus of psychosocial support provided (PS6). The consensus panel recognized that families and caregivers are paramount to the wellbeing of individuals with TSC and of the whole family. It is therefore of fundamental importance to “care for caregivers” by monitoring caregiver wellbeing, dedicating time in consultations to family and caregiver wellbeing, and generating evidence of interventional approaches that could strengthen caregiver wellbeing (PS7).
Discussion
In this study, we set out to generate evidence-informed consensus recommendations for the identification and treatment of TSC-Associated Neuropsychiatric Disorders (TAND). We used a highly systematic process for evidence evaluation and consensus building. The process led to a set of ten core principles, seven sets of cluster-based clinical recommendations, and recommendations for a “wraparound” psychosocial cluster. Recognizing that individuals and families with TSC live in highly diverse global contexts and health, educational, and social care systems, we prioritized conceptual (“big picture”) recommendations over highly detailed ones.
As outlined in the introduction, clinical practice recommendations for TAND over the years have moved from assessment and treatment when clinical concern was observed (1999), to comprehensive assessment at key developmental timepoints (2005), to annual screening (2013), and to early identification and treatment and psychosocial support for families (2021). The novel contribution of the consensus recommendations presented here was the focus on TAND clusters with the cluster-based evidence review and consensus-building. The search for natural TAND clusters started in response to the “overwhelming uniqueness” of the TAND profiles of individuals described by families and TSC clinicians which made them experience a “treatment paralysis” [11]. Data-driven methodologies using TAND-L Checklist data showed that 7 natural clusters of TAND could be identified [19,20,21]. It is important to observe that, although these clusters had good internal consistency and were therefore coherent within themselves, there is clearly significant overlap and co-occurrence between clusters. For example, the autism-like cluster very often co-occurs with characteristics of other clusters. This observation is summarized in core principle #5 which reminds us that clusters cluster together. Even though the clinical reality is therefore co-occurrence of cluster manifestations, the value of cluster-based identification and treatment lies in the fact that the potentially very complex TAND presentation of an individual can be divided into more manageable chunks for which diagnostic and treatment options may exist.
These consensus clinical recommendations represent the first systematic approach to the identification and treatment of TAND. Taking together all the recommendations presented, the overarching recommendation is shown in Fig. 3 and can be summarized in three words—screen, act, repeat. Caregivers and their support teams in health, social care, and education are encouraged to “screen” for TAND at least annually using screening tools such as the TAND-L or TAND-SQ Checklists [5, 59]. Screening in this context refers to a systematic topline check to identify any existing or emerging concerns in the individual with TSC and/or their caregiver system. Screening can be performed by anyone with appropriate clinical expertise or by caregivers themselves, but should ideally be done in participation with a TSC clinic or other relevant clinical team who can support the family.
Where screening identifies any concerns, this should be followed by action (referring to “act” in Fig. 3). Action should include further detailed evaluations (e.g., of development, for specific disorders, of educational profile and needs, of psychological profile and needs, and of social needs) to inform the most appropriate intervention or treatment plan. Action should be broad and should include a bio-psycho-social approach, where all relevant biological, psychological, and social contributors (and their treatments) are considered and integrated.
Once appropriate action has been taken, it is important to “repeat” the process at least annually to ensure that new and emerging concerns are identified and acted on as soon as possible.
Following the generation of these clinical recommendations, the next important task will be engagement with the international TSC community to ensure the appropriate translation and implementation of these new recommendations across the globe. Targeted dissemination and implementation will need to involve family stakeholder groups (such as Tuberous Sclerosis International and its strong network of national TSC organizations), as well as professional partners in health, social care, and educational settings. One of the next step strategies identified as a specific objective in the TANDem project is to use the consensus recommendations as the foundation for the creation of a ‘TAND toolkit’ of information and tips on “what to seek” (e.g., further evaluations or professional support) and “what to do” (e.g., self-help strategies) to be built into a “TAND toolkit app” (see [9] for further details).
During the final review of these recommendations by the TAND consortium, we reflected on two additional elements, not captured in the core principles or cluster recommendations. The first was the recognition that children and adults with TSC, particularly those with co-occurring intellectual disability, are a vulnerable group at increased risk of abuse and neglect and that all professionals supporting TSC families should be vigilant to identify potential markers of concern [60,61,62]. Apart from their vulnerability to abuse and neglect, individuals with TSC should also be enabled in all possible ways to be able to express their needs and preferences and to be involved in all decisions related to their health and care.
The second reflection was that people with TSC should not be merely defined by their challenges, difficulties, and disabilities. Instead, each person with TSC has their own skills, talents, and personality that can bring great pleasure, enrichment, and meaning to the lives of those around them. In the recently developed TAND-SQ Checklist [59], we added a specific question on “strengths” in response to feedback from within the TAND consortium and TSC community, very much in keeping with the need to balance “difficulties” and “strengths.” These clinical recommendations presented here should therefore be seen as an attempt to give guidance to individuals and families who are struggling with particular aspects of their TAND profile, not to “change” or “cure” the individual, but to improve their quality of life and active participation in society.
Conclusions
Here we presented the first set of evidence-informed consensus recommendations for the identification and treatment of TSC-associated neuropsychiatric disorders (TAND). The next steps should include participation with the broader TSC community to ensure targeted dissemination and implementation of these recommendations. We acknowledge that services and access to interventions are highly variable across the globe and that many families may not immediately be able to access some of the evidence-informed recommendations made here. However, these consensus recommendations are, in part, also presented as an aspirational set of next steps. Families and their clinical teams should therefore use these recommendations to think about what is available in their local communities and collaboratively consider how to get access to support in line with the recommendations made here. We hope that these international consensus recommendations will empower families and professionals who support them with a systematic framework that will reduce the “assessment and treatment gap” in TAND across the globe.
Availability of data and materials
All data generated and analyzed for this paper are included in this publication and its supplementary information files.
References
Northrup H, Aronow ME, Bebin EM, Bissler J, Darling TN, de Vries PJ, et al. Updated international tuberous sclerosis complex diagnostic criteria and surveillance and management recommendations. Pediatr Neurol. 2021;123:50–66.
Henske EP, Józwiak S, Kingswood JC, Sampson JR, Thiele EA. Tuberous sclerosis complex. Nat Rev Dis Prim. 2016;2:16035.
Curatolo P, Moavero R, de Vries PJ. Neurological and neuropsychiatric aspects of tuberous sclerosis complex. Lancet Neurol. 2015;14(7):733–45.
de Vries PJ, Belousova E, Benedik MP, Carter T, Cottin V, Curatolo P, et al. TSC-associated neuropsychiatric disorders (TAND): findings from the TOSCA natural history study. Orphanet J Rare Dis. 2018;13:157.
de Vries PJ, Whittemore VH, Leclezio L, Byars AW, Dunn D, Ess KC, et al. Tuberous sclerosis associated neuropsychiatric disorders (TAND) and the TAND checklist. Pediatr Neurol. 2015;52(1):25–35.
Roach ES, Gomez M, Northrup H. Tuberous sclerosis complex consensus conference: revised clinical diagnostic critera. J Child Neurol. 1998;13(12):624–8.
Roach ES, Dimario FJ, Kandt RS, Northrup H. Tuberous sclerosis consensus conference: recommendations for diagnostic evaluation. J Child Neurol. 1999;14(6):401–7.
de Vries P, Humphrey A, McCartney D, Prather P, Bolton P, Hunt A, et al. Consensus clinical guidelines for the assessment of cognitive and behavioural problems in Tuberous Sclerosis. Eur Child Adolesc Psychiatry. 2005;14(4):183–90.
Heunis T, Bissell S, Byars AW, Capal JK, Chambers N, Cukier S, et al. Empowering families through technology: a mobile-health project to reduce the TAND identification and treatment gap (TANDem). Front Psychiatry. 2022;13:834628.
Kingswood JC, Bruzzi P, Curatolo P, de Vries PJ, Fladrowski C, Hertzberg C, et al. TOSCA - first international registry to address knowledge gaps in the natural history and management of tuberous sclerosis complex. Orphanet J Rare Dis. 2014;9:182.
Leclezio L, de Vries PJ. Towards an improved understanding of TSC-associated neuropsychiatric disorders (TAND). Adv Autism. 2016;2(2):76–83.
Krueger DA, Northrup H, Roberds S, Smith K, Sampson J, Korf B, et al. Tuberous sclerosis complex surveillance and management: Recommendations of the 2012 international tuberous sclerosis complex consensus conference. Pediatr Neurol. 2013;49(4):255–65.
Leclezio L, Jansen A, Whittemore VH, de Vries PJ. Pilot validation of the tuberous sclerosis-associated neuropsychiatric disorders (TAND) checklist. Pediatr Neurol. 2015;52(1):16–24.
de Vries PJ, Belousova E, Benedik MP, Carter T, Cottin V, Curatolo P, et al. Tuberous sclerosis complex-associated neuropsychiatric disorders (TAND): new findings on age, sex, and genotype in relation to intellectual phenotype. Front Neurol. 2020;11:603.
Kingswood JC, D’Augères GB, Belousova E, Ferreira JC, Carter T, Castellana R, et al. TuberOus SClerosis registry to increase disease Awareness (TOSCA) - baseline data on 2093 patients. Orphanet J Rare Dis. 2017;12:2.
Capal JK, Williams ME, Pearson DA, Kissinger R, Horn PS, Murray D, et al. Profile of autism spectrum disorder in tuberous sclerosis complex: results from a longitudinal, prospective, multisite study. Ann Neurol. 2021;90(6):874–86.
Schoenberger A, Capal JK, Ondracek A, Horn PS, Murray D, Byars AW, et al. Language predictors of autism spectrum disorder in young children with tuberous sclerosis complex. Epilepsy Behav. 2020;103:106844.
Alperin S, Krueger DA, Franz DN, Agricola KD, Stires G, Horn PS, et al. Symptom rates and profile clustering in tuberous sclerosis complex-associated neuropsychiatric disorders (TAND). J Neurodev Disord. 2021;13:60.
de Vries PJ, Belousova E, Benedik MP, Carter T, Cottin V, Curatolo P, et al. Natural clusters of tuberous sclerosis complex (TSC)-associated neuropsychiatric disorders (TAND): new findings from the TOSCA TAND research project. J Neurodev Disord. 2020;12:24.
de Vries PJ, Leclezio L, Gardner-Lubbe S, Krueger D, Sahin M, Sparagana S, et al. Multivariate data analysis identifies natural clusters of tuberous sclerosis complex associated neuropsychiatric disorders (TAND). Orphanet J Rare Dis. 2021;16:447.
Leclezio L, Gardner-Lubbe S, de Vries PJ. Is it feasible to identify natural clusters of TSC-associated neuropsychiatric disorders (TAND)? Pediatr Neurol. 2018;81:38–44.
Krueger DA, Sadhwani A, Byars AW, de Vries PJ, Franz DN, Whittemore VH, et al. Everolimus for treatment of tuberous sclerosis complex-associated neuropsychiatric disorders. Ann Clin Transl Neurol. 2017;4(12):877–87.
Overwater IE, Rietman AB, Mous SE, Bindels-De Heus K, Rizopoulos D, Ten Hoopen LW, et al. A randomized controlled trial with everolimus for IQ and autism in tuberous sclerosis complex. Neurology. 2019;93(2):E200–9.
Randell E, McNamara R, Mark Davies D, Owen-Jones E, Kirby N, Angel L, et al. The use of everolimus in the treatment of neurocognitive problems in tuberous sclerosis (TRON): study protocol for a randomised controlled trial. Trials. 2016;17:398.
Djulbegovic B, Guyatt G. Evidence vs consensus in clinical practice guidelines. JAMA. 2019;322(8):725–6.
Gattrell WT, Pali Hungin A, Price A, Winchester CC, Tovey D, Hughes EL, et al. ACCORD guideline for reporting consensus-based methods in biomedical research and clinical practice: a study protocol. Res Integr Peer Rev. 2022;7:3.
Vanclooster S, Bissell S, van Eeghen AM, Chambers N, De Waele L, Byars AW, et al. The research landscape of tuberous sclerosis complex–associated neuropsychiatric disorders (TAND) - a comprehensive scoping review. J Neurodev Disord. 2022;14:13.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-5. Arlington, VA, Washington, D.C.; 2013.
de Vries PJ, Wilde L, de Vries MC, Moavero R, Pearson DA, Curatolo P. A clinical update on tuberous sclerosis complex-associated neuropsychiatric disorders (TAND). Am J Med Genet Part C Semin Med Genet. 2018;178(3):309–20.
van Eeghen AM, Pulsifer MB, Merker VL, Neumeyer AM, van Eeghen EE, Thibert RL, et al. Understanding relationships between autism, intelligence, and epilepsy: a cross-disorder approach. Dev Med Child Neurol. 2013;55(2):146–53.
World Health Organization. International statistical classification of diseases and related health problems. 11th ed. https://icd.who.int/; 2019.
Schreibman L, Dawson G, Stahmer AC, Landa R, Rogers SJ, McGee GG, et al. Naturalistic developmental behavioral interventions: empirically validated treatments for autism spectrum disorder. J Autism Dev Disord. 2015;45:2411–28.
Lord C, Charman T, Havdahl A, Carbone P, Anagnostou E, Boyd B, et al. The Lancet Commission on the future of care and clinical research in autism. Lancet. 2022;399(10321):271–334.
Eden K, de Vries P, Moss J, Richards C, Oliver C. Self-injury and aggression in tuberous sclerosis complex: cross syndrome comparison and associated risk markers. J Neurodev Disord. 2014;6(1):10.
Wilde L, Eden K, de Vries P, Moss J, Welham A, Oliver C. Self-injury and aggression in adults with tuberous sclerosis complex: frequency, associated person characteristics, and implications for assessment. Res Dev Disabil. 2017;64:119–30.
Wilde L, Wade K, Eden K, Moss J, de Vries PJ, Oliver C. Persistence of self-injury, aggression and property destruction in children and adults with tuberous sclerosis complex. J Intellect Disabil Res. 2018;62(12):1058–71.
Boronat S, Van Eeghen AM, Shinnick JE, Newberry P, Thiele EA. Stressor-related disorders in tuberous sclerosis. Ann Clin Psychiatry. 2013;25(4):243–9.
Prior D, Win S, Hassiotis A, Hall I, Martiello MA, Ali AK. Behavioural and cognitive-behavioural interventions for outwardly directed aggressive behaviour in people with intellectual disabilities. Cochrane Database Syst Rev. 2023;2(2):CD003406.
Merlo G, Chiazzese G, Taibi D, Chifari A. Development and validation of a functional behavioural assessment ontology to support behavioural health interventions. JMIR Med Informatics. 2018;6(2):e37.
van Berkel A, Ijff DM, Verkuyl JM. Cognitive benefits of the ketogenic diet in patients with epilepsy: a systematic overview. Epilepsy Behav. 2018;87:69–77.
Van Eeghen AM, Numis AI, Staley BA, Therrien SE, Thibert RL, Thiele EA. Characterizing sleep disorders of adults with tuberous sclerosis complex: a questionnaire-based study and review. Epilepsy Behav. 2011;20:68–74.
van Eeghen AM, Chu-Shore CJ, Pulsifer MB, Camposano SE, Thiele EA. Cognitive and adaptive development of patients with tuberous sclerosis complex: a retrospective, longitudinal investigation. Epilepsy Behav. 2012;23(1):10–5.
de Vries PJ, Gardiner J, Bolton PF. Neuropsychological attention deficits in tuberous sclerosis complex (TSC). Am J Med Genet Part A. 2009;149A(3):387–95.
Tierney KM, Mccartney DL, Serfontein JR, de Vries PJ. Neuropsychological attention skills and related behaviours in adults with tuberous sclerosis complex. Behav Genet. 2011;41:437–44.
Wolraich ML, Hagan JF, Allan C, Chan E, Davison D, Earls M, et al. Clinical practice guideline for the diagnosis, evaluation, and treatment of attention-deficit/hyperactivity disorder in children and adolescents. pediatrics. 2019;144(4):e20192528.
Eaton C, Yong K, Walter V, Mbizvo G, Rhodes S, Chin R. Stimulant and non-stimulant drug therapy for people with attention deficit hyperactivity disorder and epilepsy. Cochrane Database Syst Rev. 2022;13(7):CD013136.
Sun C-K, Tsent P-T, Wu C-K, Li D-J, Chen T-Y, Stubbs B, et al. Therapeutic effects of methylphenidate for attention-deficit/hyperactivity disorder in children with borderline intellectual functioning or intellectual disability: a systematic review and meta-analysis. Sci Rep. 2019;9:15908.
Ji N, Findling R. Pharmacotherapy for mental health problems in people with intellectual disability. Curr Opin Psychiatry. 2016;29(2):103–25.
Barnes MA, Clemens NH, Fall AM, Roberts G, Klein A, Starkey P, et al. Cognitive predictors of difficulties in math and reading in pre-kindergarten children at high risk for learning disabilities. J Educ Psychol. 2019;112(4):685–700.
Burgoyne K, Lervag A, Malone S, Hulme C. Speech difficulties at school entry are a significant risk factor for later reading difficulties. Early Child Res Q. 2019;49:40–8.
Larney R. The relationship between early language delay and later difficulties in literacy. Early Child Dev Care. 2002;172(2):183–93.
Crawford L. The role of assessment in a response to intervention model. Prev Sch Fail. 2014;58(4):230–6.
Hoover JJ, Love E. Supporting school-based response to intervention: a practitioner’s model. Teach Except Child. 2011;43(3):40–8.
Jansen AC, Vanclooster S, de Vries PJ, Fladrowski C, Beaure d’Augères G, Carter T, et al. Burden of illness and quality of life in tuberous sclerosis complex: findings from the TOSCA study. Front Neurol. 2020;11:904.
Hallett L, Foster T, Liu Z, Blieden M, Valentim J. Burden of disease and unmet needs in tuberous sclerosis complex with neurological manifestations: systematic review. Curr Med Res Opin. 2011;27(8):1571–83.
Rentz AM, Skalicky AM, Liu Z, Wheless JW, Dunn DW, Frost MD, et al. Tuberous sclerosis complex: a survey of health care resource use and health burden. Pediatr Neurol. 2015;52:435–41.
Amin S, Mallick AA, Lux A, O’Callaghan F. Quality of life in patients with tuberous sclerosis complex (TSC). Eur J Paediatr Neurol. 2019;23:801–7.
Graffigna G, Bosio C, Cecchini I. Assisting a child with tuberous sclerosis complex (TSC): a qualitative deep analysis of parents’ experience and caring needs. BMJ Open. 2013;3(12):e003707.
Heunis T, Chambers N, Vanclooster S, Bissell S, Byars AW, Capal JK, et al. Development and feasibility of the self-report, quantified TSC-Associated Neuropsychiatric Disorders Checklist (TAND-SQ). Pediatr Neurol. 2023;7:101–23.
Both P, ten Holt L, Mous S, Patist J, Rietman A, Dieleman G, et al. Tuberous sclerosis complex: concerns and needs of patients and parents from the transitional period to adulthood. Epilepsy Behav. 2018;83:13–21.
Jones L, Bellis MA, Wood S, Hughes K, McCoy E, Eckley L, et al. Prevalence and risk of violence against children with disabilities: a systematic review and meta-analysis of observational studies. Lancet. 2012;380:899.
Hughes K, Bellis MA, Jones L, Bates G, Eckley L, McCoy E, et al. Prevalence and risk of violence against adults with disabilities: a systematic review and meta-analysis of observational studies. Lancet. 2012;379:1621–50.
Acknowledgements
We are extremely grateful for the remarkable support from Ms. Annemie T’Seyen and the King Baudouin Foundation, to the TSC International (TSCi) community for their passion and commitment, to our TSC research and clinical colleagues for supporting us, to all the TSC families who have helped us in direct and indirect ways by sharing their stories and knowledge, and to Deborah White for her magical graphic design skills.
Funding
The work was funded by a grant from the King Baudouin Foundation Fund Dr. & Mrs. Charles Tournay‑Dubisson to PJdV and ACJ (2019‑J1120010‑213544) and supplemental funding from the Tuberous Sclerosis Association (UK) (2019‑P03) to PJdV. AJ is supported by a Senior Clinical Investigator Fellowship from the Research Foundation Flanders (FWO 1805321N).
Author information
Authors and Affiliations
Contributions
PJdV and ACJ conceptualized the TANDem project, secured funding, and recruited members of the TAND consortium. PJdV and ACJ were co-PIs on the project, and TH, SV, NC, and LDW were members of the Action Group which managed the overall project. Cluster leads, co-leads, and consortium members all contributed to evidence review and consensus-building as outlined in the manuscript. All consortium members participated in protocol development, in review of data, and in all steps of the evidence review and consensus-building process, as outlined in the “Methods” section. PJdV wrote the first draft of the manuscript, and all consortium members reviewed and contributed to the manuscript revisions, including at an in-person TAND consortium retreat in November 2022 in Stellenbosch, South Africa. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the University of Cape Town Faculty of Health Sciences Human Research Ethics Committee (HREC), the site of the principal investigator, with protocol number HREC 849/2020.
Consent for publication
Not applicable.
Competing interests
PJdV was a study steering committee member of three phase III trials in TSC sponsored by Novartis, was on the scientific advisory group of the TOSCA international disease registry sponsored by Novartis, and has provided consultancy to GW Pharma. SB is funded by Cerebra to investigate sleep and behavior in rare genetic syndromes, including TSC. AVE is on the scientific advisory board and received grant support from Jazz Pharmaceuticals. JC receives grant funding from the NIH and the Department of Defense for projects related to TSC. PD receives partial salary support from the NIH for participation in studies related to TSC, as well as from Aucta Pharmaceuticals for a study of topical sirolimus for facial angiofibromas in TSC and Marinus Pharmaceuticals for a study of ganaxolone for TSC‑related epilepsy. CS receives salary support from the TSC Alliance, a non‑profit organization that reports revenue from individual donors and corporations including Greenwich Biosciences, GW Pharma, Mallinckrodt, Nobelpharma, Novartis, Ovid, UCB, and Upsher‑Smith. DAK reports grants from the National Institutes of Health (NINDS) during the conduct of the study as well as the personal fees from Novartis Pharmaceuticals, personal fees from Greenwich Bioscience, grants from Marinus Pharmaceuticals, personal fees from Nobelpharma America, personal fees from REGENXBIO, and grants and non‑financial support from TSC Alliance outside the submitted work. MS reports grant support from Novartis, Biogen, Astellas, Aeovian, Bridgebio, and Aucta and has served on Scientific Advisory Boards for Novartis, Roche, Regenxbio, SpringWorks Therapeutics, Jaguar Therapeutics, and Alkermes. ACJ was on the scientific advisory group of the TOSCA international disease registry sponsored by Novartis and has provided consultancy to GW Pharma. The remaining authors declared no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
de Vries, P.J., Heunis, TM., Vanclooster, S. et al. International consensus recommendations for the identification and treatment of tuberous sclerosis complex-associated neuropsychiatric disorders (TAND). J Neurodevelop Disord 15, 32 (2023). https://doi.org/10.1186/s11689-023-09500-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s11689-023-09500-1