Abstract
Background
Respiratory muscle training is a continuous and standardized training of respiratory muscles, but the evidence of the effects on early stroke patients is not clear. This meta-analysis aimed to investigate the effects of respiratory muscle training on respiratory function and functional capacity in patients with early stroke.
Methods
PubMed, Embase, PEDro, ScienceDirect, AMED, CINAHL, and China National Knowledge Infrastructure databases were searched from inception to December 8, 2023 for articles about studies that 1) stroke patients with age ≥ 18 years old. Early stroke < 3 months at the time of diagnosis, 2) respiratory muscle training, including inspiratory and expiratory muscle training, 3) the following measurements are the outcomes: respiratory muscle strength, respiratory muscle endurance, pulmonary function testing, dyspnea fatigue score, and functional capacity, 4) randomized controlled trials. Studies that met the inclusion criteria were extracted data and appraised the methodological quality and risk of bias using the Physiotherapy Evidence Database scale and the Cochrane Risk of Bias tool by two independent reviewers. RevMan 5.4 with a random effect model was used for data synthesis and analysis. Mean differences (MD) or standard mean differences (SMD), and 95% confidence interval were calculated (95%CI).
Results
Nine studies met inclusion criteria, recruiting 526 participants (mean age 61.6 years). Respiratory muscle training produced a statistically significant effect on improving maximal inspiratory pressure (MD = 10.93, 95%CI: 8.51–13.36), maximal expiratory pressure (MD = 9.01, 95%CI: 5.34–12.69), forced vital capacity (MD = 0.82, 95%CI: 0.54–1.10), peak expiratory flow (MD = 1.28, 95%CI: 0.94–1.63), forced expiratory volume in 1 s (MD = 1.36, 95%CI: 1.13–1.59), functional capacity (SMD = 0.51, 95%CI: 0.05–0.98) in patients with early stroke. Subgroup analysis showed that inspiratory muscle training combined with expiratory muscle training was beneficial to the recovery of maximal inspiratory pressure (MD = 9.78, 95%CI: 5.96–13.60), maximal expiratory pressure (MD = 11.62, 95%CI: 3.80–19.43), forced vital capacity (MD = 0.87, 95%CI: 0.47–1.27), peak expiratory flow (MD = 1.51, 95%CI: 1.22–1.80), forced expiratory volume in 1 s (MD = 0.76, 95%CI: 0.41–1.11), functional capacity (SMD = 0.61, 95%CI: 0.08–1.13), while inspiratory muscle training could improve maximal inspiratory pressure (MD = 11.60, 95%CI: 8.15–15.05), maximal expiratory pressure (MD = 7.06, 95%CI: 3.50–10.62), forced vital capacity (MD = 0.71, 95%CI: 0.21–1.21), peak expiratory flow (MD = 0.84, 95%CI: 0.37–1.31), forced expiratory volume in 1 s (MD = 0.40, 95%CI: 0.08–0.72).
Conclusions
This study provides good-quality evidence that respiratory muscle training is effective in improving respiratory muscle strength, pulmonary function, and functional capacity for patients with early stroke. Inspiratory muscle training combined with expiratory muscle training seems to promote functional recovery in patients with early stroke more than inspiratory muscle training alone.
Trial registration
Prospero registration number: CRD42021291918.
Similar content being viewed by others
Introduction
Stroke has become a major global health problem due to its high incidence, high disability rate, high recurrence rate, high mortality rate and high cost [1,2,3]. With the improvement of medical management for early stroke, most early stroke patients can survive but face loss of function [3,4,5]. Early stroke not only affects sensory, motor, cognitive and verbal functions, but also affects respiratory function [6, 7]. However, people usually give priority to the recovery of limb dysfunction in patients with early stroke and pay less attention to respiratory dysfunction after early stroke [8]. Although there is no precise report on the incidence of respiratory dysfunction in early stroke patients, previous studies have found that 18–88% of stroke patients have respiratory dysfunction [6, 9]. Research shows that stroke recovery usually occurs within three months of stroke onset, while 15–30% of stroke patients may have permanent dysfunction after 3 months of onset [6, 10, 11]. This means that the critical period for respiratory function recovery in early stroke patients may be within three months after the onset of stroke. The study would pay attention to respiratory dysfunction in people who had a stroke within three months.
Respiratory dysfunction in patients with early stroke may be related to respiratory centre damage after stroke [9, 12]. Stroke lesions can induce a series of pathophysiological reactions like inflammation, oxidative stress, metabolic abnormalities, excitatory toxicity and apoptosis, which can affect the respiratory centre, destroy the nerve conduction pathways related to respiration, and further damage the integration and regulation ability of respiratory-related sensory input, thereby reducing the activity function of respiratory muscle and eventually leading to respiratory dysfunction [13]. Besides, patients may suffer from malnutrition, secondary pain, reduced hemiplegic side activity, abnormal muscle tension, chest contracture, and even immobilization after early stroke, which may cause secondary dysfunction such as respiratory pattern disorder, insufficient pulmonary ventilation and gas exchange, decreased respiratory muscle contraction coordination, abnormal thoracic activity, and ultimately further lead to respiratory dysfunction [9, 14,15,16]. Respiratory dysfunction can increase the mortality rate of early stroke patients by 2–6 times, prolong the average hospitalization time, aggravate neurological dysfunction and lose their self-care ability [17, 18]. Therefore, it is necessary to explore effective respiratory rehabilitation to improve the respiratory function of early stroke patients and promote functional recovery.
Respiratory muscle training (RMT) is a kind of continuous and standardized training of inspiratory muscles or expiratory muscles, which increases the strength and endurance of respiratory muscles by improving maximum inspiratory pressure (MIP) and maximum expiratory pressure (MEP) [19]. The conventional approach of RMT is to perform repetitive breathing exercises with a hand-held respiratory training device to provide a pressure threshold or flow-dependent resistance against inhalation or exhalation to stimulate the respiratory musculature to respond and produce changes in muscle structure [19, 20]. Clinical studies suggest that RMT may be beneficial to the recovery of stroke patients [21, 22]. However, evidence for its effect on early stroke patients remains unclear. Therefore, available clinical studies need to be reviewed for the effects of RMT in early stroke patients.
In recent years, systematic reviews and meta-analyses studying the effects of RMT in stroke patients have increased. Seven systematic reviews collated evidence that RMT can improve respiratory function in stroke [17, 23,24,25,26,27,28]. Five studies reported that RMT can improve exercise tolerance in stroke patients [17, 23,24,25, 27]. Pollock et al. [29] pointed out that RMT may improve respiratory function in stroke patients but further research is needed. While Xiao et al. [8] held a different result that there was insufficient evidence to support the effect of RMT on post-stroke function. However, these systematic reviews did not separately study the efficacy of RMT in early stroke patients, and the studies included in these systematic reviews mixed early and chronic stroke patients. Therefore, an updated review for RMT in patients with early stroke of the existing literature is required. The review was the first-time analysis of the early stroke stage.
Thus, the objectives of this review were to examine the effects of RMT on respiratory function and functional capacity in patients with early stroke.
Materials and methods
This meta-analysis was conducted following the preferred reporting items for systematic reviews and meta-analysis (PRISMA) guidelines [30].
Eligibility criteria
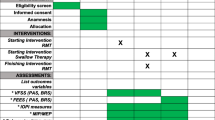
The inclusion criteria were made (as detailed in Table 1) according to the Population-Interventions-Comparison-Outcomes of interest-Study design (PICOS) framework. The exclusion criteria were: (1) unusable full text, abstract-only papers, or protocol; (2) stroke with congestive heart failure; (3) insufficient data for effect size (ES) and 95% confidence interval (CI); (4) inappropriate intervention methods, for example, the description of the training program is unclear about the intensity, duration and frequency of the training; (5) studies with less than 4 points of the PEDro [26, 27, 31, 32].
Information sources
The search was conducted in PubMed, Embase, PEDro, ScienceDirect, AMED, CINAHL, and China National Knowledge Infrastructure databases from inception to December 8, 2023.
Search strategy
Keywords and associated terms were used flexibly in the retrieval process, combined with boolean operators and truncations, to ensure that the retrieved literature is related to the subject. The language was not limited in the actual retrieval process to reduce the deviation, although the language was restricted to English at the beginning of PROSPERO registration. A comprehensive and structured retrieval strategy was formulated as follows according to relevant retrieval guidelines. After the main database search, a further manual search was done from the reference list of all retained articles to ensure that comprehensive and complete literature can be retrieved. The specific search processes of all databases are shown in Additional file 1.
(“respiratory strength training” OR “inspiratory strength training” OR “expiratory strength training” OR “respiratory muscle training” OR “RMT” OR “inspiratory muscle training” OR “IMT” OR “expiratory muscle training” OR “EMT” OR “breathing muscle training” OR breathing exercises) AND (“acute stroke” OR “sub-acute stroke” OR “early stroke” OR “cerebrovascular accident” OR “stroke” OR “cerebral stroke” OR “CVA”) AND (“respiratory function” OR “respiratory muscle strength” OR “maximum inspiratory pressure” OR “MIP” OR “maximum expiratory pressure” OR “MEP” OR “respiratory muscle endurance” OR “pulmonary function testing” OR “peak expiratory flow” OR “PEF” OR “forced expiratory volume in 1 s” OR “FEV1” OR “forced vital capacity” OR “FVC” OR “dyspnea fatigue score” OR “functional capacity” OR “6-min walking test” OR “Fugl-Meyer assessment” OR “functional ambulation category”) AND (random* control* trials)
Selection process
The retrieved studies were aggregated and stored in Endnote 20 software. After duplicate studies were removed, two reviewers (YS and JM) read the titles and abstracts of the remaining studies separately according to the inclusion and exclusion criteria, excluded the literature that did not meet the inclusion criteria, and then read the full texts of the literature that might meet the inclusion criteria to further judge whether they were included. Finally, the reviewers conducted face-to-face communication and proofreading of the final included studies. If the two reviewers disagree with the results of a study or eventual inclusion, it would be solved through discussion or consultation with a third reviewer (CS).
Data collection process
Two reviewers (YS and LH) performed independently data extraction related to the evaluation question using standard data extraction forms adapted from the Joanna Briggs Institute (JBI) tool due to its ease in collecting and presenting relevant data, allowing for an effortless comparison and analysis between each of the studies [33, 34]. To ensure that relevant data was found and extracted while minimizing biases and other errors, the standard data extraction form has been tested before formal data extraction. The data extracted from the included articles were as follows: research background (author, publication year and country), research design, participant characteristics, sample size, intervention details (modality, intensity, training time, duration, device), control group management, outcome measures, and results (mean and standard deviation of outcomes) according to the suggestion of "Cochrane Handbook for Systematic Reviews of Interventions" [35]. When there were a lack of relevant data or problems in this process, the reviewer (JH) contacted the corresponding author to obtain relevant information. The extracted data were verified by a third reviewer (KZ).
Methodological quality and risk of bias assessment
The tool chosen for the quality appraisal of this meta-analysis was the PEDro scale and cut-off values for PEDro scores were considered when selecting studies. Since the PEDro scale is an effective and reliable scoring tool for evaluating methodological quality within the physiotherapy profession and has been used frequently in systematic reviews and meta-analysis [35, 36]. The PEDro scale includes 11 items, including one external validity (eligibility criteria and source), eight items assessing the risk of bias (random allocation, concealed allocation, baseline comparability, blinding of participants, blinding of therapists, blinding of assessors, adequate follow-up (> 85%), intention-to-treat analysis), and two items assessing the completeness of the statistical report on the risk of bias (between-group statistical comparisons, reporting of point measures and measures of variability) [36, 37]. The total score ranges from 0 to 10 (the first item is not included), and higher scores indicate superior methodological quality [36]. Studies with scores between 9 and 10 are considered ‘excellent’, and scores from 6 to 8 are assessed as good, whereas scores of 5 and 4 are classified as fair quality, and scores below 4 are considered poor quality [38, 39]. Additionally, the risk of bias in included studies was assessed using the items of the Cochrane Risk of Bias tool and recorded in Review Manager 5.4 [35]. Two reviewers (YS and JX) with the same critical evaluation knowledge level used the PEDro score and the Cochrane Risk of Bias tool to independently assess methodological quality and risk of bias for included studies. Any disagreements with the score were resolved through discussion. If there were still any disagreements between the two primary reviewers, a third reviewer (YD) would resolve them.
Data synthesis and analysis
RevMan 5.4. was used for data synthesis and analysis [35]. Meta-analysis was conducted only when the data of the analyzed variables were at least 3 studies. The heterogeneity among the studies was evaluated by the Cochrane Q statistic and the inconsistency index (I2) interpreted according to the Cochrane methodology [35]. The statistical heterogeneity was categorized as negligible or small heterogeneity (0 − 40%); moderate heterogeneity (30 − 60%); substantial heterogeneity (50 − 90%); and large/large heterogeneity (> 75%) [40]. The study was considered heterogeneous if the Cochran’s Q statistic tested for significance (p < 0.1) or the I2 was > 50% [41]. Since the use of the Q statistic is questioned when the number of included studies in the meta-analysis is small and the within-study variance is large, a random-effects model was used in this study. The separate pooled estimate of ES and their respective 95% CI was calculated, and the difference was significant when the test level was p < 0.05. If the standard deviation (SD) of change was not available, meta-analyses were performed using the standard deviation of baseline measurements. In addition, when the mean and SD were not present and the available statistics were the median and quartile range (IQR), these estimates of CI were transformed using IQR divided by 1.35.
Subgroup analyses were performed to assess the effect of different types of RMT (IMT + EMT or IMT only) on outcome variables in patients with early stroke if there were a sufficient number of studies. Sensitivity analyses were performed by removing studies one by one to assess the robustness or reliability of the pooled results for each variable, and to detect whether any studies produced significant heterogeneity between RMT and ES pooled estimations. Publication bias and other types of information bias in the meta-analysis would be comprehensively tested using funnel plots if the included studies were at least 10 or more [35, 42].
Results
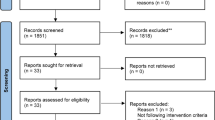
A total of 270 studies were retrieved, including 242 studies from databases, 19 studies from registers, and 9 studies from websites and citation searching. After excluding 87 duplicate studies, titles and abstracts were read, 145 irrelevant articles were excluded, and the full texts of the remaining studies were sought for reading and eligibility assessment. Finally, 35 studies were evaluated for inclusion, of which 26 studies were excluded for reasons (like stroke more than 3 months at the time of diagnosis, inappropriate intervention methods, not RCT), and 9 studies met the eligibility criteria and were included for quality analysis. Figure 1 shows the PRISMA flow diagram of study selection.
Characteristics of the included studies
The included 9 studies were conducted between 2015 and 2022, while 3 studies [6, 43, 44] published in 2021 and 2022 updated the topic of this section and were not included in the previous review. Studies were conducted in China [43,44,45,46], Korea [6, 47], Spain [22, 48], and Britain [49]. Although the included studies varied by location, the synthesis of evidence can provide guidance and help for practice and further research. The main characteristics of the included studies are summarized in Table 2.
Participants
The 9 studies enrolled 526 participants, with the number of participants varying from 40 [47] to 109 [48]. The mean age of the participants was 61.6 years. Participants included in all studies contained both genders, but there was an overall predominance of male participants. All participants in this study had less than three months of stroke onset. Three studies [6, 45, 49] included patients within 2 weeks of stroke. Two studies [22, 46] included patients within 1 to 3 weeks of stroke. One study [48] included patients within 3 weeks of stroke. Others [43, 44, 47] included patients within 3 months of stroke. Most included studies did not assess the initial MIP and MEP, while only 3 studies [22, 48, 49] evaluated the initial MIP and MEP. The average of the initial MIP and MEP was 40 cmH2O and 60 cmH2O respectively. Research shows that the normal values of MIP and MEP are as follows: MIP (118.4 ± 37.2 cmH2O for men, 84.5 ± 30.3 cmH2O for women), MEP (140 ± 30cmH2O for men, 95 ± 20 cmH2O for women), while lower than normal values are considered a decrease in MIP and MEP [50, 51]. The original average MIP and MEP in the included studies are both considered decreases.
Interventions
All included studies performed RMT in the intervention group (IG). Six studies performed IMT and EMT [6, 22, 43, 44, 47, 48], while the remaining studies only had IMT [45, 46, 49]. Both IG and the Control Group (CG) carried out regular rehabilitation therapy. Six studies [6, 43,44,45,46,47] used regular rehabilitation programs in the CG. Three studies [22, 48, 49] used sham MIP + MEP with the workloads fixed in the CG, which was not enough to improve respiratory muscle strength or endurance. Regarding the devices used in the IG, they were different: Threshold, Orygen-Dual valve, Respironics, A flow-oriented incentive spirometer, Acapella vibratory, SECCO S2 intelligent respiratory training instrument, POWERbreathe, all from the manufacturer (Details in Table 2). Although different types of devices were used, most of the studies were threshold resistance, while only Gu et al. [45] and Choi et al. [6] were variable resistance.
The parameters of intervention were different across the studies. Although the intensity of RMT in the included studies varied, they started at 30% to 50% of MIP/MEP and were adjusted with the intervention weekly or biweekly. RMT with an intensity of less than 30% may not improve inspiratory muscle strength and exercise tolerance [27]. Additionally, the frequency and duration also varied in these studies. The time of the sessions varied from 20 to 30 min. Five studies [6, 43, 44, 46, 47] tended to adopt 30 min, and the remaining studies [22, 45, 48, 49] used 5 sets or 5–10 sets with 3 or 10 repetitions. Furthermore, sessions were carried out 5 to 14 times per week. The duration of the intervention ranged between 3 to 8 weeks.
Methodological quality and risk of bias of included studies
The methodological quality and risk of bias of included studies were critically evaluated using the PEDro scale and the Cochrane Risk of Bias tool. Table 3 presents each item score and the results of 9 RCT studies. The risk of bias graph is shown in Fig. 2. The studies of Messaggi-Sartor et al. [48] and Yu et al. [46] were the highest scores with a PEDro score of eight points, and their methodological quality can be regarded as 'good'. Furthermore, there were also 6 studies [6, 22, 43,44,45, 49] whose methodological quality can be regarded as 'good'. Though the lowest score was five points for the study of Yoo and Pyun [47], its methodological quality can be regarded as ‘fair’. The mean PEDro score of the included studies was 6.5 (range 5 to 8). Therefore, it is considered good-quality evidence.
All the critically appraised studies reported random allocation, baseline similarity, between-group differences, and point estimate and variability. Eight studies [6, 22, 43,44,45,46, 48, 49] provided intention-to-treat analysis. Five studies reported respectively appropriate follow-up data [43,44,45,46,47] and reported concealed allocation [6, 44, 46, 48, 49]. Four studies [22, 46, 48, 49] provided blindness to outcome assessors, which may introduce detection bias. However, only one studies [48] showed blind participants. None of the studies blinded the therapists. Participants and therapists were not blinded, which could lead to performance bias. However, performance bias should not be considered a preferential bias effect because it is difficult or impossible to blind participants and therapists in the process of implementing complex interventions [52]. Therefore, despite the performance bias and detection bias in these studies, the lack of blinding for participants and therapists was accepted in this review but taken into account when interpreting the results.
Effect of interventions
Effect of respiratory muscle training on respiratory muscle strength
The MIP and MEP were assessed in six studies [6, 22, 45, 46, 48, 49]. RMT produced a statistically significant effect on improving MIP (n = 309, MD = 10.93, 95%CI: 8.51-13.36, p < 0.00001, I2 = 0%) (Fig. 3) and MEP (n = 309, MD = 9.01, 95%CI: 5.34–12.69, p < 0.00001, I2=37%) (Fig. 4) in patients with early stroke compared to the CG. Sensitivity exclusion analysis showed that no study significantly affected the pooled results of MIP and MEP after excluding the study one by one.
Three studies [6, 22, 48] performed IMT + EMT, while three studies [45, 46, 49] only carried out IMT. The subgroup analysis showed a statistically improvement in MIP for IMT + EMT (n = 162, MD = 9.78, 95%CI: 5.96-13.60, p <0.00001, I2 = 1%) and IMT (n = 147, MD = 11.60, 95%CI: 8.15–15.05, p<0.00001, I2 = 11%) (Fig. 3). Similarly, the subgroup analysis also displayed a statistically increase in MEP for IMT + EMT (n = 162, MD = 11.61, 95%CI: 3.80–19.43, p = 0.004, I2 = 66%) and IMT (n = 147, MD = 7.06, 95%CI: 3.50–10.62, p = 0.0001, I2 = 0%) (Fig. 4). Sensitive exclusion analysis suggested that no study significantly affected the pooled results of MIP for IMT+EMT and IMT. However, the pooled result of MEP for IMT + EMT wasnot statistically significant through excluding the study of Messaggi-Sartor et al [48]. There was no statistically significant difference between IMT + EMT and IMT in improving MIP (p = 0.49) (Fig. 3) and MEP (p = 0.30) (Fig. 4).
Effect of respiratory muscle training on pulmonary function
Six studies [6, 43,44,45,46,47] measured the results about pulmonary function. These studies all analyzed FVC and PEF. Five studies reported FEV1 except for the study of Gu et al [45]. The pooled data suggested that RMT produced a statistically significant increase in FVC (n = 325, MD = 0.82, 95%CI: 0.54–1.10, p < 0.00001, I2 = 58%) (Fig. 5), PEF (n = 325, MD = 1.28, 95%CI: 0.94–1.63, p < 0.00001, I2 = 50%) (Fig. 6) and FEV1 (n = 265, MD = 1.36, 95%CI: 1.13–1.59, p < 0.00001, I2 = 61%) (Fig. 7) for patients with early stroke compared to the CG. Sensitivity analysis for pulmonary function variables showed that no study significantly influenced the pooled results of pulmonary function when studies were removed one by one.
Four studies [6, 43, 44, 47] performed IMT + EMT for FVC, PEF and FEV1, while only one studies [46] carried out IMT for FEV1 and two studies [45, 46] conducted IMT for FVC and PEF. The subgroup analysis indicated that IMT + EMT had a statistically improvement in FVC (n = 220, MD = 0.87, 95%CI: 0.47–1.27, p < 0.0001, I2 = 68%) (Fig. 5), PEF (n = 220, MD = 1.51, 95%CI: 1.22–1.80, p < 0.00001, I2 = 14%) (Fig. 6) and FEV1 (n = 220, MD = 0.76, 95%CI: 0.41–1.11, p < 0.0001, I2 = 54%) (Fig. 7). Sensitive exclusion analysis indicated that no study significantly affected these results. The subgroup analysis also indicated that IMT produced a statistically increase in FVC (n = 105, MD = 0.71, 95%CI: 0.21–1.21, p = 0.006, I2 = 58%) (Fig. 5), PEF (n = 105, MD = 0.84, 95%CI: 0.37–1.31, p = 0.0005, I2 = 0%) (Fig. 6) and FEV1 (n = 45, MD = 0.40, 95%CI: 0.08–0.72, p = 0.02) (Fig. 7). Sensitive exclusion analysis suggested that no study significantly affected the pooled result of PEF. However, IMT did not produce a statistically significant improvement in FVC after excluding the study of Yu et al [46]. Additionally, sensitive exclusion analysis could not be conducted for FEV1 because of only one study. There was no statistically significant difference between IMT + EMT and IMT in improving FVC (p = 0.62) (Fig. 5) and FEV1 (p = 0.14) (Fig. 7), while there was a statistically significant difference between IMT + EMT and IMT in improving PEF (p = 0.02) (Fig. 6).
Effect of respiratory muscle training on functional capacity
Five studies focused on functional capacity [6, 43, 44, 46, 47]. Four studies analyzed FMA [43, 44, 46, 47], while one study [6] assessed FAC. The meta-analysis was performed with SMD due to the differences between the assessment scales. RMT produced a statistically significant improvement in functional capacity for patients with early stroke compared to the CG (n=265, SMD=0.51, 95%CI: 0.05-0.98, p=0.009, I2=65.5%) (Fig. 8). Sensitive exclusion analysis showed that RMT did not have a statistically significant increase in functional capacity when the studies of Sun et al. [43] and Choi et al. [6]were excluded separately.
Four studies [6, 43, 44, 47] performed IMT + EMT, while only one studies [46] carried out IMT. The subgroup analysis showed that IMT + EMT had a statistically significant effect on improving functional capacity (n = 220, SMD = 0.61, 95%CI: 0.08–1.13, p = 0.01, I2 = 72) (Fig. 8). Sensitive exclusion analysis indicated that IMT + EMT did not produce a statistically significant improvement in functional capacity after excluding the studies of Sun et al. [43] and Choi et al. [6] respectively. On the contrary, IMT did not show a statistically significant improvement in motor function (n = 45, SMD = 0.12, 95%CI: -0.46–0.71, p = 0.69) (Fig. 8). Sensitive exclusion analysis could not be performed due to only one study. There was no statistically significant difference between IMT + EMT and IMT in improving functional capacity (p = 0.22) (Fig. 8).
Discussion
This meta-analysis summarizes and analyzes the available evidence on the effects of RMT in patients with early stroke. This study provides good-quality evidence that RMT can improve respiratory muscle strength (MIP, MEP), pulmonary function (FVC, PEF, FEV1), and functional capacity in early stroke patients. Therefore, RMT can be considered an effective intervention for early-stage stroke patients.
Subgroup analysis showed that IMT + EMT was beneficial to the recovery of respiratory muscle strength (MIP and MEP), pulmonary function (FVC, PEF, FEV1), and functional capacity, while IMT could improve respiratory muscle strength (MIP and MEP) and pulmonary function (FVC, PEF, FEV1). Furthermore, subgroup analyses did not show significant differences between IMT + EMT and IMT interventions, except in PEF. IMT + EMT had a greater effect on PEF improvement than IMT alone. These seem to suggest that IMT + EMT can promote functional recovery in early stroke patients more than IMT alone. However, due to the limited number of studies on IMT + EMT and IMT when performing subgroup analysis, more RCTs are still needed to conduct research in this direction.
Respiratory muscle strength
This study found that RMT significantly improved MIP and MEP in patients with early stroke, which is similar to the results of most previous reviews [17, 23,24,25,26,27,28]. However, Xiao et al. [8] found that there is insufficient evidence to support that RMT can improve respiratory muscle strength in stroke patients. This may be related to the insufficient literature included in their research and no separate study on early stroke patients. Moreover, IMT + EMT and IMT also improved MIP and MEP. Early stroke patients may have decreased respiratory muscle strength due to respiratory centre injury and central diaphragm dysfunction [12, 29, 53, 54], while RMT may improve the integration and regulation of respiratory-related sensory input by promoting the recovery of cerebral cortex respiratory centre [9, 53] and activating cortical spinal cord pathway [12, 55], thereby improving diaphragm function and respiratory muscle strength. Furthermore, RMT is more likely to change the adaptive structure of respiratory muscle [56] in patients with early stroke, thereby improving the strength of respiratory muscle. However, our previous study only found that RMT improved MIP in patients with chronic stroke without affecting MEP. This indicates that RMT may have different effects on stroke patients between early and chronic stages. This may be related to the easier recovery of central nervous system plasticity within three months [11], which means that RMT is more likely to promote the recovery of respiratory muscles in early stroke patients, while RMT may be relatively difficult to promote the improvement of the respiratory muscle in chronic stroke patients. Another possibility may be the limited number of studies investigating the effects of RMT on MEP in stroke patients between early and chronic stages. Therefore, more RCTs are still needed to study the effects of respiratory muscle training on MEP in stroke patients at different stages.
Pulmonary function
The meta-analysis showed that RMT had a significant influence on FVC, PEF, and FEV1 in patients with early stroke. This finding is supported by the previous reviews [17, 23, 25, 26, 28]. Similarly, IMT + EMT and IMT also improved FVC, PEF, and FEV1. However, only PEF was different under the intervention of IMT + EMT and IMT. The effect of IMT + EMT on the improvement of PEF was greater than IMT alone. Early stroke patients may experience reduced the expansion of lung and chest wall, harden chest, reduce the compliance of chest wall, and change in the elastic properties of lung tissue because of respiratory muscle weakness, which can affect the lung volume, flow reduction and restrictive ventilation mode of early stroke patients [15, 27, 57,58,59]. RMT may improve pulmonary ventilation function by increasing respiratory muscle strength and thoracic expansion [13, 59, 60], inhibiting the weakening of lung tissue elasticity caused by limited mobility after early stroke [61,62,63]. Additionally, it may be because RMT has a pump effect on blood circulation [46], namely, diaphragm movement can promote the venous return to reduce pulmonary blood stasis, increase alveolar ventilation, and effectively exchange gas [64, 65]. However, our previous meta-analysis found that RMT did not improve FVC but improved PEF and FEV1 in chronic stroke patients. This may be related to several main reasons. The recovery of neurological function in chronic stroke patients is relatively stable [11, 66, 67], and therefore it may require the long duration and strong intensity of RMT to improve the muscle tension of the hemiplegic side chest wall and reduce spasms, thereby improving the elasticity of the lungs and thorax. Moreover, we also did not observe that RMT improved MEP during the chronic phase. It is possible that only the changes of MIP are not enough to improve the elastic recoil effect of lung tissue in the chronic phase, and thus no changes in FVC are observed. Compared with early stroke, because it is in the early stage of neurological recovery, RMT is more likely to improve respiratory muscle activity and the elasticity of the lung and thorax, thereby enhancing FVC, PEF, and FEV1.
Functional capacity
The meta-analysis still found that RMT showed a positive effect on functional capacity in patients with early stroke. Previous systematic reviews [17, 23,24,25, 27] reported a similar result, although these studies mixed early and chronic stroke patients. Furthermore, IMT + EMT was helpful for functional capacity recovery, while IMT did not. However, this finding should be interpreted with caution due to the insufficient number of studies on IMT. The reduction of inspiratory muscle and expiratory muscle in early stroke patients can affect the recovery of motor function [68, 69]. Therefore, the improvement of inspiratory and expiratory muscle strength is important for functional ability in early stroke patients. RMT can enhance the oxygen-carrying capacity of respiratory muscle by increasing the respiratory muscle strength and lung function, and improve indirectly the exercise tolerance and function of early stroke patients [70,71,72]. However, in our previous study, we did not find any effect of RMT on functional abilities in patients with chronic stroke. This may be because the neurological function of patients with chronic stroke recovers slowly, and the duration and intensity of RMT are not sufficient to improve motor function [66, 67, 73]. Moreover, compared with the early stage, stroke patients at this stage are relatively less motivated [74, 75]. Another possibility is related to the limited number of included high-quality RCTs. Therefore, more RCTs are needed to explore the effects of RMT and different modalities of RMT on motor function in patients with early and chronic stroke.
Clinical implications and study limitations
The currently available evidence seems to support the use of RMT in early stroke patients. Therefore, it is recommended to perform RMT as soon as possible for early stroke, so as to promote respiratory function and motor function. IMT + EMT combined training can be considered when performing RMT to achieve maximum functional recovery.
However, other aspects of this evidence still need to be considered in clinical practice. Firstly, the nine studies included were primarily placed in China, Korea, Spain, and Britain. Differences in stroke disability rates, participant demographics, medical level, and degree of patient rehabilitation cooperation across countries may reduce the generality of the findings, which should be considered in clinical use. Besides, given the limited number of high-quality studies available, only 9 RCTs were extracted and synthesized in this study. Not all studies reported the same variables. Therefore, the total number of participants included in each variable of the study may be insufficient, which can lead to minor trial bias. When performing subgroup analyses, partial results should be considered with caution as in some cases only 1 or 2 studies were included.
Moreover, only three studies reported the initial MIP and MEP, while patients with respiratory muscle weakness may generally respond better. Most of the included studies conducted RMT intervention based on conventional rehabilitation treatment, and increased overall activity levels may cause the superposition of treatment effects. These can affect the validity of the results. Additionally, the included studies were heterogeneous in intervention details, duration of intervention, and outcome collection, which may limit the strength of the synthesis of results. Finally, several interesting variables like respiratory muscle endurance, dyspnea fatigue, and walking ability were not present in the included studies, and RMT may help improve these variables in patients with early stroke. Thus, more clinical trials are needed to investigate whether RMT has an effect on these indicators in patients with early stroke.
Conclusions
This study provides good-quality evidence that RMT is effective in improving respiratory muscle strength (MIP, MEP), pulmonary function (FVC, PEF, FEV1), and functional capacity for patients with early stroke. For different RMT modalities, IMT + EMT seems to promote functional recovery in patients with early stroke more than IMT alone. High-quality, large-scale RCTs are needed to study the most appropriate characteristics of RMT (like IMT and EMT alone or combined, optimal dose, duration and outcome) in patients with early stroke to achieve the best clinical curative effect.
Availability of data and materials
Not applicable.
Abbreviations
- RCTs:
-
Randomised control trials
- PEDro:
-
The physical therapy evidence database
- PICOS:
-
Population-Interventions-Comparison-Outcomes of interest-Study design
- IG:
-
Intervention Group
- CG:
-
Control Group
- RMT:
-
Respiratory muscle training
- IMT:
-
Inspiratory muscle training
- EMT:
-
Expiratory muscle training
- MIP:
-
Maximal Inspiratory Pressure
- MEP:
-
Maximal Expiratory Pressure
- PEP:
-
Positive Expiratory Pressure
- FVC:
-
Forced Vital Capacity
- FEV1:
-
Forced Expiratory Volume in 1 s
- FIM:
-
Functional independence measure
- FAC:
-
Functional Ambulation Category
- MD:
-
Mean differences
- SMD:
-
Standard mean differences
- 95%CI:
-
95% Confidence interval
- JBI:
-
The Joanna Briggs Institute
- NR:
-
Not reported
References
Kritikou P, Vemmos K, Payne KA. In-patient hospital costs of stroke: a focused literature review. Value Health. 2014;17(7):A502.
Feigin VL, Nguyen G, Cercy K, et al. Global, regional, and country-specific lifetime risks of stroke, 1990 and 2016. N Engl J Med. 2018;379(25):2429–37.
Phipps MS, Cronin CA. Management of acute ischemic stroke. BMJ. 2020;368:l6983.
Catalá-Ripoll JV, Monsalve-Naharro J, Hernández-Fernández F. Incidence and predictive factors of diaphragmatic dysfunction in acute stroke. BMC Neurol. 2020;20(1):79.
Stinear CM, Lang CE, Zeiler S, Byblow WD. Advances and challenges in stroke rehabilitation. Lancet Neurol. 2020;19(4):348–60.
Choi HE, Jo GY, Do HK, On CW. Comprehensive respiratory muscle training improves pulmonary function and respiratory muscle strength in acute stroke patients. J Cardiopulm Rehabil Prev. 2021;41(3):166–71.
Ghoreyshi Z, Nilipour R, Bayat N, Nejad SS, Mehrpour M, Azimi T. The Incidence of Aphasia, Cognitive Deficits, Apraxia, Dysarthria, and Dysphagia in Acute Post Stroke Persian Speaking Adults. Indian J Otolaryngol Head Neck Surg. 2022;74(Suppl 3):5685–95.
Xiao Y, Luo M, Wang J, Luo H. Inspiratory muscle training for the recovery of function after stroke. Cochrane Database Syst Rev. 2012;2012(5):Cd009360.
Liu J, Ren H, Yu Y, Chen Z, Xu K. Pulmonary rehabilitation after stroke. Physikalische Medizin, Rehabilitationsmedizin, Kurortmedizin. 2017;27(06):329–34.
Patel J, Fluet G, Qiu Q, et al. Intensive virtual reality and robotic based upper limb training compared to usual care, and associated cortical reorganization, in the acute and early sub-acute periods post-stroke: a feasibility study. J Neuroeng Rehabil. 2019;16(1):92.
Hebert D, Lindsay MP, McIntyre A, et al. Canadian stroke best practice recommendations: stroke rehabilitation practice guidelines, update 2015. Int J Stroke. 2016;11(4):459–84.
Khedr EM, El Shinawy O, Khedr T, Aziz Ali YA, Awad EM. Assessment of corticodiaphragmatic pathway and pulmonary function in acute ischemic stroke patients. Eur J Neurol. 2000;7(3):323–30.
Jo MR, Kim NS. Combined respiratory muscle training facilitates expiratory muscle activity in stroke patients. J Phys Ther Sci. 2017;29(11):1970–3.
Naghavi FS, Koffman EE, Lin B, Du J. Post-stroke neuronal circuits and mental illnesses. Int J Physiol Pathophysiol Pharmacol. 2019;11(1):1.
Jung JH, Kim NS. The effect of progressive high-intensity inspiratory muscle training and fixed high-intensity inspiratory muscle training on the asymmetry of diaphragm thickness in stroke patients. J Phys Ther Sci. 2015;27(10):3267–9.
Sutbeyaz ST, Koseoglu F, Inan L, Coskun O. Respiratory muscle training improves cardiopulmonary function and exercise tolerance in subjects with subacute stroke: a randomized controlled trial. Clin Rehabil. 2010;24(3):240–50.
Wu F, Liu Y, Ye G, Zhang Y. Respiratory muscle training improves strength and decreases the risk of respiratory complications in stroke survivors: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2020;101(11):1991–2001.
Tong X, Kuklina EV, Gillespie C, George MG. Medical complications among hospitalizations for ischemic stroke in the United States from 1998 to 2007. Stroke. 2010;41(5):980–6.
Illi SK, Held U, Frank I, Spengler CM. Effect of respiratory muscle training on exercise performance in healthy individuals: a systematic review and meta-analysis. Sports Med. 2012;42(8):707–24.
Forbes S, Game A, Syrotuik D, Jones R, Bell GJ. The effect of inspiratory and expiratory respiratory muscle training in rowers. Res Sports Med. 2011;19(4):217–30.
Britto RR, Rezende NR, Marinho KC, Torres JL, Parreira VF, Teixeira-Salmela LF. Inspiratory muscular training in chronic stroke survivors: a randomized controlled trial. Arch Phys Med Rehabil. 2011;92(2):184–90.
Guillén-Solà A, Messagi Sartor M, Bofill Soler N, Duarte E, Barrera MC, Marco E. Respiratory muscle strength training and neuromuscular electrical stimulation in subacute dysphagic stroke patients: a randomized controlled trial. Clin Rehabil. 2017;31(6):761–71.
Gomes-Neto M, Saquetto MB, Silva CM, Carvalho VO, Ribeiro N, Conceição CS. Effects of respiratory muscle training on respiratory function, respiratory muscle strength, and exercise tolerance in patients poststroke: a systematic review with meta-analysis. Arch Phys Med Rehabil. 2016;97(11):1994–2001.
Menezes KK, Nascimento LR, Ada L, Polese JC, Avelino PR, Teixeira-Salmela LF. Respiratory muscle training increases respiratory muscle strength and reduces respiratory complications after stroke: a systematic review. J Physiother. 2016;62(3):138–44.
Menezes KK, Nascimento LR, Avelino PR, Alvarenga MTM, Teixeira-Salmela LF. Efficacy of interventions to improve respiratory function after stroke. Respir Care. 2018;63(7):920–33.
Pozuelo-Carrascosa DP, Carmona-Torres JM, Laredo-Aguilera JA, Latorre-Román P, Párraga-Montilla JA, Cobo-Cuenca AI. Effectiveness of respiratory muscle training for pulmonary function and walking ability in patients with stroke: a systematic review with meta-analysis. Int J Environ Res Public Health. 2020;17(15):5356.
Fabero-Garrido R, Del Corral T, Angulo-Díaz-Parreño S, et al. Respiratory muscle training improves exercise tolerance and respiratory muscle function/structure post-stroke at short term: a systematic review and meta-analysis. Ann Phys Rehabil Med. 2021;65(5):101596.
Zhang X, Zheng Y, Dang Y, et al. Can inspiratory muscle training benefit patients after stroke? A systematic review and meta-analysis of randomized controlled trials. Clin Rehabil. 2020;34(7):866–76.
Pollock RD, Rafferty GF, Moxham J, Kalra L. Respiratory muscle strength and training in stroke and neurology: a systematic review. Int J Stroke. 2013;8(2):124–30.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Wood L, Egger M, Gluud LL, et al. Empirical evidence of bias in treatment effect estimates in controlled trials with different interventions and outcomes: meta-epidemiological study. BMJ. 2008;336(7644):601–5.
Jüni P, Altman DG, Egger M. Systematic reviews in health care: Assessing the quality of controlled clinical trials. BMJ. 2001;323(7303):42–6.
Charrois TL. Systematic reviews: what do you need to know to get started? Can J Hosp Pharm. 2015;68(2):144–8.
Jordan Z, Munn Z, Aromataris E, Lockwood C. Now that we’re here, where are we? The JBI approach to evidence-based healthcare 20 years on. JBI Evid Implement. 2015;13(3):117–20.
Higgins JPT, Thomas J, Chandler J, et al. Cochrane Handbook for Systematic Reviews of Interventions. 2nd Edition. Chichester (UK): Wiley; 2019.
Maher CG, Sherrington C, Herbert RD, Moseley AM, Elkins M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys Ther. 2003;83(8):713–21.
Moseley AM, Rahman P, Wells GA, et al. Agreement between the Cochrane risk of bias tool and Physiotherapy Evidence Database (PEDro) scale: a meta-epidemiological study of randomized controlled trials of physical therapy interventions. PLoS ONE. 2019;14(9):e0222770.
Foley NC, Teasell RW, Bhogal SK, Speechley MR. Stroke rehabilitation evidence-based review: methodology. Top Stroke Rehabil. 2003;10(1):1–7.
Gonzalez GZ, Moseley AM, Maher CG, Nascimento DP, Costa L, Costa LO. Methodologic quality and statistical reporting of physical therapy randomized controlled trials relevant to musculoskeletal conditions. Arch Phys Med Rehabil. 2018;99(1):129–36.
Huedo-Medina TB, Sánchez-Meca J, Marín-Martínez F, Botella J. Assessing heterogeneity in meta-analysis: Q statistic or I2 index? Psychol Methods. 2006;11(2):193–206.
Bown MJ, Sutton AJ. Quality control in systematic reviews and meta-analyses. Eur J Vasc Endovasc Surg. 2010;40(5):669–77.
Lin L, Chu H. Quantifying publication bias in meta-analysis. Biometrics. 2018;74(3):785–94.
Sun YL, Li X, Zhang HR, Yang S. Progressive respiratory muscle training on functional rehabilitation of stroke patients with hemiplegia. Chin Rehabil. 2021;26(01):17–20.
Liu Z, He M, Zhang QY, Li J. Effect of respiratory muscle training on pulmonary function and motor function in stroke patients with hemiplegia. Chin Med Pharm. 2022;12(03):193–6.
Gu J, Huang H, Chen Y, Zheng B. Effect of threshold pressure load breathing training on rehabilitation of patients with early stroke. Chin J Biomed Eng. 2020;26(05):449–52.
Yu CJ, Li XP, Lin Q, Cheng K, Cai YX, Zhang HH, Zhao QY, Xia P. Effect of respiratory muscle training on respiratory function of patients with subacute stroke. Chin J Phys Med Rehabil. 2016;68(10):735–9.
Yoo HJ, Pyun SB. Efficacy of bedside respiratory muscle training in patients with stroke: a randomized controlled trial. Am J Phys Med Rehabil. 2018;97(10):691–7.
Messaggi-Sartor M, Guillen-Sola A, Depolo M, et al. Inspiratory and expiratory muscle training in subacute stroke. Neurology. 2015;85(7):564–72.
Kulnik ST, Birring SS, Moxham J, Rafferty GF, Kalra L. Does respiratory muscle training improve cough flow in acute stroke? Pilot randomized controlled trial. Stroke. 2015;46(2):447–53.
Evans JA, Whitelaw WA. The assessment of maximal respiratory mouth pressures in adults. Respir Care. 2009;54(10):1348–59.
Gil Obando LM, López López A, Avila CL. Normal values of the maximal respiratory pressures in healthy people older than 20 years old in the City of Manizales - Colombia. Colomb Med (Cali). 2012;43(2):119–25.
Rodrigues-Baroni JM, Nascimento LR, Ada L, Teixeira-Salmela LF. Walking training associated with virtual reality-based training increases walking speed of individuals with chronic stroke: systematic review with meta-analysis. Braz J Phys Ther. 2014;18(6):502–12.
Jandt SR, Caballero RM, Junior LA, Dias AS. Correlation between trunk control, respiratory muscle strength and spirometry in patients with stroke: an observational study. Physiother Res Int. 2011;16(4):218–24.
de Almeida IC, Clementino AC, Rocha EH, Brandão DC, Dornelas de Andrade A. Effects of hemiplegy on pulmonary function and diaphragmatic dome displacement. Respir Physiol Neurobiol. 2011;178(2):196–201.
Similowski T, Catala M, Rancurel G, Derenne JP. Impairment of central motor conduction to the diaphragm in stroke. Am J Respir Crit Care Med. 1996;154(2 Pt 1):436–41.
Bonnevie T, Villiot-Danger JC, Gravier FE, Dupuis J, Prieur G, Médrinal C. Inspiratory muscle training is used in some intensive care units, but many training methods have uncertain efficacy: a survey of French physiotherapists. J Physiother. 2015;61(4):204–9.
Ramos SM, Silva DMD, Buchaim DV, Buchaim RL, Audi M. Evaluation of respiratory muscular strength compared to predicted values in patients with stroke. Int J Environ Res Public Health. 2020;17(3):1091.
De Troyer A, Zegers De Beyl D, Thirion M. Function of the respiratory muscles in acute hemiplegia. Am Rev Respir Dis. 1981;123(6):631–2.
Lima IN, Fregonezi GA, Melo R, et al. Acute effects of volume-oriented incentive spirometry on chest wall volumes in patients after a stroke. Respir Care. 2014;59(7):1101–7.
Song GB, Park EC. Effects of chest resistance exercise and chest expansion exercise on stroke patients’ respiratory function and trunk control ability. J Phys Ther Sci. 2015;27(6):1655–8.
Billinger SA, Coughenour E, MacKay-Lyons MJ, Ivey FM. Reduced cardiorespiratory fitness after stroke: biological consequences and exercise-induced adaptations. Stroke Res Treat. 2012;2012:959120.
Brogan E, Langdon C, Brookes K, Budgeon C, Blacker D. Respiratory infections in acute stroke: nasogastric tubes and immobility are stronger predictors than dysphagia. Dysphagia. 2014;29(3):340–5.
Brogan E, Langdon C, Brookes K, Budgeon C, Blacker D. Dysphagia and factors associated with respiratory infections in the first week post stroke. Neuroepidemiology. 2014;43(2):140–4.
Lees N, Soni N. Respiratory physiology. In: Clinical intensive care medicine. 2015. p. 41–69.
Kim J, Park JH, Yim J. Effects of respiratory muscle and endurance training using an individualized training device on pulmonary function and exercise capacity in stroke patients. Med Sci Monit. 2014;20:2543.
Hu X, Tong K, Song R, et al. Quantitative evaluation of motor functional recovery process in chronic stroke patients during robot-assisted wrist training. J Electromyogr Kinesiol. 2009;19(4):639–50.
Ripollés P, Rojo N, Grau-Sánchez J, et al. Music supported therapy promotes motor plasticity in individuals with chronic stroke. Brain Imaging Behav. 2016;10(4):1289–307.
Cho JE, Lee HJ, Kim MK, Lee WH. The improvement in respiratory function by inspiratory muscle training is due to structural muscle changes in patients with stroke: a randomized controlled pilot trial. Top Stroke Rehabil. 2018;25(1):37–43.
Kulnik ST, Rafferty GF, Birring SS, Moxham J, Kalra L. A pilot study of respiratory muscle training to improve cough effectiveness and reduce the incidence of pneumonia in acute stroke: study protocol for a randomized controlled trial. Trials. 2014;15(1):1–10.
Bausek N, Berlin T, Aldarondo S. The power and potential of respiratory muscle training. In: Respiratory equipment and devices exhibition mgazine. 2016. p. 86–96.
Aznar-Lain S, Webster AL, Cañete S, et al. Effects of inspiratory muscle training on exercise capacity and spontaneous physical activity in elderly subjects: a randomized controlled pilot trial. Int J Sports Med. 2007;28(12):1025–9.
Montemezzo D, Fregonezi GA, Pereira DA, Britto RR, Reid WD. Influence of inspiratory muscle weakness on inspiratory muscle training responses in chronic heart failure patients: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2014;95(7):1398–407.
Murphy TH, Corbett D. Plasticity during stroke recovery: from synapse to behaviour. Nat Rev Neurosci. 2009;10(12):861–72.
Last N, Packham TL, Gewurtz RE, Letts LJ, Harris JE. Exploring patient perspectives of barriers and facilitators to participating in hospital-based stroke rehabilitation. Disabil Rehabil. 2022;44(16):4201–10.
Langhorne P, Wu O, Rodgers H, Ashburn A, Bernhardt J. A Very Early Rehabilitation Trial after stroke (AVERT): a Phase III, multicentre, randomised controlled trial. Health Technol Assess. 2017;21:1–120.
Acknowledgements
Not applicable.
Registration and protocol
This meta-analysis has been registered in PROSPERO (Register number: CRD42021291918).
Funding
No funds, grants, or other support was received.
Author information
Authors and Affiliations
Contributions
YS contributed to the study conception and design. JH, YS, ZT and CS responsible for literature search and study selection. JX, YS, and YD used the PEDro score to independently assess the quality and risk of biases for 9 RCTs. YS, LH, JH and KZ independently extracted data from included 9 RCTs using standard data extraction forms. All authors took part in data synthesis and analysis. The first draft of the manuscript was written by YS and ZK. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Database search.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, YS., Zhang, K., Huang, L. et al. The effects of respiratory muscle training on respiratory function and functional capacity in patients with early stroke: a meta-analysis. Eur Rev Aging Phys Act 21, 4 (2024). https://doi.org/10.1186/s11556-024-00338-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s11556-024-00338-7