Abstract
Objectives
Regular physical activity (PA) is considered important after total hip and knee arthroplasty (THA/TKA). Objective was to systematically assess literature on recommendations given by healthcare professionals to persons after THA and TKA and to provide an overview of existing interventions to stimulate PA and sports participation.
Methods
A systematic review with a narrative synthesis including articles published between January 1995 and January 2021 reporting on recommendations and interventions. The PubMed, Embase, CINAHL and PsycInfo databases were systematically searched for original articles reporting on physical activity and sports recommendations given by healthcare professionals to persons after THA and TKA, and articles reporting on interventions/programs to stimulate a physically active lifestyle after rehabilitation or explicitly defined as part of the rehabilitation. Methodological quality was assessed with the Mixed Methods Appraisal Tool (MMAT). The review was registered in Prospero (PROSPERO:CRD42020178556).
Results
Twenty-one articles reported on recommendations. Low-impact activities were allowed. Contact sports, most ball sports, and martial arts were not recommended. One study informed on whether health-enhancing PA recommendations were used to stimulate persons to become physically active. No studies included recommendations on sedentary behavior. Eleven studies reported on interventions. Interventions used guidance from a coach/physiotherapist; feedback on PA behavior from technology; and face-to-face, education, goal-setting, financial incentives and coaching/financial incentives combined, of which feedback and education seem to be most effective. For methodological quality, 18 out of 21 (86%) articles about recommendations and 7 out of 11 (64%) articles about interventions scored yes on more than half of the MMAT questions (0–5 score).
Conclusion
There is general agreement on what kind of sports activities can be recommended by healthcare professionals like orthopedic surgeons and physiotherapists. No attention is given to amount of PA. The same is true for limiting sedentary behavior. The number of interventions is limited and diverse, so no conclusions can be drawn. Interventions including provision of feedback about PA, seem to be effective and feasible.
Similar content being viewed by others
Background
Total hip arthroplasty (THA) and total knee arthroplasty (TKA) are clinically and cost-effective pain-relieving treatments for end stage osteoarthritis, and improve the ability to stay physically active [1]. In THA and TKA the original hip or knee joint is replaced by an artificial one. After either procedure it is of the utmost importance that persons maintain or adopt a physically active lifestyle) [2, 3]. Physical activity (PA) can be defined as any bodily movement produced by skeletal muscles that requires energy expenditure [4]. Regular PA is considered to be one of the most important lifestyle behaviors affecting health. It is proven to help prevent and treat noncommunicable diseases (NCDs) such as heart disease, stroke, diabetes, and breast and colon cancer. It also helps prevent hypertension, overweight and obesity, and can improve mental health, quality of life and well-being [5]. Being physically active on a regular basis also enhances fitness. Fitness is positively associated with functional autonomy in older adults [6]. Additionally, after THA and TKA individuals can benefit from being physically active as there are indications that this results in lower fall risk, increased bone density, improved prosthetic fixation and reduced risk of prosthetic loosening [2].
There are also negative consequences, one of the most important being prosthetic wear. The degree of prosthetic wear is not solely related to PA though. Both patient- and prosthesis-related factors contribute to the longevity of a prosthesis [7]. Moreover, the degree of wear depends not only on the amount of PA but also on the mechanical loading of the joint, which in turn depends on body weight, type of PA and technique (experienced or newbie athlete), where high-impact activity and poor motor control matter [8].
PA recommendations for persons after THA and TKA thus have to focus on amount and intensity of PA as well as on type of activity, including whether someone has experience with that activity. With respect to amount and intensity, the guidelines of the WHO published in 2020 can be used [9]. The most recent WHO guidelines recommend that every healthy adult (aged 18 to 65) do at least 150–300 min of moderate-intensity or at least 75–150 min of vigorous-intensity aerobic physical activity or an equivalent combination of moderate and vigorous activity throughout the week for substantial health benefits. Adults should also do muscle-strengthening activities at moderate or greater intensity that involve all major muscle groups on two or more days a week. For adults older than 65 it is recommended to add multicomponent physical activity that emphasizes functional balance and strength-training at moderate or greater intensity three or more days a week, to enhance functional capacity and to prevent falls. Lastly, it is recommended to limit the amount of time spent being sedentary. Although these recommendations are not specific for THA and TKA patients, they are also considered applicable to this patient group [2, 10].
For type of physical activity or sport after THA and TKA, a narrative review was published by Fawaz and Masri that gives an overview of activities allowed by healthcare professionals [11]. However, they did not systematically review the current literature so their overview might be missing information. The only overview of interventions or programs to enhance post-rehabilitation physical activity behavior of THA and TKA patients is that of Ishaku et al., who included papers up to November 2016. They concluded that studies showed a significant increase in time spent being physically active by participants in intervention groups compared to those in control groups [12]. However, research shows that a large group of patients remain inactive even when pain and functional deficits are gone after arthroplasty [10, 13,14,15,16]. Targeted interventions seem necessary to enhance physical activity behavior in this patient group.
The objective of this systematic review is therefore twofold: to systematically review the existing literature on recommendations given by healthcare professionals to patients after THA and TKA, and to provide an overview of existing interventions/programs described in the literature to stimulate a physically active lifestyle after THA and TKA.
Methods
Search strategy
A systematic review with a narrative synthesis was conducted. The review was registered in Prospero (PROSPERO: CRD42020178556) beforehand. A librarian of the Central Medical Library of UMCG was consulted for the search strategy. It was decided to perform one broad search strategy for both questions. The search strategy conducted is shown in Additional file 1: Appendix 1.
Study selection
The PubMed, Embase, CINAHL and PsycInfo databases were systematically searched for original articles reporting on PA and sports recommendations given by healthcare professionals to persons after THA and TKA, and articles reporting on interventions/programs to stimulate a physically active lifestyle after rehabilitation or explicitly defined as part of the rehabilitation. Included persons had to be over 18 years of age. Articles written in a language other than English, review articles, case reports and study protocols were excluded. The search was conducted on 26 March 2020, and articles were searched from January 1995 onwards; an update of the search was done on 13 January 2021 following the guidelines of Bramer et al. [17].
Studies identified by the search strategy were imported to EndNote X9 (Clarivate Analytics Endnote X9.3.1, Philadelphia) and duplicates were removed following the guidelines proposed by Bramer et al. [18]. Articles were first screened for eligibility based on title and abstract. All articles extracted by the authors were screened for full-text eligibility. The screening procedure was performed by two authors (M.S. and I.A.S.) independently, and differences were solved by discussion. When needed, a third assessor (Y.M.) was consulted. Reference lists of included articles were screened for possible eligible articles that were missed in the initial search strategy.
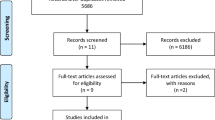
The literature search yielded 7759 articles. After removing duplicates, 5029 unique articles remained. Subsequent reading of the titles and abstracts led to exclusion of 4960 articles. Full-text was assessed in the remaining 69. Of these, 18 articles reporting on recommendations were included. The reference lists of the included articles were manually checked and three additional articles were identified, making a total of 21. With respect to articles reporting on interventions, 11 were included after full-text screening. The entire procedure was performed by two authors (M.S. and I.A.S.). Once again, a third assessor (Y.M.) was consulted when needed (for flowchart, see Fig. 1).
Data extraction and analysis
Data extraction was performed by two authors (M.S. and I.A.S.). For both research questions a separate table was created that included information about author and year, country, study design, sample size and characteristics, data collection period, type of sport/activity, measurement method and outcomes. Table 1 (first research question) includes the given recommendations and Table 2 (second research question) displays the intervention characteristics.
Quality assessment
Quality assessment was performed using the Mixed Methods Appraisal Tool (MMAT) v. 2018 [51]. The MMAT is a critical appraisal tool designed to be used in reviews including qualitative, quantitative and mixed-method articles. For each of the five different study designs the MMAT comprises, it has five questions to determine whether the risk of bias on a certain aspect is low. If the risk of bias is low the question receives a “yes”, otherwise a “no”, and when it is not clearly described it receives a “can’t tell”. Since calculating a total score has been discouraged, it was chosen to present the ratings of the individual criteria [52]. The quality of the articles was judged by two researchers independently (M.S. and I.A.S.), and differences were solved by discussion, when needed with help of a third assessor (Y.M.).
Results
Recommendations for PA
Description of studies
Twenty-one studies [19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39] published between 1995 and 2021 were analyzed. Table 1 shows an overview of the study characteristics and results. The studies were conducted in Western countries (Western Europe and the United States), except for one study from Japan [36]. Most studies concerned the hip [19,20,21,22,23,24,25,26,27,28,29,30, 33, 35,36,37, 39], with fewer studies on the knee [21,22,23,24,25,26, 29,30,31,32,33,34,35,36,37,38].
Quality assessment
The quality of articles varied. The assessment of each article can be found in Additional file 2: Appendix 2A. Of the 21 articles included, none scored “yes” on all five questions of the MMAT, while 4 positive answers were given in five articles [23, 24, 27, 28, 35], 3 in thirteen articles [19, 20, 25, 26, 29,30,31,32,33,34, 36, 38, 39], 2 in one article [22], 1 in none of the articles, and none in two of the articles [21, 37]. There wasn’t a “no” score in ten articles [20, 23, 24, 27, 28, 30, 31, 34,35,36], while nine articles [19, 22, 26, 29, 32, 33, 37,38,39] received a “no” on one out of five questions. Further, one article [25] scored a “no” on two questions and 1 [21] on four questions. The remaining questions of the MMAT were assessed as a “can’t tell”.
Outcome
In sixteen studies [19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34] the focus was on general sports activities; in the majority of these studies self-constructed (web-based) questionnaires were used, distributed among orthopedic surgeons. One study [34] included physiotherapists. One study [27] focused on the influence of high-impact sports operationalized as a University of California, Los Angeles (UCLA) activity score of 9–10 versus low-intensity activities (UCLA score 1–4) on function, dislocation rate, linear wear and prosthetic survival. One study [26] informed on how far healthcare professionals use health-enhancing PA recommendations to stimulate persons after THA and TKA to become physically active again. No study included recommendations on sedentary behavior.
Five studies [35,36,37,38,39] focused on specific sports, two of which − including persons after THA − concerned alpine skiing and/or cross-country skiing [35, 37]. Focus was on the detrimental effect of skiing on loosening, migration and wear of the prosthesis. Two studies − one in persons after THA and one in persons after TKA − focused on tennis [38, 39]. Purpose was to characterize persons who play tennis after arthroplasty in terms of their functional abilities and degree of satisfaction. One study from Japan focused on playing golf [36] after THA. In a laboratory setting it was determined to what degree the golf swing had a detrimental effect on liner-to-neck contact and cup-head translation.
Overall, there is a general consensus on what kind of sports activities can or cannot be recommended.
Interventions
Description of studies
In total 11 articles [40,41,42,43,44,45,46,47,48,49,50] were included describing an intervention or program that aims to enhance PA behavior during or after post-THA or post-TKA rehabilitation. Three studies [40, 41, 47] had post-THA participants, seven studies [42,43,44,45,46, 48, 49] post-TKA participants, and one study [50] aimed at both populations. All studies were RCTs, apart from one case series (N = 2 persons) [47]. The sample size of the RCTs ranged from 13 to 163 persons. The 11 articles studied 13 different interventions. Table 2 shows an overview of the study characteristics.
Quality assessment
The quality of articles varied. The assessment of each article can be found in Additional file 3: Appendix 2B. Of the 11 articles [40,41,42,43,44,45,46,47,48,49,50] included, two [41, 47] scored “yes” on all five questions of the MMAT, while 4 positive answers were given in two articles [46, 50], 3 in three articles [42, 45, 49], 2 in three articles [43, 44, 48], and 1 in one article [40]. There weren’t any “no” scores in three of the articles [41, 42, 47], while six articles [43, 45, 46, 48,49,50] received a “no” on one out of five questions. Two articles [40, 44] scored a ‘no’ on two questions. The remaining questions of the MMAT received a “can’t tell”.
Outcome
The 13 interventions to enhance PA were diverse: interventions using guidance from a coach/physiotherapist (N = 4) [40,41,42,43], interventions using technology-based feedback on PA behavior (N = 3) [48,49,50], face-to-face interventions (N = 1) [45], interventions including education on PA (N = 2) [46, 47], an intervention using goal-setting (N = 1) [43], an intervention using financial incentives (N = 1) [44], and an intervention using a combination of coaching and financial incentives (N = 1) [44]. To determine the effect of the intervention most studies (N = 6) used accelerometers to assess PA behavior [43,44,45,46, 49, 50]. The UCLA activity scale was used in two studies [40, 41], the International Physical Activity Questionnaire (IPAQ) in one [47]. Two studies did not use a measure of PA behavior [42, 48]. Moment of final follow-up assessment ranged from end of intervention to five years after intervention. Next to effectiveness the feasibility of five interventions was assessed [45,46,47,48, 50], which was considered good in all cases.
Combining the results from those studies using guidance (N = 4) [40,41,42,43], feedback (N = 4) [45, 48,49,50] and education (N = 2) [46, 47], feedback and education seem to be effective in enhancing PA behavior while guidance does not seem to enhance it.
Discussion
The aim of this review was twofold: to provide an overview of PA and sports recommendations given by healthcare professionals and of existing interventions/programs to stimulate a physically active lifestyle after THA and TKA. For the first objective, 21 articles were found and in general it can be concluded that after both THA and TKA return to low-impact activities is allowed or recommended. Overall, contact sports, most ball sports (except for doubles tennis and table tennis), and sports in the martial arts category were not recommended. Interventions to enhance PA behavior were found in 11 articles, describing 13 interventions. Most interventions used guidance from a coach/therapist, with feedback about PA behavior or education as a means to enhance PA behavior, of which feedback and education seem to be the most effective.
Regarding the recommendations, the focus in the majority of the studies was on general sports activities. The number of general sports activities varied between 15 and 47, probably depending on what are considered general sports activities in the different countries. Most of the time self-constructed (web-based) questionnaires were used which were distributed among orthopedic surgeons and in one study among physiotherapists. Consensus statements were drawn based on the responses. Respondents were often members of national/international orthopedic associations or orthopedic staff at hospitals. In that sense, the outcomes and recommendations derived must be seen in the light of the PA and sports culture of the different countries, although overall it can be concluded that the line of the recommendations is more or less the same.
Contact sports and high-impact sports were discouraged: contact sports probably because of the high twisting forces as well as the large lateral and rearward forces on the joints that these activities entail [53], and high-impact sports are expected to increase wear rate and therefore negatively affect implant survivorship [27]. The UCLA score was often used to give an indication of the impact or intensity of sports activities, yet its suitability as a measure to determine intensity can be questioned: in our opinion it only gives a very rough indication. More research is needed, also with objective measurement methods, to gain more insight into the association between intensity of activity and implant survivorship.
The results of the studies (n = 5) that focused on recommendations for one specific sport were in line with the recommendations as described above, but highlighted the fact that preoperative experience with a specific sport matters. Two studies on persons after THA concerned alpine and cross-country skiing, and one golf and tennis. One study on persons after TKA concerned tennis. Especially when it comes to skiing it must be taken into account that cultural aspects too play a role, as residents of mountain regions will probably be more experienced. Tennis studies included competitive/high level players only, so results may not be representative of recreational tennis players.
With respect to applying the PA recommendations it can be concluded that only one study [26] informed the degree to which healthcare professionals use these recommendations to stimulate persons after THA and TKA to become physically active again. Although the WHO recommendations apply to the general population [9], these can also be used for persons after THA and TKA, while taking into account the pros and cons of different activities in relation to survival of the prosthesis. Not following the recommendations in usual care could be ascribed to lack of priority and knowledge. In a British study it was concluded that doctors do not pay much attention to discussing the role of PA with their patients. Contrary to tobacco use and alcohol consumption, doctors tend to under-prioritize physical inactivity [54]. Nonetheless, advising patients to meet PA recommendations is of the utmost importance, as regular PA has been indicated to improve overall health and fitness [5, 6]. While sedentary behavior is increasingly recognized as having a negative impact on health, and is added to the WHO 2020 recommendations, no studies included recommendations on limiting sedentary behavior [9].
Regarding the interventions to enhance PA behavior, the 11 studies found can be considered low. The interventions were all different in terms of content, which hampered conclusions about their effectiveness. This is in line with the results of the systematic review of Hawke et al., although they used stricter inclusion criteria [55]. On the other hand, in their review Ishaku et al. concluded that studies show a significant increase in time spent being physically active, although their number of included studies was also low [12]. Besides, not all studies in our review used PA behavior as outcome measure, they used Patient Reported Outcome Measures (PROMs) (pain, function, quality of life (QoL)) and outcome of physical functioning tests instead. In an attempt to combine our results, it seems that adding a feedback component has a positive effect on PA behavior. Most studies used feedback from a device reporting daily step count. This enables individuals to monitor their activity easily; feasibility was proven to be good. Supervised PA however does not seem to achieve better results for PA behavior. Education about a physically active lifestyle seems to enhance PA behavior, yet this conclusion is based on only two studies, one of which was a case study about only two persons. And it is not only short-term effects and feasibility of interventions which should be investigated: the long-term effect on PA is what really counts − an actual change in PA behavior. Of the included studies, the follow-up was mostly limited to a few months or even only post-intervention; only one study looked at the effect of an intervention 5 years later [41]. Overall, the only conclusion that can be drawn from this review is that more research is needed into the effectiveness of interventions aiming to enhance PA behavior in persons after THA and TKA, which is in line with the studies of Hawke et al. and Ishaku et al. [12, 55]. The lack of interventions seems to reflect the lack of attention to the long-term benefits of THA and TKA, i.e. the ability to adopt a physically active lifestyle without pain and functional limitations due to osteoarthritis.
End conclusion
Based on the outcomes of this review it can be concluded that there is a general consensus on what kinds of sports activities can or cannot be allowed or recommended, which is primarily based on consensus studies. With respect to the number of publications on interventions aiming to enhance PA behavior after THA and TKA, it must be concluded that unsatisfactory attention is given to this topic. The number of interventions aiming to enhance PA behavior is very limited and reported interventions are diverse in terms of content, so no conclusions can be drawn. Interventions including the provision of feedback about PA seem to be effective and feasible, and it is recommended to further explore their working mechanism. The methodological quality of the included studies differed considerably. More high-quality studies are needed to support the current evidence, with special attention for long-term effects of interventions on change of PA behavior.
Implications for practice
Orthopedic surgeons, physiotherapists and other healthcare professionals involved in the care of persons after arthroplasty can use the general consensus to advise persons on the kind of sports activities that are allowed or can be recommended. With respect to amount and intensity of physical activity, healthcare professionals should be encouraged to stimulate persons to comply with the WHO recommendations [9]. They should likewise give more attention to limiting sedentary behavior. Interventions using PA feedback are advised for this purpose. The recommendations issued by the WHO can be used for persons after THA and TKA, taking into account the pros and cons of different activities in relation to survival of the prosthesis.
Availability of data and materials
The datasets used and/or analysed for the current study are available from the corresponding author upon reasonable request.
Change history
26 April 2022
A Correction to this paper has been published: https://doi.org/10.1186/s11556-022-00292-2
References
Ethgen O, Bruyere O, Richy F, Dardennes C, Reginster JY. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am. 2004;86(5):963–74. https://doi.org/10.2106/00004623-200405000-00012.
Stevens M, Reininga IH, Bulstra SK, Wagenmakers R, van den Akker-Scheek I. Physical activity participation among patients after total hip and knee arthroplasty. Clin Geriatr Med. 2012;28(3):509–20. https://doi.org/10.1016/j.cger.2012.05.003.
Konings MJ, De Vroey H, Weygers I, Claeys K. Effect of knee arthroplasty on sports participation and activity levels: a systematic review and meta-analysis. BMJ Open Sport Exerc Med. 2020;6(1):e000729. https://doi.org/10.1136/bmjsem-2019-000729.
Bull FC, Al-Ansari SS, Biddle S, Borodulin K, Buman MP, Cardon G, et al. World Health Organization 2020 guidelines on physical activity and sedentary behaviour. Br J Sports Med. 2020;54(24):1451–62. https://doi.org/10.1136/bjsports-2020-102955.
Organization WH. Global action plan on physical activity 2018–2030: more active people for a healthier world. Geneva: World Health Organization; 2018.
Nelson ME, Rejeski WJ, Blair SN, Duncan PW, Judge JO, King AC, et al. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116(9):1094–105. https://doi.org/10.1161/CIRCULATIONAHA.107.185650.
Schmalzried TP, Huk OL. Patient factors and wear in total hip arthroplasty. Clin Orthop Relat R. 2004;418:94–7. https://doi.org/10.1097/00003086-200401000-00016.
Kuster MS. Exercise recommendations after total joint replacement: a review of the current literature and proposal of scientifically based guidelines. Sports Med. 2002;32(7):433–45. https://doi.org/10.2165/00007256-200232070-00003.
Organization WH. WHO guidelines on physical activity and sedentary behaviour. WHO Guidelines on Physical Activity and Sedentary Behaviour. WHO Guidelines Approved by the Guidelines Review Committee. Geneva: World Health Organization; 2020.
Matsunaga-Myoji Y, Fujita K, Makimoto K, Tabuchi Y, Mawatari M. Three-year follow-up study of physical activity, physical function, and health-related quality of life after Total hip arthroplasty. J Arthroplasty. 2020;35(1):198–203. https://doi.org/10.1016/j.arth.2019.08.009.
Fawaz WS, Masri BA. Allowed activities after primary Total knee arthroplasty and Total hip arthroplasty. Orthop Clin North Am. 2020;51(4):441–52. https://doi.org/10.1016/j.ocl.2020.06.002.
Ishaku TMS, Hall M. Physical activity interventions after hip or knee joint replacement: a systematic review. Curr Phys Med Rehabil Rep. 2020;8(3):299–311. https://doi.org/10.1007/s40141-020-00275-3.
Wagenmakers R, Stevens M, Groothoff JW, Zijlstra W, Bulstra SK, van Beveren J, et al. Physical activity behavior of patients 1 year after primary total hip arthroplasty: a prospective multicenter cohort study. Phys Ther. 2011;91(3):373–80. https://doi.org/10.2522/ptj.20100148.
Kersten RF, Stevens M, van Raay JJ, Bulstra SK, van den Akker-Scheek I. Habitual physical activity after total knee replacement. Phys Ther. 2012;92(9):1109–16. https://doi.org/10.2522/ptj.20110273.
Smith TO, Parsons S, Fordham B, Ooms A, Dutton S, Hing C, et al. Behaviour change physiotherapy intervention to increase physical activity following hip and knee replacement (PEP-TALK): study protocol for a pragmatic randomised controlled trial. BMJ Open. 2020;10(7):e035014. https://doi.org/10.1136/bmjopen-2019-035014.
Smith TO, Mansfield M, Dainty J, Hilton G, Mann CJV, Sackley CM. Does physical activity change following hip and knee replacement? Matched case-control study evaluating physical activity scale for the elderly data from the osteoarthritis initiative. Physiotherapy. 2018;104(1):80–90. https://doi.org/10.1016/j.physio.2017.02.001.
Bramer W, Bain P. Updating search strategies for systematic reviews using EndNote. J Med Libr Assoc. 2017;105(3):285–9. https://doi.org/10.5195/jmla.2017.183.
Bramer WM, Giustini D, de Jonge GB, Holland L, Bekhuis T. De-duplication of database search results for systematic reviews in EndNote. J Med Libr Assoc. 2016;104(3):240–3. https://doi.org/10.3163/1536-5050.104.3.014.
Amstutz HC, Le Duff MJ. Effects of physical activity on long-term survivorship after metal-on-metal hip resurfacing arthroplasty: is it safe to return to sports? Bone Joint J. 2019;101-b(10):1186–91.
Bradley BM, Moul SJ, Doyle FJ, Wilson MJ. Return to sporting activity after Total hip arthroplasty-a survey of members of the British hip society. J Arthroplasty. 2017;32(3):898–902. https://doi.org/10.1016/j.arth.2016.09.019.
Clifford PE, Mallon WJ. Sports after total joint replacement. Clin Sports Med. 2005;24(1):175–86. https://doi.org/10.1016/j.csm.2004.08.009.
Healy WL, Iorio R, Lemos MJ. Athletic activity after joint replacement. Am J Sports Med. 2001;29(3):377–88. https://doi.org/10.1177/03635465010290032301.
Klein GR, Levine BR, Hozack WJ, Strauss EJ, D'Antonio JA, Macaulay W, et al. Return to athletic activity after total hip arthroplasty. Consensus guidelines based on a survey of the hip society and American Association of hip and Knee Surgeons. J Arthroplasty. 2007;22(2):171–5. https://doi.org/10.1016/j.arth.2006.09.001.
Laursen MK, Andersen JB, Andersen MM, Simonsen OH, Laursen MB. Danish surgeons allow the most athletic activities after total hip and knee replacement. Eur J Orthop Surg Traumatol. 2014;24(8):1571–7. https://doi.org/10.1007/s00590-014-1442-z.
McGrory BJ, Stuart MJ, Sim FH. Participation in sports after hip and knee arthroplasty: review of literature and survey of surgeon preferences. Mayo Clin Proc. 1995;70(4):342–8. https://doi.org/10.4065/70.4.342.
Meester SB, Wagenmakers R, van den Akker-Scheek I, Stevens M. Sport advice given by Dutch orthopaedic surgeons to patients after a total hip arthroplasty or total knee arthroplasty. Plos One. 2018;13(8).
Ollivier M, Frey S, Parratte S, Flecher X, Argenson JN. Does impact sport activity influence total hip arthroplasty durability? Clin Orthop Relat Res. 2012;470(11):3060–6. https://doi.org/10.1007/s11999-012-2362-z.
Payo-Ollero J, Alcalde R, Valentí A, Valentí JR. Lamo de Espinosa JM. Influence of total hip arthroplasty and physicians advices in the sports activity performed after the surgery. Revista espanola de cirugia ortopedica y traumatologia. 2020;64(4):251–7. https://doi.org/10.1016/j.recot.2020.02.004.
Swanson EA, Schmalzried TP, Dorey FJ. Activity recommendations after total hip and knee arthroplasty: a survey of the American Association for hip and Knee Surgeons. J Arthroplasty. 2009;24(6 Suppl):120–6. https://doi.org/10.1016/j.arth.2009.05.014.
Thaler M, Khosravi I, Putzer D, Siebenrock KA, Zagra L. Return to sports after Total hip arthroplasty: a survey among members of the European hip society. J Arthroplasty. 2020;36(5):1645–54. https://doi.org/10.1016/j.arth.2020.11.009.
Thaler M, Khosravi I, Putzer D, Hirschmann MT, Kort N, Tandogan RN, et al. Twenty-one sports activities are recommended by the European knee associates (EKA) six months after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2021;29(3):694–709. https://doi.org/10.1007/s00167-020-06400-y.
Vu-Han TL, Gwinner C, Perka C, Hardt S. Recommendations for Patients with High Return to Sports Expectations after TKA Remain Controversial. J Clin Med. 2020;10(1).
Vu-Han T, Hardt S, Ascherl R, Gwinner C. Perka C. Archives of Orthopaedic and Trauma Surgery: Recommendations for return to sports after total hip arthroplasty are becoming less restrictive as implants improve; 2020.
Witjes S, Hoorntje A, Koenraadt KL, Goossens P, Kerkhoffs GM, van Geenen RC. Considerable variety in usual care rehabilitation after knee arthroplasty : a survey amongst physiotherapists. Acta Orthop Belg. 2018;84(3):269–78.
Gschwend N, Frei T, Morscher E, Nigg B, Loehr J. Alpine and cross-country skiing after total hip replacement: 2 cohorts of 50 patients each, one active, the other inactive in skiing, followed for 5-10 years. Acta Orthop Scand. 2000;71(3):243–9. https://doi.org/10.1080/000164700317411825.
Hara D, Nakashima Y, Hamai S, Higaki H, Ikebe S, Shimoto T, et al. Dynamic hip kinematics during the golf swing after Total hip arthroplasty. Am J Sports Med. 2016;44(7):1801–9. https://doi.org/10.1177/0363546516637179.
Kloen PDMH, Marti RK. Down-hill skiing after a toatl hip replacement? Hip Int. 2000;10(2):77–82. https://doi.org/10.1177/112070000001000201.
Mont MA, Rajadhaksha AD, Marzen JL, Silberstein CE, Hungerford DS. Tennis after total knee arthroplasty. Am J Sports Med. 2002;30(2):163–6. https://doi.org/10.1177/03635465020300020301.
Mont MA, LaPorte DM, Mullick T, Silberstein CE, Hungerford DS. Tennis after total hip arthroplasty. Am J Sport Med. 1999;27(1):60–4. https://doi.org/10.1177/03635465990270011801.
Beck H, Beyer F, Gering F, Günther KP, Lützner C, Walther A, et al. Sports therapy interventions following Total hip replacement: a randomized controlled trial. Deutsches Aerzteblatt International. 2019;116(1/2):1–8. https://doi.org/10.3238/arztebl.2019.0001.
Heiberg KE, Figved W. Physical functioning and prediction of physical activity after Total hip arthroplasty: five-year Followup of a randomized controlled trial. Arthritis Care Res (Hoboken). 2016;68(4):454–62. https://doi.org/10.1002/acr.22679.
Hepperger C, Gfoller P, Hoser C, Ulmer H, Fischer F, Schobersberger W, et al. The effects of a 3-month controlled hiking programme on the functional abilities of patients following total knee arthroplasty: a prospective, randomized trial. Knee Surg Sports Traumatol Arthrosc. 2017;25(11):3387–95. https://doi.org/10.1007/s00167-016-4299-3.
Hoorntje A, Witjes S, Kuijer PPFM, Bussmann JBJ, Horemans HLD, Kerkhoffs GMMJ, et al. Does activity-based rehabilitation with goal attainment scaling increase physical activity among younger knee arthroplasty patients? Results from the randomized controlled ACTION trial. J Arthroplasty. 2020;35(3):706–11. https://doi.org/10.1016/j.arth.2019.10.028.
Losina E, Collins JE, Deshpande BR, Smith SR, Michl GL, Usiskin IM, et al. Financial incentives and health coaching to improve physical activity following Total knee replacement: a randomized controlled trial. Arthritis Care Res (Hoboken). 2018;70(5):732–40. https://doi.org/10.1002/acr.23324.
Paxton RJ, Forster JE, Miller MJ, Gerron KL, Stevens-Lapsley JE, Christiansen CL. A feasibility study for improved physical activity after Total knee arthroplasty. J Aging Phys Act. 2018;26(1):7–13. https://doi.org/10.1123/japa.2016-0268.
Piva SR, Almeida GJ, Gil AB, DiGioia AM, Helsel DL, Sowa GA. Effect of comprehensive behavioral and exercise intervention on physical function and activity participation after Total knee replacement: a pilot randomized study. Arthritis Care Res (Hoboken). 2017;69(12):1855–62. https://doi.org/10.1002/acr.23227.
Pozzi F, Madara K, Zeni JA Jr. A six-week supervised exercise and educational intervention after Total hip arthroplasty: a case series. Int J Sports Phys Ther. 2017;12(2):259–72.
Smith WA, Zucker-Levin A, Mihalko WM, Williams M, Loftin M, Gurney JG. A randomized study of exercise and fitness trackers in obese patients after Total knee arthroplasty. Orthop Clin North Am. 2019;50(1):35–45. https://doi.org/10.1016/j.ocl.2018.08.002.
Trudelle-Jackson E, Hines E, Medley A, Thompson M. Exploration of habitual walking behavior and home-based muscle power training in individuals with Total knee arthroplasty. J Phys Act Health. 2020;17(3):331–8. https://doi.org/10.1123/jpah.2019-0233.
Van der Walt N, Salmon LJ, Gooden B, Lyons MC, O'Sullivan M, Martina K, et al. Feedback from activity trackers improves daily step count after knee and hip arthroplasty: a randomized controlled trial. J Arthroplasty. 2018;33(11):3422–8. https://doi.org/10.1016/j.arth.2018.06.024.
Hong QN, Pluye P, Fabregues S, Bartlett G, Boardman F, Cargo M, et al. Improving the content validity of the mixed methods appraisal tool: a modified e-Delphi study. J Clin Epidemiol. 2019;111:49–59 e1. https://doi.org/10.1016/j.jclinepi.2019.03.008.
Hong QN, Pluye P, Fabregues S, Bartlett G, Boardman F, Cargo M, et al. Mixed Methods Appraisal Tool (MMAT), version 2018. Registration of copyright (#1148552), Canadian Intellectual Property Office, Industry Canada.
Pietschmann MF, Wohlleb L, Weber P, Schmidutz F, Ficklscherer A, Gulecyuz MF, et al. Sports activities after medial unicompartmental knee arthroplasty Oxford III-what can we expect? Int Orthop. 2013;37(1):31–7. https://doi.org/10.1007/s00264-012-1710-7.
Bates S, Kipps C. An Anonymous online survey of the views and attitudes of medical students and junior doctors towards physical activity (pa) teaching and promotion. Br J Sports Med. 2013;47(10):e3–e.
Hawke LJ, Shields N, Dowsey MM, Choong PFM, Taylor NF. Effectiveness of behavioural interventions on physical activity levels after hip or knee joint replacement: a systematic review. Disabil Rehabil. 2020;42(25):3573–80. https://doi.org/10.1080/09638288.2019.1603328.
Acknowledgements
PAIR study group: Giuseppe Barone1, Francesco Benvenuti2, Mihai Berteanu3,Laura Bragonzoni1, Ileana Ciobanu3, Dante Dallari4, Ani Dimitrova5, Ivo Dimitrov5, Jorunn L Helbostad6, Alina Iliescu7, Pasqualino Maietta Latessa1, Andreea Marin3, Alessandro Mazzotta4, Ann-Katrin Stensdotter6, Odd M Hals6, Håvard Østerås6, Cristiano Paggetti2, Erika Pinelli1, Nataliya Shalamanova5, Rumyana Shalamanova5, Claudio Stefanelli1, Matei Teodorescu3, Nikolay Todorov5, Stefania Toselli7, Maya Tsvetanova5, Monica Unsgaard-Tøndel6, Lora Yoncheva5, Raffaele Zinno1.
Institutional affiliations:
1. Department for Life Quality Studies, University of Bologna, Rimini Campus, Rimini, Italy.
2. Medea, Florence, Italy.
3. Carol Davila University of Medicine and Pharmacy, Bucharest, Romania.
4. Rizzoli Orthopaedic Institute, Bologna, Italy.
5. Know and Can Association, Bulgaria.
6. Norwegian University of Science and Technology, Trondheim, Norway.
7. Department of Biomedical and Neuromotor Science, University of Bologna, Bologna, Italy.
Funding
This study was funded by the Erasmus+ program. Application number: 613008-EPP-1-2019-1-IT-SPO-SCP.
Author information
Authors and Affiliations
Consortia
Contributions
YM; MS; IAS: Conception and design; Collection and assembly of data; Analysis and interpretation of the data; Drafting of the article; Critical revision of the article for important intellectual content; Final approval of the article; Obtaining funding. BG, BF, BM, BL, CI, DD, DA,DI, HJL, IA, MLP, MA, MA, SAK, HOM, ØH, PC, PE, SN, SR, SC, TM, TN, TS, TM, UTM, YL, ZR: Analysis and interpretation of the data; Drafting of the article; Critical revision of the article for important intellectual content; Final approval of the article; Obtaining funding.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors gave final approval of the submitted version.
Competing interests
No competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: the authors reported that given name of one of the PAIR study group members Nikolay Toselli is not correct. The correct name is “Stefania Toselli”.
Supplementary Information
Additional file 1: Appendix 1.
Search strategy.
Additional file 2: Appendix 2A.
Quality assessment recommendations.
Additional file 3: Appendix 2B.
Quality assessment interventions.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mooiweer, Y., Stevens, M., van den Akker-Scheek, I. et al. Being active with a total hip or knee prosthesis: a systematic review into physical activity and sports recommendations and interventions to improve physical activity behavior. Eur Rev Aging Phys Act 19, 7 (2022). https://doi.org/10.1186/s11556-022-00285-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s11556-022-00285-1