Abstract
Background
Both modular and monoblock tapered fluted titanium (TFT) stems are increasingly being used for revision total hip arthroplasty (rTHA). However, the differences between the two designs in clinical outcomes and complications are not yet clear. Here, we intend to compare the efficacy and safety of modular versus monoblock TFT stems in rTHA.
Methods
PubMed, Embase, Web of Science, and Cochrane Library databases were searched to include studies comparing modular and monoblock implants in rTHA. Data on the survivorship of stems, postoperative hip function, and complications were extracted following inclusion criteria. Inverse variance and Mantel–Haenszel methods in Review Manager (version 5.3 from Cochrane Collaboration) were used to evaluate differences between the two groups.
Results
Ten studies with a total of 2188 hips (1430 modular and 758 monoblock stems) were finally included. The main reason for the revision was aseptic loosening. Paprosky type III was the most common type in both groups. Both stems showed similar re-revision rates (modular vs monoblock: 10.3% vs 9.5%, P = 0.80) and Harris Hip Scores (WMD = 0.43, P = 0.46) for hip function. The intraoperative fracture rate was 11.6% and 5.0% (P = 0.0004) for modular and monoblock stems, respectively. The rate of subsidence > 10 mm was significantly higher in the monoblock group (4.5% vs 1.0%, P = 0.003). The application of extended trochanteric osteotomy was more popular in monoblock stems (22.7% vs 17.5%, P = 0.003). The incidence of postoperative complications such as periprosthetic femoral fracture and dislocation was similar between both stems.
Conclusions
No significant difference was found between modular and monoblock tapered stems as regards postoperative hip function, re-revision rates, and complications. Severe subsidence was more frequent in monoblock stems while modular ones were at higher risk of intraoperative fracture.
Level of evidence: Level III, systematic review of randomized control and non-randomized studies.
Trial Registration: We registered our study in the international prospective register of systematic reviews (PROSPERO) (CRD42020213642).
Similar content being viewed by others
Introduction
With the rapidly increasing number of primary total hip arthroplasties (THAs), there is a concomitant requirement for revision THA (rTHA). Failed THA generally occurs with some extent of femoral, especially proximal, bone defect, limiting the potential of bone ingrowth and rendering adequate fixation of the stem in the revision procedure quite challenging. Different femoral implants have been developed, based on different concepts of modularity and fixation, and have obtained remarkable clinical outcomes and survivorship. The earliest solution was an extensively porous-coated monoblock cylindrical cobalt-chrome stem, which was the gold standard in revision THA in North America for a few decades [1, 2]. This stem, implementing the traditional concept of “scratch fit,” relies on distal fixation at the femoral isthmus and bypasses bone-deficient regions in the metaphysis [3]. Though this stem has provided considerable long-term survivorship (88–96.5% at 10 years) in femoral revision [3,4,5], there remain concerns regarding the relatively high incidence of intraoperative fracture, thigh pain, and stress shielding of the proximal femur. Additionally, torsional remodeling of the proximal femur after primary THA (usually varus and retroversion) will not allow independent adjustment of femoral anteversion when this stem is used, as the bow restricts the prosthetic position. Proper anteversion may not be achieved. In the setting of severe femoral bone deficiency (Paprosky type IV), due to insufficient isthmic support (4–5 cm), the survival of the stem deteriorated, with a mechanical failure rate of 37.5% [6].
The tapered fluted monoblock titanium stem was developed to mitigate these defects. The stem, which engages a relatively short diaphyseal cortex, achieves both axial and rotational stability through tapered geometry and sharp longitudinal flutes. With a lower modulus of elasticity compared with cobalt-chrome, titanium decreases the modulus mismatch between the stem and the host bone, resulting in less thigh pain and less proximal femoral stress shielding [7, 8]. Owing to the conical body design, adjustment of the stem version can be conducted easily. Previous studies have shown tapered stems could provide superior initial fixation stability compared with cylindrical stems in the scenario of severe bone loss, and present promising clinical results [9, 10]. However, the risk of early stem subsidence and sequent hip instability exists.
A modular design of fluted tapered titanium stem was then developed to counter these concerns and provide greater intraoperative flexibility. In the modular stem procedure, the proximal and distal femur are prepared independently. Immediate stability can be permitted with distal fixation. Meanwhile, optimization of hip biomechanics including offset restoration, leg length correction, and stem version adjustment can be achieved with the proximal body of varying options, intraoperatively. When compared with an extensively porous-coated monoblock cylindrical cobalt-chrome stem, the tapered fluted modular titanium stem yielded improved outcomes [11, 12]. But there are several disadvantages when using modular devices, such as intraoperative fractures, modular junction fatigue fracture, corrosion, and higher implant cost.
Some researchers have compared the differences between modular and monoblock tapered fluted titanium stems and the results are still uncertain. In the study published by Cohn et al. [13], the postoperative Harris Hip Score (HHS) of revision patients in the modular group was 70.7 versus 73.9 in the monoblock group, while Yacovelli et al. reported a postoperative Hip dysfunction and Osteoarthritis Outcome Score for Joint Replacement (HOOS, JR.) of 74.3 in the modular group versus 63.8 in monoblock group, although the two studies showed no statistical significance [14]. Koutalos et al. [15] performed a systematic review to compare the clinical outcomes between the two stems and found that the tapered fluted monoblock titanium stem could provide similar clinical results to the modular stem, but all of the studies involved in their research were with observational cohort design, rather than comparative cohort studies, making the conclusion not rigorous enough.
Therefore, we carried out the present systematic review and meta-analysis to compare the principal complications and clinical outcomes of the two main types of revision hip stems directly after the procedure.
Material and methods
Study description
We registered our study in the International Prospective Register of Systematic Reviews (PROSPERO) (CRD42020213642). This work was conducted in line with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) and AMSTAR (Assessing the methodological quality of systematic reviews) Guidelines [16, 17].
Search strategy and eligibility criteria
PubMed, Embase, Web of Science, and Cochrane Library databases were searched in October 2022. The search terms are listed in Table 1. We developed specific search strategies for each database and references of the identified studies were checked for potential eligibility.
The following inclusion criteria were used to identify eligible studies: publications reporting on the outcome of modular and monoblock fluted tapered stems in hip revision surgeries; comparative study design; follow-up duration > 2 years. Furthermore, we excluded non-English language reports, case reports, conference abstracts/posters, or reviews. After the removal of duplicates, two orthopedic surgeons independently reviewed the titles and abstracts to screen for potentially eligible studies. Full texts were then assessed independently by the same two reviewers to identify the final list of publications suitable for inclusion in the current study. If disagreement occurred, a third senior orthopedic surgeon was consulted for final assessment and consensus. The flow diagram for the identification of studies is summarized in Fig. 1.
Data extraction
After the final list of included studies was set, data were extracted, including information on the publication, patient attributes, and operative and postoperative information. The primary outcomes of interest were the survivorship of stems and the follow-up postoperative hip function (Harris Hip Score, HHS). Intraoperative complications and postoperative complications were extracted as secondary outcomes. If the necessary information could not be extracted from the original paper, we contacted the corresponding author to request additional information.
Quality assessment
The quality of the included studies was assessed independently by two reviewers. In this regard, the Newcastle–Ottawa Scale (NOS) for cohort studies was used [18]. When disagreement occurred, a third senior orthopedic surgeon was consulted for final consensus.
Statistical analysis
Review Manager (version 5.3 from Cochrane Collaboration) was used to perform the statistical analysis, with P < 0.05 as a threshold of statistical significance. For continuous data with standard deviation, meta-analysis was performed to calculate the weighted mean difference (WMD) with 95% confidence intervals (CIs) using the inverse variance (IV) method. When comparing the incidence of dichotomous data, such as revision or complications, the odds ratio (OR) was calculated using the Mantel–Haenszel (M–H) method. We used the I2 statistic and Q test to measure heterogeneity. If I2 < 50% and the p-value for the Q test > 0.05, the studies were interpreted as minimally heterogeneous, and a fixed-effects model was applied for the meta-analysis. A random-effects model was applied when I2 > 50% or the p-value for the Q test was < 0.05, which indicated that the data were of high heterogeneity. Other results were presented as a descriptive summary.
Results
Overview of search results
There were 633 studies identified in the initial search. After excluding duplications and non-English publications, 346 studies were further assessed by the titles, abstracts, and full-text review for eligibility. As a result, 10 studies were included in the final analysis (Fig. 1). All of these studies were retrospective cohort designs. A total of 1430 hips with modular stems (modular group) and 758 hips with monoblock stems (monoblock group) were identified. Paprosky type III was the most common type of femoral bone defect in the modular group (62%, 600/966) and monoblock group (59%, 375/631), respectively. The main reason for the revision was aseptic loosening. The average age of patients ranged from 78 to 87.4 years old. The characteristics of the patients in the two groups are summarized in Table 2. Patients in all 10 studies were followed up for more than 2 years (2.5 to 8.5 years). In each study, the duration of follow-up was comparable between the two groups (Table 2). The primary and secondary outcomes of included studies are shown in Table 3.
Risk of bias in studies
Designs of all the included studies were cohort studies and most of them had excellent selection quality of patients, good comparability between groups, and reasonable assessment of outcomes, as shown in Additional file 1: Table S1.
Re-revisions
The re-revision rate for any reason was reported in 6 studies and the pooled data showed no statistical difference between the two groups [Modular group: 112/1088 (10.3%) vs Monoblock group: 50/526 (9.5%); OR = 0.95; 95% CI 0.66 to 1.38; P = 0.80; Heterogeneity: I2 = 35%, P = 0.17] (Fig. 2a). The pooled re-revision rate for aseptic reasons was also comparable between the two groups [Modular group: 81/1088 (7.4%) vs Monoblock group: 34/526 (6.5%); OR = 0.96; 95% CI 0.62 to 1.48; P = 0.84; Heterogeneity: I2 = 32%, P = 0.20] (Fig. 2b).
Postoperative hip function
Seven studies reported postoperative hip function estimation and data from 5 studies could be further pool-analyzed with the scale of HHS. The postoperative HHS in the modular and monoblock groups ranged from 70.7 to 86.4 points (weighted mean: 85.77), and from 73.1 to 86.2 points (weighted mean: 85.34), respectively. The difference between the two groups was insignificant (WMD = 0.43; 95% CI − 0.42 to 1.29; P = 0.32; Heterogeneity: I2 = 0%; P = 0.46) (Fig. 3).
Construction strategy
Five studies reported the intraoperative application of extended trochanteric osteotomy (ETO) and the pooled analysis showed that ETO was more frequently utilized in the monoblock group [122/699 (17.5%) vs 112/494 (22.7%); OR = 0.63; 95% CI 0.46 to 0.85; P = 0.003; Heterogeneity: I2 = 27%, P = 0.24] (Fig. 4a).
Three studies reported the intraoperative application of strut allograft and the pooled analysis showed no difference [Modular group: 52/472 (11.0%) vs Monoblock group: 41/287 (14.3%); OR = 1.03; 95% CI 0.50 to 2.13; P = 0.94; Heterogeneity: I2 = 52%, P = 0.12] (Fig. 4b).
Complications
Intraoperative fracture data were reported in 4 studies and the pooled analysis showed the modular group had a higher incidence [51/438 (11.6%) vs 18/360 (5.0%); OR = 2.72; 95% CI 1.57 to 4.71; P = 0.0004] (Fig. 5a). Five studies reported the incidence of postoperative periprosthetic femoral fracture and the pooled estimation reflected no statistical difference [Modular group: 12/663 (1.8%) vs Monoblcok group: 5/423 (1.2%); OR = 1.31; 95% CI 0.50 to 3.49; P = 0.58] (Fig. 5b). The incidence of dislocation was reported in 8 studies and the pooled analysis also showed no difference [Modular group: 40/1127 (3.5%) vs Monoblock group: 20/588 (3.4%); OR = 1.01; 95% CI 0.58 to 1.76; P = 0.96] (Fig. 5c). Six studies reported the incidence of aseptic loosening [Modular group: 17/1088 (1.6%) vs Monoblock group: 6/526 (1.1%); OR = 1.45; 95% CI 0.55 to 3.80; P = 0.45] (Fig. 5d) and infections [Modular group: 35/1088 (3.2%) vs Monoblock group: 23/526 (4.4%); OR = 0.73; 95% CI 0.42 to 1.29; P = 0.28], none of which showed significant difference through pooled analysis (Fig. 5e).
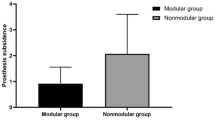
Subsidence
Five studies reported subsidence data and the pooled analysis showed comparable results with high heterogeneity (WMD = 0.13 mm; 95% CI − 0.27 to 0.52 mm; P = 0.54; Heterogeneity: I2 = 88%; P < 0.00001) (Fig. 6a). The rate of subsidence > 5 mm was also similar between the two groups [Modular group: 102/631 (16.2%) vs Monoblock group: 42/369 (11.4%); OR = 1.11; 95% = CI 0.51 to 2.43; P = 0.80; Heterogeneity: I2 = 68%, P = 0.01] through a pooled estimation of 5 studies (Fig. 6b). However, the rate of subsidence > 10 mm was significantly higher in the monoblock group [4/408 (1.0%) vs 15/336 (4.5%); OR = 0.18; 95% CI 0.06 to 0.55; P = 0.003; Heterogeneity: I2 = 0%, P = 0.46], based on the available data from 4 studies (Fig. 6c).
Discussion
The tapered fluted titanium (TFT) stem was valued in diverse common options for femoral component revisions and further studied due to prominent axial and rotational stability, ability to improve bone regeneration [27,28,29], and lower incidence of thigh pain. Monoblock TFT stems have shown promising clinical outcomes but a relatively high incidence of subsidence and dislocation. Modular TFT stems allow distal fixation of the stems for the restoration of proximal hip biomechanics. However, there remain concerns regarding the catastrophic complications associated with the fracture of junctions in modular stems. So far, several influential clinical studies have reported comparisons in clinical outcomes between these two stems. Nevertheless, published outcomes can be controversial, and whether modular or monoblock TFT stems perform better in rTHA is still a subject of interest and debate. To solve this controversy, we conducted this systematic review and meta-analysis to determine which stems would achieve fewer complications and better clinical outcomes.
In general, this analysis indicated that both modular and monoblock tapered stems revealed acceptable and comparable clinical outcomes. There was no significant difference in re-revision and complication risks between groups. Severe subsidence was more frequent in monoblock stems while modular ones were at higher risk of intraoperative fracture. This systematic review was based on cohort studies that directly compared the long-term clinical outcomes (> 2 years) of both modular and monoblock tapered stems in rTHA, and thus the evidence is of high quality.
Postoperative hip function and survivorship were similar between the modular and nonmodular groups, revealing that both of them can achieve satisfactory results for revision. However, more intraoperative fractures were detected in the modular group. Previous studies have demonstrated that the incidence of intraoperative fracture can reach 16 to 32% in modular stems [19]. A systematic review by Koutalos et al. also reflected that modular stems were associated with a higher risk of intraoperative fracture (7.6% vs 9.2%), albeit based on data from case series studies [15]. A possible reason for this result may be that the modular stems might be more popular when there is a larger bone defect, which is more vulnerable to fracture. Several researchers have recommended the prophylactic use of cerclage to prevent intraoperative fracture [30,31,32,33]. Thus, surgeons should be aware of our accumulated evidence and use the modular stems with caution.
This study also found that ETO was more frequently used in the monoblock stems. Adequate exposure of the acetabulum and femur and removal of well-fixed femoral components are important in the correction of bony deformity and mechanical stability in rTHA [34]. Osteotomy of the greater trochanter is a common procedure for extensive exposure in this setting [35]. In addition, in cases with proximal femoral varus remodeling or excessive bow, ETO can ensure straight reaming and facilitate stem placement, which is usually difficult for monoblock stems. As the modularity of the proximal and distal parts of stems enables the fixation separately, it may also explain why ETO is less frequently used in modular stems. Since the ETO procedure can facilitate surgical exposure, it may also protect the bone from intraoperative fracture. Previous studies have reported that the use of ETO could reduce the risk of intraoperative fractures and perforation [34,35,36], which may be associated with a lower risk of intraoperative events in the monoblock groups, as we found in this systematic review and meta-analysis. Nevertheless, it should be noted that the risk of nonunion of ETO is reported to be as high as 15.4% [37]. Ladurner et al. believed that the nonunion of the ETO site could lead to poor osseous support, resulting in inadequate fatigue strength at the junction of the revision stem [38].
Stem subsidence can be of great importance in the clinical setting, and this concern is usually related to the use of TFT monoblock stems. Previous studies reported the rate of subsidence > 10 mm was 15–20% in rTHA with monoblock stems and most of these events occur within the first 3 months [27, 39, 40]. Especially when using the first-generation TFT monoblock stems (Wagner SL; Zimmer, Warsaw, IN), the rate of severe subsidence can reach 20% [28, 29, 41, 42]. Though TFT monoblock stems may gain secondary osteointegration and stability after subsidence, high subsidence will jeopardize hip biomechanics and lead to hip instability, leg length discrepancy, and aseptic loosening. A high heterogeneity in the pooled analysis of stem subsidence was detected in our analysis. We further conducted a subgroup analysis according to the degree of subsidence and found that a rate of subsidence > 10 mm was significantly lower in the modular group [4/408 (1.0%) vs 15/336 (4.5%); OR = 0.18; P = 0.003], which confirmed this design clinically. Currently, Sandiford et al. have reported the subsidence of the third-generation TFT monoblock stems at a mean of 2 mm [43], which indicates that the modification of stem design helps in decreasing subsidence. When using modern stems, severe subsidence may be blamed on the surgeon experience, surgical technique, bone defect severity, and under-sizing of the component [29, 44, 45]. For the clinical protocol, the modular design of TFT stems is committed to seating the stem at an appropriate depth that can restore leg length and femoral offset, and reduce subsidence with the help of modular components [46].
This study has several limitations. First, though the design of modular and monoblock stems were restricted to TFT stems, the manufacturers varied among different studies, and the bone defect also differed among studies. We failed to complete subgroup analysis due to the paucity of studies. Though mild heterogeneity of primary outcomes was observed, bias still exists. In addition, the included studies were all retrospective studies, which compromised the level of evidence for this systematic review and meta-analysis. Second, the search methodology contained bias due to the possibly unavoidable missing of relevant studies. However, we searched four main databases to identify all the comparative studies between modular and monoblock stems in rTHA. Based on the given available data, we can answer the main questions.
Conclusion
The current systematic review and meta-analysis did not detect significant differences between modular and monoblock tapered stems as regards postoperative hip function, re-revision rates, or adverse events. Severe subsidence was more frequent in monoblock stems while modular ones were at higher risk of intraoperative fracture. Therefore, more high-quality clinical studies and clinical trials with larger sample sizes are still needed to provide more solid comparison data and conclusions.
Availability of data and materials
Data yielded in our study will be made available by the authors to any qualified researchers.
References
Hamilton WG, Cashen DV, Ho H et al (2007) Extensively porous-coated stems for femoral revision: a choice for all seasons. J Arthroplasty 22:106–110
McAuley JP, Engh CA Jr (2004) Femoral fixation in the face of considerable bone loss: cylindrical and extensively coated femoral components. Clin Orthop Relat Res 429:215–221
DeRogatis MJ, Wintermeyer E, Sperring TR et al (2019) Modular fluted titanium stems in revision hip arthroplasty. J Bone Joint Surg Am 101:745–754
Weeden SH, Paprosky WG (2002) Minimal 11-year follow-up of extensively porous-coated stems in femoral revision total hip arthroplasty. J Arthroplasty 17:134–137
Lachiewicz PF, Soileau ES (2015) What is the survivorship of fully coated femoral components in revision hip arthroplasty? Clin Orthop Relat Res 473:549–554
Sporer SM, Paprosky WG (2003) Revision total hip arthroplasty: the limits of fully coated stems. Clin Orthop Relat Res 417:203–209
Konan S, Garbuz DS, Masri BA et al (2014) Non-modular tapered fluted titanium stems in hip revision surgery: gaining attention. Bone Joint J 96-B:56–59
Munro JT, Garbuz DS, Masri BA et al (2012) Role and results of tapered fluted modular titanium stems in revision total hip arthroplasty. J Bone Joint Surg Br 94:58–60
Zhang Y, Zhang Y, Sun JN et al (2020) Comparison of cylindrical and tapered stem designs for femoral revision hip arthroplasty. BMC Musculoskelet Disord 21:411
Russell RD, Pierce W, Huo MH (2016) Tapered vs cylindrical stem fixation in a model of femoral bone deficiency in revision total hip arthroplasty. J Arthroplasty 31:1352–1355
Richards CJ, Duncan CP, Masri BA et al (2010) Femoral revision hip arthroplasty: a comparison of two stem designs. Clin Orthop Relat Res 468:491–496
Garbuz DS, Toms A, Masri BA et al (2006) Improved outcome in femoral revision arthroplasty with tapered fluted modular titanium stems. Clin Orthop Relat Res 453:199–202
Cohn MR, Tetreault MW, Li J et al (2020) Is there a benefit to modularity for femoral revisions when using a splined, tapered titanium stem? J Arthroplasty 35:S278–s283
Yacovelli S, Ottaway J, Banerjee S et al (2021) Modern revision femoral stem designs have no difference in rates of subsidence. J Arthroplasty 36:268–273
Koutalos AA, Varitimidis S, Malizos KN et al (2022) Clinical, functional and radiographic outcomes after revision total hip arthroplasty with tapered fluted modular or non-modular stems: a systematic review. Hip Int 32:475–487
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg 88:105906
Bojcic R, Todoric M, Puljak L (2022) Adopting AMSTAR 2 critical appraisal tool for systematic reviews: speed of the tool uptake and barriers for its adoption. BMC Med Res Methodol 22:104
Saracco M, Ciriello V, D'Angelo F et al (2023) Do prior intra-articular injections impact on the risk of periprosthetic joint infection in patients undergoing total hip arthroplasty? A meta-analysis of the current evidences with a focus on the timing of injection before surgery. EFORT Open Rev 8:459–467
Feng S, Zhang Y, Bao YH et al (2020) Comparison of modular and nonmodular tapered fluted titanium stems in femoral revision hip arthroplasty: a minimum 6-year follow-up study. Sci Rep 10:13692
Huang Y, Shao H, Zhou Y et al (2019) Femoral bone remodeling in revision total hip arthroplasty with use of modular compared with monoblock tapered fluted titanium stems: The role of stem length and stiffness. J Bone Joint Surg Am 101:531–538
Clair AJ, Cizmic Z, Vigdorchik JM et al (2019) Nonmodular stems are a viable alternative to modular stems in revision total hip arthroplasty. J Arthroplasty 34:S292–s296
Clair AJ, Gabor JA, Patel KS et al (2020) Subsidence following revision total hip arthroplasty using modular and monolithic components. J Arthroplasty 35:S299–s303
Huang Y, Zhou Y, Shao H et al (2017) What is the difference between modular and nonmodular tapered fluted titanium stems in revision total hip arthroplasty. J Arthroplasty 32:3108–3113
Moreta J, Uriarte I, Ormaza A et al (2019) Outcomes of Vancouver B2 and B3 periprosthetic femoral fractures after total hip arthroplasty in elderly patients. Hip Int 29:184–190
Zeng M, Xie J, Li M et al (2015) Cementless femoral revision in patients with a previous cemented prosthesis. Int Orthop 39:1513–1518
Chatziagorou G, Lindahl H, Kärrholm J (2019) Surgical treatment of Vancouver type B periprosthetic femoral fractures: patient characteristics and outcomes of 1381 fractures treated in Sweden between 2001 and 2011. Bone Joint J 101-b:1447–1458
Böhm P, Bischel O (2001) Femoral revision with the Wagner SL revision stem : evaluation of one hundred and twenty-nine revisions followed for a mean of 4.8 years. J Bone Joint Surg Am 83:1023–1031
Regis D, Sandri A, Bonetti I et al (2011) Femoral revision with the Wagner tapered stem: a ten- to 15-year follow-up study. J Bone Joint Surg Br 93:1320–1326
Böhm P, Bischel O (2004) The use of tapered stems for femoral revision surgery. Clin Orthop Relat Res 148–159
Tamvakopoulos GS, Servant CT, Clark G et al (2007) Medium-term follow-up series using a modular distal fixation prosthesis to address proximal femoral bone deficiency in revision total hip arthroplasty. A 5- to 9-year follow-up study. Hip Int 17:143–149
Meek RM, Garbuz DS, Masri BA et al (2004) Intraoperative fracture of the femur in revision total hip arthroplasty with a diaphyseal fitting stem. J Bone Joint Surg Am 86:480–485
Jones RE (2004) Modular revision stems in total hip arthroplasty. Clin Orthop Relat Res 420:142–147
Tsiridis E, Haddad FS, Gie GA (2003) The management of periprosthetic femoral fractures around hip replacements. Injury 34:95–105
MacDonald SJ, Cole C, Guerin J et al (2003) Extended trochanteric osteotomy via the direct lateral approach in revision hip arthroplasty. Clin Orthop Relat Res 417:210–216
Jando VT, Greidanus NV, Masri BA et al (2005) Trochanteric osteotomies in revision total hip arthroplasty: contemporary techniques and results. Instr Course Lect 54:143–155
Park YS, Moon YW, Lim SJ (2007) Revision total hip arthroplasty using a fluted and tapered modular distal fixation stem with and without extended trochanteric osteotomy. J Arthroplasty 22:993–999
Garabano G, Gessara AM, Pesciallo CA et al (2021) Extended trochanteric osteotomy (ETO) and fluted tapered modular stems in revision hip arthroplasty. Does ETO integrity or consolidation, really matter? J Orthop 23:250–255
Ladurner A, Zurmühle P, Zdravkovic V et al (2017) Modified extended trochanteric osteotomy for the treatment of vancouver B2/B3 periprosthetic fractures of the femur. J Arthroplasty 32:2487–2495
Weber M, Hempfing A, Orler R et al (2002) Femoral revision using the Wagner stem: results at 2-9 years. Int Orthop 26:36–39
Sandiford NA, Duncan CP, Garbuz DS et al (2015) Tapered, fluted titanium stems in revision total hip arthroplasty: role and results in contemporary practice. Instr Course Lect 64:359–366
Gutiérrez Del Alamo J, Garcia-Cimbrelo E, Castellanos V et al (2007) Radiographic bone regeneration and clinical outcome with the Wagner SL revision stem: a 5-year to 12-year follow-up study. J Arthroplasty 22:515–524
Singh SP, Bhalodiya HP (2013) Results of Wagner SL revision stem with impaction bone grafting in revision total hip arthroplasty. Indian J Orthop 47:357–363
Sandiford NA, Garbuz DS, Masri BA et al (2017) Nonmodular tapered fluted titanium stems osseointegrate reliably at short term in revision THAs. Clin Orthop Relat Res 475:186–192
Isacson J, Stark A, Wallensten R (2000) The Wagner revision prosthesis consistently restores femoral bone structure. Int Orthop 24:139–142
Berry DJ (2002) Femoral revision: distal fixation with fluted, tapered grit-blasted stems. J Arthroplasty 17:142–146
Pomeroy E, Flynn SO, Grigoras M et al (2022) Subsidence of monoblock and modular titanium fluted tapered stems in revision hip arthroplasty: A retrospective multicentre comparison study. J Clin Orthop Trauma 34:102021
Acknowledgements
Not applicable.
Funding
This study was supported by special funding from the National Clinical Research Center for Orthopedics, Sports Medicine, and Rehabilitation. We declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
LJT, LWH, and XC: conceptualization; LH, ZWP, and WDF: study design, data collection and analysis; WDF: original manuscript writing; ZWP and LHY: language check, review and editing. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors received no financial or material support for the research, authorship, and/or publication of this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1
: Table S1. Newcastle–Ottawa Quality Assessment Scale (NOS) of included studies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Wang, D., Li, H., Zhang, W. et al. Efficacy and safety of modular versus monoblock stems in revision total hip arthroplasty: a systematic review and meta-analysis. J Orthop Traumatol 24, 50 (2023). https://doi.org/10.1186/s10195-023-00731-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10195-023-00731-5