Abstract
Background
Having previously shown headache disorders to be prevalent in Mongolia, here we elaborate on headache as a public-health concern in this country, reporting symptom burden and headache-attributed impaired participation at individual and societal levels, and conducting a health-care needs assessment.
Methods
The study followed the standardized methodology developed by the Global Campaign against Headache, generating a representative general-population sample through multi-level randomized cluster sampling. Participants aged 18–65 years were interviewed at unannounced household visits by interviewers administering the HARDSHIP questionnaire. Symptom burden was established through questions on frequency, duration and intensity of headache, with proportion of time in ictal state calculated from frequency and duration. Individual impaired participation was established through the HALT questionnaire, enquiring into lost time from paid and household work and from leisure activities. Symptom burden and impaired participation yesterday were also assessed in those reporting headache yesterday. Population-level estimates were derived by factoring in prevalence.
Results
The total sample included 2,043 participants. Those reporting any headache in the last year (n = 1,351) spent, on average, 9.7% of all their time with headache, losing 1.3 workdays and 2.4 household days/3 months. These losses were considerably higher among those with probable medication-overuse headache (37.5%, 3.5 workdays, 6.7 household days) or other headache on ≥ 15 days/month (H15+) (21.9%, 2.4 workdays, 5.1 household days). At population-level (including those with and without headache), 6.2–7.4% of all time was spent with headache, 3.1% with H15+; 0.8 workdays and 1.4 household days/person/3 months were lost to headache, 0.3 workdays and 0.6 household days to migraine (the biggest contributor of all headache types). Our needs assessment estimated that one third (33.2%) of the adult population of Mongolia have headache (mostly migraine or H15+) likely to benefit from health care.
Conclusion
This first population-based study on headache burden in Mongolia shows high levels of individual and societal burden, with H15 + the cause of greater burden at population level than migraine and TTH combined. Migraine, however, has the biggest impact on the nation’s productivity. From a purely economic perspective, Mongolia, with limited health resources, would probably be best served by focusing on mitigating migraine-attributed burden.
Similar content being viewed by others
Background
This manuscript continues the series of population-based studies of headache-attributed burden among adults, conducted within the Global Campaign against Headache [1,2,3,4,5,6,7,8,9,10,11,12]. It reports a study from Mongolia, a country in the Western Pacific Region (WPR). It builds upon our previously published prevalence data from this country, which showed headache disorders to be common, with a very high prevalence of disorders characterized by headache on ≥ 15 days/month (H15+) [13]. The report noted that these findings carried messages for national health policy. However, for health policy to be fully informed, both the data on associated burden and a health-care needs assessment reflecting these data were required. Our purpose here was to provide these.
This was the first such study in Mongolia, and second of its type conducted by the Global Campaign in WPR, following a study in China [9]. The findings therefore add to our knowledge and understanding of the global burden of headache.
Methods
Full details of the study design, interview process and data collection and management have been published [13]. In summary, guided by a pilot study (to ensure feasibility), a cross-sectional population-based study was conducted during August to November 2017 among randomly selected adults (18–65 years) living in Mongolia. The study used standardized methods and questionnaire developed by the Global Campaign [14, 15]. Representativeness was achieved through multi-level randomized cluster-sampling [13]. Face-to-face interviews during unannounced home visits were performed using the Headache-Attributed Restriction, Disability, Social Handicap and Impaired Participation (HARDSHIP) questionnaire [15] translated into Mongolian language following the Global Campaign’s translation protocol [16].
Headache diagnoses
After a neutral screening question (“have you had a headache in the last year”), participants were asked the diagnostic questions incorporated into HARDSHIP [15], based on ICHD-3 criteria [17]. Diagnoses made algorithmically included probable medication overuse headache (pMOH), other H15+, definite migraine, definite tension-type headache (TTH), probable migraine and probable TTH, made in that order. Definite and probable migraine, and definite and probable TTH, were combined for analyses. Only one diagnosis was made in each participant: those reporting more than one type of headache were asked to respond according to the type that was most bothersome [13].
Burden measures
Individual burden
Symptom burden was recorded in terms of headache frequency, usual duration and usual intensity of headache. Frequency was reported in days/month, and duration in hours, both treated as continuous variables. Intensity was reported as a categorical variable, “mild”, “moderate” or “severe”, and converted to a numerical scale 1–3.
From these primary measures, two secondary measures were derived: proportion of time in ictal state (pTIS) and headache-attributed lost health. pTIS was calculated as frequency*duration (with duration capped at 24 h since frequency was reported in days/month) divided by total time (30*24 hours). Lost health was estimated, in those with migraine or TTH, as pTIS*DW, where DW was the disability weight provided by the Global Burden of Disease study [18] for the ictal state of the disorder.
Enquiry included symptom burden yesterday (duration and intensity of headache) in those reporting headache yesterday (HY) [15]. pTIS yesterday was calculated as the quotient of duration and 24.
We estimated impaired participation in paid and household work over the preceding 3 months using the Headache-Attributed Lost Time (HALT) questionnaire [19]. The methodology has been described in detail [19]. Days absent from work were added to those with less than half achieved while at work, both counted as lost days. In counterbalance, any days with more than half achieved were ignored. A similar approach was applied to household work (less than half achieved equated to nothing achieved, while more than half achieved was ignored) [19]. We also counted the number of days in which leisure activity was missed.
Impaired participation yesterday in those with HY was reported more directly, as everything, more than half, less than half or nothing achieved, making no distinction between paid work, household work and leisure time. As with HALT, less than half and nothing were summed and counterbalanced by summing more than half with everything achieved.
To assess quality of life (QoL), HARDSHIP incorporated WHOQoL-8 [20]. The unitless summed score (possible range of 8–40, with higher scores indicating better QoL) was treated as a continuous variable.
Population-level burden
pTIS and headache-attributed impaired participation at population level were calculated from means at individual level, factoring in headache prevalence and adjusting for age and gender. Independent estimates were made based on 1-year and 1-day prevalences. From HALT data, separate estimates were made for the three domains of participation: work, household and leisure. From HY data, such distinction was not possible (thus reflecting overall impaired participation only).
Health-care needs assessment
We defined “need” for health care in terms of numbers likely to benefit from effective provision of health care. Accordingly, we counted everyone with H15+ (whether pMOH or other), all participants with migraine reporting headache frequency of ≥ 3 days/month, and all participants with migraine or TTH meeting at least one of the following two criteria: (a) pTIS > 3.3% (i.e., > 1 day/month) and usual intensity ≥ 2 (i.e., moderate or severe); (b) lost participation over the preceding 3 months from either paid or household work of ≥ 3 days. Double counting was avoided. Age- and gender-adjusted prevalences were calculated.
Statistics and analyses
Continuous variables were described using means, standard errors of the mean (SEMs) and medians. In comparisons between genders and between headache types, we used ANOVA tests for continuous variables, chi-squared tests for categorical variables.
Statistical analyses were performed using SPSS version 28 (SPSS, INC, Chicago, IL). We considered p < 0.05 as significant.
Results
The sociodemographic characteristics of the sample (N = 2,043), and headache prevalences, have already been reported [13]. The participating proportion was 98.3%. Males were somewhat under-represented in the sample (39.8%, vs. 49.2% in the national population in 2017 [21]), for which corrections were necessary. The crude 1-year prevalence of any headache was 66.1%, higher in females (73.3%) than males (55.4%). Age- and gender-adjusted prevalences were 23.1% for migraine, 29.1% for TTH, 5.7% for pMOH and 5.0% for other H15+ [13]. HY was reported by 20.1% (males 12.2%, females 25.3%) [13].
Individual burden
Symptom burden
Table 1 shows the measures of symptom burden by headache type and gender. Study participants with any headache spent, on average, 9.7% of all their time with headache, but, also on average, no headache type was rated more than mild-to-moderate. Migraine was more burdensome than TTH on all measures in both genders (in particular, duration and pTIS were double), although none were tested for significance (Table 1). pMOH and other H15 + were, of course, much more frequent, with commensurately higher values of pTIS. There were no gender-related differences of interest (Table 1).
Lost health, estimated using DWs for the ictal state from GBD [18], was 3.0% for migraine in both genders and 0.1% (the lower limit of estimation) for TTH (Table 1).
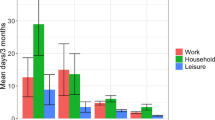
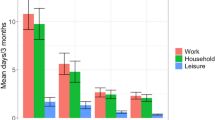
Impaired participation
Table 2 and Fig. 1 show headache-attributed impaired participation. Overall, headache of any type was associated with 1.3 lost paid workdays, 2.4 lost household workdays and 0.4 lost leisure days over the preceding 3 months. Household losses were significantly higher among females (2.7 days) than among males (1.7 days; p = 0.004). Migraine caused 3–5 times more lost days than TTH, in all three domains and in both genders (Table 2). However, pMOH and other H15 + were associated with even higher losses, pMOH particularly so among females (Table 2). Figure 1 shows clear gradients across headache types, in all domains but especially in work and household days.
Burden associated with headache yesterday
Table 3 shows symptom burden and impaired participation associated with HY (N = 409). The overall mean duration was 9.1 h, with mean intensity of 1.8 (moderate). Nonetheless, two thirds of those with HY achieved everything as normal (n = 167; 40.8%) or more than half (n = 100; 24.4%) (Table 3); hence the level of impaired participation in those with HY was 34.7%. No gender-related differences were found in any of these measures.
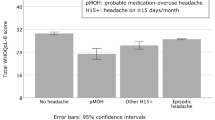
Quality of life
Table 4 and Fig. 2 show self-reported QoL according to headache status. All headache types were associated with diminished QoL, significantly except for TTH. There was a clear gradient downwards (but with, mostly, overlapping CIs) from no headache to TTH to migraine to other H15 + to pMOH.
Population-level burden
Table 5 shows pTIS and impaired participation at population level.
Based on 1-year prevalence, frequency and usual headache duration, and adjusted for age and gender, an estimated 6.2% of all time in the adult general population was spent with headache. Based on 1-day prevalence and duration of HY, this proportion increased to 7.4%. Most time was spent with pMOH (2.1%), followed by migraine (1.7%) and then TTH and other H15+ (both 1.0%).
From HALT data, impaired participation at population level was measured as 0.8 and 1.4 days/person/3 months lost from paid and household work respectively, but only 0.3 lost leisure days. Of all headache types, migraine caused the biggest losses in both paid (0.3 days) and household work (0.6 days), followed by pMOH (0.2 work and 0.3 household lost days/person/3 months). TTH and other H15 + each caused lesser detriments (0.1 work and 0.2 household lost days/person/3 months).
Based on HY data, overall impaired participation in the adult general population attributed to headache was estimated as 6.7%.
Health-care needs assessment
One third (34.4%; 703/2,041) of the participants had headache likely to benefit from health care: all those with H15+, 370 with migraine and 88 with TTH (Table 6). Adjusting for age and gender, we estimated that 33.2% of the general population aged 18–65 years in Mongolia had need for headache-related health care, according to our definition of “need”: 18.2% for migraine, 4.3% for TTH, 5.7% for pMOH and 5.0% for other H15+.
Discussion
This is the first paper to report headache-attributed burden in Mongolia. It adds to our earlier paper on prevalence [13], using data collected in the same study from the same participants.
In summary, recalling frequency, usual duration and usual intensity over the preceding 30 days, study participants with headache (66.1% of the sample) reported an average of 9.7% of all their time with headache rated mild-to-moderate. Headache yesterday, when reported, was on average rated moderate. Those with migraine reported higher symptom burden than those with TTH, but, at individual level, pMOH and other H15 + far outweighed migraine. Multiplying pTIS for migraine by the ictal state DW from GBD [18] gave a value of 3.0%. Despite the terminology used by GBD, this is an estimate of lost health rather than disability; in other words, the intermittent symptoms of migraine were equivalent to a continuous health diminution of 3.0%. Consequential impaired participation, estimated from recall over the preceding 3 months, was 1.3 days in paid work, 2.4 days in household work and 0.4 days in leisure activity, with a clear gradient between headache types (pMOH > other H15 + > migraine > TTH) in both genders. QoL estimates (despite the non-specificity for headache of WHOQoL-8) reflected symptom burden and impaired participation, with a clear downward gradient from no headache to TTH to migraine to other H15 + to pMOH. These measures show high individual burden from prevalent disease.
A main purpose of this study was to provide population-level estimates to inform health policy. An average pTIS of 9.7% among all headache sufferers diluted to a population-level pTIS of 6.2% when factoring in 1-year prevalence and correcting for age and gender. Over half of this was attributable to pMOH (2.1%) and other H15+ (1.0%), a quarter (1.7%) to migraine. The calculation based on HY for all headache yielded a similar, albeit slightly higher, estimate of 7.4%, indicating robustness of these estimates.
Of particular economic interest are the population-level estimates of impaired participation. On average, each adult person (with or without headache) lost 0.8 workdays and 1.4 household days to headache over a period of 3 months, migraine rather than pMOH being the principal contributor in both cases (more is said about this later). These losses – from work and household chores – can be interpreted as productivity losses, while those from paid work may translate into losses from gross domestic product (GDP). If 3 months are assumed to equate to 65 workdays, an estimated 1.2% of all workdays (0.8/65) are lost to headache. It is worth noting that the individual data on impaired participation were heavily skewed, indicating a severely affected minority for whom targeted intervention might be considered an economic priority.
From HY data we could estimate only total impaired participation across all three domains (paid work, household work and leisure), with limited ability to infer how much of the 6.7% impairment at population level pertained to income-generating work. However, given that most days in a week for most people are workdays, this finding of 6.7% overall impairment suggests that the 1.2% workday loss derived from HALT (dependent on 90-day recall) is an underestimate. Of course, the estimate from HY was based on a much lower N, but it remained acceptable (409) since the original sample was large.
Migraine was associated with the largest detriment in productivity at population level despite that pMOH was associated with higher population-level pTIS (2.1% vs. 1.7%) and higher individual-level burden (in other words, time with pMOH was rated worse than time with migraine). It appears that, during an attack, migraine nonetheless had greater impact on productivity. Associated symptoms (particularly nausea) might have been partly responsible, but a plausible explanation is that people with highly frequent headache develop coping mechanisms, while occasional unpredictable attacks are highly disruptive.
Pursuing the purpose of informing national health policy, our needs assessment found that one third (33.2%) of the adult Mongolian population were likely to benefit from – and were therefore in need of – headache-related health care. This high proportion was mainly driven by the high prevalences of H15+ (10.7%) and migraine on ≥ 3 days/month (15.0%). TTH contributed relatively little (4.3%). We have previously discussed our criteria for defining “need” in this context [22], some of which, arguably, are arbitrary. However, it is uncontroversial that all of those with H15 + should be offered care, and the same appears true for those with migraine on ≥ 3 days/month since this is often considered the threshold for initiating preventative medication. If all other criteria were dropped, an estimated one quarter (25.9%: calculation not shown) of the adult population in Mongolia would still be considered to need headache-related health care.
Strengths and limitations
As previously noted [13], the strengths of this survey included conduct in accordance with standardized methods [14, 15] in a large (N = 2,043) and nationally representative sample with a very high participating proportion (98.3%). Additionally, we estimated headache-attributed burden and impaired participation from data derived from both the preceding day and 1–3 months.
Limitations were those inherent in all cross-sectional retrospective studies. We had a preponderance of females in our sample, but estimates were corrected for gender and age. In addition, there was oversampling of people with high levels of education [13], a factor associated with higher prevalence of migraine but lower prevalence of pMOH [13].
Conclusions
This first population-based study on headache burden in Mongolia, with the aim of informing health policy, shows that 6.2–7.4% of all time in the adult population is spent with headache. With its very high prevalence and high individual burden, H15 + causes more burden at population-level than migraine and TTH combined. Migraine, however, has greatest negative impact on the nation’s productivity. An estimated one third of the adult population have a headache disorder (mostly H15 + or migraine) likely to benefit from health care. From a purely economic perspective, Mongolia, with limited health resources, would probably be best served by focusing on mitigating migraine-attributed burden.
Data availability
The data are held on file at Mongolian National University of Medical Sciences and at Norwegian University of Science and Technology. Once analysis and publications are completed, they will be freely available for non-commercial purposes to any person requesting access in accordance with the policy of the Global Campaign against Headache.
Abbreviations
- ANOVA:
-
Analysis Of Variance
- CI:
-
Confidence Interval
- DW:
-
Disability Weight
- GBD:
-
Global Burden of Disease
- GDP:
-
Gross Domestic Product
- HARDSHIP:
-
Headache-Attributed Restriction, Disability, Social Handicap and Impaired Participation Questionnaire
- ICHD:
-
International Classification of Headache Disorders
- HALT:
-
Headache-Attributed Lost Time
- HY:
-
Headache Yesterday
- MNUMS:
-
Mongolian National University of Medical Sciences
- MOH:
-
Medication-Overuse Headache
- pMOH:
-
probable MOH
- pTIS:
-
proportion of Time In Ictal State
- QoL:
-
Quality of Life
- SEM:
-
Standard Error of the Mean
- TTH:
-
Tension-Type Headache
- WHO:
-
World Health Organization
- WPR:
-
Western Pacific Region
References
Zebenigus M, Tekle-Haimanot R, Worku DK, Thomas H, Steiner TJ (2017) The burden of headache disorders in Ethiopia: national estimates from a population-based door-to-door survey. J Headache Pain 18:58. https://doi.org/10.1186/s10194-017-0765-7
Zebenigus M, Tekle-Haimanot R, Worku DK, Thomas H, Steiner TJ (2016) The prevalence of primary headache disorders in Ethiopia. J Headache Pain 17:110. https://doi.org/10.1186/s10194-016-0704-z
Mbewe E, Zairemthiama P, Paul R, Birbeck GL, Steiner TJ (2015) The burden of primary headache disorders in Zambia: national estimates from a population-based door-to-door survey. J Headache Pain 16:36. https://doi.org/10.1186/s10194-015-0513-9
Mbewe E, Zairemthiama P, Yeh HH, Paul R, Birbeck GL, Steiner TJ (2015) The epidemiology of primary headache disorders in Zambia: a population-based door-to-door survey. J Headache Pain 16:515. https://doi.org/10.1186/s10194-015-0515-7
Manandhar K, Risal A, Linde M, Steiner TJ (2015) The burden of headache disorders in Nepal: estimates from a population-based survey. J Headache Pain 17:3. https://doi.org/10.1186/s10194-016-0594-0
Manandhar K, Risal A, Steiner TJ, Holen A, Linde M (2015) The prevalence of primary headache disorders in Nepal: a nationwide population-based study. J Headache Pain 16:95. https://doi.org/10.1186/s10194-015-0580-y
Rao GN, Kulkarni GB, Gururaj G, Stovner LJ, Steiner TJ (2015) The burden attributable to headache disorders in India: estimates from a community-based study in Karnataka State. J Headache Pain 16:94. https://doi.org/10.1186/s10194-015-0574-9
Gururaj G, Kulkarni GB, Rao GN, Subbakrishna DK, Stovner LJ, Steiner TJ (2014) Prevalence and sociodemographic correlates of primary headache disorders: results of a population-based survey from Bangalore, India. Indian J Public Health 58:241–248. https://doi.org/10.4103/0019-557x.146280
Yu S, Liu R, Zhao G, Yang X, Qiao X, Feng J et al (2012) The prevalence and burden of primary headaches in China: a population-based door-to-door survey. Headache 52:582–591. https://doi.org/10.1111/j.1526-4610.2011.02061.x
Al Jumah M, Al Khathaami AM, Kojan S, Hussain M, Thomas H, Steiner TJ (2020) The prevalence of primary headache disorders in Saudi Arabia: a cross-sectional population-based study. J Headache Pain 21:11. https://doi.org/10.1186/s10194-020-1081-1
Herekar AA, Ahmad A, Uqaili UL, Ahmed B, Effendi J, Alvi SZ et al (2017) Primary headache disorders in the adult general population of Pakistan - a cross sectional nationwide prevalence survey. J Headache Pain 18:28. https://doi.org/10.1186/s10194-017-0734-1
Ayzenberg I, Katsarava Z, Sborowski A, Chernysh M, Osipova V, Tabeeva G et al (2012) The prevalence of primary headache disorders in Russia: a countrywide survey. Cephalalgia 32:373–381. https://doi.org/10.1177/0333102412438977
Luvsannorov O, Tsenddorj B, Baldorj D, Enkhtuya S, Purev D, Thomas H et al (2019) Primary headache disorders among the adult population of Mongolia: prevalences and associations from a population-based survey. J Headache Pain 20:114. https://doi.org/10.1186/s10194-019-1061-5
Stovner LJ, Al Jumah M, Birbeck GL, Gururaj G, Jensen R, Katsarava Z et al (2014) The methodology of population surveys of headache prevalence, burden and cost: principles and recommendations from the global campaign against Headache. J Headache Pain 15:5. https://doi.org/10.1186/1129-2377-15-5
Steiner TJ, Gururaj G, Andrée C, Katsarava Z, Ayzenberg I, Yu SY et al (2014) Diagnosis, prevalence estimation and burden measurement in population surveys of headache: presenting the HARDSHIP questionnaire. J Headache Pain 15:3. https://doi.org/10.1186/1129-2377-15-3
Peters MBJ, Houchin C, Kandoura T, Steiner TJ (2007) Translation protocol for lay documents. J Headache Pain 8:S43–S44
Headache Classification Committee of the International Headache Society (IHS) (2018) The International Classification of Headache Disorders, 3rd edition. Cephalalgia 38: 1-211. https://doi.org/10.1177/0333102417738202
Salomon JA, Haagsma JA, Davis A, de Noordhout CM, Polinder S, Havelaar AH et al (2015) Disability weights for the global burden of Disease 2013 study. Lancet Glob Health 3:e712–e723. https://doi.org/10.1016/s2214-109x(15)00069-8
Steiner TJ, Lipton RB (2018) The headache-attributed Lost Time (HALT) indices: measures of burden for clinical management and population-based research. J Headache Pain 9:12. https://doi.org/10.1186/s10194-018-0837-3
Group TWQ (1998) Development of the World Health Organization WHOQOL-BREF quality of life assessment. WHOQOL Group Psychol Med 28:551–558. https://doi.org/10.1017/s0033291798006667
National Statistics Office of Mongolia Population of Mongolia, by sex and urban/rural. https://www.1212.mn/en/statistic/statcate/573051/table-view/DT_NSO_0300_027V1 (accessed 17 July 2024).
Al Jumah M, Al Khathaami AM, Kojan S, Husøy A, Steiner TJ (2024) The burden of headache disorders in the adult general population of the Kingdom of Saudi Arabia: estimates from a cross-sectional population-based study including a health-care needs assessment. J Headache Pain 25:66. https://doi.org/10.1186/s10194-024-01767-6
Acknowledgements
This study was a project within the Global Campaign against Headache.
Funding
The study was supported by a grant from Lifting The Burden, a United Kingdom-based non-governmental organization conducting the Global Campaign against Headache in official relations with the World Health Organization.
Open access funding provided by NTNU Norwegian University of Science and Technology (incl St. Olavs Hospital - Trondheim University Hospital)
Author information
Authors and Affiliations
Contributions
OL and TJS conceived the study and developed the protocol. OL was principal investigator. BT, DB, SE and DP contributed to data collection. AH performed the data analysis with input from TJS. AH and TJS drafted the manuscript. All authors reviewed it critically for intellectual content, and approved the version submitted.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Ethics Committee of Research of the Mongolian National University of Medical Sciences (MNUMS) approved the study protocol. Informed written (signed) consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
TJS is a Director and Trustee of Lifting The Burden and is associate editor of The Journal of Headache and Pain. AH is a member of the Junior Editorial Board of The Journal of Headache and Pain. Otherwise, no author declares a conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Luvsannorov, O., Tsenddorj, B., Baldorj, D. et al. The burden of headache disorders in the adult population of Mongolia: estimates, and a health-care needs assessment, from a cross-sectional population-based study. J Headache Pain 25, 146 (2024). https://doi.org/10.1186/s10194-024-01856-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10194-024-01856-6