Abstract
Background
Cervical cancer is the third most common gynecological malignancy. Conventional treatment options are known to be ineffective for the majority of patients with advanced or recurrent cervical cancer. Therefore, novel therapeutic agents for cervical cancer are necessary. In this study, the effects of CKD-602 in cervical cancer were investigated.
Methods
Three established human, immortalized, cervical cancer cell lines (CaSki, HeLa and SiHa) were used in this study. Following treatment with CKD-602, apoptosis was quantified using fluorescein isothiocyanate Annexin V-FITC and propidium iodide (PI) detection kit and cell cycle analysis was analyzed using fluorescence activated cell sorting (FACS). Transwell chambers were used for invasion assays. Western blot assay was performed to analyze proteomics. CaSki cells were subcutaneously injected into BALB/c-nude mice and cervical cancer xenograft model was established to elucidate the antitumor effect of CKD-602 in vivo.
Results
Treatment with CKD-602 induced apoptosis and increased expression of the enzyme PARP, cleaved PARP, and BAX. In addition, expression of phosphorylated p53 increased. Cell cycle arrest at G2/M phase and inhibition of invasion were detected after treatment with CKD-602. A significant decrease in cervical cancer tumor volume was observed in this in vivo model, following treatment with CKD-602.
Conclusions
This is the first report of CKD-602 having an antitumor effect in cervical cancer in both an in vitro and in vivo models. The results of this study indicate that CKD-602 may be a novel potential drug, targeting cervical cancer, providing new opportunities in the development of new therapeutic strategies.
Similar content being viewed by others
Background
Cervical cancer is the third most common gynecological malignancy and is responsible for 10–15% of cancer-related death in women (Jemal et al., 2011). Conventional treatment options (e.g., chemotherapy, radiation and surgical resection) are known to be ineffective for the majority of patients with advanced or recurrent cervical cancer, highlighting the need to identify novel treatment agents (Smith et al., 1993). Only modest response rates with excessive toxicity were reported without an improvement in survival rate (Chambers et al., 1994). Therefore, novel therapeutic agents for cervical cancer are necessary.
Type I and type II topoisomerase inhibitors interfere with DNA ‘unwinding’ during DNA replication and RNA transcription. Topoisomerase I (TOP1) cuts one strand in the double-stranded DNA, independent of ATP. In contrast, topoisomerase II (TOP2) cuts both strands in DNA and is dependent on ATP for its activity (Xu and Her, 2015). Camptothecin (CPT) is the TOP1 inhibitor which was originally isolated from the Chinese tree Camptotheca acuminate, however it is no longer in use due to detrimental side effects It was replaced by more effective and safer TOP1 inhibitors such as topotecan and irinotecan (Wall and Wani, 1995).
The synthetic water-solube camptothecin analogue, CKD-602, 7-[2-(N-isopropylamino) ethyl]-(20S)-camptothecin (belotecan, Chong Kun Dang Pharmaceutical Corporation, Seoul, Korea), has been shown to be effective in the treatment of various cancers (e.g. glioblastoma, colon and ovarian cancer). The antitumor activity of CKD-602 in cervical cancer has not yet been fully investigated (Lee et al., 1998). In this study, the effects of CKD-602 in cervical cancer cell lines both in vitro and in vivo were investigated.
Materials and methods
Cell lines and reagents
Three established human, immortalized, cervical cancer cell lines (CaSki, HeLa and SiHa) were used in this study. All three cell lines were integrated with high-risk Human papillomavirus (HPV); CaSki and Siha cell lines were integrated with HPV-16 and the HeLa cell line was integrated with HPV-18. All cell lines were maintained in Roswell Park Memorial Institute (RPMI) 1640, Eagle’s Minimum Essential Medium (MEM) and Dulbecco’s modified Eagle’s medium (DMEM) (Gibco/ThermoFisher Scientific, Waltham, MA, USA) supplemented with 10% fetal bovine serum (FBS, Gibco) and 1% penicillin and streptomycin (Gibco) at 37 °C in a 5% CO2 incubator. The CKD-602 was dissolved in distilled water with 50 mg D-mannitol (Sigma–Aldrich, St Louis, MO, USA), 0.06 mg at 5 mg/1 ml tartaric acid (Sigma-Aldrich), and stored as stock in aliquots at 4 °C. For in vitro use, final concentrations between 15 and 150 ng/ml CKD-602 were obtained by appropriate dilutions of the stock solution in each cell medium. For in vivo use, final concentrations of 25 mg/kg CKD-602 were obtained by appropriate dilutions of the stock solution with RPMI 1640 medium (Gibco). The CKD-602 was donated from Chong Kun Dang Pharmaceutical Corporation (Seoul, Korea).
Apoptosis assay
Apoptosis was quantified using the fluorescein isothiocyanate annexin V-FITC and propidium iodide (PI) Apoptosis Detection Kit I (BD Pharmingen, La Jolla, CA, USA) according to the manufacturer’s instructions. Briefly, CKD-602-treated and non-treated 1 × 106 cells were washed in ice-cold phosphate buffered saline (PBS), resuspended in 100 μL of binding buffer, and incubated with 5 μL of annexin V-FITC and 5 μL of PI for 15 min in a dark room, at room temperature, as per manufacturer’s guidelines. Flow cytometric analysis was immediately performed using a FACS Calibur flow cytometer (FACS Calibur; Becton Dickinson, Franklin Lakes, NJ, USA).
Cell-cycle analysis
The cells at a density of 2 × 105 cells/well in MEM/DMEM with 10% FBS were added to the wells of a 6-well plate and incubated overnight. Each cell was treated with 1/2 IC50 and IC50 CKD-602 for 48 h. Following treatment, cells were harvested by centrifugation at 1300 rpm for 3 min, washed twice in ice-cold PBS and fixed by incubating the cells overnight at − 20 °C with 70% ethanol. Cells were then washed with ice-cold PBS and resuspended in 500 μl PI/RNase staining solution (Invitrogen/ThermoFisher Scientific, Waltham, MA, USA). The cell cycle position was evaluated by FACS using an excitation laser set at 480 nm and a detection wavelength of 575 nm. A minimum of 10,000~30,000 events/sample was analyzed.
Cell invasion assay
A cell invasion assay was performed to elucidate whether CKD-602 is capable of inhibiting cervical cancer cell invasion (in CaSki, Hela and Siha cell lines). Transwell chambers were used (Corning INc., Corning, NY, USA) and 100 ul cells (1-2 × 105 per well) added to the upper chamber of 24-well plates, which was pre-coated with 30 μl of Matrigel (R&D Systems. catalog no. 1918-FN) for 2 h under a cell incubator. Concurrently, CKD-602 was diluted with 0.65 ml 20% FBS-DMEM complete medium(final concentration for CaSki, HeLa and Siha were: 120 ng/ml; 300 ng/ml and 300 ng/ml, respectively)was added to the lower chamber. After 48 h, the invaded cells in the lower chamber were fixed, stained with 0.1% crystal violet solution and then photographed under inverted microscope (× 200).
Western blot analysis
Briefly, CKD-602-treated and non-treated cells were washed twice in PBS and cell lysates prepared using the radioimmunoprecipitation assay (RIPA). For immnunoblotting, 30 μg protein was resolved on 4–12% SDS-PAGE, transferred onto PVDF membrane (Bio-Rad, Hercules, CA, USA) by electroblotting, and blocked in 5% BSA in TBST. Membranes were then probed overnight at 4 °C with the following antibodies: Cyclin B1 (4138); cdc2 (9116); phopho-cdc2 (Tyr15; 9111); p21 (Waf1/Cip1;2947); p53 (2527); phopho-p53 (Ser15;9286), and PARP (9542) (1:1000; Cell Signaling Technology, Inc. (Danvers, MA, USA). Antibodies to c-PARP (ab32064; 1:1000), phopho-Cyclin B1 (S126; ab133439; 1:10,000), BCL2-associated X protein (Bax, ab32503; 1:2000), matrix mettloproteinases 2 (MMP2, ab97779; 1:5000), and vascular endothelial growth factor (VEGF, ab52917; 1:5000) and Cyclin A1 (sc56301; 1:1000) were acquired from Abcam (Cambridge, UK). The antibodies for CDK2 (sc6248; 1:5000) and the housekeeping gene, glyceraldehyde 3-phosphate dehydrogenase (GAPDH, sc32232, 1:5000) were acquired from Santa Cruz Biotechnology (Dallas, TX, USA).
The cell membrane was washed with phosphate buffered saline with Tween 20 (PBST) and incubated with corresponding secondary antibodies for 1 h at room temperature. Membranes were washed again with PBST and blots were developed into X-Ray films using the enhanced chemiluminescence (ECL) method previously described, or the Chemidoc MP system, Bio-Rad.
Xenograft model
All animal experimental protocols were reviewed and approved by the Catholic University Animal Care and Use Committee and performed in accordance with the National Institute of Health Guide for the Care and Use of Experimental Animals. Normal six-week-old female BALB/c-nude mice (17–22 g) were purchased from Orient Bio (Gyeonggi-do, Korea). Specifically, CaSki cells (4 × 106/head) were subcutaneously injected into the right leg of the mouse. After two weeks, when the tumor had attained an average volume of approximately 80mm3, tumor sizes were measured using a vernier caliper weekly and tumor volume calculated [(tumor length) × (tumor width) 2/2]. The dose of CKD-602 (25 mg/kg) was chosen based upon previous reports (Kim et al., 2013). The CKD-602 was injected intravenously for 16 days at 4-day intervals and PBS as a negative control was injected in same way. After CKD-602 treatment, tumor volumes and body weights were measured every 3–4 days from day 17. Mice were killed 4 weeks after establishment of the xenograft.
Statistical analysis
All statistical analyses were performed using one-way ANOVA comparing variable groups (Graphpad Prism5 software). All experiments were repeated at least three times. In certain cases, the Student’s t-test was also performed. Values are expressed as mean ± standard error of the mean (SEM) for control and treated samples. A p value of < 0.05 was considered statistically significant (*p < 0.05, **p < 0.01, ***p < 0.001, ns = not significant).
Results
CKD-602 promotes pro-apoptotic activity in cervical cancer
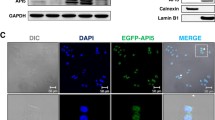
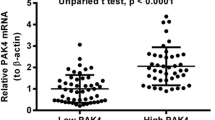
Using the cell viability assay, treatment with CKD-602 showed a significant cytotoxic effect in all cervical cancer cell lines in a time- (p < 0.05) and dose- (p < 0.05) dependent manner (Additional file 1: Figure S1). The IC50 (50% inhibition concentration of cell viability) values were 30 ng/ml (95% CI: 18.29–63.30) for Caski cells, 150 ng/ml (95% CI: 100.3–179.4) for HeLa cells, and 150 ng/ml (95% CI: 64.63–254.3) for SiHa cells at 48 h after treatment. To investigate the efficacy of CKD-602 in cervical cancer, pro-apoptotic activity was measured. A strong pro-apoptotic activity was observed in the treatment groups after 48 h of treatment (Fig. 1a and b). Compared to the control, apoptosis rates significantly increased in Caski, HeLa and Siha when treated with different concentrations (half the IC50 and IC50 values). The treatment increased the expression of PARP, cleaved PARP and Bcl2-associated X protein (BAX). In addition, expression of both p53 and phosphorylated p53 (Ser15) was increased (Fig. 1c).
Pro-apoptotic activity in cervical cancer cells (CaSki, HeLa and SiHa) following CKD-602 treatment. Cells were incubated with CKD602 in a dose-dependent manner (0 [control], ½ IC50, IC50 ng/ml each cells) for 48 h. a. The percentage of apoptosic cells was evaluated using flow cytometic analysis with Annexin V and PI staining. b. The percentage of apoptosic cells measured by flow cytometry. Results are expressed as the mean ± SEM (*p < 0.05 and **p < 0.01). c. Western blot analysis of apoptosis-related proteins in cervical cancer cells
CKD-602 induces cell-cycle arrest in the G2/M phase in cervical cancer
Cell cycle analysis was performed following CKD-602 treatment with different concentrations (half the IC50 and IC50 values) after 48 h of treatment (Fig. 2). Treatment induced the G2/M phase cell accumulation in all cell lines in a concentration-dependent manner. The proportion of the cell population in G2/M phase at 48 h increased from 26.3 to 64.5% (CaSki cells), 23.4 to 70.9% (HeLa cells) and 16.0 to 61.0% (SiHa cells). This increase was statistically significant (*p < 0.05 and ** p < 0.01). We investigated the G2/M – related protein levels. The increases in cyclin B1 and phosphorylated cyclin B1 (phosphor Ser126) expression levels were present in all the cell lines. Expression of Cdc2 protein did not show substantial change but phospho-cdc2 (Tyr15) protein expression increased after CKD-602 treatment.
Induction of G2/M arrest in cervical cancer cells following treatment with CKD-602. a. Cells were incubated with CKD602 in a dose-dependent manner (0, ½ IC50, IC50 ng/ml each cells) for 48 h. Cells were then harvested and fixed with ethanol followed by PI staining to determine cellular distribution in different phases of the cell cycle using flow cytometry. b. Percentage of cell cycle progression measured by flow cytometry. Results are expressed as the mean ± SEM (*p < 0.05 and **p < 0.01). c. Western blot analysis of cell cycle-related proteins in cervical cancer cells
CKD-602 inhibits cancer invasion in cervical cancer
An in vitro invasion assay was performed to investigate whether CKD-602 treatment affected the invasive ability of cervical cancer cells. The assay was performed in chambers that had the upper wells coated with Matrigel to mimic the extracellular matrix in vivo. All the cervical cancer cell lines were treated with IC50 concentrations and representative photomicrographs of the membrane-associated cells (× 200) taken and analyzed (Fig. 3a). Significant differences of invasive ability were detected between the control cells and the CKD-602 treated cells (Fig. 3b) (*p < 0.05 and **p < 0.01). The protein expression levels of MMP2 and VEGF, two proteins known to be specifically related to the invasive ability of cells, decreased following CKD-602 treatment (Fig. 3c).
Invasive ability of CKD-602 in cervical cancer cells. a. Photomicrographs showing invasive potential of CKD602 in cervical cancer cells using matrigel precoated transwell assay (× 200) and b. Mean ± SEM (*p < 0.05 and ** p < 0.01). c. Western blot analysis of cell invasion-related proteins in cervical cancer cells
Inhibition of tumor growth in CaSki-xenografted nude mice
Based on the in vitro data, it was then investigated whether CKD-602 would also be effective in an in vivo model. Groups of BALB/c-nude mice (five per group) were subcutaneously injected with CaSki cells and then treated (intravenously) with CKD-602 (25 m/kg) or PBS two weeks after the transplantation, when the tumors were approximately 80 mm3 (Fig. 4a). Seventeen days after the last injections, the mice were killed and the tumor volume measured and body weights of the mice recorded (Fig. 4b). Treatment with CKD-602 significantly inhibited the tumor growth of in this xenograft model compared with the control (p < 0.05). There was no significant difference in bodyweight between the xenograft mice and the controls, indicating that treatment with CKD-602 was well tolerated (Fig. 4b).
Antitumor efficacy of CKD-602 in a CaSKi xenograft model. a. Schematic diagram of the treatment regimen of CKD-602. Groups of BALB/c-nude mice (five per group) were subcutaneously challenged with CaSki 4 × 106 CaSki tumor cells per mouse. b. Tumor volume in CaSki tumor-bearing mice in control mice and the CKD-602-treated mice. Results are expressed as mean ± SEM (*p < 0.05). c. Body weight of CaSki tumor-bearing mice in control mice and CKD-602-treated mice
Discussion
Topoisomerase I (TOP1) inhibitors (e.g. toptecan and iritonecan) are currently used in the treatment of cervical cancer treatment (https://www.nccn.org). Previous studies have demonstrated that CKD-602, a TOP1 inhibitor, is effective in the treatment of various cancers such as small cell lung carcinoma, oral squamous cell carcinoma and glioblastoma (Kim et al., 2013; Kim et al., 2015; Lee et al., 1998). In the current study, treatment with CKD-602 as a potential anticancer drug targeting cervical cancer was investigated for the first time. In both in vitro and in vivo models, treatment with CKD-602 promoted apoptosis, induced cell cycle arrest in G2/M phase and inhibited cancer invasion.
Based upon previous reports indicating that CKD-602 has anticancer effects (Kim et al., 2013; Lee et al., 1998) a possible pro-apoptotic effect in cervical cancer was investigated. Using three distinct human cervical cancer cell lines (CaSki [HPV − 16], HeLa [HPV-18], and SiHa [HPV-16]), it was demonstrated that activation of BAX and PARP cleavage were enhanced 48 h after treatment (Fig. 1). In addition, phosphorylation of p53 occurred after treatment. Previous studies have reported that phosphorylation of p53 modulates the functions of p53 and is causally related to apoptosis (Milne et al., 1995; Zhang et al., 1994). Furthermore, it has been demonstrated that p53 can activate the expression of BAX, a member of the Bcl-2 family, and that BAX can act to accelerate apoptosis (Basu and Haldar, 1998; Haupt et al., 2003; Miyashita et al., 1994). Pro-apoptotic signaling induced by TOP1 inhibitors has been reported in previous studies, suggesting that TOP1 possesses a protein-kinase activity that is specific to serine residues (García et al., 2014; Gobert et al., 1999; Tazi et al., 1997). Together, the data from the current study indicates that treatment with CKD-602 may induce apoptosis through phosphorylation of p53 in cervical cancer.
The effect of CKD-602 treatment in cell-cycle arrest in cervical cancer was investigated. It was found that treatment with CKD-602 is capable of inducing G2/M phase cell-cycle arrest in cervical cancer. Cell-cycle arrest at the G2/M phase is associated with enhanced apoptosis and is a cellular response to various DNA-damaging agents (DiPaola, 2002). A previous study has demonstrated CKD-602-induced cell-cycle arrest at the G2/M phase in oral squamous cell carcinoma cancer and the data from the current study indicates that the same may be true in cervical cancer (Kim et al., 2015). As shown in Fig. 2, expression of cyclin B1, phosphorylated cyclin B1 and p21 increased in cervical cancer following CKD-602 treatment. It is well known that p53 regulates the G2/M checkpoint through cyclin B1 (Innocente et al., 1999) however it has also been reported that some TOP1 inhibitors can induce p53-independent G2/M arrest (Bozko et al., 2002; Wu et al., 2015). Further studies are required to determine if G2/M arrest after CKD-602 treatment is p53-dependent or independent.
Several TOP1inhibitors have been reported to be involved in the inhibition of cancer invasion (Elstner et al., 2007; Min et al., 2011). The results of the current study are the first to show that inhibition of cancer invasion by CKD-602, a TOP1 inhibitor. It was found that expression of MMP2 and VEGF decreased 48 h after CKD-602 treatment in 3 cervical cancer cell lines (CaSki, HeLa and SiHa). Matrix metalloproteinases (MMPs), a family of enzymes, proteolytically degrade various components of the extracellular matrix (ECM). Increased expression of MMPs is associated with the increase of tumor cells in an organ (Zhang et al., 2015).Vascular epithelial growth factor (VEGF) is a mitogen that induces a rapid and complete angiogenic response to cancersous/tumor cells in an organ (Carmeliet, 2005). In addition, a previous study has shown that cell invasion is promoted via VEGF and MMP2 in cervical cancer (Chen et al., 2014).
Conclusions
This is the first study to identify and report the anticancer effects of CKD-602 treatment in cervical cancer, in both in vitro and in vivo models. The data suggests that p53-mediated apoptosis, cell cycle arrest at G2/ M phase and inhibition of invasion through MMP2 and VEGF were involved in these processes. CKD-602 may be a potential drug targeting cervical cancer that will lead to new opportunities to develop new therapeutic strategies.
Abbreviations
- BAX:
-
Bcl2-associated X protein
- CPT:
-
camptothecin
- FACS:
-
fluorescence activated cell sorting
- MEM:
-
Minimum Essential Medium
- PI:
-
propidium iodide
- RPMI:
-
Roswell Park Memorial Institute
- TOP1:
-
topoisomerase I
- TOP2:
-
topoisomerase II
References
Basu A, Haldar S. The relationship between BcI2, Bax and p53: consequences for cell cycle progression and cell death. Mol Hum Reprod. 1998;4:1099–109.
Bozko P, Larsen AK, Raymond E, Skladanowski A. Influence of G2 arrest on the cytotoxicity of DNA topoisomerase inhibitors toward human carcinoma cells with different p53 status. Acta Biochim Pol. 2002;49:109–19.
Carmeliet P. VEGF as a key mediator of angiogenesis in cancer. Oncology. 2005;69(Suppl 3):4–10.
Chambers SK, Lamb L, Kohorn EI, Schwartz PE, Chambers JT. Chemotherapy of recurrent/advanced cervical cancer: results of the Yale University PBM-PFU protocol. Gynecol Oncol. 1994;53:161–9.
Chen B, Zhang C, Dong P, Guo Y, Mu N. Molecular regulation of cervical cancer growth and invasion by VEGFa. Tumour Biol. 2014;35:11587–93.
DiPaola RS. To arrest or not to G(2)-M cell-cycle arrest : commentary re: A. K. Tyagi et al., Silibinin strongly synergizes human prostate carcinoma DU145 cells to doxorubicin-induced growth inhibition, G(2)-M arrest, and apoptosis. Clin cancer res. 8: 3512-3519, 2002. Clin Cancer Res. 2002;8:3311–4.
Elstner A, Holtkamp N, von Deimling A. Involvement of Hif-1 in desferrioxamine-induced invasion of glioblastoma cells. Clin Exp Metastasis. 2007;24:57–66.
García CP, Videla Richardson GA, Romorini L, Miriuka SG, Sevlever GE, Scassa ME. Topoisomerase I inhibitor, camptothecin, induces apoptogenic signaling in human embryonic stem cells. Stem Cell Res. 2014;12:400–14.
Gobert C, Skladanowski A, Larsen AK. The interaction between p53 and DNA topoisomerase I is regulated differently in cells with wild-type and mutant p53. Natl Acad Sci U. S. A. 1999;96:10355–60.
Haupt S, Berger M, Goldberg Z, Haupt Y. Apoptosis - the p53 network. J Cell Sci. 2003;116:4077–85.
Innocente SA, Abrahamson JL, Cogswell JP, Lee JM. p53 regulates a G2 checkpoint through cyclin B1. Natl Acad Sci U S A. 1999;96:2147–52.
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90.
Kim YH, Lee JK, Kim B, DeWitt JP, Lee JE, Han JH, Kim SK, Oh CW, Kim CY. Combination therapy of cilengitide with belotecan against experimental glioblastoma. Int J Cancer. 2013;133:749–56.
Kim YK, Koo NY, Yun PY. Anticancer effects of CKD-602 (Camtobell®) via G2/M phase arrest in oral squamous cell carcinoma cell line. Oncol Lett. 2015;9:136–42.
Lee JH, Lee JM, Kim JK, Ahn SK, Lee SJ, Kim MY, Jew SS, Park JG, Hong CI. Antitumor activity of 7-[2-(N-isopropylamino)ethyl]-(20S)-camptothecin, CKD602, as a potent DNA topoisomerase I inhibitor. Arch Pharm Res. 1998;21:581–90.
Milne DM, Campbell LE, Campbell DG, Meek DW. p53 is phosphorylated in vitro and in vivo by an ultraviolet radiation-induced protein kinase characteristic of the c-Jun kinase, JNK1. J Biol Chem. 1995;70:5511–8.
Min R, Zun Z, Min Y, Wenhu D, Wenjun Y, Chenping Z. Shikonin inhibits tumor invasion via down-regulation of NF-κB-mediated MMP-9 expression in human ACC-M cells. Oral Dis. 2011;17:362–9.
Miyashita T, Harigai M, Hanada M, Reed JC. Identification of a p53-dependent negative response element in the bcl-2 gene. Cancer Res. 1994;54:3131–5.
Smith HO, Stringer CA, Kavanagh JJ, Gershenson DM, Edwards CL, Wharton JT. Treatment of advanced or recurrent squamous cell carcinoma of the uterine cervix with mitomycin-C, bleomycin, and cisplatin chemotherapy. Gynecol Oncol. 1993;48:11–5.
Tazi J, Rossi F, Labourier E, Gallouzi I, Brunel C, Antoine E. DNA topoisomerase I: customs officer at the border between DNA and RNA worlds? Journal of molecular medicine (Ber). 1997;75:786–800.
Wall ME, Wani MC. Camptothecin and taxol: discovery to clinic--thirteenth Bruce F. Cain memorial award lecture. Cancer Res. 1995:55; 753–60.
Wu CC, Huang KF, Yang TY, Li YL, Wen CL, Hsu SL, Chen TH. The topoisomerase 1 inhibitor Austrobailignan-1 isolated from Koelreuteria henryi induces a G2/M-phase arrest and cell death independently of p53 in non-small cell lung Cancer cells. PLoS One. 2015;10:e0132052.
Xu Y, Her C. Inhibition of topoisomerase (DNA) I (TOP1): DNA damage repair and anticancer therapy. Biomolecules. 2015;5:1652–70.
Zhang L, Zhou Y, Cheng C, Cui H, Cheng L, Kong P, et al. Genomic analyses reveal mutational signatures and frequently altered genes in esophageal squamous cell carcinoma. Am J Hum Genet. 2015;96:597–611.
Zhang W, McClain C, Gau JP, Guo XY, Deisseroth AB. Hyperphosphorylation of p53 induced by okadaic acid attenuates its transcriptional activation function. Cancer Res. 1994;54:4448–53.
Acknowledgements
We acknowledge the support of Chong Kun Dang Corporation for the donation of CKD-602 supplements for the study.
Funding
This work was supported by Chong Kun Dang Corporation and Bio & Medical Technology Development Program of the National Research Foundation (NRF) funded by the Ministry of Science & ICT (2018M3A9E8021512).
Availability of data and materials
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
Author information
Authors and Affiliations
Contributions
Sungha Lee and Youn Jin Choi wrote the manuscript. Youn Jin Choi and Soo Young Hur designed the study. Jung Yoon Ho, Jing Jing Liu and Hyewon Lee did animal experiments and analyzed the data. Jae Young Park, Minwha Baik, Minji Ko, Seon Ui Lee and Jung Yoon Ho performed the in vitro analysis and interpreted the data. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
All animal experimental protocols were reviewed and approved by the Catholic University Animal Care and Use Committee and performed in accordance with the National Institute of Health Guide for the Care and Use of Experimental Animals.
Consent for publication
There is no contains about any individual person’s data in any form and there is no need to get consent for publication.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Figure S1. Cell viability following CKD-602 treatment. (TIF 130 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Lee, S., Ho, J.Y., Liu, J.J. et al. CKD-602, a topoisomerase I inhibitor, induces apoptosis and cell-cycle arrest and inhibits invasion in cervical cancer. Mol Med 25, 23 (2019). https://doi.org/10.1186/s10020-019-0089-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s10020-019-0089-y