Abstract
Introduction
A primary intraparenchymal meningioma located in the subcortical region of the brain without a dural attachment is extremely rare. To the best of our knowledge, this is the first report showing that meningioma can mimic cavernous malformations.
Case presentation
We present the case of a 42-year-old German man who presented to our institution with seizure. Both computed tomography and magnetic resonance imaging scans showed characters of an intra-axial subcortical lesion with a ‘popcorn’ appearance and hemosiderin deposits in the right parietal lobe. The initial diagnosis was cavernous malformation. Intraoperatively, the lesion presented as a subcortical mass that had no connection to the dura or the ventricle. The histological diagnosis showed a WHO Grade 1 ‘raddled’ psammomatous meningioma with extensive metaplastic ossification. A literature review of 29 cases of intraparenchymal meningiomas regarding their clinical presentations, location and management was performed.
Conclusions
Meningiomas can be found in any region of the brain with and without dural attachment. Intraparenchymal meningiomas can have multiple entities mimicking their presentation. Caution must be used regarding the preoperative differential diagnosis.
Similar content being viewed by others
Introduction
Meningiomas account for approximately 15% of all intracranial neoplasms [1]. Meningiomas are usually attached to the dura and thought to arise from the arachnoid cap or meningothelial cells. Occasionally meningiomas develop without dural attachment, mainly in the intraventricular region, within the sylvian fissure, pineal region, or infratentorial compartment, and in pediatric and young patients [2–6]. The majority of meningiomas exhibit highly stereotypic imaging characteristics, which often facilitate their diagnosis without the need of invasive diagnostic procedures. In cases of absence of dural attachment, it is often difficult in the preoperative diagnosis to distinguish meningioma from high-grade glioma, cavernous angioma, or metastatic brain tumors and sarcomatous lesions [7–10]. Primary intraparenchymal meningiomas are rare and they are challenging to diagnose, especially when presenting with a typical magnetic resonance imaging (MRI) scan appearance.
We present a rare case of primary intraparenchymal meningioma that, preoperatively, was not typical for meningioma and showed characteristics of cavernous malformation. We reviewed all cases of intraparenchymal meningiomas in the literature to gather information regarding their sites, clinical presentations, pathological features, management, and outcome.
Case presentation
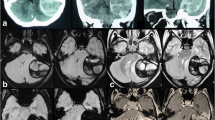
A right-handed 42-year-old German man presented to our institution with convulsive seizures. There were no other neurological symptoms or signs and no neurological deficits. The initial computed tomography (CT) scan of his brain revealed a hyperdense lesion with calcification in the right parietal area. His cranial MRI scan (Figures 1, 2 and 3) demonstrated a popcorn-shaped mass in the subcortical white matter of his right parietal lobe. The lesion had smooth lobulated margins and no dural attachment was apparent. The lesion was hypointense on T1-weighted images and mixed hypo- and hyperintense on T2-weighted images. There were local mass effect, peritumoral edema and heterogeneously contrast enhancement. On his T2* gradient echo images the lesion showed focal spots of (dark signal) hypointense areas centrally compatible with calcifications, demonstrated on his CT scans, and a surrounding hypointense rim interpreted as hemosiderin deposition typical of cerebral cavernoma.
A right parietal craniotomy was performed under MRI-guided navigational assistance. Grossly, no mass or any other pathologic tissue was observed below the dura or on the cortex. Using a sulcal approach, the mass reached about 2cm into the cortex, showing a good cleavage. The mass was completely calcified (like a stone) and measured about 1.5×1.5cm in diameter. A gross total resection could be achieved. Postoperatively, he had no neurological deficits.A histological examination of the specimen showed (at low magnification (5× objectives)) a tightly packed and parallel laminated mass of fibrous tissue (Figure 4). There were a few irregularly shaped small foci within the lesion, which were partly filled with flimsy tissue. At higher magnification (10× and 20× objective), many faded whorl structures and psammoma bodies were identified (Figure 5).Furthermore, the lesion contained areas of transition into mature lamellar bone and was partly bordered by brain tissue with piloid gliosis. There was no periodic acid-Schiff-positive inclusions, nor hemosiderin deposits. An immunohistochemistry analysis revealed focal positivity for epithelial membrane antigen and Vimentin (Figure 6). Staining the sample with reticulin did not reveal a hemangiopericytomas-like pattern. No other histological sign of atypia or malignancy was observed. The pathological examination was performed by two independent and board-certified pathologists. The final diagnosis was a ‘raddled’ psammomatous meningioma with extensive metaplastic ossification. The postoperative course was uneventful. He was discharged and returned to everyday life, showing no deficits.
In the literature review, we identified 36 cases of intraparenchymal meningiomas, including our case report. Case reports with insufficient information and meningiomas secondary to underlying meningioangiomatosis were excluded; 29 cases were included in total. There were 18 male (62.1%) and 11 female (37.9%) subjects, with the age ranging between 0.4 and 60 years (mean: 21.2 years). Of the 29 intraparenchymal meningioma cases, 26 were located in the supratentorial region (89.7%) and three were located in the infratentorial region of the brain (10.3%). The frontal location was dominant, being reported in 12 cases (41.4%). The most frequently reported clinical presentation was seizure, being reported in 20 cases (69.0%). In almost all of the cases, the radiological appearance was a solid mass showing contrast enhancement.
Preoperatively, three cases mimicked a glioma, one case mimicked metastasis und one case mimicked a cavernoma. Total surgical resection was the standard treatment approach and was achieved in all the cases, except in three cases involving the brainstem, in which only a subtotal resection was performed. Radiotherapy following the surgery was done in four cases und one subject additionally underwent adjuvant chemotherapy. Regarding the histopathology, the fibrous type proved to be dominant, being reported in 11 cases (37.9%). The majority of the patients had no postoperative deficits. The location, clinical presentation, radiological finding, and outcomes are summarized in Table 1.
Discussion
Intraparenchymal meningiomas are meningiomas that arise within the brain tissue without dural attachment and have also been used to characterize meningiomas that are not dural based [10]. The etiology of intraparenchymal meningiomas is unclear. Some authors presume that intraparenchymal meningiomas arise from arachnoid cells of the pia mater, which enter the surface of brain or sulcus with perforating blood vessels. Others suggest that the arachnoid cell rests during the migration progress [10]. The pineal region, the intraventricular region, and within the sylvian fissure are typical locations where a meningioma may develop without dural attachment [5, 38–40]. Meningiomas show characteristic imaging features such as: broad-based dural attachment, signal changes in the skull due to tumor infiltration, sharp demarcation between the tumor and the brain, mass effect on adjacent brain tissue, and homogeneous enhancement of a contrast agent [41, 42]. The site of origin provides a clear diagnosis in most cases. However, meningiomas can be mimicked by other intracranial tumors and pseudo-tumors such as glioma, ependymoma, metastasis, and cavernous malformation [7, 43].
Our case report shows several factors which pointed to the diagnosis of cavernous malformation: the subcortical location, clinical presentation, radiological findings like the characteristic popcorn appearance on the MRI scan, and hemosiderin deposition. Other findings, such as peritumoral edema, calcifications, hypointense appearance to gray matter on T1-weighted MRI scans, and mixed signal intensity on T2-weighted MRI scans, are also reported in cavernous malformations in different stages after hemorrhage. It has been reported that cavernoma malformations may mimic meningioma [25, 44–46]. Cavernous malformations may be misdiagnosed as the more commonly seen meningiomas, particularly when they do not display the same MRI characteristics as a typical cavernoma [45, 17]. To the best of our knowledge, this is the first report demonstrating that meningiomas can mimic cavernous malformations.
Our case report highlights the fact that preoperative diagnosis of atypical meningioma is challenging and classical MRI features may not be sufficient to distinguish the different pathologic entities, moreover, they can be misleading. Therefore, caution must be used in the preoperative differential diagnosis. In our case report, an angiography could have helped to distinguish the meningioma from a cavernous malformation, but this is not guaranteed due to the possibility of showing the same radiological features [41].
The literature review shows that intraparenchymal meningiomas occur in all regions of the brain, including supratentorial and infratentorial areas. Intraparenchymal meningiomas were, in most cases, not considered and misdiagnosed as other lesions. The clinical presentation was site dependent; seizures were the most common symptom. Unlike the usual meningioma, where the meningothelial variant of meningioma is the most common, the fibrous variant of meningioma is dominant in intraparenchymal meningiomas [47]. It seems that the fibrous variant of meningioma is generally dominant in meningiomas without dural attachment, such as intraventricular meningiomas. The large number of published cases of meningiomas without dural-base attachment establishes the fact that not all meningiomas are dural based.
Conclusions
The meningioma in our patient had two unusual features: the subcortical location and the radiological appearance mimicking cavernous malformation. This case report highlights the fact that the typical radiological appearance of one lesion may sometimes be misleading. Intraparenchymal meningiomas can have multiple entities mimicking their presentation. Caution must be used in the preoperative differential diagnosis.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Abbreviations
- CT:
-
Computed tomography
- MRI:
-
Magnetic resonance imaging.
References
Nakamura M, Roser F, Bundschuh O, Vorkapic P, Samii M: Intraventricular meningiomas: a review of 16 cases with reference to the literature. Surg Neurol. 2003, 59: 491-504.
Karadereler S, Aker F, Berkman Z: Intraparenchymal meningioma in a child. Case report and review of the literature. J Neurosurg. 2004, 101 (Suppl 1): 112-115.
Sano K, Wakai S, Ochiai C, Takakura K: Characteristics of intracranial meningiomas in childhood. Childs Brain. 1981, 8: 98-106.
Abraham J, Chandy J: Meningiomas of the posterior fossa without dural attachment. J Neurosurg. 1963, 20: 177-179. 10.3171/jns.1963.20.2.0177.
Chiocca EA, Boviatsis EJ, Westmark RM: Deep sylvian fissure meningioma without dural attachment in an adult: case report. Neurosurgery. 1994, 35: 944-946. 10.1227/00006123-199411000-00021.
Okamoto S, Handa H, Yamashita J, Tokuriki Y: Deep Sylvian meningiomas. Surg Neurol. 1985, 23: 303-308. 10.1016/0090-3019(85)90101-6.
Ahmed M, Lee JH, Masaryk TJ: Meningiomas: Imaging Mimics. Meningiomas Diagnosis, Treatment, and Outcome. Edited by: Lee JH. 2009, London: Springer-Verlag Limited, 67-87.
Chang A, Ross S: Diagnostic Neuroradiology: CT, MRI, fMRI, MRS, PET, and Octreotide SPECT. Meningiomas Diagnosis, Treatment, and Outcome. Edited by: Lee JH. 2009, London: Springer-Verlag Limited, 55-65.
Shen WC, Chenn CA, Hsue CT, Lin TY: Dural cavernous angioma mimicking a meningioma and causing facial pain. J Neuroimaging. 2000, 10: 183-185.
Wada T, Suzuki M, Beppu T, Arai H, Yoshida Y, Ogawa A, Sasou S: A case of subcortical meningioma. Acta Neurochir (Wien). 2000, 142: 209-213. 10.1007/s007010050026.
Emoto S, Okada T: A case of subcortical meningioma. Nippon Geka Hokan. 1954, 23: 397-400.
Drake JM, Hendrick EB, Becker LE, Chuang SH, Hoffman HJ, Humphreys RP: Intracranial meningio mas in children. Pediatr Neurosci. 1986, 12: 134-139.
Suematsu K, Tokuda S, Miyazaki Y: Intracranial Meningioma in a five-month-old infant: A case report and review of the literature. No To Shinkei. 1974, 26: 453-464.
Morimoto M, Aoki H, Sadamitsu N, Nakajima R: Cystic meningioma-report of two cases. No Shinkei Geka. 1976, 4: 805-809. Japanese
Mena H, Garcia J: Primary brain sarcomas light and electron microscopic features. Cancer. 1978, 42: 1298-1307. 10.1002/1097-0142(197809)42:3<1298::AID-CNCR2820420340>3.0.CO;2-K.
Legius E, Vles JS, Casaer P, Plets C, Dom R: Intraparenchymal meningioma in a 14-month-old infant: case report. Brain Dev. 1985, 7: 622-624. 10.1016/S0387-7604(85)80011-5.
Schroeder BA, Samaraweera RN, Starshak RJ, Oechler HW: Intraparenchymal meningioma in a child: CT and MR findings. J Comput Assist Tomogr. 1987, 11: 192-193. 10.1097/00004728-198701000-00046.
Kimura H, Nakagawa K, Sakaki S, Matsumoto M: Intracranial meningioma of an infant: a case report. no Shinkei Geka. Neurol Surg. 1987, 15: 663-668.
Sakaki S, Nakagawa K, Kimura H, Ohue S: Intracranial Meningiomas in Infancy. Surg Neurol. 1987, 28: 51-57. 10.1016/0090-3019(87)90206-0.
Mamourian AC, Lewandowski AE, Towfighi J: Cystic intraparenchymal meningioma in a child: case report. AJNR. 1991, 12: 366-367.
Matsumoto M, Nakazawa K, Hashimoto T, Nakamura N: A case of meningioma in a child associ ated with focal motor seizure. Shoni No Noshinkei. 1992, 17: 285-288.
Nakahara S, Yoshino K, Hasegawa Y, Tani S, Numoto RT, Tanaka J: A meningioma in the posterior fossa without dural attachment: case report. No Shinkei Geka. 1993, 21: 849-852.
Kaneko F, Sasaki K, Kobayashi T: Intra-axial meningioma in childhood-case report. Tokushima Shimin Byoin Igaku Zasshi. 1993, 7: 131-134. Japanese
Kohama I, Sohma T, Nunomura K, Igarashi K, Ishikawa A: Intraparenchymal meningioma in an infant-case report. Neurol Med Chir. 1996, 36: 598-601. 10.2176/nmc.36.598.
Sathi S, Folkerth R, Madsen JR: Cavernous angioma of the posterior fossa dura mimicking a meningioma: case report and review of literature. Surg Neurol. 1992, 38: 257-260. 10.1016/0090-3019(92)90035-L.
Sanli M, Altinors N, Demiralp O: Intraparenchymal meningioma: an unusual radiological and anatomic presentation of a meningioma. Case report. Neurosurg Rev. 1996, 19: 285-287. 10.1007/BF00314848.
Starshak RJ: Cystic meningiomas in children: a diagnostic challenge. Pediatr Radiol. 1996, 26: 711-714. 10.1007/BF01383385.
Teo JG, Goh KY, Rosenblum MK, Muszynski CA, Epstein FJ: Intraparenchymal clear cell meningioma of the brainstem in a 2-year-old child. Case report and literature review. Pediatr Neurosurg. 1998, 28: 27-30. 10.1159/000028614.
Shimizu K, Furuhata S, Sasai S, Tominaga S, Takayima Y: Intracerebral cystic meningioma-case report. Neurol Med Chir (Tokyo). 1999, 39: 530-533. 10.2176/nmc.39.530.
Tekko I, Cinel L, Zorludemir S: Intraparenchymal meningioma. J Clin Neurosci. 2005, 12 (5): 605-607. 10.1016/j.jocn.2004.08.023.
Kim C-H, Park S-H, Hwang J-H, Hamm I-S: A subcortical anaplastic meningioma. J Korean Neurosurg Soc. 2005, 37: 235-237.
Zhang J, Chi LY, Meng B, Li F, Zhu SG: Meningioma without dural attachment: case report, classification, and review of the literature. Surg Neurol. 2007, 67 (5): 535-539. 10.1016/j.surneu.2006.07.011.
Dutta D, Lee HN, Munshi A, Gupta T, Kane S, Sridhar E, Jalali R: Intracerebral cystic rhabdoid meningioma. J Clin Neurosci. 2009, 16: 1073-1074. 10.1016/j.jocn.2008.07.085.
Yamada SM, Kawanishi YFY, Shimizu K: A cystic meningioma misdiagnosed as malignant glioma by radiologic and intraoperative histological examinations. Brain Tumor Pathol. 2010, 27: 111-115. 10.1007/s10014-010-0273-9.
Shimbo D, Kato T, Takeda M, Ikeda H: Intraparenchymal Meningioma in child: case report. Neurol Med Chir (Tokyo). 2011, 51: 793-797. 10.2176/nmc.51.793.
Jiang X-B, Ke C, Han Z-N, Lin S-H, Mou Y-G, Luo R-Z, Wu S-X, Chen Z-P: Intraparenchymal papillary meningioma of brainstem: case report and literature review. World J Surg Oncol. 2012, 10: 2-6. 10.1186/1477-7819-10-2.
Louis DN, Scheithauer BW, Budka H, Von Deimling A, Kepes JJ, Kleihues P, Cavenee WK: World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of the Nervous System. 2000, Lyon: IARC Press
Tung H, Apuzzo MLJ: Meningiomas of the Third Ventricle and Pineal Region. Meningiomas. Edited by: Al-Mefty O. 1991, New York: Raven Press, 583-592.
Cho BK, Wang KC, Chang KH: Deep sylvian meningioma in a child. Childs Nerv Syst. 1990, 6: 228-230. 10.1007/BF01850980.
Winkler P, Buhl R, Tonn J: Intraventricular Meningiomas. Meningiomas Diagnosis, Treatment, and Outcome. Edited by: Lee JH. 2009, London: Springer-Verlag Limited, 495-514.
Curnes J: MR imaging of peripheral intracranial neoplasms extraaxial vs intraaxial masses. J Comput Assist Tomogr. 1987, 11: 932-937. 10.1097/00004728-198711000-00002.
Wasenko JJ, Hochhauser L, Stopa EG, Winfield JA: Cystic meningiomas: MR characteristics and surgical correlations. AJNR. 1994, 15: 1959-1965.
Elsharkawy AE, Abuamona R, Bergmann M, Salem S, Gafumbegete E, Röttger E: Cortical anaplastic ependymoma with significant desmoplasia: case report and literature review. Case Rep Oncol Med. 2013, 2013: 6-
Perry A, Stafford SL, Scheithauer BW, Suman VJ, Lohse CM: Meningioma grading: an analysis of histologic parameters. Am J Surg Pathol. 1997, 21: 1455-1465. 10.1097/00000478-199712000-00008.
Hwang SW, Pfannl RM, Wu J: Convexity dural cavernous malformation with intradural and extradural extension mimicking a meningioma: a case report. Acta Neurochir (Wien). 2009, 151: 79-83. 10.1007/s00701-008-0175-3.
Perry JR, Tucker WS, Chui M, Bilbao JM: Dural cavernous hemangioma: an under-recognized lesion mimicking meningioma. Can J Neurol Sci. 1993, 20 (3): 230-233.
Prayson RA: Pathology of Meningiomas. Meningiomas Diagnosis, Treatment, and Outcome. Edited by: Lee JH. 2009, London: Springer-Verlag Limited, 31-43.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
SJ carried out the design of the study and drafted the manuscript. ACS carried out the neuropathological examination and drafted the pathology section of the manuscript. UW carried out the neuroradiological assessment. TAP conceived of the study, participated in its design and coordination, and helped to draft the manuscript. AEE conceived of the study, participated in its design and coordination, helped to draft the manuscript, and carried out the literature review and discussion section. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Jadik, S., Stan, A.C., Dietrich, U. et al. Intraparenchymal meningioma mimicking cavernous malformation: a case report and review of the literature. J Med Case Reports 8, 467 (2014). https://doi.org/10.1186/1752-1947-8-467
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1752-1947-8-467