Abstract
Background
Research has shown that obese individuals have cognitive deficiencies in executive function, leading to poor planning and impulse control, and decision-making difficulties. An intervention that could help reduce these deficits and in turn help weight loss maintenance is Cognitive Remediation Therapy for Obesity (CRT-O). We aim to examine the efficacy of manualised CRT-O, which is intended to improve executive function, enhance reflective practice and help weight loss maintenance.
Methods/Design
A randomised controlled trial (registered with the Australian New Zealand Clinical Trials Registry) will be conducted. First, 90 obese adults (body mass index >30 kg/m2) in the community will receive three weekly sessions of a group Behaviour Weight Loss Treatment (BWLT), and then will be randomised either to receive CRT-O or to enter a no-treatment control group. CRT-O training will comprise twice-weekly sessions of 45 minutes over a 4 to 6 week period, for a total of eight sessions. Measurement points will be at baseline, post CRT-O (or 4 to 6 weeks after BWLT for the no-treatment control), 3 months post treatment and 1 year post treatment. The primary outcome will be executive function and secondary outcome measures will include participants’ body mass index, hip to waist ratio, eating behaviours and quality of life.
Discussion
This is the first study of its kind to examine the efficacy of Cognitive Remediation Therapy for obese adults through a randomised controlled trial.
Trial Registration
Australian New Zealand Clinical Trials Registry number: 12613000537752. Date of registration: 14 May 2013.
Similar content being viewed by others
Background
Approximately 1 billion adults are currently overweight (body mass index (BMI) 25 to 29.9 kg/m2) and a further 475 million are obese (BMI >30 kg/m2) [1]. Ranking second only to smoking as a preventable cause of death, obesity contributes to over 300,000 deaths per year [2]. Obesity is also associated with a wide range of medical and psychological sequelae, eating disorder behaviours such as binge eating and subsequent impaired health-related quality of life (HRQoL) [3–5]. Although 5% to 10% weight loss is associated with clear health benefits, the prevention of weight regain has remained a challenge. Even with the help of professionals and extended behavioural treatments, weight regain typically occurs when professional contact ends [6]. By 3 to 5 years post-treatment, about 85% of patients have regained weight or even exceeded their pre-treatment weight [7].
Empirical research has found obesity to be associated with cognitive impairment, especially in executive function, irrespective of the presence of binge eating [8] and independent of co-morbid medical conditions such as diabetes, hypertension and cancer, which are themselves associated with adverse cognitive effects [9, 10]. Executive function encompasses a range of cognitive processes facilitating initiation, planning, regulation, inhibition, sequencing and achievement of complex goal-oriented behaviour [11]. The association of obesity and executive deficits is found across the age span, in children, adolescents, older adults, middle-aged adults and young adults [12–14]. A review [15] found that the evidence is highly consistent, with 22 out of 24 studies showing a negative association between obesity and cognition, especially in executive function. For example, inhibitory control, an aspect of executive function, involves the suppression of actions that are contextually inappropriate and interfere with behavioural goals. Studies of obese adults in the community have found executive deficits to be positively associated with disinhibited eating and greater food cravings [16]. Furthermore, obese individuals have been found to demonstrate cognitive impulsivity, an autonomic readiness to make quick decisions, which prevents successful inhibition of a prepotent behavioural response. It has been shown that impulsive subjects have marked limitations for learning suitable associations between reward and punishment [17, 18] and as a result they are more influenced by immediate rewards than by future consequence [18]. Hence, executive deficits have been shown to impair the capacity for impulse regulation, including control over the impulse to eat excessively [19]. Furthermore, evidence indicates a positive association between a higher BMI and decision-making impairments [20]. Findings from a study on the decision-making profiles of obese adult females using the Iowa Gambling Task showed a preference for high immediate reward, despite higher future losses in terms of both physical and psychological outcomes [18]. Studies have also shown that obese individuals perform similarly on the Iowa Gambling Task as those with anorexia nervosa, for example, see [21], and as patients with orbitofrontal dysfunction [22], and worse than those who are substance dependent [23]. While executive function deficits have been shown to be similar in anorexia nervosa and obesity, obese individuals show worse performance in the inhibition response measured by the Stroop test compared to individuals with anorexia nervosa or healthy controls [24].
The mechanism by which obesity is associated with cognitive function is, however, unclear at present [8]. Smith and colleagues [15] suggested a bidirectional relationship between obesity and executive function, where obesity impairs executive function via biological mechanisms, such as inflammatory markers or glucose abnormalities, and impaired executive function impacts on obesity by causing an inability to regulate food intake, plan ahead, inhibit responses or act impulsively. There is some evidence for this bidirectional association. One longitudinal study showed that poor executive function at age four predicted a high BMI at age six [14]. It is possible, based on the evidence presented above, that cognitive deficiencies may contribute to increased adiposity by exacerbating weight gain or regain after weight loss, and targeting these deficits in the obese has the potential to improve participants’ response to therapy. This led to the development of a novel treatment for weight disorders, namely Cognitive Remediation Therapy for Obesity (CRT-O) [15, 25].
CRT-O is a manualised treatment derived from Cognitive Remediation Therapy (CRT), which is used to treat people with addiction, feeding or eating disorders. In trials of people with a substance-use disorder, computer-assisted CRT has been shown to reduce individuals’ need for immediate reward and improve their decision-making [26]. Experimental studies have shown that practicing inhibitory control, an aspect of executive function, reduces the consumption of high-calorie foods [12, 27, 28]. Specifically, studies have shown that improving inhibition of behaviour towards high-calorie items, via a computerised go/no-go task, reduced the consumption of palatable foods across a 1-day period [12, 28]. Similarly, manualised Cognitive Remediation Therapy for Anorexia Nervosa (CRT-AN) has been shown to be associated with cognitive improvements in addition to improvements in eating-disorder-related quality of life at the end of treatment and eating-disorder psychopathology at a 6-month follow-up [29]. Furthermore, there were low dropout rates and high levels of acceptability among both patients and therapists [30].
Like CRT-AN, CRT-O is designed to provide individuals with the tools to think differently about their cognitive style and how they address food. However, in CRT-O the intent is to help maintain weight loss and prevent further weight gain by linking the thinking style to food intake and exercise behaviours. CRT-O is a brief eight-session individual therapy where simple cognitive tasks and exercises that encourage reflective learning and insight into a participant’s own thinking process are administered together with intra-session experimentation. The rationale being that this will improve various aspects of executive function, including cognitive flexibility, central coherence (attention to detail) and problem-solving and will in turn improve participants’ ability to follow the guidelines of a behavioural weight-loss programme. Supporting this are promising results from a small trial (n =44) by Verbeken et al. [12], testing executive function training with games in children. In this study, moderate to large effect sizes (standardised mean differences between 0.5 and 0.6) were found in executive function outcomes, such as improvements in a behaviour rating inventory of executive function and in a working memory task that favoured training. However, there were smaller effects for a task assessing response inhibition. To our knowledge the efficacy of this approach has not yet been investigated in adults.
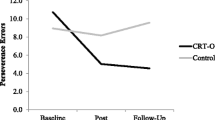
We have designed the present randomised controlled trial (RCT) to test the efficacy of manualised individual face-to-face CRT-O as developed by Smith and colleagues [25]. The primary outcome in this superiority trial is improvement in executive function demonstrated at end of treatment and at 3 months, and maintained at the 1-year follow-up. Secondary outcomes are participants’ BMI, hip to waist ratio, eating behaviours and quality of life. Since studies on anorexia nervosa have found an improvement in quality of life, we wish to examine whether quality of life improves after CRT-O. In this RCT, all participants receive standard care for weight loss, namely group-based Behaviour Weight Loss Treatment (BWLT), and are then randomised to a CRT-O group or a no-treatment control group. CRT-O targets executive function deficits and changes in thinking style, whereas BWLT targets health literacy and weight-loss strategies including psycho-education, weight monitoring, dietary advice and exercise planning. Perceived barriers to weight management are discussed and challenged.
The primary hypothesis is that, compared to those who receive BWLT only, participants who receive BWLT plus CRT-O will demonstrate improved executive function post treatment, which is maintained at the 3-month and 1-year follow-ups. The secondary hypotheses are that that executive function changes will predict changes in weight, and compared to those who receive BWLT only, participants who receive BWLT plus CRT-O will have improved (i) weight loss (assessed by BMI and hip to waist ratio), (ii) HRQoL and (iii) dietary habits (including reduced binge eating) at post treatment and maintained at the 3-month and 1-year follow-ups.
Methods/Design
Participants
First, 90 obese individuals are recruited via direct advertisement to the community in Sydney, Australia. Inclusion criteria are: BMI ≥30 kg/m2, age 18 to 55 years, current weight under 180 kg, ability to provide informed consent and having completed 10 years of education in English. Participants who are depressed, have a binge eating disorder, are currently on psychotropic medication, have hypertension (medicated or not medicated), type 2 diabetes, or high cholesterol are eligible. Participants are excluded if they have a history of psychosis, head injury, neurological disorder including degenerative or inflammatory conditions or stroke, attention deficit hyperactivity disorder, epilepsy, developmental or intellectual disability; are unable to complete the testing (e.g. due to hearing, vision or language impediment); are on regular sedative or stimulant medication; and/or report regular substance use or abuse (for alcohol, more than two standard drinks five times a week). Individuals are also be excluded if they regularly use sedatives, hypnotics, antipsychotics, or anti-cholinergic or cholinergic medication. The sample size of 45 per group has been determined based on power estimates using Cohen’s tables for an estimated effect size of 0.6, power of 0.8, one-tailed test, P <0.05 and attrition of 20%. Although there are no previous studies of adults with obesity, these levels are commensurate with those achieved by Verbeken et al. [12].
Procedure
Recruitment was via advertisements placed on social media sites, university and community centre notice boards and via media interviews with journalists from metropolitan and community newspapers. The initial screen was by phone to establish potential eligibility. This was followed by a face-to-face psychological and neuropsychological assessment. All 90 participants then receive group-based BWLT that will run once a week for 3 weeks, each ses sion lasting 90 minutes. At the completion of the third and final session, participants are randomly allocated to CRT-O or no treatment. Randomisation and allocation concealment are conducted using an external computer-based program [31]. The RCT is registered with the Australian New Zealand Registry of Clinical Trials (trial id ACTRN12613000537752) (Figure 1).
Assessment
After providing information on demographic and medical factors, including their weight, height, waist and hip circumferences, participants undergo a battery of neuropsychological and psychological tests. All assessment measures will be administered at baseline, after 7 to 9 weeks (3 weeks of BWLT and 4 to 6 weeks of either CRT or no treatment), and at the 3-month and 1-year post-CRT follow-ups. At the follow-ups, participants will also be asked whether they received any further treatment for their obesity. We will control for this in the final analyses.
Neuropsychological assessment
The six neuropsychological tests employed are selected because they cover different aspects of executive functioning and are commonly used in clinical and research settings. The tests are administered individually to all subjects by a trained clinical psychologist or neuropsychologist.
-
1.
The Wisconsin Card Sorting Test (WCST) 64: The computerised version of WCST [32–34] will be used. In this test, subjects are instructed to categorise a series of cards according to one of three stimulus features (colour, shape or number of illustrations on them), without this principle being revealed to the subject. After each association, the only feedback given is whether a match is correct or incorrect, the idea being that subjects should infer how to categorise based on the feedback they receive. This test measures categorisation, inference, testing of hypotheses, cognitive flexibility, cognitive inhibition and response to feedback [16]. The number of total errors and perseverative errors and failure to maintain a set are the dependent measures. WCST is considered to be a valid measure of abstract reasoning ability to maintain an appropriate planning and problem-solving strategy across changing stimulus conditions to achieve a future goal, and it is the most widely used test of executive function [35].
-
2.
Digit Span, a subtest of the Wechsler Adult Intelligence Test III [36]: In this test, the subject is presented with a series of digits to be repeated in the same order (Digit Span Forward) followed by another series to be repeated backwards (Digit Span Backward). Digit Span Forward assesses the phonological loop and Digit Span Backward assesses central executive aspects of the verbal working memory [37]. The score is calculated based on the number of correct responses that could be immediately retained.
-
3.
Trail Making Test (TMT) [38]: This will be used to assess psychomotor speed, visual integration, cognitive flexibility and inhibitory control. This test measures the subject's ability to connect written numbers in an ascending order (Trail A), and, afterwards, to connect numbers and letters, alternating numbers in ascending order and letters in alphabetical order (Trail B), for example, 1-A-2-B. The score is the response time taken to complete the respective trails [35].
-
4.
Computerised Reward–Loss Task [39]: This is a probabilistic classification task that assesses decision-making. In each trial, participants view one of four images and are asked to guess whether it belongs to category A or B. In the reward-learning task, if the participant correctly guesses the category membership for a trial, a reward of +25 points is received. If the participant guesses incorrectly, no feedback is given. In the punishment-learning task, if the participant guesses incorrectly for a trial, a punishment of -25 points is received, and correct guesses receive no feedback. The reward and punishment trials are intermixed so that no-feedback trials are ambiguous. The ±25 points symbolise quarter dollars that are won or lost, but no real payments are used in this study. The dependent variables are the number of errors made and completion time.
-
5.
Behaviour Rating Inventory of Executive Function, Adult Version (BRIEF-A) [40]: This is a widely used, standardised measure based on a multidimensional model of executive function and the only available self-report measure of executive function at present. The BRIEF-A captures information on an adult’s executive functions or self-regulation in his or her everyday environment.
-
6.
Rey–Osterrieth Complex Figure Test [41, 42]: This test (both copy and a 3-minute recall) will be used to measure attention to detail (central coherence), perceptual and organisational skills, and nonverbal memory. Scores will be calculated for the copy and 3-minute delay portions of the test using the scoring manual.
Pre-morbid IQ
The Australian version of the National Adult Reading Test, Revised [43, 44] is administered to control for pre-morbid intelligence. This is a widely used reading test that provides an estimate of pre-morbid IQ. It consists of 50 irregularly spelled words, listed roughly in order of difficulty. The test involves participants being presented with a word card and instructed to read each word out aloud. Interviewers then record correct pronunciations, with the total number of correct responses being the score.
Anthropometric measures
For participants, we measure: (1) height and weight with calibrated scales (from which we will derive BMI in kg/m2), and (2) hip and waist circumferences to calculate the waist to hip ratio.
Demographics and medical history
Age, gender, education and socio-economic status (by postcode) are recorded in the general questionnaire. This form also includes medical history, current medical conditions and medication.
Nutrition and lifestyle behaviours
These are assessed using a written 24-hour dietary recall method [45]. A brief questionnaire examining basic food group frequencies and portion sizes, and a questionnaire on frequency and intensity of exercise are used, both adapted from large Australian population questionnaires in the Australian Women’s Health project [46] and the National Nutrition Survey, Australia [47].
Psychological assessment
The Clinical Obesity Maintenance Model [48] proposed by Raman and colleagues argues that psychological variables, such as habitual cluster behaviours, emotional dysregulation and mood, interact with executive functioning and impact on the overeating and binge eating behaviours of obese individuals. Hence, the following measures are included in this RCT to investigate the broader range of maintaining mechanisms, including but not limited to executive deficits, and to ensure both groups are equivalent at baseline in other measures that may impact on weight.
Depression, Anxiety and Stress Scales
Depression symptoms in the obese in this study are measured by the 21-item Depression, Anxiety and Stress Scales [49]. Obesity has been shown to increase the risk of developing depression and depression has been found to be predictive of obesity [50], and there is a dose–response gradient in that the association between depression and obesity was stronger than the association between depression and being overweight [51]. There is ample evidence that depressive disorders are also associated with deficits in attentional functions, executive control and lowered cognitive flexibility [52]; verbal learning and memory [53] and interpretation biases [54–57]. This test has been validated in a number of clinical and non-clinical populations and is psychometrically sound with good reliability and validity to measure depressive symptoms [49, 58].
Eating disorder symptoms
Individuals with eating disorder symptoms, such as binge eating, may have more difficulty losing weight [59] and hence this will be controlled for in our analyses. Eating disorder symptoms are measured by the Eating Disorder Examination Questionnaire [60]. Acceptable internal consistency and test–retest reliability have been demonstrated for this questionnaire [61]. It has 36 items and measures concerns about shape, weight and eating; restraint and self-reported binge eating. Subscale scores for shape, weight and eating concerns and restraint range between 0 and 6. A higher score indicates more severe eating psychopathology.
The Grazing Questionnaire
The Grazing Questionnaire [62] is used to measure the participants’ food grazing behaviours, i.e., to assess whether there is a pattern of continual overeating. Grazing is increasingly recognised as an important eating behaviour associated with obesity [62]. This questionnaire has been validated in a university sample of both genders and has demonstrated high internal consistency, test–retest reliability and convergent validity at initial testing [62].
Habit clusters
Habit clusters are measured by the Modified Self-Reported Habit Index [63]. Research has shown that when cognitive resources become limited, individuals are inclined to make heuristic-based choices [64]. This is reflected in obesity-maintaining dietary habits. Given the habitual nature of eating and the rapidity with which people make eating decisions [64], the behaviours are likely to be the consequence of automatic responses to contextual food cues, many of which lead to increased caloric consumption and poor dietary choices [65, 66]. This index has been shown to be a valid and reliable scale to measure physical activity habits [67]. For the purposes of this study, this index has been modified to include other obesity-related behaviours such as sedentary behaviours, smoking and alcohol consumption.
Emotion dysregulation
Emotion dysregulation is measured by the Difficulties in Emotion Regulation Scale (DERS) [68]. Emotion regulation has been described as a continuous, dynamic system responsive to all emotional experience, consisting of both autonomic and controlled processes [69, 70], perhaps mediated by executive function [48]. Since it relates to obesity, problems in attentional and inhibitory control have been associated with binge eating and eating pathology in adults [71]. The DERS is a 36-item self-report questionnaire that assesses clinically relevant difficulties in emotion regulation (with a particular emphasis on negative emotions). There is evidence to support the reliability of DERS scores. Specifically, DERS scores have been found to demonstrate good test–retest reliability [72] and the overall DERS score and subscale scores have been found to have high internal consistency within both clinical, for example [68, 73], and nonclinical populations, for example [68, 74]. Support for the construct and predictive validity of DERS scores within both clinical and nonclinical populations has also been found, for example [69].
Health-related quality of life
HRQoL is measured with the 12-item Short Form [75], which is a widely used quality of life measure with good construct and criterion validity and with adequate sensitivity to change.
Behavioural weight-loss group intervention
The BWLT in this RCT targets diet and exercise through behavioural modification techniques over three 90-minute weekly sessions. In the first session, obesity-related risk awareness, challenges with perceived barriers and perceived personal control are discussed in depth. Cognitive challenging techniques are taught and in-session goal setting practices are conducted. In the second session, participants receive comprehensive education about nutrition, hunger management and healthy eating practices. Problem-solving techniques are taught so that participants can effectively deal with difficult situations that threaten their weight-control efforts. National physical activity guidelines are discussed and further training given on goal setting and goal achievement. In this last session, attention is given to motivation enhancement and relapse prevention strategies to help individuals maintain their weight loss.
Cognitive Remediation Therapy for Obesity
CRT-O is a manualised intervention that consists of mental exercises aimed at improving cognitive strategies, thinking skills and information processing through practice. CRT, in particular, promotes reflection on thinking styles, develops metacognition and helps to explore and apply new thinking strategies in everyday life. The primary function of CRT is to improve the thinking process rather than the content [76–78]. In the absence of a published manual, a CRT-O manual was developed to meet the needs of the obese participants for the purposes of this RCT. The intervention is conducted face-to-face and delivered by the first author (JR), who is a registered clinical psychologist in Australia. The principles, structure and main components of the original CRT-AN are maintained. Some important modifications, however, have been made to adapt the manual for obesity and these are described in Smith et al. [25].
Treatment fidelity
The first author (JR) was trained in a workshop on CRT-AN by the developers of this treatment approach (Kate Tchanturia and Helen Davies, Institute of Psychiatry, King’s College London, UK). The third author (ES) piloted the different versions of manualised CRT-O with three people. Concomitant interventions outside of the trial setting are neither encouraged nor prohibited during the intervention phase. To increase transparency and documentation as well as for quality and treatment fidelity assessment, 10% of the sessions will be audiotaped.
Data collection, management and analysis
Data is collected at baseline, end-of-treatment and the 3-month follow-up by the trial therapist. An independent assessment, blind to intervention group, will be made at the 1-year follow-up. Data is entered, cleaned and coded by a research assistant, blind to group allocation, and stored at a secure university facility according to university protocols. An independent statistician will conduct all preliminary analyses. The Statistical Package for Social Sciences (SPSS) statistics will be used.
Neuropsychological measures will first be examined independently and will then be integrated in an executive function composite following the procedure recommended by Rosnow and Rosenthal [79, 80] and applied by Clark et al. [81]. The composite score will be generated by converting each executive function scale across all assessment points to z- scores, and then averaging across the measures.
Descriptive statistics will be used to present demographic and clinical data including eating disorder features. Baseline univariate between-group tests will be used to compare outcome variables and clinical and demographic data for the groups. Data will be analysed following the intention-to-treat principle. Linear mixed effects modelling [82] will be used to test for between-group differences in the continuous outcome measures, namely the composite scores of cognitive function, waist circumference and BMI, and potential confounds (e.g., levels of depression, anxiety, stress and emotion dysregulation). Generalised estimating equations [83] with a logit response function, or logistic regression, will be used for dichotomous outcomes, such as achieving a 5% reduction in body weight. Effect sizes between and within the two groups will be calculated with Cohen’s d computed with the pooled standard deviation, and the odds ratio will be presented where appropriate.
Ethics and dissemination
The study has been approved by the Human Research Ethics Committee of the University of Western Sydney (H9787). Written informed consent has been obtained from each subject after thorough information about the study was provided. Participants were advised that all data collected will be de-identified prior to analysis and stored securely in electronic and paper forms. All identifying information (e.g., signed consent forms) will be kept separate from other data and will be held in confidence. Only investigators and authorised research personnel will have access to the data. The results will be submitted to peer-reviewed scientific publications, presented at national and international scientific meetings, presented to relevant community fora and released in lay synopsis form to media outlets.
Discussion
Obesity is an important global public health issue. Due to the long-term failure of interventions for obesity, there is a desperate need to develop novel and innovative approaches to treatment. In particular, weight-loss maintenance remains a major challenge. Obese individuals are known to suffer from significant cognitive deficits, especially in executive function. We have identified the possibility that an intervention such as CRT could improve treatment outcomes and has the potential to improve current therapy practices.
The application to CRT for obesity is highly novel. Executive function deficiencies in the obese are a potential target and unlike other contributing factors (e.g. diet and exercise) have not previously been investigated. CRT-O, which aims to improve specific deficiencies such as inflexibility, poor problem-solving and poor attention to detail (central coherence), could have benefits for the health of the increasing number of obese individuals in our community and reduce the economic burden from obesity and its medical and psychological sequelae. Our study is designed to compare two groups, a BWLT and CRT-O group with a BWLT and no-treatment group, to allow us to draw conclusions about the specific efficacy of CRT-O following BWLT training compared to no treatment.
The strengths of our study design include adequate concealment of randomised group allocation, use of validated and standardised assessments, and independent blinded data analysis. A limitation is that follow-up assessments are blinded only at 1 year. However, this is an important outcome time, since to be clinically meaningful for longer-term weight-loss maintenance, improvements in cognition need to be sustained over time. Furthermore, the Institute of Medicine has defined criteria for assessing successful weight maintenance as a weight loss of ≥5% of body weight that is maintained for at least a year [84]. For the purposes of this study, the Institute of Medicine’s criteria will be used as a standard definition of successful weight maintenance at this study's 1-year follow-up. Another limitation is that therapeutic time with a therapist is not matched between conditions and participants are not blind to condition, i.e., we are not employing a control–therapy comparison. As obesity tends to get worse without treatment, at our 1-year follow-up, we will examine whether individuals’ BMI is significantly higher in the no-treatment group compared to the CRT-O group. We will also control for any additional treatment each group received in that time and whether the change of executive function predicted that weight loss.
The design of this RCT offers a pathway to address, for the first time, the integral aspects of executive function and its impact on obesity, and their interaction with other maintaining factors such as emotion dysregulation, depression and habitual cluster behaviours. It is hoped that the findings of this RCT will provide an important first step towards an understanding of the potential of CRT in obesity. Based on the limited success of current behavioural weight-loss programmes and coupled with the data on the executive function deficiencies in obesity, it appears likely that improving an individual’s executive function has the potential to enhance treatment outcomes for obesity.
Trial status
Recruitment is now complete; therapy and data collection are in progress.
Abbreviations
- BMI:
-
body mass index
- BRIEF-A:
-
Behavior Rating Inventory of Executive Function, Adult Version
- BWLT:
-
Behaviour Weight Loss Treatment
- CRT:
-
Cognitive Remediation Therapy
- CRT-AN:
-
Cognitive Remediation Therapy for Anorexia Nervosa
- CRT-O:
-
Cognitive Remediation Therapy for Obesity
- DERS:
-
Difficulties in Emotion Regulation Scale
- HRQoL:
-
health-related quality of life
- RCT:
-
randomised controlled trial
- WCST:
-
Wisconsin Card Sorting Test.
References
World Health Organisation: Obesity and Overweight Fact Sheet. 2004, [http://www.who.int/mediacentre/factsheets/fs311/en/]
Satcher D: Surgeon general’s column. Commissioned Corps Bull. 2002, 16 (2): 1-2.
Pagoto S, Schnieder K, Appelhans BM, Curtin C, Haduk A: Psychological comorbidities of obesity. Psychological Co-Morbidities of Physical Illness: A Behavioral Medicine Perspective. Edited by: Pagoto S. 2011, New York: Springer, 1-72.
Reichborn-Kjennerud T, Bulik CM, Sullivan PF, Tambs K, Harris JR: Psychiatric and medical symptoms in binge eating in the absence of compensatory behaviors. Obesity. 2004, 12: 1445-1454. 10.1038/oby.2004.181.
Vetter ML, Wadden TA, Lavenberg J, Moore RH, Volger S, Perez JL, Sarwer DB, Tsai AG: Relation of health-related quality of life to metabolic syndrome, obesity, depression and comorbid illnesses. Int J Obes. 2011, 35: 1087-1094. 10.1038/ijo.2010.230.
Perri MG, Corsica JA: Improving the maintenance of weight lost in behavioral treatment of obesity. Handbook of Obesity Treatment. Edited by: Wadden TA, Stunkard JA. 2002, New York: Guilford Press, 357-379.
Wadden TA, Osei S: The treatment of obesity: an overview. Handbook of Obesity Treatment. Edited by: Wadden TA, Stunkard JA. 2002, New York: Guilford Press, 229-248.
Gunstad J, Lhotsky A, Wendell CR, Ferrucci L, Zonderman AB: Longitudinal examination of obesity and cognitive function: results from the Baltimore Longitudinal Study of Aging. Neuroepidemiology. 2010, 34: 222-229. 10.1159/000297742.
Biessels GJ, Deary IJ, Ryan CM: Cognition and diabetes: a lifespan perspective. Lancet Neurol. 2008, 7: 184-190. 10.1016/S1474-4422(08)70021-8.
Anderson-Hanley C, Nimon JP, Westen SC: Cognitive health benefits of strengthening exercise for community-dwelling older adults. J Clin Exp Neuropsychol. 2010, 32: 996-1001. 10.1080/13803391003662702.
McCabe DP, Roediger HL, McDaniel MA, Balota DA, Hambrick DZ: The relationship between working memory capacity and executive functioning: evidence for a common executive attention construct. Neuropsychology. 2010, 14: 222-243.
Verbeken S, Braet C, Goossens L, van der Oord S: Executive function training with game elements for obese children: a novel treatment to enhance self-regulatory abilities for weight-control. Behav Res Ther. 2013, 51: 290-299. 10.1016/j.brat.2013.02.006.
Reinert KRS, Po'e EK, Barkin SL: The relationship between executive function and obesity in children and adolescents: a systematic literature review. J Obes. 2013, 820956
Guxens MM, Julvez J, Plana E, Forns J, Basagana X, Torrent M, Sunyer J: Cognitive function and overweight in preschool children. Am J Epidemiol. 2009, 170: 438-446. 10.1093/aje/kwp140.
Smith E, Hay P, Campbell L, Trollor J: A review of the relationship between obesity and cognition across the lifespan: implications for novel approaches to prevention and treatment. Obes Rev. 2011, 12: 740-755.
Mobbs O, Crepin C, Thiery C, Golay A, Van der Linden M: Obesity and the four facets of impulsivity. Patient Educ Couns. 2010, 79: 372-377. 10.1016/j.pec.2010.03.003.
Wilbertz G, Tebartz van Elst L, Delgado MR, Maier S, Feige B, Philipsen A, Blechert J: Orbitofrontal reward sensitivity and impulsivity in adult attention deficit hyperactivity disorder. Neuroimage. 2012, 60: 353-361. 10.1016/j.neuroimage.2011.12.011.
Danner UN, Ouwehand C, van Haastert NL, Hornsveld H, de Ridder DT: Decision-making impairments in women with binge eating disorder in comparison with obese and normal weight women. Eur Eat Disord Rev. 2012, 20: e56-e62. 10.1002/erv.1098.
Davis C, Levitan RD, Muglia P, Bewell C, Kennedy J: Decision-making deficits and overeating: a risk model for obesity. Obes Res. 2004, 12: 929-935. 10.1038/oby.2004.113.
Brogan A, Hevey D, Pignatti R: Anorexia, bulimia, and obesity: shared decision making deficits on the Iowa Gambling Task (IGT). J Int Neuropsychol Soc. 2010, 16: 711-715. 10.1017/S1355617710000354.
Tchanturia K, Liao P, Uher R, Lawrence N, Treasure J, Campbell IC: An investigation of decision making in anorexia nervosa using the Iowa Gambling Task and skin conductance measurements. J Int Neuropsychol Soc. 2007, 13: 635-641.
Bechara A, Damasio AR, Damasio H, Anderson SW: Insensitivity to future consequences following damage to human prefrontal cortex. Cognition. 1994, 50: 7-15. 10.1016/0010-0277(94)90018-3.
Bechara A, Damasio H: Decision-making and addiction: impaired activation of somatic states in substance dependent individuals when pondering decisions with negative future consequences. Neuropsychologia. 2002, 40: 1675-1689. 10.1016/S0028-3932(02)00015-5.
Fagundo AB, de la Torre R, Jimenez-Murcia S, Aguera Z, Granero R, Tarrega S, Botella C, Banos R, Fernandez-Real JM, Rodriguez R, Forcano L, Fruhbeck J, Gomez-Ambrosi J, Tinahones FJ, Fernandez-Garcia JC, Casanueva FF, Fernandez-Aranda F: Executive functions profile in extreme eating/weight conditions: from anorexia nervosa to obesity. PLoS One. 2012, 7: e43382-10.1371/journal.pone.0043382.
Smith E, Hay P, Raman J: Cognitive remediation therapy adaptation for obesity. Cognitive Remediation Therapy (CRT) for Eating and Weight Disorders. Edited by: Tchanturia K. 2014, London: Routledge
Vocci FJ: Cognitive remediation in the treatment of stimulant abuse disorders: a research agenda. Exp Clin Psychopharmacol. 2008, 16: 484-497.
Houben K, Jansen A: Training inhibitory control: recipe for resisting sweet temptations. Appetite. 2011, 56: 345-349. 10.1016/j.appet.2010.12.017.
Veling H, Aarts H, Stroebe W: Using stop signals to reduce impulsive choices for palatable unhealthy foods. Br J Health Psychol. 2013, 18: 354-368. 10.1111/j.2044-8287.2012.02092.x.
Dingemans AE, Danner UN, Donker JM, Aardoom JJ, van Meer FT, Obias K, van Elburg AA, van Furth EF: The effectiveness of cognitive remediation therapy in patients with a severe or enduring eating disorder: a randomized controlled trial. Psychother Psychosom. 2014, 83: 29-36. 10.1159/000355240.
Tchanturia K, Lloyd S, Lang K: Cognitive remediation therapy for anorexia nervosa: current evidence and future research directions. Int J Eat Disord. 2013, 46: 492-495. 10.1002/eat.22106.
Sealed envelope web site. [http://sealedenvelope.com]
Grant DA: Perceptual versus analytical responses to the number concept of a Weigl-type card sorting test. J Exp Psychol. 1951, 41: 23-29.
Harris ME: Wisconsin Card Sorting Test: Computer version, research edition. 1990, Odessa, FL: Psychological Assessment Resources
Heaton RK: A Manual for the Wisconsin Card Sorting Test. 1981, Odessa, FL: Psychological Assessment Resources
Lezak M, Howieson M, Loring D: Neuropsychological Assessment. 2004, New York: Oxford University Press, 4
Wechsler DA: Digit Span Subtest: Wechsler Adult Intelligence Scale. 1997, San Antonio, TX: The Psychological Corporation, 3
Kaufman A, Lichtenberger E: Assessing Adolescent and Adult Intelligence. 2006, Hoboken, NJ: Wiley, 3-3
Battery AIT: The Trail Making Task: Manual of Directions and Scoring. 1944, Washington, DC: War Department, Adjutant General’s Office
Keri S, Moustafa AA, Myers CE, Benedek G, Gluck MA: Alpha-synuclein locus duplication impairs reward-learning. Proc Natl Acad Sci. 2010, 107: 15992-15994. 10.1073/pnas.1006068107.
Roth RM, Isquith PK, Gioia GA: BRIEF-A: Behavior Rating Inventory of Executive Function – Adult Version. 2005, Lutz, FL: Psychological Assessment Resources
Rey A: L’examen psychologique dans les cas d’encephalopathie traumatique. (Les problems.). Arch Psychol. 1941, 28: 215-285.
Osterrieth PA: The test of copying a complex figure: a contribution to the study of perception and memory. Arch Psychol. 1944, 30: 286-356.
Nelson HE: The National Adult Reading Test (NART): Test Manual. 1982, London: NFER-Nelson
NART for Australians. [http://www.cogsci.mq.edu.au/research/resources/nart/]
Bingham SA: Dietary assessments in the European prospective study of diet and cancer (EPIC). Eur J Cancer Prev. 1997, 6: 118-124.
Dobson AB, Lee W, Byles C, Bryson J, Mishra L, Warner-Smith G, Young P, Schofield A: Australian Longitudinal Study on Women's Health: Younger cohort, Wave 3. 2003, [http://www.ada.edu.au/longitudinal/browse/australian-longitudinal-study-on-womens-health], : Food Frequency Questionnaire
McLennan W, Podger A: National Nutrition Survey Users’ Guide. 1998, Canberra: Australian Bureau of Statistics & Department of Health and Family Services
Raman J, Smith E, Hay P: The Clinical Obesity Maintenance Model: an integration of psychological constructs including mood, emotional regulation, disordered overeating, habitual cluster behaviours, health literacy and cognitive function. J Obes. 2013, 240128
Henry JD, Crawford JR: The 21-item version of the Depression Anxiety Stress Scales (DASS–21): normative data and psychometric evaluation in a large non-clinical sample. Br J Clin Psychol. 2005, 44: 227-239. 10.1348/014466505X29657.
Luppino LM, de Wit PF, Bouvy T, Stijnen P, Cuijpers BH, Penninx F, Zitman F: Overweight, obesity and depression: a systematic meta-analysis of longitudinal studies. Arch Gen Psychiatry. 2010, 67: 220-229. 10.1001/archgenpsychiatry.2010.2.
Renn BN, Feliciano L, Segal DL: The bidirectional relationship of depression and diabetes: a systematic review. Clin Psychol Rev. 2011, 31: 1239-1246. 10.1016/j.cpr.2011.08.001.
Davis RN, Nolen-Hoeksema S: Cognitive inflexibility among ruminators and nonruminators. Cognit Ther Res. 2000, 24: 699-711. 10.1023/A:1005591412406.
Watkins E, Teasdale JD: Rumination and overgeneral memory in depression: effects of self-focus and analytic thinking. J Abnorm Psychol. 2001, 110: 353-357.
Disner SJ, Beevers CG, Haigh EA, Beck AT: Neural mechanisms of the cognitive model of depression. Nat Rev Neurosci. 2011, 12: 467-477. 10.1038/nrn3027.
Marazziti D, Consoli G, Picchetti M, Carlini M, Faravelli L: Cognitive impairment in major depression. Eur J Pharmacol. 2010, 626: 83-86. 10.1016/j.ejphar.2009.08.046.
Ukjermann J, Channon S, Lehmkamper C, Abdel-Hamid M, Vollmoeller W, Daum I: Executive function, mentalizing and humor in major depression. J Int Neuropsychol Soc. 2008, 14: 55-62.
Péron J, El Tamer S, Grandjean D, Leray E, Travers D, Drapier D, Vérin M, Millet B: Major depressive disorder skews the recognition of emotional prosody. Prog Neuropsychopharmacol Biol Psychiatry. 2011, 35: 987-996. 10.1016/j.pnpbp.2011.01.019.
Antony MM, Bieling PJ, Cox BJ, Enns MW, Swinson RP: Psychometric properties of the 42-item and 21-item versions of the Depression Anxiety Stress Scales (DASS) in clinical groups and a community sample. Psychol Assess. 1998, 10: 176-181.
Texeira PJ, Going SB, Houtkooper LB, Cussler EC, Metcalfe LL, Blew RM, Sardinha LM, Lohman TG: Pretreatment predictors of attrition and successful weight management in women. Int J Obes Relat Metab Disord. 2004, 28: 1124-1133. 10.1038/sj.ijo.0802727.
Fairburn CG: Cognitive Behavior Therapy and Eating Disorders. 2008, New York: Guilford Press
Mond JM, Hay PJ, Rodgers B, Owen C, Beumont PJV: Validity of the Eating Disorder Examination Questionnaire (EDE-Q) in screening for eating disorders in community samples. Behav Res Ther. 2004, 42: 551-567. 10.1016/S0005-7967(03)00161-X.
Lane B, Szabó M: Uncontrolled, repetitive eating of small amounts of food or ‘grazing’: development and evaluation of a new measure of atypical eating. Behav Change. 2013, 30: 57-73. 10.1017/bec.2013.6.
Verplanken B, Orbell S: Reflections on past behavior: a self-report index of habit strength. Appl Soc Psychol. 2003, 33: 1313-1330. 10.1111/j.1559-1816.2003.tb01951.x.
Cohen DA, Babey SH: Contextual influences on eating behaviours: heuristic processing and dietary choices. Obes Rev. 2012, 13: 766-779. 10.1111/j.1467-789X.2012.01001.x.
Cohen DA, Farley TA: Eating as an automatic behavior. Prev Chronic Dis. 2008, 5: A23
Milosavljevic M, Koch C, Rangel A: Consumers can make decisions in as little as a third of a second. Judgm Decis Mak. 2011, 6: 520-530.
Gardner B, Abraham C, Lally P, de Bruijn GJ: Towards parsimony in habit measurement: testing the convergent and predictive validity of an automaticity subscale of the Self-Report Habit Index. Int J Behav Nutr Phys Act. 2012, 9: 102-10.1186/1479-5868-9-102.
Gratz KL, Roemer L: Multidimensional assessment of emotion regulation and dysregulation: development, factor structure, and initial validation of the Difficulties in Emotion Regulation Scale. J Psychopathol Behav Assess. 2004, 36: 41-54.
Bargh JA, Williams LE: The case for nonconscious emotion regulation. Handbook of Emotion Regulation. Edited by: Gross JJ. 2007, New York: Guilford Press, 429-445.
Gross JJ, Thompson RA: Emotion regulation: conceptual foundations. Handbook of Emotion Regulation. Edited by: Gross JJ. 2007, New York: Guilford, 3-24.
Claes L, Nederkoorn C, Vandereycken W, Guerrieri R, Vertommen H: Impulsiveness and lack of inhibitory control in eating disorders. Eat Behav. 2006, 7: 196-203. 10.1016/j.eatbeh.2006.05.001.
Bardeen JR, Fergus TA, Orcutt HK: An examination of the latent structure of the Difficulties in Emotion Regulation Scale. J Psychopathol Behav Assess. 2012, 34: 382-392. 10.1007/s10862-012-9280-y.
Fox HC, Axelrod SR, Paliwal P, Sleeper J, Sinha R: Difficulties in emotion regulation and impulse control during cocaine abstinence. Drug Alcohol Depend. 2007, 89: 298-301. 10.1016/j.drugalcdep.2006.12.026.
Johnson KA, Zvolensky MJ, Marshall EC, Gonzalez A, Abrams K, Vujanovic AA: Linkages between cigarette smoking outcome expectancies and negative emotional vulnerability. Addict Behav. 2008, 33: 1416-1424. 10.1016/j.addbeh.2008.05.001.
Ware JE, Kosinski M, Keller SD: A 12 Item Short Form health survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996, 34: 220S-233S. 10.1097/00005650-199603000-00003.
Lindvall C, Lask B: Implications for treatment. Eating Disorders and the Brain. Edited by: Lask B, Frampton I. 2011, Oxford, UK: T Wiley/Blackwell, 191-206.
Owen I, Lindvall Dahlgren C, Lask B: Cognitive Remediation Therapy. Eating Disorders in Childhood and Adolescence. Edited by: Lask B, Bryant-Waugh R. 2013, New York: Routledge, 301-308.
Tchanturia K, Campbell C, Morris R, Treasure J: Neuropsychological studies in anorexia nervosa. Int J Eat Disord. 2005, 37 (Suppl): S72-S76.
Rosnow RL, Rosenthal R: If you’re looking at the cell means, you’re not looking at only the interaction (unless all main effects are zero). Psychol Bull. 1991, 110: 574-576.
Rosnow RL, Rosenthal R: Statistical procedures and the justification of knowledge in psychological science. Am Psychol. 1989, 44: 1276-1284.
Clark DM, Ehlers A, Hackmann A, McManus F, Fennell M, Grey N, Waddington L, Wild J: Cognitive therapy versus exposure and applied relaxation in social phobia: a randomized controlled trial. J Consult Clin Psych. 2006, 74: 568-578.
Hedeker D, Gibbons R: Longitudinal Data Analysis. 2006, Hoboken, NJ: J Wiley & Sons
Zeger SL, Liang KY: Longitudinal data analysis for discrete and continuous outcomes. Biometrics. 1986, 42: 121-130. 10.2307/2531248.
Stern JS, Hirsch J, Blair SN, Foreyt JP, Frank A, Kumanyika SK, Madans JH, Marlatt GA, St Jeor ST, Stunkard AJ: Weighing the options: criteria for evaluating weight-management programs. Obes Res. 1995, 3: 591-604.
Acknowledgements
JR is a doctoral thesis candidate supported by a fellowship from the NSW Institute of Psychiatry, Australia. This trial and employment of the research assistant Melissa Rouel is supported by a Diabetes Australia Research Trust Grant.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
JR, ES and PH designed the RCT. JR and ES are trained in BWLT and CRT-O. JR will deliver the therapies supervised by ES. PH and ES supervise JR in her doctoral thesis. JR and a research assistant are collecting data. All data will be entered, cleaned and coded by the research assistant, JR and PH. The data will be analysed by JR under the supervision of PH and ES and in consultation with a statistician at the Centre for Health Research at the University of Western Sydney. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Raman, J., Hay, P. & Smith, E. Manualised Cognitive Remediation Therapy for adult obesity: study protocol for a randomised controlled trial. Trials 15, 426 (2014). https://doi.org/10.1186/1745-6215-15-426
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1745-6215-15-426