Abstract
Background
The different effects of LDL-C levels and statins therapy on coronary atherosclerotic plaque between Western and Asian remain to be settled.
Methods
PubMed, EMBASE, and Cochrane databases were searched from Jan. 2000 to Sep. 2014 for randomized controlled or blinded end-points trials assessing the effects of LDL-C lowering therapy on regression of coronary atherosclerotic plaque (CAP) in patients with coronary heart disease by intravascular ultrasound. The significance of plaques regression was assessed by computing standardized mean difference (SMD) of the volume of CAP between the baseline and follow-up.
Results
Twenty trials (ten in the West and ten in Asia) were identified. For Westerns, Mean lowering LDL-C by 49.4% and/or to level 61.9 mg/dL in the group of patients with baseline mean LDL-C 123.2 mg/dL could significantly reduce the volume of CAP at follow up (SMD −0.156 mm3, 95% CI −0.248 ~ −0.064, p = 0.001). LDL-C lowering by rosuvastatin (mean 40 mg daily) could significantly decrease the volumes of CAP at follow up. For Asians, Mean lowering LDL-C by 36.1% and/or to level 84.0 mg/dL with baseline mean LDL-C 134.2 mg/dL could significantly reduce the volume of CAP at follow up (SMD −0.211 mm3, 95% CI −0.331 ~ −0.092, p = 0.001). LDL-C lowering by rosuvastatin (mean 14.1 mg daily) and atorvastatin (mean 18.9 mg daily) could significantly decrease the volumes of CAP at follow up.
Conclusions
There was a different effect of LDL-C lowering on CAP between Westerns and Asians. For regressing CAP, Asians need lower dosage of statins or lower intensity LDL-C lowering therapy than Westerns.
Similar content being viewed by others
Background
Atherosclerotic plaque is the hallmark and cornerstone of atherosclerotic disease. Disruption of coronary atherosclerotic plaque (CAP) may lead to sudden cardiac death, acute myocardial infarction, or unstable angina [1]. Intravascular ultrasound (IVUS) is considered to be gold standard for measurement of atherosclerotic plaque [2].
The meta-analysis of twenty trials evaluated the effects of LDL-C lowering on CAP indicated that intensive LDL-C lowering with statins could slow atherosclerotic plaque progression and lead to plaque regression [3]. But the meta-analysis did not investigate the effects of LDL-C lowering on CAP in different race.
In this meta-analysis, we investigated the difference between Western and Asian in the effect of LDL-C lowering therapy on the progression of the CAP from the current trials on LDL-C lowering therapy retarding the progression of the CAP and identified the different targets of LDL-C that result in the regression of the CAP for Western and Asian.
Methods
Materials and methods of this meta-analysis were detailed in the paper by Gao et al. [3].
Search strategy and selection criteria
An electronic literature search was performed to identify all relevant studies published in PubMed, EMBASE, and Cochrane databases in the English language from Jan. 1, 2000 to Sep. 13, 2014, using the terms “atherosclerosis” and “cholesterol blood level”. Trials were included using the criteria as: 1) randomized controlled or prospective, blinded end-points trials, and its primary end point was CAP change detected by IVUS; 2) report of LDL-C levels at baseline and follow-up; 3) data on the volume of CAP at baseline and follow-up, and volume of CAP was calculated as vessel volume minus lumen volume; Exclusion criteria were: 1) only CAP area or volume index or percent atheroma volume were detected; 2) the levels of LDL-C at baseline or follow-up were not provided; and 3) target plaques were unstable.
Data extraction and quality assessment
Two investigators independently reviewed all potentially eligible studies and collected data on patient and study characteristics, and any disagreement was resolved by consensus. The primary end point of this study was the volume change of CAP detected by IVUS. Quality assessments of trials were evaluated with Jadad quality scale.
Data synthesis and analysis
Volume changes of CAP from baseline to follow-up were analyzed using standardized mean differences (SMD).
Volume changes of plaque in every arm were used for pooled analysis. The trials were firstly grouped into group Western and Asian according to the location of the trials. Then, according to the levels and the reducing percentage of LDL-C at follow-up, the arms were grouped to following groups: ≤70, >70 ≤ 100 HP, >70 ≤ 100 MP, >70 ≤ 100 LP, >100 mg/dL; and <0, ≥0 < 30, ≥30 < 40, ≥40 < 50, ≥50% respectively [3], to investigate the effect of different levels of LDL-C at follow up on CAPs. According to statins, the arms were grouped to: rosuvastatin, atorvastatin, pitavastatin, simvastatin, fluvastatin and pravastatin groups, to investigate the effect of different statins on CAPs. The volume of CAP at follow up was compared with that at baseline to evaluate effect of LDL-C levels on regression of CAP.
Heterogeneity across trials (arms) was assessed via a standard χ2 test with significance being set at p < 0.10 and also assessed by means of I2 statistic with significance being set at I2 > 50%. Pooled analyses were calculated using fixed-effect models, whereas random-effect models were applied in case of significant heterogeneity across trials (arms). Sensitivity analyses (exclusion of one study at one time) were performed to determine the stability of the results. Publication bias was assessed using the Egger regression asymmetry test. Statistical analyses were performed using STATA software 12.0 (StataCorp, College Station, Texas).
All continuous variables were expressed as mean ± SD, and continuous variables were compared between the Western and Asian groups using Student’s t test (SigmaStat 3.5). A P value <0.05 was considered to be statistically significant.
Results
Eligible studies
The flow of selecting studies for the meta-analysis was shown in Figure 1. Briefly, of the initial 673 articles, one hundred and twenty-two of abstracts were reviewed, resulting in exclusion of 102 articles, and 20 articles were reviewed in full text, resulting in exclusion of 10 trials and inclusion of 18 additional trials cited in the 20 articles. Twenty two RCTs [4–25] and six blinded end-points trial [26–31] were carefully evaluated, and eight trials [4, 8, 9, 18, 19, 21, 27, 31] were excluded because of specific the index of plaque or lack of some data. Sixteen RCT (ESTABLISH [11], REVERSAL [10], A-PLUS [5], ACTIVATE [6], ILLUSTRATE [7], JAPAN-ACS [20], REACH [14], SATURN [16], ARTMAP [17], ERASE [23], STRADIVARIUS [24], PERISCOPE [25], and trials by Yokoyama M [12], by Kawasaki M [13], by Hong MK [15], and Tani S [22]) and four blinded end-points trial (ASTEROID [26], COSMOS [29], trial by Jensen LO [28] and trial by Nasu K [30]) were finally analyzed.
The characteristics of the included trials were as same as in the study [3] and shown in Table 1. Briefly, among the 20 trials, 10 trials are completed in European, America and Australia [10, 5–7, 16, 23–26, 28], 10 in Asia [20, 11–15, 17, 22, 29, 30], and there were 15 trials assessing statins (statin vs. usual care in 6 trials [11–14, 22, 30]; intensive statin vs. moderate statin treatment in 5 trials [10, 15–17, 20]; follow up vs baseline in 3 trial [26, 28, 29], before acute coronary syndrome (ACS) vs after ACS in one trial [23]), 2 trials assessing enzyme acyl–coenzyme A: cholesterol acyltransferase (ACAT) inhibition [5, 6], one trial assessing cholesteryl ester transfer protein (CETP) inhibitor torcetrapib [7], one trial assessing a decreasing obesity drug: rimonabant [24], and one trial assessing glucose-lowering agents [25]. Overall, 5910 patients with coronary heart disease (CHD) underwent serial IVUS examination for evaluating regression of CAP. Follow-up periods ranged from 2 to 24 months. The levels of LDL-C of each arm at baseline and follow-up were shown in Table 2.Risk of bias of included studies, evaluated through Cochrane’s methods, showed an overall acceptable quality of selected trials (Figures 2 and 3).
The effect of the levels of LDL-C at follow-up on regression of coronary atherosclerotic plaque in Western and Asian
For Western, meta-analysis indicated that LDL-C lowering in group ≤70 mg/dL could lead to regression of CAP, but LDL-C lowering in group >70 ≤ 100 HP, >70 ≤ 100 MP, >70 ≤ 100 LP and >100 mg/dL could not (Figure 4, Table 3).
Meta- analysis of the effects of reduction levels of LDL-C at follow up on the regression of coronary atherosclerotic plaque in Western. Abbreviations: Ato, Atorvastatin; Ros, Rosuvastatin; Pra, Pravastatin; Pit, Pitavastatin; Sim, Simvastatin; Flu, Fluvastatin; Con, Control; Pac, Pactimibe; Tor, Torcetrapib, Ava 50, 250, 750, Avasimibe 50, 250, 750 mg; Bef, before ACS; Aft, after ACS; Gli, Glimepiride; Pio, Pioglitazone; Rim, Rimonabant.
In group ≤70 mg/dL (including three arms) with mean 23.1 months of follow up, the volumes of CAP (160.6 mm3) at follow up were significantly decreased, compared with the volumes (171.4 mm3) at baseline [SMD −0.156 mm3, 95% CI (confidence interval) -0.248 ~ −0.064, p = 0.001]. There was no significant heterogeneity among arms (χ2 for heterogeneity = 0.33, p =0.886, I2 = 0%).
Sensitivity analyses suggested that LDL-C lowering in group ≤70 mg/dL could lead to regression of CAP with reduction of the CAP volume ranged from −0.139 mm3 (SMD, 95% CI: −0.257 ~ −0.021) when the arm of 2006 ASTEROID Ros was omitted to −0.175 mm3 (SMD, 95% CI: −0.317 ~ −0.034) when the arm of 2011 SATURN Ros was omitted. No publication bias was found, the values of p by Egger’s test was 0.789.
For Asian, according to the levels of LDL-C at follow-up, the arms were grouped to three groups: ≤70, >70 ≤ 100 HP and >100 mg/dL.
LDL-C lowering in group ≤70 mg/dL and >70 ≤ 100 HP could lead to regression of CAP, but LDL-C lowering in group >100 mg/dL could not (Figure 5, Table 3).
Meta- analysis of the effects of reduction levels of LDL-C at follow up on the regression of coronary atherosclerotic plaque in Asian. Abbreviation as in Figure 4.
In group ≤70 mg/dL (including four arms) with mean 6.9 months of follow up and group >70 ≤ 100HP mg/dL (including eight arms) with mean 11.0 months of follow up, the volumes of CAP (179.9, 87.5 mm3 respectively) at follow up were significantly decreased, compared with the volumes (192.2, 96.4 mm3 respectively) at baseline [SMD −0.157 mm3, 95% CI −0.307 ~ −0.008, p = 0.039; SMD −0.211 mm3, 95% CI −0.331 ~ −0.092, p = 0.001; respectively]. There was no significant heterogeneity among arms (χ2 for heterogeneity = 0.24, p =0.955, I2 = 0% for group ≤70 mg/dL; χ2 for heterogeneity = 2.68, p =0.913, I2 = 0% for group >70 ≤ 100HP mg/dL).
Sensitivity analyses suggested that LDL-C lowering in group >70 ≤ 100 HP mg/dL could lead to regression of CAP with reduction of the CAP volume ranged from −0.177 mm3 (SMD, 95% CI: −0.314 ~ −0.040) when the arm of 2009 JAPAN-ACS Ato was omitted to −0.231 mm3 (SMD, 95% CI: −0.368 ~ −0.094) when the arm of 2009 COSMOS Ros was omitted; but that LDL-C lowering in group ≤ 70 mg/dL could not significantly lead to regression of CAP with reduction of the CAP volume when the arm of 2012 ARTMAP Ros or 2012 ARTMAP Ato was omitted (Table 3).
No publication bias was found, the values of p by Egger’s test for group ≤70 and >70 ≤ 100HP mg/dL were 0.970, 0.083 respectively.
The effect of the LDL-C reducing percentage at follow-up on regression of CAP in Western and Asian
For Western, meta-analysis showed that LDL-C lowering in group ≥40 < 50, ≥50% could lead to regression of CAP, but LDL-C lowering in group <0, ≥0 < 30% and ≥30 < 40 could not (Figure 6, Table 3).
Meta- analysis of the effects of reduction percentages of LDL-C at follow up on the regression of coronary atherosclerotic plaque in Western. Abbreviation as in Figure 4.
In group ≥40 < 50% (including four arms) with mean 22.6 months of follow up, the volumes of CAP (143.1 mm3) at follow up were significantly decreased, compared with the volumes (148.8 mm3) at baseline (SMD −0.095 mm3, 95% CI −0.171 ~ −0.019, p = 0.014). There was no significant heterogeneity among arms (χ2 for heterogeneity = 1.64, P = 0.651, I2 = 0%).
Sensitivity analyses showed that LDL-C lowering in group ≥40 < 50 could still lead to regression of CAP with reduction of the plaque volume ranged from −0.065 mm3 (95% CI −0.163 ~ 0.032) when the arm of 2011 SATURN Ros was omitted to −0.116 mm3 (SMD, 95% CI −0.201 ~ −0.032) when 2004 REVERSAL Ato was omitted. Publication bias analysis suggested the values of p by Egger’s test were 0.804.
In group group <0, ≥0 < 30% and ≥30 < 40, meta-analysis were showed in Table 3.
For Asian, according to the reducing percentage of LDL-C at follow-up, the arms were grouped to following groups: ≥0 < 30, ≥30 < 40, ≥40 < 50.
LDL-C lowering in group ≥30 < 40, ≥40 < 50% could lead to regression of CAP, but LDL-C lowering in group ≥0 < 30% could not (Figure 7, Table 3).
Meta- analysis of the effects of reduction percentages of LDL-C at follow up on the regression of coronary atherosclerotic plaque in Asian. Abbreviation as in Figure 4.
In group ≥30 < 40% (including nine arms) with mean 10.9 months of follow up, and group ≥40 < 50% (including four arms) with mean 6.9 months of follow up, the volumes of CAP (90.0, 179.9 mm3 respectively) at follow up were significantly decreased, compared with the volumes (98.6, 192.2 mm3 respectively) at baseline (SMD −0.206 mm3, 95% CI −0.324 ~ −0.088, p = 0.001; SMD −0.157 mm3, 95% CI −0.307 ~ −0.008, p = 0.039; respectively). There was no significant heterogeneity among arms (χ2 for heterogeneity = 2.91, P = 0.840, I2 = 0%; χ2 for heterogeneity = 0.33, p =0.955, I2 = 0%; for group ≥30 < 40, and group ≥40 < 50 respectively).
Sensitivity analyses showed that LDL-C lowering in group ≥30 < 40% could still lead to regression of CAP with reduction of the plaque volume ranged from −0.172 mm3 (95% CI −0.306 ~ −0.038) when the arm of 2009 JAPAN-ACS Ato was omitted to −0.223 mm3 (SMD, 95% CI −0.357 ~ −0.089) when 2009 COSMOS Ros was omitted. Publication bias analysis suggested that bias was significant with 0.004 of p value by Egger’s test.
Mean levels of LDL-C at baseline and follow up, mean reducing percentage of LDL-C in each group were showed in Table 4.
The effect of lowering LDL-C by statins on regression of coronary atherosclerotic plaque in Western and Asian
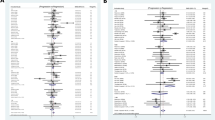
For Western, atorvastatin, rosuvastatin, pravastatin and simvastatin were used in trials to investigate the effects of LDL-C lowering on CAP. Meta-analysis indicated that LDL-C lowering by rosuvastatin could lead to regression of CAP, but LDL-C lowering by atorvastatin, pravastatin, and simvastatin could not (Figure 8, Table 5).
Meta- analysis of the effects of LDL-C lowering by different statins on the regression of coronary atherosclerotic plaque in Western. Abbreviation as in Figure 4.
LDL-C lowering by rosuvastatin (mean 40.0 mg daily for mean 24 months) could significantly decrease the volumes of CAP at follow up, compared with the volumes at baseline (SMD −0.158 mm3, 95% CI: −0.253 ~ −0.064, p = 0.001). There was no significant heterogeneity among arms (χ2 for heterogeneity = 0.18, p =0.672, I2 = 0%).
Sensitivity analyses suggested that lowering LDL-C by rosuvastatin could lead to regression of CAP with reduction of the plaque volume ranged from −0.142 mm3 (SMD, 95% CI: −0.263 ~ −0.020) when the arm of 2006 ASTEROID Ros was omitted to −0.183 mm3 (SMD, 95% CI: −0.332 ~ −0.035) when the arm of 2011 SATURN Ros was omitted. But publication bias was found, the values of p by Egger’s test was 0.000 (Table 5).
For Asian, atorvastatin, rosuvastatin, pitavastatin, pravastatin, fluvastatin and simvastatin were used in trials to investigate the effects of LDL-C lowering on CAP. Meta-analysis indicated that LDL-C lowering by rosuvastatin, atorvastatin could lead to regression of CAP, but LDL-C lowering by pitavastatin, pravastatin, fluvastatin and simvastatin could not (Figure 9, Table 5).
Meta- analysis of the effects of LDL-C lowering by different statins on the regression of coronary atherosclerotic plaque in Asian. Abbreviation as in Figure 4.
LDL-C lowering by rosuvastatin (mean 14.1 mg daily for mean 10.3 months), atorvastatin (mean 18.9 mg daily for mean 7.8 months) could significantly decrease the volumes of CAP at follow up, compared with the volumes at baseline (SMD −0.172 mm3, 95% CI: −0.331 ~ −0.012, p = 0.035; SMD −0.185, 95% CI: −0.330 ~ −0.040, p = 0.013; respectively). There was no significant heterogeneity among arms (χ2 for heterogeneity = 0.17, p =0.917, I2 = 0% for rosuvastatin; χ2 for heterogeneity = 1.94, p =0.858, I2 = 0% for atorvastatin).
Sensitivity analyses suggested that lowering LDL-C by rosuvastatin could not significantly lead to regression of CAP when the arm of 2012 ARTMAP Ros or 2009 COSMOS Ros was omitted. Also, Lowering LDL-C by atorvastatin could not significantly lead to regression of CAP when the arm of 2009 JAPAN-ACS Ato was omitted. No publication bias was found, the values of p by Egger’s test for rosuvastatin and atorvastatin group were 0.660, 0.456 respectively (Table 5).
Intensity of lowering LDL-C by different statins was shown in Table 6. Rosuvastatin and atorvastatin could reduce LDL-C by more than 40%.
The difference between Western and Asian in usage of statins
The meta analysis showed that rosuvastatin and atorvastatin can regress CAP (Table 5). LDL-C levels, intensity of lowering LDL-C by rosuvastatin and atorvastatin, its dosage and duration were compared between Western and Asian (Table 7). Intensity of lowering LDL-C by rosuvastatin and atorvastatin in Western group were similar to that in Asian group, but the dosages of rosuvastatin and atorvastatin in Asian group were significantly lower than those in Western group, and the duration of statins administration in Asian group were significantly shorter than those in Western, as showed in Table 7.
Discussion
This meta-analysis revealed that intensive LDL-C lowering can regress CAP both in Western and Asian. For regressing CAP, the dosage of statins administrated in Westerns was different from that in Asians. Asians need lower dosage of atorvastatin or rosuvastatin than Westerns though there was no difference between Westerns and Asians in pharmacokinetic and pharmacodynamic study [32, 33].
The effect difference of LDL-C lowering on CAP between Western and Asian
For Western including American, Canadian, German, French, English, Australian and Dane [10, 5–7, 16, 23–26, 28], the meta-analysis (Table 3) in subgroup ≤70 mg and ≥40 < 50% of Western indicated that LDL-C level lowering to <69.3 mg or reducing by > 45% for 22.6 months of follow up (Table 4) could lead to regression of CAP, but the meta-analysis (Table 3) in subgroup >70 ≤ 100 HP mg of Western showed that LDL-C level lowering to 73.2 mg or reducing by 43.6% for 21.7 months of follow up (Table 4) was not enough for regressing CAP.
For Asian including Japanese and Korean [20, 11–15, 17, 22, 29, 30], the meta-analysis in subgroup ≤70 mg and ≥40 < 50% of Asian indicated that LDL-C level lowering to 57.0 mg or reducing by 47.2% for 6.9 months of follow up could lead to regression of CAP, but sensitivity analyses showed that LDL-C lowering in this two subgroup could not significantly lead to regression of CAP when the arm of 2012 ARTMAP Ros or 2012 ARTMAP Ato was omitted (Table 3). The meta-analysis in subgroup ≥ 30 < 40% of Asian indicated that LDL-C level lowering to 84.6 mg or reducing by 36.0% for 10.9 months of follow up could also lead to regression of CAP, but publication bias was significant. The meta-analysis in subgroup >70 ≤ 100HP mg of Asian with good sensitivity and no publication bias indicated that LDL-C level lowering to 84.0 mg or reducing by 36.1% for 11 months of follow up with could lead to regression of CAP (Table 3).
Taken all the results of meta-analysis together, for Western, it was recommended that LDL-C level might be reduced by >45% or to a target level < 69 mg/dL for regressing CAP; for Asian, LDL-C level might be reduced by >36% or to a target level < 84 mg/dL.
Different effects of statins on Westerns and Asians
Whether statins has different effect on Westerns and Asians remains to be settled.
The study by Lee E et al. [34] and MEGA Study [35] suggested statins have different effects on Westerns and Asians. In 2005, Lee E et al. [34] prospectively examined the pharmacokinetics of rosuvastatin in White and Asian individuals living in Singapore, and reported that plasma exposure to rosuvastatin and its metabolites was significantly higher in Chinese, Malay, and Asian-Indian subjects compared with Western subjects living in the same environment. But the mechanisms underlying ethnic differences in rosuvastatin disposition remain to be unearthed [36]. MEGA Study [35] indicated that a small dose of pravastatin that was half the dose administered to western patients, reduced LDL-C by 19-22% (which is lower than that reductions of 23–35% in western patients), but could substantially reduce the risk of coronary heart disease in Japanese.
But two meta-analysis did not demonstrate the difference of rosuvastatin and atorvastatin on Westerns and Asians. The meta-analysis including the 36 trials of pharmacodynamics of rosuvastatin in Western and Asian hypercholesterolemia patients did not confirm that there was significant difference in the exposure-response relationship for LDL-C reduction between Westerners and Asians [33].The meta-analysis including 22 pharmacokinetic studies also demonstrated no differences in the systemic exposure to atorvastatin between Asian and Caucasian subjects [32].
Our meta-analysis revealed that there were difference of rosuvastatin and atorvastatin in lowering LDL-C and regressing CAP between Westerns and Asians. The meta-analysis of rosuvastatin including 2 trials with 869 Western patients indicated that 40 mg of rosuvastatin daily for 24 months with reducing LDL-C by 49.9% could regress CAP. But the meta-analysis of rosuvastatin including 3 trials with 304 Asian patients showed that 14.1 mg of rosuvastatin daily for 10.3 months with reducing LDL-C by 44.0% could also regress CAP though the result of sensitivity analyses is not as good as that in Western (Table 5). The meta-analysis of atorvastatin including 2 trials with 772 Western patients showed that 80 mg of atorvastatin daily for 22 months with reducing LDL-C by 43.0% could not significantly regress CAP. But the meta-analysis of atorvastatin including 6 trials with 366 Asian patients demonstrated that 18.9 mg of atorvastatin daily for 7.8 months with reducing LDL-C by 40.7% could significantly regress CAP though the result of sensitivity analyses is not as good as that expected (Table 5).
Comparison between Western and Asian in using rosuvastatin and atorvastatin indicated that the dosages of rosuvastatin and atorvastatin in Asian group were significantly lower than those in Western (Table 7).
Based on this meta-analysis, reducing LDL-C by >40% in Westerns need atorvastatin 80 mg or rosuvastatin 40 mg, but in Asians need only atorvastatin 18.9 mg or rosuvastatin 14.1 mg. For regressing CAP, 40 mg of rosuvastatin might be daily administrated in Western for 24 months; 14.1 mg of rosuvastatin or 18.9 mg of atorvastatin might be daily administrated in Asian for 10.7 or 7.8 months respectively.
Study limitation
As with the meta-analysis [3], this study has some limitations. There might be publication bias, difference of the method detected and follow up duration. But those differences in measurements and plaque selection did not affect the change of the target plaque with LDL-C levels. So, it has little effect on homogeneous of studies, and on the relationship between CAP change and LDL-C level. But the trials of single statin on LDL-C and CAP of specific population (for example, 2 trials about atorvastatin on Western with 727 participants or 6 on Asian with 366 in Table 5) were limited, the effect of statin on specific population remains to be investigated. The duration of follow up between Western and Asian was different (Table 4, 6 and 7), and treatment duration might have some effect on CAP regression. But the trials from Asian and Western were respectively meta-analysed in this study. Therefore, the difference in follow-up duration between Asian and Western did not influence the results of the meta-analysis. The CAP regression in short period of statins therapy in Asian suggested that the CAPs in Asian were easily regressed by statins.
This meta-analysis did not investigate the effect of reduction of LDL-C on adverse cardiovascular events because all participants of the included trial must be alive at follow up. But in the Extended-ESTABLISH study, the incidence of adverse cardiovascular events in statin group with CAP regression were reduced to half that seen in the control group [37]. In the Extended JAPAN-ACS study [38], there was no significantly different association of incidence of adverse cardiovascular events with the CAP regression extent, but that greater external elastic membrane volume regression (<−6.56%) had a significantly lower incidence of cumulative events than the lesser suggested the importance of CAP regression in reducing adverse cardiovascular events. A meta-analysis [39] included 7864 CAD patients showed that rates of plaque volume regression were significantly associated with the incidence of MI or revascularization.
Conclusions
LDL-C lowering therapy has a different effect on atherosclerotic plaque between Westerns and Asians. This systemic review demonstrated that there is a different effect of LDL-C lowering on CAP between Westerns and Asians. For regressing CAP, Asians need lower dosage of statins or lower intensity LDL-C lowering therapy (by >36%) than Westerns (by 45%).
Abbreviations
- ACAT:
-
Acyl–coenzyme A: cholesterol acyltransferase
- ACS:
-
Acute coronary syndrome
- ATP III:
-
Adult Treatment Panel III
- CAD:
-
Coronary artery disease
- CAG:
-
Coronary angiography
- CAP:
-
Coronary atherosclerotic plaque
- CETP:
-
Cholesteryl ester transfer protein
- CHD:
-
Coronary heart disease
- IVUS:
-
Intravascular ultrasound
- CI:
-
Confidence interval
- LDL-C:
-
Low-density lipoprotein cholesterol
- RCT:
-
Randomized controlled trial
- SMD:
-
Standardized mean differences.
References
Falk E, Shah PK, Fuster V: Coronary plaque disruption.Circulation 1995, 92:657–71. 10.1161/01.CIR.92.3.657
Nissen SE, Yock P: Intravascular ultrasound: novel pathophysiological insights and current clinical applications.Circulation 2001, 103:604–16. 10.1161/01.CIR.103.4.604
Gao WQ, Feng QZ, Li YF, Li YX, Huang Y, Chen YM, et al.: Systematic study of the effects of lowering low-density lipoprotein-cholesterol on regression of coronary atherosclerotic plaques using intravascular ultrasound.BMC Cardiovasc Disord 2014, 14:60. 10.1186/1471-2261-14-60
Schartl M, Bocksch W, Koschyk DH, Voelker W, Karsch KR, Kreuzer J, et al.: Use of intravascular ultrasound to compare effects of different strategies of lipid-lowering therapy on plaque volume and composition in patients with coronary artery disease.Circulation 2001, 104:387–92. 10.1161/hc2901.093188
Tardif JC, Gregoire J, L’Allier PL, Anderson TJ, Bertrand O, Reeves F, et al.: Effects of the acyl coenzyme A:cholesterol acyltransferase inhibitor avasimibe on human atherosclerotic lesions.Circulation 2004, 110:3372–7. 10.1161/01.CIR.0000147777.12010.EF
Nissen SE, Tuzcu EM, Brewer HB, Sipahi I, Nicholls SJ, Ganz P, et al.: Effect of ACAT inhibition on the progression of coronary atherosclerosis.N Engl J Med 2006, 354:1253–63. 10.1056/NEJMoa054699
Nissen SE, Tardif JC, Nicholls SJ, Revkin JH, Shear CL, Duggan WT, et al.: Effect of torcetrapib on the progression of coronary atherosclerosis.N Engl J Med 2007, 356:1304–16. 10.1056/NEJMoa070635
Nozue T, Yamamoto S, Tohyama S, Umezawa S, Kunishima T, Sato A, et al.: Statin treatment for coronary artery plaque composition based on intravascular ultrasound radiofrequency data analysis.Am Heart J 2012, 163:191–9.e1. 10.1016/j.ahj.2011.11.004
Zhang X, Wang H, Liu S, Gong P, Lin J, Lu J, et al.: Intensive-dose atorvastatin regimen halts progression of atherosclerotic plaques in new-onset unstable angina with borderline vulnerable plaque lesions.J Cardiovasc Pharmacol Ther 2013, 18:119–25. 10.1177/1074248412465792
Nissen SE, Tuzcu EM, Schoenhagen P, Brown BG, Ganz P, Vogel RA, et al.: Effect of intensive compared with moderate lipid-lowering therapy on progression of coronary atherosclerosis: a randomized controlled trial.JAMA 2004, 291:1071–80. 10.1001/jama.291.9.1071
Okazaki S, Yokoyama T, Miyauchi K, Shimada K, Kurata T, Sato H, et al.: Early statin treatment in patients with acute coronary syndrome: demonstration of the beneficial effect on atherosclerotic lesions by serial volumetric intravascular ultrasound analysis during half a year after coronary event: the ESTABLISH Study.Circulation 2004, 110:1061–8. 10.1161/01.CIR.0000140261.58966.A4
Yokoyama M, Komiyama N, Courtney BK, Nakayama T, Namikawa S, Kuriyama N, et al.: Plasma low-density lipoprotein reduction and structural effects on coronary atherosclerotic plaques by atorvastatin as clinically assessed with intravascular ultrasound radio-frequency signal analysis: a randomized prospective study.Am Heart J 2005, 150:287.
Kawasaki M, Sano K, Okubo M, Yokoyama H, Ito Y, Murata I, et al.: Volumetric quantitative analysis of tissue characteristics of coronary plaques after statin therapy using three-dimensional integrated backscatter intravascular ultrasound.J Am Coll Cardiol 2005, 45:1946–53. 10.1016/j.jacc.2004.09.081
Yamada T, Azuma A, Sasaki S, Sawada T, Matsubara H: Randomized evaluation of atorvastatin in patients with coronary heart disease: a serial intravascular ultrasound study.Circ J 2007, 71:1845–50. 10.1253/circj.71.1845
Hong MK, Park DW, Lee CW, Lee SW, Kim YH, Kang DH, et al.: Effects of statin treatments on coronary plaques assessed by volumetric virtual histology intravascular ultrasound analysis.JACC Cardiovasc Interv 2009, 2:679–88. 10.1016/j.jcin.2009.03.015
Nicholls SJ, Ballantyne CM, Barter PJ, Chapman MJ, Erbel RM, Libby P, et al.: Effect of two intensive statin regimens on progression of coronary disease.N Engl J Med 2011, 365:2078–87. 10.1056/NEJMoa1110874
Lee CW, Kang SJ, Ahn JM, Song HG, Lee JY, Kim WJ, et al.: Comparison of effects of atorvastatin (20 mg) versus rosuvastatin (10 mg) therapy on mild coronary atherosclerotic plaques (from the ARTMAP trial).Am J Cardiol 2012, 109:1700–4. 10.1016/j.amjcard.2012.01.399
Hong YJ, Jeong MH, Hachinohe D, Ahmed K, Choi YH, Cho SH, et al.: Comparison of effects of rosuvastatin and atorvastatin on plaque regression in Korean patients with untreated intermediate coronary stenosis.Circ J 2011, 75:398–406. 10.1253/circj.CJ-10-0658
Kovarnik T, Mintz GS, Skalicka H, Kral A, Horak J, Skulec R, et al.: Virtual histology evaluation of atherosclerosis regression during atorvastatin and ezetimibe administration: HEAVEN study.Circ J 2012, 76:176–83. 10.1253/circj.CJ-11-0730
Hiro T, Kimura T, Morimoto T, Miyauchi K, Nakagawa Y, Yamagishi M, et al.: Effect of intensive statin therapy on regression of coronary atherosclerosis in patients with acute coronary syndrome: a multicenter randomized trial evaluated by volumetric intravascular ultrasound using pitavastatin versus atorvastatin (JAPAN-ACS [Japan assessment of pitavastatin and atorvastatin in acute coronary syndrome] study).J Am Coll Cardiol 2009, 54:293–302. 10.1016/j.jacc.2009.04.033
Petronio AS, Amoroso G, Limbruno U, Papini B, De Carlo M, Micheli A, et al.: Simvastatin does not inhibit intimal hyperplasia and restenosis but promotes plaque regression in normocholesterolemic patients undergoing coronary stenting: a randomized study with intravascular ultrasound.Am Heart J 2005, 149:520–6. 10.1016/j.ahj.2004.10.032
Tani S, Watanabe I, Anazawa T, Kawamata H, Tachibana E, Furukawa K, et al.: Effect of pravastatin on malondialdehyde-modified low-density lipoprotein levels and coronary plaque regression as determined by three-dimensional intravascular ultrasound.Am J Cardiol 2005, 96:1089–94. 10.1016/j.amjcard.2005.05.069
Rodes-Cabau J, Tardif JC, Cossette M, Bertrand OF, Ibrahim R, Larose E, et al.: Acute effects of statin therapy on coronary atherosclerosis following an acute coronary syndrome.Am J Cardiol 2009, 104:750–7. 10.1016/j.amjcard.2009.05.009
Nissen SE, Nicholls SJ, Wolski K, Rodes-Cabau J, Cannon CP, Deanfield JE, et al.: Effect of rimonabant on progression of atherosclerosis in patients with abdominal obesity and coronary artery disease: the STRADIVARIUS randomized controlled trial.JAMA 2008, 299:1547–60. 10.1001/jama.299.13.1547
Nissen SE, Nicholls SJ, Wolski K, Nesto R, Kupfer S, Perez A, et al.: Comparison of pioglitazone vs glimepiride on progression of coronary atherosclerosis in patients with type 2 diabetes: the PERISCOPE randomized controlled trial.JAMA 2008, 299:1561–73. 10.1001/jama.299.13.1561
Nissen SE, Nicholls SJ, Sipahi I, Libby P, Raichlen JS, Ballantyne CM, et al.: Effect of very high-intensity statin therapy on regression of coronary atherosclerosis: the ASTEROID trial.JAMA 2006, 295:1556–65. 10.1001/jama.295.13.jpc60002
Matsuzaki M, Hiramori K, Imaizumi T, Kitabatake A, Hishida H, Nomura M, et al.: Intravascular ultrasound evaluation of coronary plaque regression by low density lipoprotein-apheresis in familial hypercholesterolemia: the Low Density Lipoprotein-Apheresis Coronary Morphology and Reserve Trial (LACMART).J Am Coll Cardiol 2002, 40:220–7. 10.1016/S0735-1097(02)01955-1
Jensen LO, Thayssen P, Pedersen KE, Stender S, Haghfelt T: Regression of coronary atherosclerosis by simvastatin: a serial intravascular ultrasound study.Circulation 2004, 110:265–70. 10.1161/01.CIR.0000135215.75876.41
Takayama T, Hiro T, Yamagishi M, Daida H, Hirayama A, Saito S, et al.: Effect of rosuvastatin on coronary atheroma in stable coronary artery disease: multicenter coronary atherosclerosis study measuring effects of rosuvastatin using intravascular ultrasound in Japanese subjects (COSMOS).Circ J 2009, 73:2110–7. 10.1253/circj.CJ-09-0358
Nasu K, Tsuchikane E, Katoh O, Tanaka N, Kimura M, Ehara M, et al.: Effect of fluvastatin on progression of coronary atherosclerotic plaque evaluated by virtual histology intravascular ultrasound.JACC Cardiovasc Interv 2009, 2:689–96.
Hattori K, Ozaki Y, Ismail TF, Okumura M, Naruse H, Kan S, et al.: Impact of statin therapy on plaque characteristics as assessed by serial OCT, grayscale and integrated backscatter-IVUS.JACC Cardiovasc Imaging 2012, 5:169–77. 10.1016/j.jcmg.2011.11.012
Gandelman K, Fung GL, Messig M, Laskey R: Systemic exposure to atorvastatin between Asian and Caucasian subjects: a combined analysis of 22 studies.Am J Ther 2012, 19:164–73. 10.1097/MJT.0b013e3181f28fb5
Yang J, Li LJ, Wang K, He YC, Sheng YC, Xu L, et al.: Race differences: modeling the pharmacodynamics of rosuvastatin in Western and Asian hypercholesterolemia patients.Acta Pharmacol Sin 2011, 32:116–25. 10.1038/aps.2010.169
Lee E, Ryan S, Birmingham B, Zalikowski J, March R, Ambrose H, et al.: Rosuvastatin pharmacokinetics and pharmacogenetics in white and Asian subjects residing in the same environment.Clin Pharmacol Ther 2005, 78:330–41. 10.1016/j.clpt.2005.06.013
Nakamura H, Arakawa K, Itakura H, Kitabatake A, Goto Y, Toyota T, et al.: Primary prevention of cardiovascular disease with pravastatin in Japan (MEGA Study): a prospective randomised controlled trial.Lancet 2006, 368:1155–63. 10.1016/S0140-6736(06)69472-5
Tirona RG: Ethnic differences in statin disposition.Clin Pharmacol Ther 2005, 78:311–6. 10.1016/j.clpt.2005.07.006
Dohi T, Miyauchi K, Okazaki S, Yokoyama T, Yanagisawa N, Tamura H, et al.: Early intensive statin treatment for six months improves long-term clinical outcomes in patients with acute coronary syndrome (Extended-ESTABLISH trial): a follow-up study.Atherosclerosis 2010, 210:497–502. 10.1016/j.atherosclerosis.2009.12.001
Miyauchi K, Daida H, Morimoto T, Hiro T, Kimura T, Nakagawa Y, et al.: Reverse vessel remodeling but not coronary plaque regression could predict future cardiovascular events in ACS patients with intensive statin therapy–the extended JAPAN-ACS study.Circ J 2012, 76:825–32. 10.1253/circj.CJ-12-0135
D’Ascenzo F, Agostoni P, Abbate A, Castagno D, Lipinski MJ, Vetrovec GW, et al.: Atherosclerotic coronary plaque regression and the risk of adverse cardiovascular events: a meta-regression of randomized clinical trials.Atherosclerosis 2013, 226:178–85. 10.1016/j.atherosclerosis.2012.10.065
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1471-2261/15/6/prepub
Author information
Authors and Affiliations
Corresponding authors
Additional information
Competing interests
The authors declare that they have no competing interests. This study was not funded.
Authors’ contributions
LYF, FQZ, GWQ and ZXJ carried out data extraction, participated in the analysis and drafted the manuscript. CYD and HY participated in the design of the study, helped to draft the manuscript, and participated in its statistical analysis. All authors read and approved the final manuscript.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Li, YF., Feng, QZ., Gao, WQ. et al. The difference between Asian and Western in the effect of LDL-C lowering therapy on coronary atherosclerotic plaque: a meta-analysis report. BMC Cardiovasc Disord 15, 6 (2015). https://doi.org/10.1186/1471-2261-15-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2261-15-6